Abstract
Objective
This study aimed to investigate the effectiveness and safety of a method combining double-balloon catheter for cervical ripening and intravenous drip of oxytocin on the induction of term labor, providing the reference for clinical safety.
Methods
A total of 120 pregnant women with a gestation between 37+0 and 41+6 weeks, indications of labor induction, singleton pregnancy with cephalic presentation were enrolled. The patients were divided into the research group receiving cervical dilation balloon combined with intravenous drip of oxytocin and the control group receiving an intravenous drip of oxytocin at a concentration of 0.5% for labor induction (n = 60 for each). The effectiveness and safety of labor induction were evaluated by the rates of successful cervical ripening promotion and labor induction, as well as the vaginal delivery rate, induced labor time, total duration of labor, the total amount of postpartum hemorrhage within 24 h after giving birth, the incidences of postpartum hemorrhage, cervical laceration, puerperal infection and neonatal outcomes.
Results
There was no statistical difference in the basal demographic and clinical characteristics, including ages, gestational weeks, delivery times and Bishop scores at admission between two groups. The rate of successful cervical ripening promotion (research vs. control = 90.00% vs. 55.00%), the rate of successful induction (95.00% vs. 40.00%), the vaginal delivery rate (93.33% vs. 63.33%), the induced labor time (15.03 ± 5.40 vs. 30.68 ± 10.82 h), and the total duration of labor (8.12 ± 2.65 vs. 15.01 ± 6.06 h) were significantly different between two groups (all P < 0.05). There was no significant difference in the total amount of postpartum hemorrhage, incidences of postpartum hemorrhage, cervical laceration, puerperal infection as well as the neonatal outcomes, including neonatal weight, neonatal asphyxia and incidence of meconium aspiration syndrome between two groups.
Conclusions
Compared to labor induction of oxytocin, the method combining double-balloon catheter for cervical ripening and intravenous drip of oxytocin for the induction of term labor has a higher vaginal delivery rate, shorter total duration of labor, and does not increase the incidences of postpartum hemorrhage and neonatal infection, which is a more effective and safer method for induction of term labor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The labor induction in late pregnancy refers to use of drugs or other interventions to start labor before natural labor to achieve vaginal delivery. The labor induction in late pregnancy is commonly used for preventing post-term pregnancy, relieving or alleviating maternal complications, protecting the fetus from the adverse intrauterine environment, which is a common method used to treat high-risk pregnancy in obstetrics [1]. In a delayed pregnancy (pregnancy ≥ 41 but < 42 weeks), the risk of maternal and infants will elevate with the increase of gestational ages, which is usually required timely elective delivery [2, 3]. In addition, patients with oligohydramnios, gestational hypertension or gestational diabetes mellitus would also have a high risk for labor induction to terminate the pregnancy [4,5,6,7,8,9].
The optimal age at giving birth is 24–29 years when the women are mature with high egg quality and fewer pregnancy complications. In the women aged more than 35 years, the fertility significantly declines and the time from attempting to get pregnant to successful pregnancy would prolong. Even getting pregnant, women in advanced maternal age will have an increased risk of pregnancy complications, such as gestational diabetes mellitus and gestational hypertension [10]. However, at present, delayed childbearing has become a global problem [11,12,13,14], leading to increasing the high-risk pregnancy and the need for labor induction to terminate the pregnancy. Currently, the rate of induction of term labor is up to 30% [15].
Regarding the patients with delayed pregnancy, oligohydramnios, gestational hypertension or gestational diabetes mellitus, the cervix has usually not ripened when labor induction. It has been shown that the Bishop score ≤6 indicates that the cervical condition is poor and the rate of successful labor induction is low. While the Bishop score is >8, the vaginal delivery rate is close to the spontaneous delivery rate [16].
The methods for promotion of cervical ripening and labor induction include pharmacological labor induction (such as oxytocin, prostaglandin E1, E2) and mechanical labor induction (such balloon, hygroscopic cervical dilator) [17,18,19,20].
The conventional oxytocin labor induction is a safe, low cost and easily operated method which is still commonly used in primary hospitals such as township hospitals. However, its effect on the improvement of the cervical condition is relatively weak, and the rate of successful labor induction is low.
Although prostaglandin for promoting cervical ripening and labor induction has good improvement in the cervical condition, it may have risks for induction of frequent uterine contractions, rigid uterine contractions, third-degree perineal laceration, fetal distress, and neonatal asphyxia [21].
The double-balloon catheter is a new mechanical method for promotion of cervical ripening. The two balloons placed on the internal and external cervical orifice cause pressure and stimulate the cervix to release prostaglandin, promoting cervical ripening. In China, the double-balloon catheter for cervical ripening is rarely used, and clinical study is still required to comprehensively investigate its safety and effectiveness. This study aimed to evaluate the safety and effectiveness of cervical dilation balloon combined with intravenous drip of oxytocin for promoting cervical ripening and induction of term labor by comparison with the conventional oxytocin induction.
Materials and methods
Participants
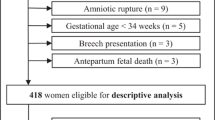
A total of 120 term-pregnant women hospitalized between January 2014 and June 2015 with indications of labor induction were enrolled. All the patients received examinations of blood routine, urine routine, biochemistry, liver and kidney functions, coagulation functions, vaginal discharge, color Doppler ultrasound, electrocardiogram, fetal heart rate monitoring (nonstress test, NST), Bishop score, vaginal examination and estimation of fetal weight. The inclusion criteria were: (1) 18–40 years old; (2) 37+0–41+6 gestational weeks; (3) Bishop score ≤6 before labor induction; (4) single alive fetus with cephalic presentation; (5) in cephalopelvic proportion; (6) without premature rupture of membrane; (7) NST reaction type before labor induction. The indications of labor induction included delayed pregnancy, oligohydramnios (amniotic fluid index = 3.0–8.0 cm), gestational diabetes mellitus, intrahepatic cholestasis of pregnancy, good control of gestational hypertension, with vaginal trial production condition and required pregnancy termination.
Exclusion criteria were patients with serve maternal complications and could not tolerate or undergo vaginal delivery, including (1) placenta previa, vasa previa and antepartum hemorrhage; (2) invasive cervical carcinoma; (3) untreated human immunodeficiency virus infection; (4) allergic to induction drugs [22].
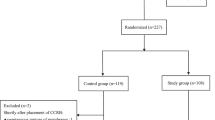
The 120 patients were randomly divided into the research group receiving double-balloon catheter for cervical ripening combined with intravenous drip of oxytocin for labor induction and the control group receiving an intravenous drip of oxytocin at a concentration of 0.5% (n = 60 for each). Informed consent was obtained from all the patients. This study was approved by the institutional review board of the Longgang District Center Hospital of Shenzhen.
Materials
Double-balloon catheter (Type CVB-18F) was obtained from Shenzhen Yixinda Medical New Technology Co. Ltd., China. Oxytocin injection (10 IU/piece, lot no. 141217-1) was obtained from Anhui Fengyuan Pharmaceutical Co., Ltd, China.
Clinical interventions
The control group received an intravenous drip of oxytocin at a concentration of 0.5%. At 9 a.m. on the first day, 2.5 IU of oxytocin was diluted in 500 ml of 0.9% sodium chloride injection. The initial drip rate was 8 drops/min, and if there were no regular contractions, the drip rate was increased by 4 drops every 15 min, with a maximal drip rate of 40 drops/min. If there were still no regular contractions after completion of the 2.5 IU of oxytocin, the concentration of oxytocin was adjusted to 1%. If there were still no regular contractions after 12 h of intravenous drip, artificial rupture of membranes will be taken and the intravenous drip was stopped to let the patient have a rest. At 9 a.m. on the second day, the patient was evaluated by Bishop score and received intravenous drip of oxytocin again as the previous day. If the pregnant women could not enter the stage of active labor within 48 h, the labor induction was regarded as failing and other methods for pregnancy termination were used.
In the research group, cervical dilation balloon was placed at 9 pm on the first day. (1) The patients were in the lithotomy position, and the vulva, vagina and cervix were disinfected. The cervix was clipped with a cervical clamp, and the balloon catheter was inserted into the cervical tube and pushed toward uterine cavity to make both balloons pass through the internal cervical orifice; (2) 40 ml of 0.9% sodium chloride was injected into the uterine balloon, making the cervical balloon close to the internal cervical orifice and vaginal balloon placed outside the cervical orifice; (3) 20 ml of 0.9% sodium chloride was injected into vaginal balloon; (4) the fluid amount in the cervical balloon and vaginal balloon was alternatively increased by 20 ml each time until both totally reached to 80 ml. The proximal end of the catheter was fixed on the lower abdomen of pregnant women.
The pregnant women had a normal rest on the night. For the patients without spontaneous labor or rupture of membrane, after 12 h, the balloons were removed at 9 a.m. on the second day, and were evaluated by Bishop score again and underwent artificial rupture of membranes. The condition of amniotic fluid and fetal heart rate was monitored for 1 h. If the patients were not in labor, 0.5% oxytocin was given to induce uterine contractions the same as the control group. If the patients did not enter the stage of active labor within 48 h, the labor induction was regarded as failing, and other methods for pregnancy termination were used.
Evaluation of effectiveness
For evaluation of the effect of promoting cervical ripening, the Bishop scores were compared between before and 12 h after the labor induction. The increased scores of ≥ 3, 2 and < 2 were regarded as significantly effective, effective and ineffective, respectively.
Effect of labor induction: patients entered the stage of active labor within 24 h, and 25–48 h were regarded as significantly effective, and effective, respectively. The patients who did not enter the stage of active labor after 48 h were regarded as ineffective. The patients who entered the stage of active labor within 24 h or 25–48 h, but were switched to cesarean section due to labor stagnation or fetal distress, were still regarded as significantly effective or effective, respectively. The rate of successful labor induction = number of cases that entered the stage of active labor within 48 h/60.
Delivery ways: the cases of vaginal spontaneous labor, forceps delivery and cesarean section were recorded. Vaginal delivery rate = the number of vaginal spontaneous labor cases plus the number of forceps delivery cases/60.
The induced labor time was defined as the time from application of labor induction to the occurrence of regular uterine contractions. Total duration of labor was defined as the time from the occurrence of regular uterine contractions to the delivery of placenta. The total amount of postpartum hemorrhage within 24 h after giving birth was recorded.
Evaluation of safety
The incidences of postpartum hemorrhage, cervical laceration, uterine rupture, puerperal infection, neonatal asphyxia, neonatal infection and meconium aspiration syndrome were recorded.
The definition of neonatal asphyxia is according to neonatal Apgar score in 5 min. The Apgar score consisted of 5 items including heart rate, respiration, muscle tone, laryngeal reflex, and skin color, each of which was 0–2 points, with a total score of 10. Apgar score in 5 min, 8–10 scores normal, 4–7 scores mild asphyxia, 0–3 scores severe asphyxia.
Statistical analysis
All the statistical analyses were performed using the SPSS 19.0 statistical software. Shapiro–Wilk test was used for normality analysis, and a P > 0.05 indicated that the data were in normal distribution. The T test was used for analyzing the data with a normal distribution, while Mann–Whitney U was applied for analyzing the data with non-normal distribution. The χ2 test was used for the comparison of proportions between groups. A value of P < 0.05 was considered statistically significant.
Results
General information
The general information included ages, gestational ages, delivery times and Bishop score at admission. Among them, ages and gestational ages were of normal distribution, while delivery times and the Bishop scores were of non-normal distribution (Table 1).
Effect of promoting cervical ripening
After the application of cervical dilation balloon for 12 h in the research group and an intravenous drip of oxytocin for 12 h in the control group, the Bishop scores were 6.14 ± 1.88 and 4.83 ± 1.83 (both with normal distribution), respectively. The rate of successful promoting cervical ripening in the research group and the control group was 90.00 and 55.00%, respectively. The difference was statistically significant (Table 2).
Effect of labor induction
The rate of successful labor induction in the research group and the control group was 95.00 and 40.00%, respectively. The difference was statistically significant (P < 0.05) (Table 3).
Vaginal delivery rate
There were 56 cases with vaginal delivery (4 cases with forceps delivery) in the research group. Among them, 39 cases delivered within 24 h, 15 cases delivered within 25–48 h, and 2 cases were switched to other labor induction methods due to the failure of induction and underwent spontaneous delivery after 48 h. The vaginal delivery rate was 93.33%. There were 4 cases with cesarean section, and the indications of cesarean section were persistent occiput posterior, relative cephalopelvic disproportion and fetal distress.
There were 38 cases with vaginal delivery in the control group (2 cases with forceps delivery). Among them, 6 cases delivered within 24 h, 14 cases delivered within 25–48 h, and 18 cases were switched to other labor induction methods due to the failure of induction and underwent spontaneous delivery after 48 h. The vaginal delivery rate was 63.33%. There were 22 cases with cesarean section, and the indications of cesarean section were fetal distress and abnormal labor. The vaginal delivery rate in the research group was higher than that in the control group (P < 0.05, Table 4).
Induced labor time and total duration of labor
In the research group, the induced labor time and total duration of labor were 15.03 ± 5.40 and 8.12 ± 2.65 h, respectively, which were shorter than those in the control group (30.68 ± 10.82 and 15.01 ± 6.06 h, respectively, P < 0.05).
Maternal and neonatal outcomes
The amount of postpartum hemorrhage within 24 h after giving birth in the research group and the control group was 292.33 ± 71.61 ml and 295.93 ± 78.38 ml, respectively. There were no statistical differences in the incidences of postpartum hemorrhage, cervical laceration and puerperal infection between groups (all P > 0.05). The neonatal weight in the research group and the control group was 3.10 ± 0.31 and 3.21 ± 0.25 kg, respectively. The incidences of neonatal asphyxia, neonatal infection and meconium staining of the amniotic fluid were not statistically different between groups (Table 5).
One case of MAS in the study group, 1 case of MAS in the control group, the incidences of MAS were both 1.67% in these two groups.
Discussion
Cervical ripening mainly refers to the softening, shortening, disappearance and dilatation of the cervix. Any factors that affect the activities of collagenase and elastase, as well as the changes of matrix composition, can affect cervical ripening [10]. The histochemical changes during the process of cervical ripening include enhancing collagenase and elastase activities, fragmentation, dissolution and content decrease of collagen, a decrease of chondroitin sulfate, softening of the cervix, an increase of cervical water content, as well as decrease, loosening and separation of collagenous fiber. In late pregnancy, the factors such as strong mechanical stimulation and endocrine change can lead to cervical softening and ripening, oxytocin releasing and promotion of regular uterine contractions, resulting in labor [23,24,25,26]. Most of the pregnant women with delayed pregnancy requiring early pregnancy termination do not have the mature cervical condition. Pharmacological or mechanical stimulation can be used for promotion of cervical ripening to make the cervix softened, thinned and expanded, shortening the time from labor induction to delivery [27].
The common methods for promotion of cervical ripening and labor induction include pharmacological (such as oxytocin, prostaglandin E1, E2) and mechanical stimulation (such as balloon, hygroscopic cervical dilator).
The oxytocin acts on the receptors on the uterine smooth muscle cells, making the smooth muscle contracted and cervix expanded. Oxytocin also can stimulate the synthesis of prostaglandins via decidual oxytocin receptor, leading to cervical softening, which has an effect on promotion of cervical ripening as well as induction and enhancement of contractions. The oxytocin is low cost and does not have a direct effect on the fetus. It does not pass through the placenta, but has the risks to induce excessively strong contractions and fetal distress [28]. There are few oxytocin receptors in the cervix; therefore, the oxytocin has little direct effect on the cervix. In addition, patients with an intravenous drip of oxytocin require being especially monitored the vital signs of pregnant women, contractions and fetal heart rate. The activity of pregnant women is limited and the induced labor time is relatively long, and the pregnant women and their family members easily get anxiety. This study showed that after the intravenous drip of oxytocin for 12 h, the Bishop score and the rates of successful cervical ripening promotion and induction in the control group were lower than those in the research group.
The double-balloon catheter for cervical ripening is a new device for the promotion of cervical ripening, and its main principles of promoting cervical ripening are as follows: the catheter and the balloons at the internal and external cervical orifices cause moderate and persistent tension to expand the cervix. The distal balloon close to the internal cervical orifice has a stripping effect on the fetal membrane, and promotes the synthesis and releasing of prostaglandins at the local cervix, which in turn promote the cervical softening and ripening as well as contractions [29,30,31]. In this study, cervical dilation balloon combined with subsequent low-dose oxytocin had an effect on the induction and enhancement of contractions, which significantly shortened the time of labor, improved the rate of successful labor induction and vaginal delivery rate, and decreased the cesarean section rate.
It has been reported that the rate of the double-balloon catheter for successful cervical ripening and labor induction ranges 75–92% [1]. In this study, the research group had a rate of successful promoting cervical ripening of 90.00%, which was further elevated up to 95% after combining with an intravenous drip of oxytocin (both higher than that of the control group), indicating that this method is effective for the promotion of cervical ripening and labor induction. However, there were only 8 patients receiving pure double-balloon catheter for cervical ripening, and they underwent spontaneous delivery before removing cervical balloon or within 1 h after removing cervical balloon, suggesting that the balloon catheter did not have a strong effect on the induction of contractions so that combining with intravenous drip of oxytocin was necessary for most patients.
This study showed that both balloon combined with intravenous drip of oxytocin and pure intravenous drip of oxytocin could be used for labor induction and promotion of vaginal delivery. Double-balloon catheter for cervical ripening combined with intravenous drip of oxytocin for labor induction was superior to pure oxytocin in the rate of successful cervical ripening promotion, the rate of successful induction, vaginal delivery rate, shortening the induced labor time and total duration of labor. It did not increase the incidences of postpartum hemorrhage, cervical laceration, uterine rupture, puerperal infection, neonatal asphyxia and infection, and meconium aspiration syndrome.
The incidences of MAS in these two groups were both 1.67%. The possible reasons why there were MSAF and MAS in this research may be: induction of labor for late pregnancy was usually because of pathological pregnancy, such as prolonged pregnancy, oligohydramnios, intrahepatic cholestasis of pregnancy syndrome, pregnancy-induced hypertension or gestational diabetes mellitus. These pathological pregnancies were usually accompanied with adverse placental function or fetal intrauterine anoxia. In addition, the regular uterine contractions which occurred after the launch of labor can also aggravate fetal intrauterine anoxia.
The cervical dilatation double balloon was used to make cervical ripening, and the catheter and the double balloon provide a gentle and lasting tension to dilate the cervix; the distal balloon close to the endocervix has a peeling effect on fetal membranes; promoting prostaglandin synthesis and release in the local cervix, thereby promoting cervical softening and inducing uterine contraction. Using the cervical dilatation double balloon itself does not produce contractions directly, and it is relatively safe.
The cervical dilatation double balloon itself does not produce uterine contractions directly, so after using it to attain cervical maturity, the subsequent use of oxytocin to induce contractions should be needed. This process improves the rate of successful labor induction, shortens the time from labor to birth, and reduces the occurrence of uterus contractions which are too strong or too frequently, fetal distress and amniotic fluid embolism complications at the same time.
References
Bacak SJ, Olsonchen C, Pressman E (2015) Timing of induction of labor. Semin Perinatol 39:450–458
Alimena S, Nold C, Herson V, Fang YM (2016) Rates of intrauterine fetal demise and neonatal morbidity at term: determining optimal timing of delivery. J Matern Fetal Neonatal Med 30:181–185
Torricelli M, Voltolini C, Conti N, Bocchi C, Severi FM, Petraglia F (2013) Weight gain regardless of pre-pregnancy BMI and influence of fetal gender in response to labor induction in postdate pregnancy. J Matern Fetal Neonatal Med 26:1016–1019
Rezaie KK, Keikha F, Rezaie KK, Abdollahimohammad A, Salehin S (2014) Perinatal outcome after diagnosis of oligohydramnious at term. Iran Red Crescent Med J 16:e11772
Moore TR (2011) The role of amniotic fluid assessment in indicated preterm delivery. Semin Perinatol 35:286–291
Shibata T, Nakago S, Kato H, Tokuda H, Matsuki R, Kotsuji F (2016) Management of severe pregnancy-induced hypertension after 34 weeks of gestation: a prospective study to reduce the rate of cesarean section. Hypertens Pregnancy 35:82–90
Garcia-Simon R, Montañes A, Clemente J, Del Pino MD, Romero MA, Fabre E, Oros D (2015) Economic implications of labor induction. Int J Gynaecol Obstet 133:112–115
Feghali MN, Caritis SN, Catov JM, Scifres CM (2016) Timing of delivery and pregnancy outcomes in women with gestational diabetes. Am J Obstet Gynecol 215:241–243
Kalra B, Gupta Y, Kalra S (2016) Timing of delivery in gestational diabetes mellitus: need for person-centered, shared decision-making. Diabetes Therapy 7:1–6
Committee EI, Committee MFM, Liu K, Case A (2011) Advanced reproductive age and fertility. Int J Gynecol Obstet 33:1165
Behboudigandevani S, Ziaei S, Farahani FK, Jasper M (2015) The perspectives of iranian women on delayed childbearing: a qualitative study. J Nurs Res 23:313–321
Balasch J, Gratacós E (2012) Delayed childbearing: effects on fertility and the outcome of pregnancy. Curr Opin Obstet Gynecol 24:187
Olusanya BO, Solanke OA (2012) Perinatal correlates of delayed childbearing in a developing country. Arch Gynecol Obstet 285:951–957
Joseph KS, Allen AC, Dodds L, Turner LA, Scott H, Liston R (2005) The perinatal effects of delayed childbearing. Obstet Gynecol 105:1410–1418
Rath W (2005) A clinical evaluation of controlled-release dinoprostone for cervical ripening—a review of current evidence in hospital and outpatient settings. J Perinat Med 33:491–499
Laughon SK, Zhang J, Troendle J, Sun L, Reddy UM (2011) Using a simplified Bishop score to predict vaginal delivery. Obstet Gynecol 117:805
Mozurkewich EL, Chilimigras JL, Berman DR, Perni UC, Romero VC, King VJ, Keeton KL (2011) Methods of induction of labour: a systematic review. BMC Pregnancy Childbirth 11:84
Alfirevic Z, Keeney E, Dowswell T, Welton NJ, Medley N, Dias S, Jones LV, Gyte G, Caldwell DM (2016) Which method is best for the induction of labour? A systematic review, network meta-analysis and cost-effectiveness analysis. Health Technol Assess 20:1–584
Kehl S, Böhm L, Weiss C, Heimrich J, Dammer U, Baier F, Sütterlin M, Beckmann MW, Faschingbauer F (2016) Timing of sequential use of double-balloon catheter and oral misoprostol for induction of labor. J Obstet Gynaecol Res 42:1495–1501
Kansu-Celik H, Gun-Eryılmaz O, Dogan NU, Haktankaçmaz S, Cinar M, Yilmaz SS, Gülerman C (2017) Prostaglandin E2 induction of labor and cervical ripening for term isolated oligohydramnios in pregnant women with Bishop score ≤5. J Chin Med Assoc 80:169–172
Kacvinska A, Drab M, Totka A, Holoman K, Gabor M (2016) The effect of prostaglandin induced labor and selected factors on the occurrence and extent of birth-canal injuries. Bratisl Lek Listy 117:511–514
Tolcher MC, Holbert MR, Weaver AL, Mcgree ME, Olson JE, El-Nashar SA, Famuyide AO, Brost BC (2015) Predicting cesarean delivery after induction of labor among nulliparous women at term. Obstet Gynecol 126:1059–1068
Jozwiak M, Mol BW, Bloemenkamp KW (2010) Induction of labour in nulliparous women with an unfavourable cervix. BJOG 117:892
Iliodromiti Z, Antonakopoulos N, Sifakis S, Tsikouras P, Daniilidis A, Dafopoulos K, Botsis D, Vrachnis N (2012) Endocrine, paracrine, and autocrine placental mediators in labor. Hormones 11:397–409
Zhao Y, Koga K, Osuga Y, Izumi G, Takamura M, Harada M, Hirata T, Hirota Y, Yoshino O, Fujii T (2013) Cyclic stretch augments production of neutrophil chemokines and matrix metalloproteinase-1 in human uterine smooth muscle cells. Am J Reprod Immunol 69:240–247
Gonzalez JM, Dong Z, Romero R, Girardi G (2011) Cervical remodeling/ripening at term and preterm delivery: the same mechanism initiated by different mediators and different effector cells. PLoS ONE 6:e26877
Ivars J, Garabedian C, Devos P, Therby D, Carlier S, Deruelle P, Subtil D (2016) Simplified Bishop score including parity predicts successful induction of labor. Eur J Obstet Gynecol Reprod Biol 203:309–314
Springhall E, Wallace EM, Stewart L, Knight M, Mockler JC, Davies-Tuck M (2017) Customised management of the third stage of labour. Aust N Z J Obstet Gynaecol 57:302–307
Malmnäs C (1969) Induction of labour in the second and third trimester of pregnancy by a cervical balloon and intrauterine oxytocin infusion. Acta Obstet Gynecol Scand 48(Suppl 3):18+
Dueñas-Garcia OF, Young CA, Mikhail M (2010) Uterine rupture secondary to the use a cook balloon as tamponade. J Minim Invas Gyn 17:S187
Ducarme G, Grange J, Vital M (2016) Expansion dilatation balloons for cervical ripening in obstetric practice. J Gynecol Obstet Biol Reprod (Paris) 45:112–119
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This study was supported by the grants from the Nature Science Foundation of China (81470015 and 81670256), the Science and Technology Project of Special Funds of Guangzhou (2014J4100168), Guangdong Science and Technology Project (2016A020216005, 2015B090903063 and 2015A020212006), the Natural Science Foundation of Guangdong Province (2014A030313079) and Guangzhou Science and Technology Project (201510010052).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the institutional review board of Longgang District Center Hospital of Shenzhen.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Wu, X., Wang, C., Li, Y. et al. Cervical dilation balloon combined with intravenous drip of oxytocin for induction of term labor: a multicenter clinical trial. Arch Gynecol Obstet 297, 77–83 (2018). https://doi.org/10.1007/s00404-017-4564-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-017-4564-9