Abstract
Purpose
Low levels of plasmatic pregnancy-associated plasma protein-A (PAPP-A) and high levels of free-beta human chorionic gonadotropin (beta-hCG) could influence the outcome of pregnancy. The objective of this study is to assess the correlation between PAPP-A and free beta-hCG and birth weight.
Materials and methods
Prospective follow-up study performed on 3332 patients in the first trimester of pregnancy who were subjected to a screening test focused on evaluation of fetal aneuploidy (SCA-TEST). The values of PAPP-A and free beta-hCG were both analyzed as raw values and subsequently converted to a multiple of the median (MoM). Statistical analysis was performed using SPSS version 17.0.1 (SPSS Inc., Chicago, USA).
Results
The incidence of “small for gestational age” in patients with PAPP-A MoM <1st and <5th ‰ was statistically significant (12 and 9.8 %; p < 0.0001). Also statistically significant data have been highlighted about free beta MoM > 95th ‰ (7 %; p = 0.03). The values of PAPP-A MoM > 99th ‰ are significantly correlated with an increased risk of “large for gestational age” (16.7 %; p < 0.0001).
Conclusion
Our study demonstrates that specific values of PAPP-A and free beta-hCG could identify the risk of low or high birth weight since the first trimester of pregnancy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the last few years, a particular attention has been placed on fetal growth restriction (FGR), in order to detect early predictors and to reduce the high morbidity and mortality associated to this complication. Today the evaluation of fetal growth could take advantage of prenatal imaging techniques, which allow a more careful study using accurate curves of estimated fetal weight, built and individualized on unselected populations. Based on various studies conducted over the past decade, it is clear that in the first trimester we could suspect the onset of some obstetric complications, such as FGR or premature labor/birth [1–4]. Particularly, some authors have given special emphasis to the evaluation of some proteins examined during the screening for fetal aneuploidy in the first trimester of pregnancy [5–7].
The analysis of the literature showed how different clinical and biological factors, including the findings of low levels of plasmatic pregnancy-associated plasma protein-A (PAPP-A) and high levels of free-beta human chorionic gonadotropin (beta-hCG), could influence the outcome of pregnancy. PAPP-A is a glycoprotein produced by trophoblast syncytium; it appears in maternal blood in early pregnancy and its value increases during the gestation until the end of the same [8].
Conserva et al. [8] have shown that a value of PAPP-A < 5th ‰ for gestational age is associated with obstetric complications such as preterm labor and low birth weight (<10th ‰). A low value of this glycoprotein was detected only in cases of vascular insufficiency, such as fetuses with intra-uterine growth restriction (FGR) or preterm birth [9, 10]. The same studies demonstrated how glycoprotein PAPP-A has a key role in the development of the placenta in early pregnancy [10, 11].
The combined test (SCA-TEST) also provides the evaluation of free beta-hCG, whose values have been studied in the first trimester of pregnancy to confirm if it has any influence on birth weight. As environments with low oxygen levels have higher production of free beta-hCG by chorionic villus sampling, it is possible that this condition occurs in a pregnancy with gestational hypertensive syndrome or FGR. The study performed by Goetzinger et al. [10] confirmed that levels of free beta-hCG > 95th ‰ for gestational age are associated with a low birth weight.
In view to reduce perinatal mortality and morbidity in fetuses with diagnosis of FGR, some authors have focused their attention on the study of the placenta and placental vascularization, as there is a reduced supplementation of oxygen by mother to fetus. The results have shown that low levels of PAPP-A are associated with an increased incidence of obstetric complications. The volume of the placenta, as previously demonstrated by Metzenbauer et al. [12, 13], is reduced in pregnant women with low levels of this glycoprotein, even if it, as only predictive value, would be insufficient to have a clinical role to identify FGR [14].
The objective of the present study is to assess the correlation between PAPP-A and free beta-hCG in the first trimester of pregnancy and birth weight.
Materials and methods
Population study
We performed a prospective follow-up study on 3332 patients in the first trimester of pregnancy (between 11 + 0 and 13 + 6 gestational weeks), who were subjected to a screening test focused on the evaluation of fetal aneuploidy (SCA-TEST) at the Center for Prenatal Diagnosis and Fetal Medicine Maternal Artemisia Main Center of Rome, in the period between January 2007 and December 2008. The study protocol was approved by the Ethics Committee and conformed to the ethical guidelines of the Helsinki Declaration (as revised in Tokyo, 2004). Each woman signed an informed consent before entering the study, and her anonymity was preserved.
Study design
The patients who required the execution of SCA-TEST to evaluate the combined risk of Down syndrome from a population of unselected women were considered eligible for the study. The social and medical history of the mother (age, ethnicity, BMI, smoking, diabetes) and the pregnancy history (gestational age, spontaneous or IVF pregnancy, treatment with progesterone) were obtained during the execution of the screening test, and included in a database. The effective gestational age was calculated by last menstrual period (LMP) and measurement of CRL (between 42 and 85 mm). We included only Caucasian women with single pregnancies; and live fetuses, without any fetal defects observed during the ultrasound exam to evaluate NT and CRL. All enrolled patients were recorded and identified by a personal number. The ultrasound used to perform scans were “© Voluson 730 Pro” and “Voluson E8 ©” General Electrics. The probes used were 2D transabdominal probes (4.5–16.5 MHz).
NT measurement
The scan of the fetus should be median sagittal (to make sure that you have got a proper scan, you have to display the fetal profile) and it has to be done by an adequate zoom showing fetus that fills three-quarters of the screen image, displaying profile and upper chest. An essential element is to differentiate fetal skin and amniotic membrane. We have to wait so that the fetus moves slightly away from the membrane itself. The fetus has to be in a “neutral” position (Fig. 1), not too extended and not particularly flexed; the same scan has to be used to measure CRL. In a hyper-extended position it may overestimate the detection of NT. The caliper should be sited on the point of maximum thickness of NT and the inner edge of the two-internal hyperechoic lines. In the examination, several measurements should be performed and, the measurement which has better followed the above requirements has to be used in the calculation of risk. In 95 % of cases, the measurement of NT could be obtained by transabdominal scan; in the remaining 5 % of the cases the trans-vaginal scan is used, when the NT is borderline, or when there is a low echogenicity, due to the low acoustic impedance of pregnancy tissues.
CRL measurement
CRL should be measured with the fetus in a sagittal, neutral position (neither hyper nor overflexed), excluding the yolk sac. The measurement is obtained by maximum length of fetal echoes, by calipers sited at the cephalic extreme and at the end of the fetal trunk, with a straight line between the two poles; it should be between 42 and 85 mm.
Dosage of biochemical markers
The kit used to evaluate the levels of free beta-hCG and PAPP-A were the BRAHMS free beta-hCG and the PAPP-A KRIPTOR CAL., two automatic system based on immunofluorescence. According to previous scientific studies [8], normal range of the two markers was processed in relation to the different gestational age (Manual SCA-TEST-vers 2.0 SIDi.P.). For the free beta-hCG, see Table 1. For the PAPP-A see Table 2.
Uterine artery velocimetry
When the patients underwent to our center for the screening of fetal aneuploidy during the first trimester of pregnancy, we analyzed the pulsatility index of both uterine arteries. As each arterial fluximetric wave also the uterine artery has an increased flow’s phase during ventricular contraction (systolic flow) and a reduced speed flow’ step during ventricular relaxation (diastolic flow). PI and RI express the correlation between systolic flow and diastolic flow. The reference values indicate when there is a mean value of PI more than 1.45 the flowmetry of the uterine arteries is called “inadequate”. The sonographer has to perform doppler ultrasound when the patient is placed in a slightly lateral decubitus, holds her breath and has not any uterine contraction. Then we evaluated the mean value of the measurements on the arteries of the two sides (left and right). Not respecting these conditions could lead to an increased vascular impedance for the compression of myometrial vessels (arcuate, radial and spiral arteries).
Follow-up
Patients were contacted by a telephone interview by a doctor of the center, who was not aware of the combined test screening results. The following information was recorded: date of birth, mode of delivery (spontaneous vaginal delivery/operative delivery or caesarean section), birth weight, maternal diseases complicating pregnancy (gestational diabetes and hypertension), maternal and/or fetus complications at delivery, and presence of neonatal abnormalities and/or disease.
Statistical analysis
Assuming an incidence of SGA in the order of 4 %, with a test power of 80 % and a significance level of 5 %, we needed 2400 fetuses to verify the differences in the incidence of the two groups determined by percentile equal to 5 %; 3332 patients were considered eligible for the study. The considered variables, such as BMI, gestational age at delivery and maternal age were expressed as mean ± standard deviation (M ± SD), while qualitative variables were expressed as a percentage (%). A linear model of logistic regression has been used for statistical analysis of the data.
The values of PAPP-A and free beta-hCG, studied at 1st, 5th, 95th and 99th ‰, were both analyzed as raw values and subsequently converted to a multiple of the median (MoM) in order to assess the association with small for gestational age (SGA) babies and large for gestational age (LGA) babies through the univariate analysis.
Statistical analysis was performed using SPSS version 17.0.1 (SPSS Inc., Chicago, USA). The test used to calculate the p value related to the smoke and to velocimetry of uterine arteries was the Fisher’s Exact Test for Count Data. A p value <0.05 was considered statistically significant.
Results
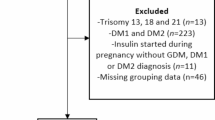
From January 2007 to December 2008, altogether 3332 women came to our center for the evaluation of nuchal translucency (NT) and enrolled in the study; 113 were excluded (2.7 %) for spontaneous miscarriage, 67 (1.6 %) for major fetal abnormalities, 279 (6.7 %) for twin pregnancies, 69 (2 %) were not Caucasian women, and 4 (0.01 %) women had diabetes. In the evaluation of PAPP-A and free beta-hCG, 250 patients were ruled out due to a computer problem; 72 patients were lost to follow-up. Overall a total of 2478 women were identified and analysed.
The SGA patients (<5th ‰) were 50 (2.0 %), the SGA (<10th ‰) were 74 (2.7 %) and LGA patients (>95th ‰) were finally 1418 (55.6 %).
The association between incidence of SGA (<5th and <10th ‰) and LGA (>95th ‰) and the dosage of serum PAPP-A MoM and free beta MoM was assessed by univariate analysis. The incidence of SGA in patients with PAPP-A MoM < 1st ‰ was statistically significant (12 %; p < 0.0001), as well as in patients with PAPP-A MoM < 5th ‰ (9.8 %; p < 0.0001). Also statistically significant data have been highlighted regarding values of free beta MoM > 95th ‰ (7 %; p = 0.03); on the opposite way, however, it does not show any statistical significance analysis of the raw values of PAPP-A > 99th ‰ (p = 0.13) (Tables 3, 4, 5).
By analysis of the association between the values of PAPP-A MOM and free Beta MOM with LGA, it was shown that: the values of PAPP-A MoM > 99th ‰ are correlated with an increased risk of LGA with high statistical significance (16.7 %; p < 0.0001), however no statistical significance was found between the values of free Beta MOM and risk of LGA. The results are shown in Tables 6 and 7. We have analyzed other variables, which could affect the birth of infants SGA or LGA such as BMI, gestational age at delivery (GAD), maternal age at birth, sex, smoking and preterm delivery (PP). Regarding the BMI, this factor seems to affect fetal growth only in the case of a SGA < 5th ‰ and a BMI of the mother significant (22.7 ± 2.8 vs 21.7 ± 6.0 SD; p = 0.02); considering instead a SGA < 10th ‰ maternal BMI does not affect fetal growth (21.7 ± 6.1 vs 21.7 ± 5.9 SD). However a difference, extremely significant from a statistical point of view, is evident among patients who gave LGA birth: these patients, in fact, have a higher BMI (22.2 ± 5.6 vs 21.2 ± 6.3 SD). Low GAD and high maternal age at delivery statistically significantly correlate with the risk of SGA births. Particularly the GAD has a high statistical significance in both the case of SGA < 5th ‰ (34.4 ± 2.6 vs 39.2 ± 1.7 DS) that in the case of SGA < 10th ‰ (34.9 ± 2.7 vs 39.3 ± 1.7 DS). Maternal age would seem instead to have a more important role in the incidence of SGA < 5th ‰ compared to SGA < 10th ‰ (34.6 ± 4.9 vs 32.9 ± 4.0 SD; 34.3 ± 5.3 vs 32.9 ± 4.0 SD). Some considered variables (BMI, GAD and maternal age at delivery) correlate statistically significantly with LGA babies.
The smoke instead seems to not affect statistically on the birth of SGA infants <5th ‰ (p = 0.62) nor SGA infants <10th ‰ (p = 0.78); it does not affect born LGA babies (p = 0.67). As for the sex of the baby, it is more likely that an SGA infant is female, and conversely, LGA infants are male.
Another variable that we analyzed was the incidence of preterm deliveries (<37 weeks) in patients with a low value of plasmatic PAPP-A. In this sense, our study showed a high rate of correlation between values of PAPP-A MoM > 95th ‰ (19.8 %; p < 0.0001) or even values of PAPP-A MoM > 99th ‰ (37.5 %; p < 0.0001) and preterm birth, with a low incidence and statistical significance for values of PAPP-A MoM <1stand <5th ‰ (p = 0.002; p = 0.003). The values of free Beta MoM on the other side seem to affect the risk of preterm birth only if >95th ‰ (p = 0.01).
In multivariable analysis, considering the four subdivisions of PAPP-A MoM, free Beta hCG MoM, maternal age and preterm birth, shows that a value of PAPPA-A MoM < 5th ‰, a value of free Beta hCG MoM > 95th ‰, maternal age and preterm delivery correlate, independently from each other with the risk of SGA and could therefore be considered predictors.
Considering all these variables studied, because the analysis of the literature we have found that several authors have also evaluated the level of uterine artery Doppler flow in the first trimester of gestation, our ultimate goal was to evaluate our population results. Then we divided our cohort of patients into two groups. From 132 patients with PAPP-A < 5th ‰, the first group were women with Uta PI values >95th ‰ and the second group of women with Uta PI values <95th ‰.
The analysis obtained also confirmed in our data a significant incidence of risk of SGA infants (<10th ‰) (p < 0.0001) (Table 8).
Discussion
Several authors have focused their attention to find biomarkers or predictors of obstetric complications, such as preterm birth, pre-eclampsia or FGR [3–8]. In particular, relatively to fetal growth restriction, it was demonstrated by scientific literature that a low value of plasmatic PAPP-A, dosed during the first trimester of pregnancy is associated with low birth weight [8]. Since the first trimester is therefore possible, according to these studies, to identify risk conditions of SGA or FGR, through the combination of demographic characteristics and maternal and fetal parameters using biochemical markers that are part of screening for fetal aneuploidy [8, 10, 15–17].
Our study in fact, in line with what has already been written in the literature, confirms that a low level of PAPP-A MOM (<1 and <5th ‰) as well as a high value of free BetaMOM (>95th ‰) are associated with SGA babies [10, 15]. It was also highlighted as a value of PAPP-A MOM > 99th ‰ is highly correlated with the incidence of LGA births (16.7 %; p < 0.001).
By adding maternal characteristics such as BMI, gestational age at birth, maternal age and smoking, we wanted to analyze whether these factors could have an effect on birth weight. Univariate analysis in which were introduced the above variables, BMI does not affect SGA infants, if we consider a value <10th ‰, on the contrary, instead, a high value of maternal BMI, in agreement with what has already been described by Goetzinger [10], influence the birth of an infant with weight >95th ‰ with a significant statistical difference (p < 0.0001). A statistically significant difference could be detected in our study evaluating the gestational age at delivery with a significant statistic both in the case of a value <5th ‰ in the case of a value <10th ‰ (p < 0.0001). In the same way we could highlight that higher is the maternal age higher will be the risk to have a child with SGA < 5th and <10th ‰ (respectively: p < 0.002, p < 0.02).
About a high birth weight (LGA), the three just considered variables affect our sample; then it is more likely that in this case women have a higher BMI, gestational age at delivery and a greater age (p < 0.0001, p < 0.0001; p = 0.002). Our data are in line with what is written in the literature [15, 18]. Considering also other variable such as the smoke we saw that it does not affect in any way the birth weight considering the SGA as LGA.
The women who smoke have the same risk to have a child SGA compared to non-smoking women, since it is in contrast with the literature [19]. This could be linked to several factors: as one of more frequent obstetric complications is preterm delivery (<37 weeks) we wanted to assess whether the value of PAPP-A and free beta-hCG could in any way affect the incidence. Actually there is a big difference between the two plasma proteins, as the free Beta hCG MoM seem to have no role in the prediction of preterm delivery. On the other side PAPP-A MoM value, if either <1st and the 5th ‰ is that if >95th and >99th ‰, has a statistically significant impact on the risk of this complication (respectively p = 0.002 and p = 0.003, p < 0.0001 and p < 0.0001). Such value is in line with what has been described in the literature by Conserva et al. [8], who found that an association between preterm birth and low birth weight was probably linked to vascular insufficiency of the placenta.
In view of the fact that low birth weight is one of the most frequent obstetric complications, there are several studies, which were performed to recognize the possible causes. It is known that the placenta has a key role in growth and incidence of fetal complications related to this failure (pre-eclampsia, FGR, preterm birth). The impedance of blood flow in the uterine arteries decreases during pregnancy reflecting the invasion of trophoblast into the spiral arteries and converting them into low-resistance vessels. The value of uterine artery Doppler flow has been shown to have utility in identifying diseases such as pre-eclampsia with placental insufficiency and FGR [20–22]. A value of UTA PI > 95th ‰ is considered pathological.
Based on what was also analyzed by other authors in the scientific literature [20, 23], we added another important variable: the measurement of uterine artery velocimetry (UTA PI). In the first trimester, the study of these arteries has a diagnostic sensitivity for low birth weight of 25 %; however, it has a number of false positives by 5–10 %.
The analysis of these two groups highlights that the risk of FGR in the second group of pregnant women is higher with a statistically significant difference. Then it seems likely that the combination of two very important variables may increase the risk of having a baby with a low birth weight; this fact confirms once again that the study of the uterine circulation plays an important role in the identification of pregnant women at risk of obstetric complications.
In conclusion, our study demonstrates, in agreement with what was observed in other works, the possibility, since the first trimester of pregnancy, of identifying women with risk of developing infants with low birth weight.
The strength of our study is characterized not only by the size of the sample but also by the fact that it is a prospective case–control and that the study population is predominantly low-risk. It proposes several questions, based mainly on the doctor-patient relationship, which mainly concern the kind of approach we have to keep with the pregnant woman, who, after identifying the above risk factors, needs explanations about complications that could take over.
References
Bukowski R, Smith GC, Malone FD, Ball RH, Nyberg DA, Comstock CH, FASTER Research Consortium et al (2007) Fetal growth in early pregnancy and risk of delivering low birth weight infant: prospective cohort study. BMJ 334(7598):836
Dugoff L, Society for Maternal-Fetal Medicine (2010) First- and second-trimester maternal serum markers for aneuploidy and adverse obstetric outcomes. Obstet Gynecol 115(5):1052–1061
Krantz D, Goetzl L, Simpson JL, Thom E, Zachary J, Hallahan TW, First Trimester Maternal Serum Biochemistry and Fetal Nuchal Translucency Screening (BUN) Study Group et al (2004) Association of extreme first-trimester free human chorionic gonadotropin-beta, pregnancy-associated plasma protein A, and nuchal translucency with intrauterine growth restriction and other adverse pregnancy outcomes. Am J Obstet Gynecol 191(4):1452–1458
Roman A, Desai N, Krantz D, Liu HP, Rosner J, Vohra N et al (2014) Maternal serum analytes as predictors of IUGR with different degrees of placental vascular dysfunction. Prenat Diagn 34(7):692–698
Smith GC, Crossley JA, Aitken DA, Jenkins N, Lyall F, Cameron AD et al (2007) Circulating angiogenic factors in early pregnancy and the risk of preeclampsia, intrauterine growth restriction, spontaneous preterm birth, and stillbirth. Obstet Gynecol 109(6):1316–1324
Proctor LK, Toal M, Keating S, Chitayat D, Okun N, Windrim RC et al (2009) Placental size and the prediction of severe early-onset intrauterine growth restriction in women with low pregnancy-associated plasma protein-A. Ultrasound Obstet Gynecol 34(3):274–282
Lees C (2010) First-trimester screening for pre-eclampsia and fetal growth restriction: a test seeking both a treatment and an optimal timing. Ultrasound Obstet Gynecol 35(6):647–649
Conserva V, Signaroldi M, Mastroianni C, Stampalija T, Ghisoni L, Ferrazzi E (2010) Distinction between fetal growth restriction and small for gestational age newborn weight enhances the prognostic value of low PAPP-A in the first trimester. Prenat Diagn 30(10):1007–1009
Goldenberg RL, Culhane JF, Iams JD, Romero R (2008) Epidemiology and causes of preterm birth. Lancet 371(9606):75–84
Goetzinger KR, Singla A, Gerkowicz S, Dicke JM, Gray DL, Odibo A (2009) The efficiency of first-trimester serum analytes and maternal characteristics in predicting fetal growth disorders. Am J Obstet Gynecol 201(4):412.e1–412.e6
Goetzinger KR, Singla A, Gerkowicz S, Dicke JM, Gray DL, Odibo AO (2010) Predicting the risk of pre-eclampsia between 11 and 13 weeks’ gestation by combining maternal characteristics and serum analytes, PAPP-A and free β-hCG. Prenat Diagn 30(12–13):1138–1142
Metzenbauer M, Hafner E, Hoefinger D, Schuchter K, Stangl G, Ogris E et al (2001) Three-dimensional ultrasound measurement of the placental volume in early pregnancy: method and correlation with biochemical placenta parameters. Placenta 22(6):602–605
Metzenbauer M, Hafner E, Schuchter K, Philipp K (2002) First-trimester placental volume as a marker for chromosomal anomalies: preliminary results from an unselected population. Ultrasound Obstet Gynecol 19(3):240–242
Rizzo G, Capponi A, Pietrolucci ME, Capece A, Arduini D (2009) First-trimester placental volume and vascularization measured by 3-dimensional power Doppler sonography in pregnancies with low serum pregnancy-associated plasma protein a levels. J Ultrasound Med 28(12):1615–1622
Papastefanou I, Souka A, Eleuftheriades M, Pilalis A, Kassanos D (2012) First trimester fetal ultrasound parameters associated with PAPP-A and fβ-hCG. J Matern Fetal Neonatal Med 25(7):1029–1033
Papastefanou I, Souka AP, Pilalis A, Eleftheriades M, Michalitsi V, Kassanos D (2012) First trimester prediction of small- and large-for-gestation neonates by an integrated model incorporating ultrasound parameters, biochemical indices and maternal characteristics. Acta Obstet Gynecol Scand 91(1):104–111
Pilalis A, Souka AP, Antsaklis P, Daskalakis G, Papantoniou N, Mesogitis S et al (2007) Screening for pre-eclampsia and fetal growth restriction by uterine artery Doppler and PAPP-A at 11-14 weeks’ gestation. Ultrasound Obstet Gynecol 29(2):135–140
Poon LC, Karagiannis G, Staboulidou I, Shafiei A, Nicolaides KH (2011) Reference range of birth weight with gestation and first-trimester prediction of small-for-gestation neonates. Prenat Diagn 31(1):58–65
Carbone JF, Tuuli MG, Bradshaw R, Liebsch J, Odibo AO (2012) Efficiency of first-trimester growth restriction and low pregnancy-associated plasma protein-A in predicting small for gestational age at delivery. Prenat Diagn 32(8):724–729
Goetzinger KR, Cahill AG, Kemna J, Odibo L, Macones GA, Odibo AO (2012) First-trimester prediction of preterm birth using ADAM12, PAPP-A, uterine artery Doppler, and maternal characteristics. Prenat Diagn 32(10):1002–1007
Dugoff L, Lynch AM, Cioffi-Ragan D, Hobbins JC, Schultz LK, Malone FD, FASTER Trial Research Consortium et al (2005) First trimester uterine artery Doppler abnormalities predict subsequent intrauterine growth restriction. Am J Obstet Gynecol 193(3):1208–1212
Spencer K, Yu CK, Cowans NJ, Otigbah C, Nicolaides KH (2005) Prediction of pregnancy complications by first-trimester maternal serum PAPP-A and free beta-hCG and with second-trimester uterine artery Doppler. Prenat Diagn 25(10):949–953
Odibo AO, Zhong Y, Longtine M, Tuuli M, Odibo L, Cahill AG et al (2011) First-trimester serum analytes, biophysical tests and the association with pathological morphometry in the placenta of pregnancies with preeclampsia and fetal growth restriction. Placenta 32(4):333–338
Acknowledgments
The present article has been realized also thanks to the important scientific collaboration with Dr Francesca Romana Giorlandino (Department of Biochemistry - Altamedica Main Center - Rome - Italy) and Dr Diana Giannarelli (Department of Statistics - National Cancer Institute "Regina Elena" - Rome - Italy).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Cignini, P., Savasta, L.M., Gulino, F.A. et al. Predictive value of pregnancy-associated plasma protein-A (PAPP-A) and free beta-hCG on fetal growth restriction: results of a prospective study. Arch Gynecol Obstet 293, 1227–1233 (2016). https://doi.org/10.1007/s00404-015-3947-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-015-3947-z