Abstract
Purpose
The available literature on the treatment options for recurrent or metastatic endometrial cancer (EC) is full of controversies. Therefore, we explore the results of the AGO pattern of care studies from the years 2013, 2009 and 2006.
Methods
A questionnaire was developed and sent to all 682 German gynecological departments in 2013 (775 in 2009, 500 in 2006, respectively). The results of the questionnaires were compared with each other using Fisher’s exact test.
Results
Responses were available in 40.0 % in 2013, 33.3 % in 2009 and 35.8 % in 2006. In 2013 the most preferred endocrine drug was progestin (79.8 %), followed by tamoxifen (42.8 %), aromatase inhibitor (19.8 %), fulvestrant (16.3 %) and a combination (3.9 %) (p < 0.001). 65.3, 59.8, 51.7 and 38.2 % of the participants used platinum, taxane, a combination of cytostatic drugs, anthracycline in metastatic EC, respectively (p = 0.215). 96.2, 92.7, 49.8 and 60.9 % of the participants performed an operation, radiotherapy, endocrine therapy and chemotherapy in 2013 because of a local recurrence, respectively (p < 0.001). Compared to 2009 and 2006 these rates remained stable (no p value <0.05). Because of a distant metastasis 50.4, 64.2, 78.5 and 90.8 % of the participants performed an operation, radiotherapy, endocrine therapy and chemotherapy in 2013, respectively (p < 0.001). Compared to 2009 and 2006 more participants performed an operation or radiotherapy and less an endocrine treatment.
Conclusions
Whereas progestin was the favorite drug, the participants of this study did not prefer a specific cytostatic drug for metastatic EC in 2013. This might have reflected the available literature, which did not provide a real standard of care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
More than 11,500 women develop endometrial cancer (EC) per year in Germany [1]. The 5-year survival rate amounts to be 81 % [1]. Therefore, a distinct fraction of patients is faced with local recurrence or distant metastasis.
Distant metastasis is fatal whereas some patients presenting with a central recurrence of the pelvis might be cured by surgery and/or radiotherapy [2–4]. The 5-year survival rates of the latter ranges between 21 and 60 % [3, 4]. Conversely, patients being not suitable for these treatment options are faced with a short median overall survival of approximately 12 months and 3-year survival rates of 8–14 % [2, 5]. Therefore, these patients require tolerable treatment modalities in order to palliate symptoms, preserve quality of life and delay the progression of disease.
The available literature on these treatment options is full of limitations, partially contradictory and therefore conclusive recommendations are not available [6–8]. Therefore we explored the results of the Arbeitsgemeinschaft Gynäkologische Onkologie (AGO) pattern of care studies from 2013, 2009 and 2006, in order to describe whether the use of treatment modalities changed during 2013 and 2006. Furthermore we tried to elucidate which is the favorite cytostatic and endocrine drug among German gynecologists for patients with recurrent or metastatic EC.
Materials and methods
A questionnaire was created in order to explore the common therapeutic approaches on EC in 2006 and was modified for the surveys in 2009 and 2013. Here, we report the results of 4 multiple-choice questions dealing with the treatment decisions for recurrent and metastatic EC. The results on the surgical procedures and on the treatment decisions for primary EC were published elsewhere [9, 10]. The questionnaire was sent to all German gynecological departments in November 2013, in August 2009 and in March 2006. The list of the addresses was provided by the German Society of Gynecology and Obstetrics (DGGG, Deutsche Gesellschaft für Gynäkologie und Geburtshilfe). A data-extraction form was compiled before reviewing the questionnaires as described before [9–11]. Briefly, a questionnaire was excluded from the whole analysis, if no question concerning the treatment decisions was answered. If a single question was not answered, the questionnaire was excluded from the analysis of the single question. Thereby, the reported percentages reflect the portion of participants, who answered the question and not who participated at the whole survey. We compared the results of the 2013, 2009 and 2006 questionnaires using Fisher’s Exact Test, in order to describe potential changes in the treatment behavior during this time period. In a last step we performed a subgroup-analysis in order to explore whether the characteristics of the participating centers (see Table 1) influenced the treatment decisions. SPSS 21 (SPSS Inc, Chicago, IL, USA) was used for statistical analyses.
Results
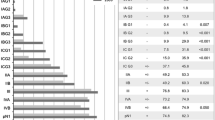
In 2013 273 out of 682 (40.0 %), in 2009 258 out of 775 (33.3 %) and in 2006 179 out of 500 (35.8 %) hospitals answered the questionnaire, respectively. Characteristics of the participating centers are summarized in Table 1. One questionnaire was excluded from the 2006 analysis as no question was answered.
In 2013 the most frequent used endocrine agent was progestin (79.8 %), followed by tamoxifen (42.8 %), aromatase inhibitor (19.8 %), fulvestrant (16.3 %) and a combination of endocrine therapy (3.9 %) (p < 0.001) (see Table 2).
In 2013 65.3, 59.8, 51.7 and 38.2 % of the participants used platinum, taxane, a combination of cytostatic drugs and anthracycline, respectively (p = 0.215) (see Table 3).
For patients with local recurrence 96.2 % of the interviewed colleagues performed an operation, 92.7 % performed radiotherapy, 49.8 % used endocrine therapy and 60.9 % used chemotherapy in 2013 (p < 0.001) (see Table 4). These rates were largely unchanged in 2013 compared to 2009 and 2006 (all p values >0.05) (see Table 4). For patients with metastatic EC 50.4 % of the interviewed colleagues performed an operation, 64.2 % performed radiotherapy, 78.5 % used endocrine therapy and 90.8 % used chemotherapy in 2013 (p < 0.001) (see Table 5). Compared to 2009 these rates remained largely unchanged (p values >0.05). Conversely, in 2006 less colleagues performed an operation and radiotherapy but more colleagues used endocrine therapy (p values <0.05) (see Table 5).
According to the subgroup analyses patients received more often tamoxifen, aromatase inhibitor and fulvestrant if they were treated at a university hospital compared to teaching hospitals or any other hospitals (all p values <0.05) (see Table 2). Furthermore, patients received more often a platinum, taxane or anthracycline containing chemotherapy or a combination if they were treated at a university hospital or at a teaching hospital compared to any other hospital (all p values <0.05) (see Table 3). However, suggroup analyses depicted no further difference if other characteristics of the participating centers were used for stratification like size of hospitals, educational status of the participants or membership at AGO (data not shown).
Discussion
The major findings of the here presented analyses are: (a) progestins are the most often used endocrine drugs, (b) there is no favorite chemotherapy, (c) most participants use chemotherapy to treat metastatic disease, (d) treatment of local recurrence remained largely unchanged over time favoring operation and radiotherapy and (e) subgroup analyses only depicted a difference in terms of the preferred endocrine and cytostatic drugs, if the type of hospital was used for stratification.
To date no randomized trial has been completed to address the question whether patients with advanced, recurrent of metastatic EC should first receive an endocrine treatment or chemotherapy. According to our results more participants used chemotherapy (90.8 %) as endocrine treatment (78.5 %) in 2013. There is an agreement to a certain extent that patients with asymptomatic metastatic disease suffering from a low grade, endometroid EC should receive endocrine treatment [7, 8]. Endocrine drugs have been mostly tested in phase II studies with less than 100 patients [7]. Therefore, response rate has emerged as decision-making end-point [7]. Conclusively, no standard of care exists and the choice of the systemic drug bases on a cross-study comparison with all its limitations. Historically, progestins have been evaluated since the 1960s with variable response rates [7]. First studies report response rates up to 56 % but later trials report response rates between 15 and 25 % and a median time of progression of 2.5 months as more rigid definitions of response have been used [7]. Interestingly, the majority of our participants (79.8 %) seems to be convinced by these data and use progestins. The GOG have tested a combination of progestins (medroxy progesterone acetate or megestron acetate) together with tamoxifen because estrogenic compounds like tamoxifen have shown to increase the expression of progesterone receptor [12, 13]. The reported response rates have been higher (27 and 33 %) and favor the combination [12, 13]. On the other side, the progression-free survival and overall survival remain largely unchanged [12, 13]. Among the participants of our study only 3.9 % opted for this opportunity. Of course, the reasons of this go beyond the scope of the study and are speculative. The efficacy of tamoxifen, letrozole or anastrozole alone is small with a response rate of roughly 10 % in phase II studies [14–16]. Fulvestrant alone achieves a partial response in 11 % and stable disease in 23 % out of 35 patients [17]. Despite the more or less same response rates, the participants of our studies use tamoxifen (42.8 %) more often as aromatase inhibitors (19.8 %) or fulvestrant (16.3 %).
Beside these endocrine treatment options cytotoxic agents like platinum, anthracyclines and taxanes have shown activity in various phase II studies [6]. In these trials Paclitaxel show response rates between 30.4 and 35.7 % as first line treatment and response rates between 22.2 and 27.3 % as second line treatment [18–21]. Doxorubicin achieved response rates of 37.2 % and the rates for Cisplatin ranges between 20 and 42 % as a first line treatment [6]. Remarkably, with the exception of four trials the majority of all phase II trial does not include more than 50 patients [6]. Furthermore a dozen randomized phase III are available comparing different chemotherapeutical regimens with variable quality [6]. Historically, doxorubicin plus cisplatin was accepted as the GOG standard combination regimen in the 1990s [22]. With the emergence of paclitaxel, GOG 177 compared doxorubicin plus cisplatin with or without paclitaxel in 1998–2000 [23]. The triplet shows a higher response rate of 57 % and—as an exception of the available trials—a benefit in overall survival (15.3 vs. 12.3 %, p = 0.037) [23]. In 2012, GOG 209 has been published as abstract and compared this triplet with carboplatin plus paclitaxel [24]. As the doublet is non-inferior in terms of efficacy but less toxic as the triplet, carboplatin plus paclitaxel arises as something like the today standard combination regimen in metastatic EC [24]. According to a meta-analysis more intense combination chemotherapy improves significantly disease-free survival and slightly improves overall survival [6]. In summary, the clinicians are faced to outbalance the modest gain in terms of overall survival (3 months benefit in the GOG 177) of combination chemotherapy with an increased risk of toxicity in a cohort of sick patients who finally will decease after roughly a little bit more than one year [6]. Our participants slightly favor platinum (65.3 %) and taxanes (59.8 %) over a combination of chemotherapy (51.7 %) or anthracyclines (38.2 %).
In contrast to the very low 3-year survival rates of 8 and 14 % for patients with distant metastasis and lateral pelvic recurrence, respectively, some patients might be cured if central recurrence of pelvic malignancy occurs [2]. Various studies report 5-year overall survival rates between 21 and 60 % after pelvic exenteration [3, 4]. However, they are faced with various short and long term complications affecting nearly every patient [4]. Salvage radiotherapy in a case of central recurrence achieves a 77 % response rate and a 3-year survival rate of 73 % [2]. Indeed, the participants of our study opt for the surgical approach and for the radiotherapy in this setting and are in line with those data (Tables 4, 5).
Subgroup analyses were able to depict a difference only if type of hospital was used for stratification (see Tables 2, 3). Patients, being treated at university hospitals compared to teaching hospitals or any other hospitals, received more often another endocrine treatment than progestins in a case of metastatic disease. For sure, explanations for these finding are rather speculative and go beyond the scope of the study. Possibly, progestins might represent a more traditional approach in the treatment of metastastic EC as they were introduced in the 1960s [7]. Contrastingly, the other endocrine agents were tested during the last decade in various trials [14–17]. Possibly, university hospitals and teaching hospitals, which participate more often in clinical trials, preferred these drugs. Remarkably, no differences were detectable in terms of size of hospitals, membership at AGO or the disposition of a gynecological oncologist among the here presented questions.
To the best of our knowledge, this is the first nationwide study analyzing patterns of care in more than 700 German hospitals over a time period of 7 years at three different time points. For sure, limitations inherent to questionnaire-based data must be recognized as a potential weakness of this study in contrast to clinical chart-based data or tumor registry-based data. However, the two last approaches may feature other limitations. German tumor registries for example do not provide detailed information on the cytostatic and endocrine drugs. Clinical chart-based data might be the most authentic source but the effort might be exorbitant for the interviewed colleagues. Conclusively, a very low return rate and a selection bias might occur. Moreover one might assume that the provided list of German hospitals in 2006 was not complete as only 500 hospitals were mentioned in contrast to 775 hospitals in 2009. However, the difference of 775–682 hospitals in 2013 might be reasonable due to austerity program and a consecutive closing and pooling of German hospitals. Moreover, a certain limitation might result from the fact, that it is not clear, who compiled the questionnaire in each center. In summary, a certain bias might occur as less than a half of all German hospitals participated in all our three surveys and as the answers of the colleagues might not be as realistic as data out of clinical charts or tumor registries. However, the advantage of a questionnaire might overbalance these problems as it allows to gather more detailed information in a nationwide analysis of gynecologic departments.
In conclusion, local recurrence and distant metastasis of EC were more or less treated in the same way during 2006 and 2013 in Germany. Interestingly, only the type of hospital altered treatment decisions in terms of the preferred endocrine and cytostatic drug according to the subgroup analyses. Size of the participating hospitals or the disposition of a gynecological oncologist or the membership in the AGO did not lead to any difference suggesting a more or less equal treatment among German hospitals in 2013. Whereas progestins were the most often used endocrine drug in recurrent or metastatic EC, the participants of the study did not prefer a certain cytostatic drug. This might have reflected the available, inconsistent and limited literature not providing a real standard of care in this topic of gynecologic oncology.
References
Gebärmutterkörper (2010) Krebs in Deutschland 80–83. Accessed at http://www.rki.de/Krebs/DE/Content/Publikationen/Krebs_in_Deutschland/kid_2013/kid_2013_c54-55_gebaermutterkoerper.pdf;jsessionid=D687D7570E564374CAB3C53CCABF8F0E.2_cid390?__blob=publicationFile
Creutzberg CL, van Putten WLJ, Koper P et al (2003) Survival after relapse in patients with endometrial cancer: results from a randomized trial. Gynecol Oncol 89:201–209
Fleisch MC, Pantke P, Beckmann MW et al (2007) Predictors for long-term survival after interdisciplinary salvage surgery for advanced or recurrent gynecologic cancers. J Surg Oncol 95:476–484
Westin SN, Rallapalli V, Fellman B et al (2014) Overall survival after pelvic exenteration for gynecologic malignancy. Gynecol Oncol 134:546–551
Temkin SM, Fleming G (2009) Current treatment of metastatic endometrial cancer. Cancer Control 16:38–45
Humber CE, Tierney J, Symonds R (2007) Chemotherapy for advanced, recurrent or metastatic endometrial cancer: a systematic review of Cochrane collaboration. Ann Oncol 18:409–420
Sommeijer DW, Sjoquist KM, Friedlander M (2013) Hormonal treatment in recurrent and metastatic gynaecological cancers: a review of the current literature. Curr Oncol Reports 15:541–548
Bradford LS, Rauh-Hain JA, Schorge J et al (2013) Advances in the management of recurrent endometrial cancer. Am J Clin Oncol, PMID 23764681
Battista MJ, Schmidt M, Rieks N et al (2014) Nationwide analysis on surgical procedures for patients with endometrial cancer in Germany: Results of the AGO pattern of care studies from the years 2013, 2009, and 2006. J Canc Res Clin Oncol 140:2087–2093
Battista MJ, Schmidt M, Rieks N et al (2015) Adjuvant treatment decisions for patients with endometrial cancer in Germany: results of the nationwide AGO pattern of care studies from the years 2013, 2009, and 2006. J Canc Res Clin Oncol 141:555–562
Battista MJ, Steiner E, Rieks N et al (2013) Nationwide analysis on surgical staging procedures and systemic treatment for patients with endometrial cancer in Germany. Int J Gynecol Canc 23:105–112
Fiorica JV, Brunetto V, Hanjani P et al (2004) Phase II trial of alternating courses of megestrol acetate and tamoxifen in advanced endometrial carcinoma: a Gynecologic Oncology Group study. Gynecol Oncol 92:10–14
Whitney C, Brunetto V, Zaino R et al (2004) Phase II study of medroxyprogesterone acetate plus tamoxifen in advanced endometrial carcinoma: a Gynecologic Oncology Group study. Gynecol Oncol 92:4–9
Rose PG, Brunetto V, VanLe L et al (2000) A phase II trial of anastrozole in advanced recurrent or persistent endometrial carcinoma: a Gynecologic Oncology Group study. Gynecol Oncol 78:212–216
Thigpen BT, Brady MF, Homesley HD et al (2001) Tamoxifen in the treatment of advanced or recurrent endometrial carcinoma: A Gynecologic Oncology Group Study. J Clin Oncol 19:364–367
Ma B, Oza A, Eisenhauer E et al (2004) The activity of letrozole in patients with advanced or recurrent endometrial cancer and correlation with biological markers–a study of the National Cancer Institute of Canada Clinical Trials Group. Int J Gynecol Canc 14:650–658
Emons G, Günthert A, Thiel F et al (2013) Phase II study of fulvestrant 250 mg/month in patients with recurrent or metastatic endometrial cancer: a study of the Arbeitsgemeinschaft Gynäkologische Onkologie. Gynecol Oncol 129:495–499
Lissoni A, Zanetta G, Losa G et al (1996) Phase II study of paclitaxel as salvage treatment in advancer endometrial cancer. Ann Oncol 13:861–863
Ball HG, Blessing JA, Lentz SS et al (1996) Phase II trial of paclitaxel in patients with advanced or recurrent adenocarcinoma of the endometrium. Gynecol Oncol 281:278–281
Lincoln S, Blessing JA, Lee RB et al (2003) Activity of paclitaxel as second-line chemotherapy in endometrial carcinoma: a gynecologic oncology group study. Gynecol Oncol 88:277–281
Hirai Y, Hasumi K, Onose R et al (2004) Phase II trial of 3-h infusion of paclitaxel in patients with adenocarcinoma of endometrium: Japanese Multicenter Study Group. Gynecol Oncol 94:471–476
Obel J, Friberg G, Fleming G (2006) Chemotherapy in endometrial cancer. Clin Adv Hematol Oncol 6:459–468
Fleming GF, Brunetto V, Cella D et al (2004) Phase III trial of doxorubicin plus cisplatin with or without paclitaxel plus filgrastim in advanced endometrial carcinoma: a Gynecologic Oncology Group Study. J Clin Oncol 22:2159–2166
Miller D, Filiaci V, Fleming G et al (2012) Late-Breaking Abstract 1: Randomized phase III noninferiority trial of first line chemotherapy for metastatic or recurrent endometrial carcinoma: a Gynecologic Oncology Group study. Gynecol Oncol 125:771
Conflict of interest
The authors declare that they have no conflicts of interests and signed the conflict of interest form.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Battista, M.J., Schmidt, M., Eichbaum, M. et al. Management of recurrent or metastatic endometrial cancer in Germany: results of the nationwide AGO pattern of care studies from the years 2013, 2009 and 2006. Arch Gynecol Obstet 292, 1355–1360 (2015). https://doi.org/10.1007/s00404-015-3786-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-015-3786-y