Abstract
Objective
To assess differences between fetuses with isolated and non-isolated trisomy 21 in umbilical artery (UA) Doppler findings in the second and third trimester and to correlate those with placental histology.
Methods
Retrospective analysis of UA pulsatility index (PI) in 281 fetuses with trisomy 21. Cases were divided into isolated trisomy 21 (group I, n = 148, 52.7 %) and non-isolated trisomy 21 (group II, n = 133, 47.3 %). UA measurements were evaluated in five different time periods (A–E; <20 + 0 to ≥35 + 0 weeks) and were assigned histopathology of the placenta.
Results
In 118/281 (42 %) cases, UA measurement was abnormal. The frequency of PI values above the 95th percentile increased significantly with gestational age in both groups (period A 32.9 % vs. period E 63.6 %, p < 0.0001). There was neither a difference in abnormal UA PI values between isolated and non-isolated cases [37.8 % (56/148) vs. 46.6 % (62/133)] nor a correlation to placental findings.
Conclusions
Fetuses with trisomy 21 often present with elevated UA PI in the late second or third trimester, irrespective of small for gestational age growth, malformations or histopathological findings of impaired placentation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trisomy 21 is worldwide the most common chromosomal abnormality and occurs in 1 in every 600 live births [1, 2]. The prevalence of pregnancies affected by trisomy 21 has increased significantly in recent years, mainly due to increasing maternal age at birth [1, 3, 4].
Newborns with trisomy 21 exhibit a significantly lower birth weight compared to controls that range often between the 10th and 25th percentile [5, 6]. Growth dysfunction in trisomic fetuses can be primarily fetal in origin, but might also be the consequence of an impaired placentation. Disturbance of syncytiotrophoblast formation is observed in various pathological clinical conditions such as preeclampsia and intrauterine growth restriction, but also in trisomy 21. In vitro studies in trisomy 21-affected placentas demonstrated an abnormal trophoblast fusion in more than 90 %, accompanied by decrease in the synthesis and secretion of syncytiotrophoblastic pregnancy-associated hormones [7, 8]. Histological observations have indicated that trisomy 21 may be associated with large irregular hypovascular villi and abnormalities of the trophoblastic layer [8, 9]. In the third trimester, the placenta of trisomic (18, 13 and 21) fetuses exhibited a significant reduction in small muscular artery count and a small muscular artery to villous ratio [10]. Abnormal umbilical artery (UA) Doppler waveforms correlated strongly with these findings, but numbers examined were small [10]. Interestingly, there was a wide range in deviation and not all placentas with the same trisomy were uniformly affected [10]. There was no correlation of small muscular artery counts with fetal weight [10]. These data suggest that abnormal UA flow pattern might occur irrespective of fetal growth restriction in fetuses affected by autosomal trisomies. Other Doppler studies in fetuses with abnormal karyotypes revealed conflicting results [11–13]. In these studies, fetuses with different chromosomal aberrations were included. Other studies have been performed mainly in the first or early second trimester [14–16].
Therefore, the aim of the present study was to assess possible differences between fetuses with isolated and non-isolated trisomy 21 in UA Doppler findings in the second and third trimester in a large cohort and to correlate those findings with placental perfusion and histology.
Methods
This study is a cross-sectional study of UA pulsatility index (PI) in 281 fetuses with trisomy 21 between January 2002 and April 2012 in a single tertiary referral center. Gestational age was between 15 and 40 weeks. Appropriate patients were identified from our perinatal database using the key words “Down syndrome” and “trisomy 21”. Data were correlated with a second pediatric database. A total of 297 pregnancies with fetal or neonatal Down syndrome were identified, including three cases with trisomy 21 mosaicism. 16 pregnancies were excluded because of missing Doppler data, leaving 281 pregnancies for analysis.
Umbilical artery measurements were evaluated according to gestational age at first presentation in our department in five different time periods: A: ≤19 + 6 weeks, B: 20 + 0 to 24 + 6 weeks, C: 25 + 0 to 29 + 6 weeks, D: 30 + 0 to 34 + 6 weeks and E: ≥35 + 0 weeks. On average 2.3 UA PI values per pregnancy were documented. Only the first UA Doppler measurement of each case was considered for the study. All PI values were matched to 95 % confidence intervals of a normal control population using the reference curves of Martinez Crespo et al. [16] for the UA PI between 15 and 18 weeks of gestation and the one of Acharya et al. [17] for the UA PI between 19 and 40 weeks of gestation. The 95th percentile was used as a cut-off. Cases with trisomy 21 were divided into two main groups: group 1 contained isolated cases that demonstrated only soft markers or no sonographic abnormalities (n = 148, 52.7 %) and group 2 with non-isolated trisomy 21 (n = 133, 47.3 %) summarizing fetuses with miscellaneous malformations. Malformations comprised cardiac defects (n = 114), gastrointestinal anomalies (n = 19), and various effusions (n = 27). There were 38 fetuses with small for gestational age (SGA) growth, of those 18 belonged to group 1 and 20 to group 2. SGA was defined as either the abdominal circumference <5th percentile and/or a birth weight less than the 10th percentile.
Placental histology was documented in 141 cases. Histopathological examination of the placenta comprised placental weight and microscopic evaluation of placental villous maturation, existence of delayed villous maturation, endangiopathia obliterans, intervillous thrombi, placental infarct and villous stromal fibrosis.
Pathologists were blinded to UA Doppler data, but not to zytogenetic findings. Results of UA Doppler in isolated and non-isolated cases of trisomy 21 and placental histology were correlated.
For data analyses, the statistical software package SPSS 20.0 (SPSS Inc., Chicago, IL, USA) was used. Significance was assumed at p value of <0.05. Statistical analysis comprised 2-tail t test, Fisher´s exact test, Mann–Whitney U test and trend test.
Results
This study is a retrospective analysis of UA Doppler recordings in 281 pregnancies with trisomy 21. In 254 fetuses, the diagnosis was confirmed prenatally by karyotyping, in 18 cases the diagnosis was suspected prenatally but established after birth because parents declined invasive testing, and in 9 cases with unsuspicious prenatal ultrasound, trisomy 21 was diagnosed after birth. Mean maternal age was 35 years (range 17–49 years). On average, the first ultrasound examination took place at 22 weeks of gestation (range 14–39 weeks). 103 children were born alive (36.7 %), 13 fetuses suffered intrauterine fetal death (4.6 %) and 165 (58.7 %) pregnancies were terminated in accordance with German law regulations. For live birth, the mean gestational age was 37.4 (29–41) weeks and the mean birth weight was 2833 ± 644 g, which represents the 25th percentile.
Overall, 42.0 % (118/281) of UA PI values were above the 95th percentile according to reference curves. The frequency of PI values above the 95th percentile increased significantly with gestational age (period A 32.9 % vs. period E 63.6 %, Cochran–Armitage trend test p < 0.0001) (Table 1).
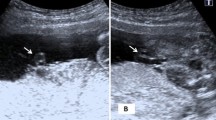
There were no differences in abnormal UA PI values in isolated and non-isolated cases of trisomy 21 [(37.8 % (56/148) vs. 46.6 % (62/133) Fishers exact test p = 0.2194)]. In cases with isolated trisomy 21, 4.1 % (6/148) presented with absent or reversed end-diastolic flow (ARED) in the UA. The corresponding number for non-isolated trisomy 21 was 4.5 % (6/133). Doppler measurements above the 95th percentile increased significantly with advancing gestation in both groups (Fig. 1). While the proportion of pathological UA Doppler findings in fetuses with isolated trisomy 21 increased stepwise from time period A to E, the rise in abnormal findings in non-isolated cases was most evident between interval B and C. In the last three time periods, the proportion of abnormal UA PI remained stable in non-isolated cases (Fig. 1). Statistical trend test revealed no significant values for both time courses (p = 0.44).
In 48/130 (36.9 %) cases, abnormal UA values occurred in fetuses without malformations or SGA, respectively. Mean birth weight was lower in fetuses with abnormal compared to fetuses with normal UA flow pattern, but differences did neither reach statistical significance (1371 vs. 1548 g, p < 0.47) in the whole cohort or in living pregnancies (2729 vs. 2922 g, p < 0.16).
In 141 of 281 (50.2 %) pregnancies, histologic evaluation of the placenta was available. Placental histology was mainly performed in the second trimester (time periods A–C, n = 121) and only in 15 % in time period D–E (n = 22), the mean gestational age was 24.4 ± 6.1 weeks. Mean placental weight was 233.5 ± 128.5 g. We found intervillous thrombi in 78.7 % (n = 111), retardation of villous maturation in 49.6 % (n = 70), arrest of villous maturation in 66 % (n = 93), increased numbers of vessels in 18.4 % (n = 26), decreased number of vessels in 12.1 % (n = 17) and stromal fibrosis in 20.6 % (n = 29). Endangiopathia was observed in 17 % (n = 24), subtrophoblastic calcification in 36.9 % (n = 52) and placental infarction in 4.3 % (n = 6).
Comparing the groups with normal (n = 76) and increased (n = 65) UA Doppler, we found more placentas with retardation or arrest of villous maturation (58.6 vs. 41.4 % and 59.1 vs. 40.9 %) in the group of isolated trisomy 21 and more endangiopathia (57.7 vs. 42.3 %) and higher number of vessels (54.2 vs. 45.8 %) in the second group. However, none of these findings gained statistical significance (p > 0.05). Differences in placental histology between the groups of isolated and non-isolated trisomy 21, as well as to the subgroup of SGA were also insignificant.
Discussion
Our study demonstrated abnormal UA Doppler recordings in 42.0 % of second- and third-trimester cases with trisomy 21. Furthermore, there was an increase in abnormal UA Doppler findings from the early second to the late third trimester of pregnancy (32.9 vs. 63.6 %). This is in contrast to normal pregnancies, where UA impedance decreases with increasing gestational age. The reduction of UA resistance is the result of an increase of the number and lumen of the vessels in tertiary villi of the placenta, a process that starts in the late first trimester [18]. Pathological recordings of UA PI have been described in association with several chromosomal aberrations [10, 13–15, 19]. The majority of the studies evaluated limited periods in pregnancies, most commonly the first or early second trimester. While in most first trimester studies no significant differences between fetuses with trisomy 21 and controls were found [14, 15, 20], one study reported significantly higher values of UA PI in cases of trisomy 21 compared to normal fetuses [21]. Martinez Crespo et al. [16] reported UA Doppler findings in 26 fetuses with chromosomal anomalies between 10 and 18 weeks of gestation. Of those with trisomy 21 investigated between 14 and 18 weeks, 33.3 % (3/9) showed values above the 95th percentile. These results are comparable to our findings (32.9 %) in period A.
Hecher et al. [22] analyzed second- and third-trimester Doppler studies of the UA in 20 fetuses with chromosomal anomalies, including 8 with trisomy 21. While none of the cases with trisomy 21 (n = 3) had abnormal Doppler findings in the second trimester, four of five cases (80 %) had UA PI values above the 95th percentile in the third trimester. Two of them were associated with SGA, but the other two presented without malformations or SGA [22]. In a series of 192 fetuses with absent UA end-diastolic velocity (ARED) flow >20 weeks, four (2.1 %) were diagnosed with trisomy 21 [13]. However, no specific information was given on associated conditions in these four cases. Others reported on three cases with trisomy 21 with fetal growth restriction and UA ARED flow in the third trimester [23]. In contrast to typical placental insufficiency, the biophysical test results and amniotic fluid volume assessment were normal. In our series, six of the isolated cases and six of the non-isolated cases presented with UA ARED flow in the third trimester.
Abnormal UA Doppler findings have been associated with disturbance in placental function of chromosomal abnormal fetuses and the higher rate of fetal growth restriction [7, 10, 24]. In contrast to fetuses with trisomy 18 or 13, fetuses affected by trisomy 21 are usually only mildly growth restricted. In our study, the rate of SGA was 13.5 % (38/281) overall and 15.8 % (6/38) beyond 30 weeks. We could demonstrate that in fetuses with trisomy 21 increased UA indices occurred irrespective of malformations or classical uteroplacental dysfunction. However, in most of the reported studies, isolated fetal malformations were not associated with abnormal UA Doppler indices [25] while others [26] described higher rates of malformations among appropriated for gestational age fetuses with abnormal UA Doppler findings compared to ones with normal Doppler.
The frequency of abnormal values above the 95th percentile increased significantly with gestational age in both groups in our study. The degree of placental developmental alteration seems to aggravate with advancing gestational age, resulting in an increasing percentage of trisomic fetuses exhibiting elevated UA Doppler indices. However, about one-third of cases with trisomy 21 presented with normal Doppler indices in the third trimester. This matches the results of previous small case series demonstrating normal Doppler waveforms in third-trimester fetuses with various trisomies. The authors proposed that in fetuses with trisomies there is a non-uniform affection of the different fetal organs, including the placenta [27].
Although the mean birth weight was lower in fetuses with abnormal compared to fetuses with normal UA flow pattern in our study, no statistical significance was reached and no correlation was found to placental histology. Especially, there was no difference in the number of vessels, intervillous thrombi or placental infarction. Others found a significant reduction in small musculary artery count and small musculary artery to villous ratio that correlated closely with abnormal UA Doppler in the third trimester, mainly in fetuses with trisomy 18 and 13 [10]. In third-trimester euploid SGA fetuses compared with euploid controls, abnormal Doppler velocimetry of the UA and uterine arteries was clearly linked to abnormal placental morphology, for example, intervillous thrombi and zones of placental infarction [28]. A reason for the non-significant findings between increased UA Doppler and placental histology in our study could be the evaluation mainly in the second trimester.
Conclusion
There is a significant increase in abnormal UA resistance in fetuses affected by trisomy 21 throughout gestation. This finding is present irrespective of malformations or small fetal growth. Although impaired placentation might be assumed as a key pathomechanism, no correlation to placental histology was found in our study. Trisomy 21 should be considered especially in the third trimester appropriate for gestational age fetus with abnormal UA velocimetry, but normal biophysical profile.
Abbreviations
- SGA:
-
Small for gestational age
- IUGR:
-
Intrauterine growth restriction
- PI:
-
Pulsatility index
- UA:
-
Umbilical artery
- ARED:
-
Absent or reverse end-diastolic flow
References
Loane M, Morris JK, Addor MC et al (2013) Twenty-year trends in the prevalence of Down syndrome and other trisomies in Europe: impact of maternal age and prenatal screening. Eur J Hum Genet 21:27–33
Sherman SL, Allen EG, Bean LH et al (2007) Epidemiology of Down syndrome. Ment Retard Dev Disabil Res Rev 13:221–227
Irving C, Basu A, Richmond S et al (2008) Twenty-year trends in prevalence and survival of Down syndrome. Eur J Hum Genet 16:1336–1340
Cocchi G, Gualdi S, Bower C et al (2010) International trends of Down syndrome 1993–2004: births in relation to maternal age and terminations of pregnancies. Birth Defects Res A Clin Mol Teratol 88:474–479
Clementi M, Calzolari E, Turolla L et al (1990) Neonatal growth patterns in a population of consecutively born Down syndrome children. Am J Med Genet Suppl 7:71–74
Weijerman ME, van Furth AM, Noordegraaf A et al (2008) Prevalence, neonatal characteristics, and first-year mortality of Down syndrome: a national study. J Pediatr 152:15–19
Malassiné A, Frendo JL, Evain-Brion D (2010) Trisomy 21-affected placentas highlight prerequisite factors for human trophoblast fusion and differentiation. Int J Dev Biol 54:475–482
Pidoux G, Gerbaud P, Cocquebert M et al (2012) Review: human trophoblast fusion and differentiation: lessons from trisomy 21 placenta. Placenta 33(Suppl):S81–S86
Qureshi F, Jacques SM, Johnson MP et al (1997) Trisomy 21 placentas: histopathological and immunohistochemical findings using proliferating cell nuclear antigen. Fetal Diagn Ther 12:210–215
Rochelson B, Kaplan C, Guzman E et al (1990) A quantitative analysis of placental vasculature in the third-trimester fetus with autosomal trisomy. Obstet Gynecol 75:59–63
Wenstrom KD, Weiner CP, Williamson RA (1991) Diverse maternal and fetal pathology associated with absent diastolic flow in the umbilical artery of high-risk fetuses. Obstet Gynecol 77:374–378
Trudinger BJ, Cook CM (1985) Umbilical and uterine artery flow velocity waveforms in pregnancy associated with major fetal abnormality. Br J Obstet Gynaecol 92:666–670
Rizzo G, Pietropolli A, Capponi A et al (1994) Chromosomal abnormalities in fetuses with absent end-diastolic velocity in umbilical artery: analysis of risk factors for an abnormal karyotype. Am J Obstet Gynecol 171:827–831
Jauniaux E, Gavrill P, Khun P et al (1996) Fetal heart rate and umbilico-placental Doppler flow velocity waveforms in early pregnancies with a chromosomal abnormality and/or an increased nuchal translucency thickness. Hum Reprod 11:435–439
Zoppi MA, Ibba RM, Putzolu M et al (2000) First trimester umbilical artery pulsatility index in fetuses presenting enlarged nuchal translucency. Prenat Diagn 20:701–704
Martinez Crespo JM, Comas C, Ojuel H et al (1996) Umbilical artery pulsatility index in early pregnancies with chromosome anomalies. Br J Obstet Gynaecol 103:330–334
Acharya G, Erkinaro T, Mäkikallio K et al (2004) Relationships among Doppler-derived umbilical artery absolute velocities, cardiac function, and placental volume blood flow and resistance in fetal sheep. Am J Physiol Heart Circ Physiol 286:1266–1272
Baschat AA, Gembruch U (2003) Development of fetal cardiac and extracardiac Doppler flows in early gestation. In: Yagel S, Silverman NH, Gembruch U (eds) Fetal cardiology. Martin Dunitz, London, pp 121–139
Borell A, Martinez JM, Farre MT et al (2001) Reversed end-diastolic flow in the first trimester umbilical artery: an ominous new sign for fetal outcome. Am J Obstet Gynecol 185:204–207
Brown R, Di Luzio L, Gomes C et al (1998) The umbilical artery pulsatility index in the first trimester: is there an association with increased nuchal translucency or chromosomal abnormality? Ultrasound Obstet Gynecol 12:244–247
Martinez JM, Borrell A, Antolin E et al (1997) Combining nuchal translucency with umbilical Doppler velocimetry for detecting fetal trisomies in the first trimester of pregnancy. Br J Obstet Gynaecol 104:11–14
Hecher K, Spernol R, Wimmer-Hebein D et al (1992) Doppler ultrasound of the umbilical artery in fetuses with sonographically abnormal findings and/or chromosome abnormalities. Geburtshilfe Frauenheilkd 52:275–282
Wong G, Levine D (2005) Fetuses with trisomy 21 having conflicting findings on antenatal testing for fetal well-being. J Ultrasound Med 24:1541–1545
Robinson WP, Peñaherrera MS, Jiang R et al (2010) Assessing the role of placental trisomy in preeclampsia and intrauterine growth restriction. Prenat Diagn 30:1–8
Meise C, Germer U, Gembruch U (2001) Arterial Doppler ultrasound in 115 second- and third-trimester fetuses with congenital heart disease. Ultrasound Obstet Gynecol 17:398–402
Gaziano EP, Knox GE, Wager GP et al (1990) Pulsed Doppler umbilical artery waveforms: significance of elevated umbilical artery systolic/diastolic ratios in the normally grown fetus. Obstet Gynecol 75:189–193
Berkowitz GS, Mehalek KE, Chitkara U et al (1988) Doppler umbilical velocimetry in the prediction of adverse outcome in pregnancies at risk for intrauterine growth retardation. Obstet Gynecol 71:742–746
Vedmedovska N, Rezeberga D, Teibe U et al (2011) Microscopic lesions of placenta and Doppler velocimetry related to fetal growth restriction. Arch Gynecol Obstet 284:1087–1093
Acknowledgments
There were no funding resources that supported this work.
Conflict of interest
All authors declare there is no conflict of interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Flöck, A., Remig, I., Müller, A. et al. Conflicting umbilical artery Doppler findings in fetuses with trisomy 21. Arch Gynecol Obstet 292, 613–617 (2015). https://doi.org/10.1007/s00404-015-3703-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-015-3703-4