Abstract
Background
Anogenital warts are a common human papillomavirus infection. They cause emotional distress, especially when they are in the anogenital region. Cryotherapy is a first-line treatment. Previous clinical trials and case series have reported variable results with retinoids (isotretinoin) as adjuvant therapy.
Objective
To determine the safety and efficacy of low-dose oral isotretinoin as adjuvant treatment of anogenital warts.
Methods
Forty-six patients with anogenital warts were randomly assigned to isotretinoin + cryotherapy (n = 23) or only cryotherapy (n = 23). Patients were allocated via an interactive web-based randomization system. Evaluators were blinded to treatments. Isotretinoin 20 mg/daily + cryotherapy or cryotherapy were prescribed for 6 weeks. Patients were followed for 4 months. Genotyping of lesions was performed before treatment started. Dermatology Life Quality Index (DLQI) and Columbia-Suicide Severity Rating Scale (C-SSRS) were measured at the beginning and end of therapy. All patients completed the study.
Results
Both Groups had 50% clearance at the end of treatment. Recurrence in the combined group was not significantly lower than in the cryotherapy group (P = 0.59). Improvement was observed in the DLQI of all patients in both groups (P = 0.001). No suicidal intention was detected with the C-SSRS. Two patients (one in each group) had liver function test abnormalities after treatment.
Conclusion
Combined therapy showed a slight not significant efficacy for anogenital warts in Hispanic patients. Low-dose isotretinoin seems to be safe even when it is used with cryotherapy on anogenital warts.
Trial registration
On April 25, 2019 with registration number DE19-00004, CONBIOÉTICA-19-CEI-001–20160404. Prospectively registered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Warts are caused by infection with human papillomavirus (HPV). They appear in different sites of the body and have a varied clinical expression. Anogenital warts (AGW), also known as condyloma acuminate or venereal warts, are mostly associated with HPV types 6 and 11 but sometimes with other oncogenic types [1, 2].
HPV infection requires the virus to reach the basal cell layer of the epithelium. Once there, it increases cell proliferation in the basal and supra basal cell layers, [3] with warts becoming visible 3–4 weeks after the initial infection [4]. Approximately, 40–60% of patients present complete spontaneous regression of warts in 2 years [5]. The cellular immune response plays a very important role in regression. [6] Patients with persistent lesions usually require treatment and sometimes these tend to be recalcitrant [7].
In the most recent European and American guidelines [8, 9], one of the first-line treatments for anogenital warts was cryotherapy. A recent review and meta-analysis comparing the efficacy and safety of cryotherapy versus other AGW treatments shows that cryotherapy efficacy does not differ from other local treatments except electrosurgery which was weakly associated with a better clearance of warts. Finally, the study concludes that cryotherapy is an acceptable first-line therapy to treat anogenital warts [10].
Retinoids affect epidermal growth and increase keratinocyte differentiation affecting HPV replication; [11] these changes collectively create a peeling effect. Also, retinoids are potent immunomodulators [12, 13] and some studies show that they can downregulate HPV transcription in infected cells. [14,15,16] Recently, studies revealed that vitamin A (retinol) deficiency is present in patients affected with recalcitrant cutaneous warts compared with healthy controls. [17] Treatment with retinoids appears to be a promising therapeutic or adjuvant choice.
There are some randomized controlled trials where oral isotretinoin was used as combination [18] and in monotherapy [19,20,21,22,23] to treat warts, also we found some case series (we only considered those with ≥ 10 patients and a minimum duration of 6 weeks of therapy) [24,25,26] and case reports [27,28,29,30,31,32,33,34,35] where oral retinoids other than isotretinoin alone or in combination with other treatment modalities have been used. Table 1 shows randomized controlled trials and case series where oral isotretinoin was used for treating anogenital warts. Recently, a systematic review and meta-analysis [36] demonstrated no superiority in clinical response and recurrence comparing high-dose isotretinoin (1 mg/kg/day) to a low-dose regimen (0.5 mg/kg/day).
The aim of this study is to determine whether isotretinoin used as an adjuvant to cryotherapy is safe and effective for AGW, compared to standard cryotherapy alone. Furthermore, we propose a severity scale and determine if the genotype is related to severity and clinical response.
Methods
Study design
This was a prospective randomized evaluator-blinded study performed in a single center between May 1, 2019 and January 14, 2020. This study was approved by the Ethics, Research and Biosecurity Committees of the School of Medicine and Dr. Jose Eleuterio Gonzalez University Hospital, Universidad Autonoma de Nuevo Leon with approval number DE19-00004. No changes to the methods were made after trial commencement.
Patients
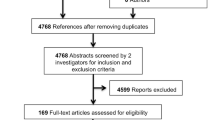
Patients with a diagnosis of AGW who attended the Dermatology Clinic of the Dr. José Eleuterio González University Hospital from May 1, 2019 to January 14, 2020 were invited to participate in this study. Patients who had received any local or systemic treatment in the month prior to enrolment were excluded. All those patients who had received prior therapies (all of them for 6 months or more) had multiple lesions, these were classified as AGW resistant to treatment. None of the patients had a history of immunodeficiency, autoimmune disease, or actual history of pregnancy or menstrual irregularities. During the study, it was recommended to use barrier protection or some other equally effective contraceptive method. We also encouraged to reduce or avoid alcohol consumption during the study. All the participants provided informed consent. Patients were also able to drop out at any time during the trial if they wished (Fig. 1).
Sample size calculation and randomization
A sample size of 23 patients in each arm of the study was estimated to provide an 80% power to detect a difference between groups in the proportion of complete clearance of warts assuming rates of 61.9% for patients receiving placebo and 90% for patients receiving isotretinoin and cryotherapy at an alfa of 0.1 using a two-sided \(\chi^{2}\) test. Patients were randomized in a 1:1 ratio to treatment with cryotherapy plus isotretinoin or only cryotherapy via an interactive web-based randomization system by an independent physician. Forty-six patients were randomly assigned to two groups. Group A (23 patients) received treatment with standard cryotherapy at 2-week intervals with a total number of three sessions plus oral very low dose of isotretinoin 20 mg/day (0.1–0.2 mg/kg/day) for 1.5 months. Patients of group 2 (23 patients) received only standard cryotherapy at 2-week intervals with a total number of three sessions.
Blinding
A blind evaluation was performed by two independent dermatologists. The parameters assessed were disease severity and therapeutic response.
Baseline assessments
At baseline and at the end of the treatment, both groups answered a Dermatological Quality of Life Index (DLQI) survey. The Columbia Suicide Gravity Classification Scale (CSSR-S) was applied to group A before and after isotretinoin treatment. Skin biopsies were performed using a 2-mm punch for histopathological study as well identification of HPV genotype using a Direct Flow CHIP system by Master Diagnostica® (based on direct PCR from crude-cell extracts, automatic flow-through hybridization, and colorimetric detection of 18 high-risk and 18 low-risk HPV genotypes). A urine pregnancy test was done in all reproductive age females and contraception during the treatment period and 1 month after stopping the treatment was advised. All patients were tested for HIV. In group A, liver and renal function tests, cholesterol and triglyceride levels were performed at baseline and at treatment end. The severity scale was performed before treatment by visual measure of the affected anogenital area as follows: Grade 1: < 10%; Grade 2: 11–30%; Grade 3: 31–50%; Grade 4: 51–70%; Grade 5: 71–90%; Grade 6: > 90%. Clinical photographs were taken before and after treatment to evaluate clinical response.
Intervention
Every patient received cryotherapy (Brymill Cry-AC Tracker). Two cryotherapy cycles were applied until reaching a – 40 ℃ temperature and maintained for 10 s using the C aperture (0.022 inches) with a lesion distance of 10 mm and a peri-lesional margin of 1 mm. This was carried out every two weeks until complete clearance of the lesions for a maximum of three sessions. (Fig. 2) The end point of each treatment session was mild erythema. In case of skin blisters, patients were allowed to drain the blister by puncturing at one end with a sterile needle.
Isotretinoin administration
Every 2 weeks, a 15 capsule blister of isotretinoin (Faclynel®, Italmex® Pharma) 20 mg was given to Group A to take one daily orally with meals. Three cryotherapy sessions along with 45 daily capsules (6.42 weeks) were administered. Both groups were evaluated at week 8 (2 weeks after the last cryotherapy session) to determine clinical response, photographic follow-up, and Dermatologic Life Quality Index (DLQI). The Columbia-Suicide Severity Rating Scale (C-SSRS) was performed at this time only for group A. Two blinded independent dermatologists reviewed the clinical photographs before and after therapy to determine the degree of clinical improvement and the presence of any complications. For patients with complete clearance, a second evaluation was performed to identify recurrences at week 24. Follow-up for both groups was during a 4-month period. For patients with regular or bad response, we offered to continue standard treatment (cryotherapy) in our clinic out of the trial.
Outcomes
Outcomes included severity assessment, clearance after 6 weeks of treatment, recurrence evaluation after 4 months of follow-up, adverse effects analysis, baseline and post-treatment changes in DLQI and C-SSRS, and wart genotypification.
Statistical methods
The baseline data (demographic, DLQI, CSSR-S, Severity), outcomes, and descriptive statistics of median, interquartile ranges and percentages were used for the variable analysis. The Mann–Whitney U and Kruskal–Wallis tests for abnormal distribution and the Chi-square for dichotomic and polytomous variables were applied in the two groups. Statistical analysis was performed with IBM SPSS version 25 (IBM, Inc., Armond, NY) Results were statistically significant if the P value was less than 0.05.
Results
Participants
After evaluation, 46 eligible patients were consecutively enrolled. The study was completed by 23 patients in each treatment group (Fig. 2). None of our subjects were lost to follow-up. All had perfect adherence to treatment. The key characteristics of the participants of each group at baseline are summarized in Table 2. The main previous treatments (at least 6 months prior to the start of the study) for patients in both groups were cryotherapy followed by electrosurgery and podophyllin, all types of therapy are listed in Table 2. These treatments did not have improvement for at least 6 months of therapy, for this reason, they were classified as resistant to treatment. There was no difference in the number of patients who had received prior therapy without a good response between both groups (Table 2).
Outcomes and estimation
Severity
A severity scale was designed and each patient was evaluated before treatment. Half of the subjects (23 patients) were evaluated as grade 1, while only 2.2% (1 patient) was evaluated as grade 6. Approximately 37% (17 patients) were graded as 2 and 3. The remaining 11% (five patients) were graded as 4 and 5. Group A had a higher severity vs group B as shown in Table 3 with this being close to a significant difference between the groups (p = 0.1). Cohen's κ was run to determine if there was agreement between the two experts on the degree of the initial evaluation of the lesions and the percentage of severity between them. There was moderate agreement between the two experts in the initial evaluation of the lesions, κ = 0.515 (95% CI 0.29–0.73), p < 0.0005. There was also moderate agreement in the. degree of severity, κ = 0.51 (95% CI 0.31–0.70), p < 0.0005.
DLQI and C-SSRS
The Dermatology Life Quality Index (DLQI) scores were recorded before and after treatment. These significantly improved in both groups at the end of the treatment period. Group A changed at the start from 8 points to 0 (p < 0.01) and Group B from 7 points to 0 p < 0.01). There was no significant difference between the groups. The Columbia-Suicide Severity Rating Scale (C-SSRS) demonstrated no suicide risk before or after treatment with isotretinoin.
Genotype
Genotypification results and correlations by groups are shown in Table 4. More than half of the genotypes found were low risk, with the most frequent genotype being 6. In Group A, the patients presented lesions with a greater number of genotypes when compared to Group B, however, there was no statistically significant difference between the two groups. Group A presented a greater number of patients with a high-risk genotype, also without a significant difference.
Side effects
The clinical and laboratory side effects presented during the study are shown in Table 5. None of the patients required discontinuation of treatment. In group A, 47.8% of the patients reported severe pain during application and 26.1% blister formation. In Group B, 30.4% reported severe pain and 13% blister formation. All patients in both groups presented post-inflammatory hyperpigmentation; in group B, ulceration was significantly superior.
In Group A, side effects related to isotretinoin such as dry skin (56.5%) and transaminase elevation (two patients) were observed. There were minimal changes in baseline transaminase when we compared baseline levels with those at the end of the study (one patient in each group elevated GGT mildly, less than twofold as is shown in Table 5).
Clearance
Clinical response in both groups is shown in Figs. 3 and 4, and Table 6. Both groups had 50% clearance at the end of treatment. Clearance was reached faster in Group A than in Group B when measured by weeks (53.4% vs 20%, p = 0.12).
Relapse
Seven of 15 (46.6%) patients who had complete clearance in Group A relapsed after 4 months (week 22) of follow-up, whereas 11 of 15 (73.33%) in Group B relapsed (Table 6).
Discussion
AGW are a common disease. They cause aesthetic disfigurement that leads to sexual and psychological distress in patients. Treatment can be challenging (especially in widespread infection due to autoinoculation) even in immunocompetent patients.
Although there are previous studies that have evaluated the effectiveness of isotretinoin in the treatment of AGW, to our knowledge, this is the first blind, randomized, cryotherapy-controlled group low-dose isotretinoin trial for the treatment of AGW with histopathological confirmation and genotype determination. Most patients were men with a median age of 25 years; other authors have reported similar data in 20–39-year olds. [37, 38] This could be directly related to the age where there is more sexual activity [19].
Lesion severity was slightly higher in Group A (p = 0.1). Also, in this group, the accumulated high-risk genotype virus was higher than Group B (61.9% vs 47.6%, p = 0.35). Disease duration was the same (median of 7 months). Al-Awadhi et al. [39] found no relation in number or size (severity) to high-risk genotypes, but their study shows that the risk of having a genital wart with a high-risk genotype is increased in warts that persist for more than 6 months. Thus, they did not find a relationship between high-risk genotypes and the size of lesions, but their chronicity.
There are only a few previous randomized clinical trials studies evaluating effectiveness of systemic retinoids in AGW. First in 1988, Olsen et al. [18] made a study where they compare high-dose isotretinoin (1 mg/kg/day for 6 weeks) plus interferon (IFN)-alpha (5 million units subcutaneously daily for 2 weeks, then three times per week for an additional 4 weeks) vs isotretinoin (1 mg/kg/day for 6 weeks) alone to treat AGW. The study showed complete clearance of 100% in the combination group vs 0% in the isotretinoin group. Accumulated change in % from baseline surface area of condyloma was 74.65% at 12 weeks of follow-up.
In a study by Cardamakis et al. [19], high-dose oral isotretinoin (1 mg/kg/day up to 3 months) was used vs IFN alfa-2a (3 × 105 IU subcutaneously three times weekly up to 8 weeks) plus oral isotretinoin (1 mg/kg/day up to 3 months) to treat condyloma acuminatum. In their study, complete clearance was 61.9% and 90.9%, respectively, with a global response of 76.4% with no recurrence in either groups (mean 10.14 months of follow-up).
Another paper by the same authors [20] compared high-dose oral isotretinoin (1 mg/kg/day up to 3 months) vs IFN alfa-2a (3 × 105 IU subcutaneously three times weekly up to 8 weeks) plus oral isotretinoin (1 mg/kg/day up to 3 months) to treat condyloma acuminatum. In their study, complete clearance was achieved in both groups with recurrence of 16.6% (1–6 months of follow-up) vs 15.5% (3–6 months of follow-up), respectively.
Finally, Georgala et al. [21] treated AGW with a low dose of isotretinoin (0.5 mg/kg/day up to 3 months) vs placebo. Complete clearance was reached in 32.1% of patients treated with isotretinoin compared with 0% in the placebo group. Recurrence was 11.1% in the isotretinoin group with 12 months of follow-up.
There are other case series (with complete clearance of 62%) [24] and case reports [28, 31,32,33, 40] that show that systemic isotretinoin has an effect on a variety of warts, particularly genital warts.
In our study, 65.2% of patients in Group A had complete remission, whereas 65.2% of patients in Group B had no difference in response. Most of the previous studies showed a superior response in combination therapy groups. [18, 19] Time to complete clearance was slightly shorter in the combination therapy group (p = 0.12).
Relapse in our patients was less common in patients in Group A with an accumulated relapse at week 22 (month 4) of 46.66% vs 73.33% of Group B. There is only one study [20] (studies comparing against placebo were not taken into account) where complete clearance was reached in both therapy groups and relapse rates were reported. There were no significant relapse rates between both groups with relapse rates from 16.6% when isotretinoin was used only and 15.5% in a combined therapy group of isotretinoin + interferon). These reported relapse rates were significantly less than in our study (46.6% in combination therapy vs 73.3% in cryotherapy only); however, their treatment time was longer (up to 3 months vs up to 6 weeks in our study). Therefore, if therapy is extended, this may reduce the chance of relapse. Further studies are needed to confirm this.
The mean DLQI in Group A and B were similar (moderate impairment) with a score of 8 and 7, respectively. Both groups showed significant improvement with statistical significance (p = 0.01) after treatment. In another study carried out in a Hispanic population that evaluated the quality of life in patients with AGW, most patients (81%) presented mild (2–5 points)-to-moderate (6–10 points) impairment. [38]
In a recent multicenter study [41] conducted in the United States and two Latin American countries, the prevalence of HPV type in men and its relationship with recurrences in treatment with surgical excision were evaluated; genotypification was performed in 86.6% of patients. Authors found that the prevalence of low- and high-risk genotypes was 43.87 and 56.12%, respectively, with a 65.5% of prevalence for more than 1 genotype in individuals. Regarding recurrence, a constant proportion was again observed during HPV type 6 and/or 11 events. Approximately, 63–69% were positive for ≥ 1 of the 9-valent HPV vaccine types.
In our study, the accumulated low-risk prevalence was 38.1% for Group A vs 52.4% in Group B and high-risk prevalence was 61.9% in Group A vs 47.6% in Group B with a statistical difference of p = 0.35. A higher prevalence of patients affected with more than two types of HPV was found in Group A (52.8%) than in Group B (19.2%).
Pooled data show a prevalence of low- and high-risk genotypes at 45.23 and 54.76%, respectively, and 59.52% of individuals presented more than 1 genotype, like most data reported in the literature.
The literature shows a slower clearance trend in AGW with high-risk genotypes; [37] however, in our study, the complete clearance time was slightly shorter in the combination therapy group despite a higher prevalence of high-risk genotypes. It can be thought that if the genotypes were homogeneously distributed, the difference in complete clearance and time to achieve complete clearance could be greater with more effective results in the combination therapy group.
Regarding adverse events, cryotherapy is associated with post-inflammatory macula, pain, and scar formation. The most common adverse effect associated with cryotherapy in our study was the formation of post-inflammatory hyperpigmentation (100% in both groups). Isotretinoin´s most common side effects are cheilitis, dryness of the skin and mucous membrane, and cholesterol, triglyceride and transaminase elevation. Although ingestion of isotretinoin (in acne patients) has been associated with a risk of suicide attempts, [42] recent studies did not find a causal link. [43, 44] Current recommendations are to screen for suicide risk before starting therapy. [45] No suicide risk was detected at the beginning or end of therapy in our study. Regarding the adverse effects associated with the intake of isotretinoin in Group A, cutaneous and mucosal dryness predominated (56.5%). Only one patient had a slight elevation of transaminases which returned to normal when treatment was discontinued at the end of the study period.
Limitations
The strengths of our study are the investigator-blinded assessment of severity and clinical outcomes, histopathological confirmation and genotyping. Some of the limitations were the small sample size and all patients were Hispanic (most of them males) from a single tertiary referral center. Also, this was a randomized study, but the study design did not permit blinding of the treating dermatologist. Since assessment was made through clinical and photographic observation, there was moderate agreement in the degree of severity. In four cases, a genotype study could not be performed since patients did not have more AGW at the time of reporting. Our treatment period was 6 weeks and the follow-up period was only 4 months. A longer treatment and follow-up periods are required to address the clearance and recurrence of genital warts.
Conclusion
Our study used low-dose oral isotretinoin as an adjunct to cryotherapy to treat AGW and compared it to cryotherapy alone. This combined therapy showed slight not significant efficacy for AGW in Hispanic patients when compared with only cryotherapy. The most notable benefit (also, not significant) in the combination therapy group was a reduction in the clearance time of the lesions. Low-dose isotretinoin seems to be safe even when it is used with cryotherapy on AGW. This combination is an interesting option to be considered for treating AGW. This still needs to be confirmed in a larger population, with longer treatment use and follow-up.
References
Aubin F, Prétet JL, Jacquard AC et al (2008) Human papillomavirus genotype distribution in external acuminata condylomata: a large French national study (EDiTH IV). Clin Infect Dis 47:610–615. https://doi.org/10.1086/590560
Ingles DJ, Pierce Campbell CM, Messina JA, Stoler MH, Lin HY, Fulp WJ et al (2014) Human papillomavirus virus (HPV) genotype- and age-specific analyses of external genital lesions among men in the HPV infection in men (HIM) Study. J Infec Dis. 211(7):1060–1067. https://doi.org/10.1093/infdis/jiu587
Doorbar J (2006) Molecular biology of human papillomavirus infection and cervical cancer. Clin Sci (Lond) 110(5):525–541. https://doi.org/10.1042/CS20050369
Christensen ND, Cladel NM, Reed CA, Han R (2000) Rabbit oral papillomavirus complete genome sequence and immunity following genital infection. Virology 269:451–461. https://doi.org/10.1006/viro.2000.0237
Messing AM, Epstein WL (1963) Natural history of warts: a two year study. Arch Dermatol 87:301–310. https://doi.org/10.1001/archderm.1963.01590150022004
Sterling JC, Gibbs S, Haque Hussain SS, Mohd Mustapa MF, Handfield-Jones SE (2014) British Association of Dermatologists’ guidelines for the management of cutaneous warts 2014. Br J Dermatol 171:696–712. https://doi.org/10.1111/bjd.13310
Stanley MA (2009) Immune responses to human papilloma viruses. Indian J Med Res 130:266–276
Lacey CJN, Woodhall SC, Wikstrom A et al (2013) 2012 European guideline for the management of anogenital warts. J Eur Acad Dermatol Venereol 27:e263–e270. https://doi.org/10.1111/j.1468-3083.2012.04493.x
Centers for Disease Control. STD treatment guidelines. Available at: http://www.cdc.gov/std/tg2015/. Published 2015. Accessed on June, 22 2020.
Bertolotti A, Dupin N, Bouscarat F, Milpied B, Derancourt C (2017) Cryotherapy to treat anogenital warts in nonimmunocompromised adults: Systematic review and meta-analysis. J Am Acad Dermatol 77(3):518–526. https://doi.org/10.1016/j.jaad.2017.04.012
Stellmach V, Leask A, Fuchs E (1991) Retinoid-mediated transcriptional regulation of keratin genes in human epidermal and squamous cell carcinoma cells. Proc Natl Acad Sci USA 88:45–82
Mucida D, Park Y, Kim G et al (2007) Reciprocal TH17 and regulatory T cell differentiation mediated by retinoic acid. Science 317:256–260. https://doi.org/10.1126/science.1145697
Jason J, Archibald LK, Nwanyanwu OC (2002) Vitamin A levels and immunity in humans. Clin Diagn Lab Immunol 9:616–621. https://doi.org/10.1128/cdli.9.3.616-621.2002
Bartsch D, Boye B, Baust C et al (1992) Retinoic acid-mediated repression of human papillomavirus 18 transcription and different ligand regulation of the retinoic acid receptor beta gene in non-tumorigenic and tumorigenic HeLa hybrid cells. EMBO J 11:2283–2291
Faluhelyi Z, Rodler I, Csejtey A et al (2004) All-trans retinoic acid (ATRA) suppresses transcription of human papillomavirus type 16 (HPV16) in a dose-dependent manner. Anticancer Res 24:807–809
Reppucci A, DiLorenzo T, Abramson A et al (1991) In vitro modulation of human laringuela papillota cell differentiation by retinoic acid. Otolaryngol Head Neck Surg 105:528–532. https://doi.org/10.1177/019459989110500404
El-Esawy F, Mustafa AI, El-Shimi O (2019) Serum retinol-binding protein: a novel biomarker for recalcitrant cutaneous warts. Int J Dermatol 58(12):1435–1438. https://doi.org/10.1111/ijd.14475
Olsen EA, Kelly FF, Vollmer RT, Buddin DA, Weck PK (1989) Comparative study of systemic interferon alfa-nl and isotretinoin in the treatment of resistant condylomata acuminata. J Am Acad Dermatol 20(6):1023–1030. https://doi.org/10.1016/s0190-9622(89)70127-4
Cardamakis E, Kotoulas IG, Relakis K, Metalinos K, Michopoulos J, Stathopoulos E et al (1995) Comparative study of systemic interferon alfa-2a plus isotretinoin versus isotretinoin in the treatment of recurrent condyloma acuminatum in men. Urology 45:857–860. https://doi.org/10.1016/S0090-4295(99)80094-6
Cardamakis EK, Kotoulas IG, Dimopoulos DP, Stathopoulos EN, Michopoulos JT, Tzingounis VA (1996) Comparative study of systemic interferon alfa-2a with oral isotretinoin and oral isotretinoin alone in the treatment of recurrent condylomata accuminata. Arch Gynecol Obstet 258:35–41. https://doi.org/10.1007/BF01370930
Georgala S, Katoulis AC, Georgala C, Bozi E, Mortakis A (2004) Oral isotretinoin in the treatment of recalcitrant condylomata acuminata of the cervix: a randomised placebo controlled trial. Sex Transm Infect 80:216–218. https://doi.org/10.1136/sti.2003.006841
Olguín-García MG, Jurado-Santa Cruz F, Peralta-Pedrero ML, Morales-Sánchez MA (2015) A double-blind, randomized, placebo-controlled trial of oral isotretinoin in the treatment of recalcitrant facial flat warts. J Dermatolog Treat 26:78–82
Kaur GJ, Brar BK, Kumar S, Brar SK, Singh B (2017) Evaluation of the efficacy and safety of oral isotretinoin versus topical isotretinoin in the treatment of plane warts: a randomized open trial. Int J Dermatol 56(12):1352–1358. https://doi.org/10.1111/ijd.13727
Tsambaos D, Georgiou S, Monastirli A, Sakkis T, Sagriotis A, Goerz G (1997) Treatment of condylomata acuminata with oral isotretinoin. J Urol 158:1810–1812. https://doi.org/10.1016/s0022-5347(01)64136-3
Olguín-García MG, Cancela RG, Peralta-Pedrero ML (2010) Estudio preexperimental para el tratamiento de verrugas planas faciales con isotretinoı’na oral. Dermatol Rev Mex 54:267–272
Al-Hamamy HR, Salman HA, Abdulsattar NA (2012) Treatment of plane warts with a low-dose oral isotretinoin. ISRN Dermatol 2012:163929. https://doi.org/10.5402/2012/163929
Katz RA (1986) Isotretinoin treatment of recalcitrant warts in an immunosuppressed man. Arch Dermatol 122(1):19–20. https://doi.org/10.1001/archderm.1986.01660130021014
Yildirim M, Inaloz HS, Baysal V, Kesici D, Candir O (2004) A case of condyloma acuminatum treated successfully with low-dose isotretinoin and interferon. Int J Clin Pract 58(9):889–891. https://doi.org/10.1111/j.1742-1241.2004.00071.x
Monastirli A, Matsouka P, Pasmatzi E, Melachrinou M, Georgiou S, Solomou E et al (2005) Complete remission of recalcitrant viral warts under oral isotretinoin in a patient with low-grade b-cell lymphoma. Acta Derm Venereol 1(1):1–1. https://doi.org/10.1080/00015550510027090
Miljkovic J (2012) A novel therapeutic approach to plane warts: a report on two cases. Acta Dermatovenerol Alp Pannonica Adriat 21:63–64
Pasmatzi E, Kapranos N, Monastirli A, Melachrinou M, Georgiou S, Tsambaos D (2012) Large benign condyloma acuminatum: successful treatment with isotretinoin and interferon alpha. Acta Derm Venereol 92(3):249–250. https://doi.org/10.2340/00015555-1257
Yew YW, Pan JY (2013) Complete remission of recalcitrant genital warts with a combination approach of surgical debulking and oral isotretinoin in a patient with systemic lupus erythematosus. Dermatol Ther 27(2):79–82. https://doi.org/10.1111/dth.12059
Jha AK, Sonthalia S, Ganguly S (2018) Oral isotretinoin as an adjunctive treatment for recurrent genital warts. J Am Acad Dermatol 78(2):e35–e36. https://doi.org/10.1016/j.jaad.2017.08.057
Białecka A, Męcińska-Jundziłł K, Adamska U, Cichewicz A, Białecki M, Drewa G, Czajkowski R (2018) Plane warts on the back of the hand successfully treated with oral isotretinoin. Postepy Dermatol Alergol 35(2):227–229. https://doi.org/10.5114/pdia.2017.70259
Herold M, Nielson C, Longo MI (2018) Isotretinoin and Candida immunotherapy for recalcitrant warts in solid organ transplant recipients. Derm Ther. https://doi.org/10.1111/dth.12803
Yang TH, Lee TH, Huang YC (2019) Oral isotretinoin for treating mucocutaneous human papillomavirus infections: a systematic review and meta-analysis. Indian J Dermatol Venereol Leprol 85:569–577. https://doi.org/10.4103/ijdvl.IJDVL_269_18
Moreira ED Jr, Giuliano AR, Palefsky J, Flores CA, Goldstone S, Ferris D et al (2014) Incidence, clearance, and disease progression of genital human papillomavirus infection in heterosexual men. J Infect Dis 210:192–199. https://doi.org/10.1093/infdis/jiu077
Camargo CC, D’Elia MPB, Miot HA (2017) Quality of life in men affected by anogenital warts. An Bras Dermatol 92(3):427–429. https://doi.org/10.1590/abd1806-4841.20175282
Al-Awadhi R, Al-Mutairi N, Albatineh AN, Chehadeh W (2019) Association of HPV genotypes with external anogenital warts: a cross sectional study. BMC Infect Dis 19(1):375. https://doi.org/10.1186/s12879-019-4005-4
Dave DD, Abdelmaksoud A (2019) Low dose Isotretinoin as an adjuvant therapy for treatment of different clinical variants of warts: a case series. Dermatol Ther. https://doi.org/10.1111/dth.12836
Giuliano AR, Sirak B, Abrahamsen M, Silva RJC, Baggio ML, Galan L et al (2019) Genital wart recurrence among men residing in Brazil, Mexico, and the United States. J Infect Dis 219(5):703–710. https://doi.org/10.1093/infdis/jiy533
Sundström A, Alfredsson L, Sjölin-Forsberg G, Gerdén B, Bergman U, Jokinen J (2010) Association of suicide attempts with acne and treatment with isotretinoin: retrospective Swedish cohort study. BMJ 341:c5812. https://doi.org/10.1136/bmj.c5812
Huang YC, Cheng YC (2017) Isotretinoin treatment for acne and risk of depression: a systematic review and meta-analysis. J Am Acad Dermatol 76(6):1068–76.e9. https://doi.org/10.1016/j.jaad.2016.12.028
Singer S, Tkachenko E, Sharma P, Barbieri JS, Mostaghimi A (2019) Psychiatric adverse events in patients taking isotretinoin as reported in a food and drug administration database from 1997 to 2017. JAMA Dermatol 155(10):1162–1166. https://doi.org/10.1001/jamadermatol.2019.1416
Droitcourt C, Poizeau F, Kerbrat S et al (2019) Isotretinoin and risk factors for suicide attempt: a population-based comprehensive case series and nested case-control study using 2010–2014 French Health Insurance Data. J Eur Acad Dermatol Venereol. https://doi.org/10.1111/jdv.16005 (published online ahead of print, 2019 Oct 6)
Acknowledgements
We thank all the patients who participated in this study. Thanks to Dr Sergio Lozano, for his support in the English language writing.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
ILRR obtained compiled, analyzed all data, and prepared initial draft. ILRR, SCA, VGR and AVM analyzed and interpreted data, drafted, and critically evaluated the manuscript for important intellectual content. ILRR, SCA, VGR, AVM, GGM, RFM and JOC helped in obtaining, compiling and interpretation of data, and literature search. ILRR evaluated clinical response and SCA, VGR and AVM assessed pre- and post-treatment photographs. All authors were involved in the drafting and revision of the manuscript and have agreed to the final content.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no competing interest and therefore nothing else to declare, and have contributed significantly and take full responsibility for the manuscript. The authors of the paper are obliged to confirm that it has not been previously published.
Ethical approval
This study was registered and approved (registration number: DE19-00004) by the Institutional Review Board Ethical Committee of the Dr. Jose Eleuterio González University Hospital of the Universidad Autónoma de Nuevo León, Mexico (CONBIOÉTICA-19-CEI-001-20160404).
Informed consent
Informed consent was obtained from study subjects for enrollment and publication of material with the understanding that their names and initials will not be published and due efforts will be made to conceal their identity but anonymity cannot be guaranteed. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki declaration of 1975 as revised in 1983.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Reyna-Rodríguez, I.L., Chavez-Alvarez, S., Garza-Rodríguez, V. et al. Cryotherapy plus low-dose oral isotretinoin vs cryotherapy only for the treatment of anogenital warts: a randomized clinical trial. Arch Dermatol Res 313, 815–827 (2021). https://doi.org/10.1007/s00403-020-02182-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-020-02182-y