Abstract
Background
The influence of obesity on patient-reported outcome measures (PROMs) following total hip arthroplasty (THA) is currently controversial. This study aimed to compare PROM scores for pain, functional status, and global physical/mental health based on body mass index (BMI) classification.
Methods
Primary, elective THA procedures at a single institution between 2018 and 2021 were retrospectively reviewed, and patients were stratified into four groups based on BMI: normal weight (18.5–24.99 kg/m2), overweight (25–29.99 kg/m2), obese (30–39.99 kg/m2), and morbidly obese (> 40 kg/m2). Patient-Reported Outcome Measurement Information System (PROMIS) and Hip Disability and Osteoarthritis Outcome Score for Joint Replacement (HOOS, JR) scores were collected. Preoperative, postoperative, and pre/post- changes (pre/post-Δ) in scores were compared between groups. Multiple linear regression was used to assess for confounders.
Results
We analyzed 3,404 patients undergoing 3,903 THAs, including 919 (23.5%) normal weight, 1,374 (35.2%) overweight, 1,356 (35.2%) obese, and 254 (6.5%) morbidly obese cases. HOOS, JR scores were worse preoperatively and postoperatively for higher BMI classes, however HOOS, JR pre/post-Δ was comparable between groups. All PROMIS measures were worse preoperatively and postoperatively in higher BMI classes, though pre/post-Δ were comparable for all groups. Clinically significant improvements for all BMI classes were observed in all PROM metrics except PROMIS mental health. Regression analysis demonstrated that obesity, but not morbid obesity, was independently associated with greater improvement in HOOS, JR.
Conclusions
Obese patients undergoing THA achieve lower absolute scores for pain, function, and self-perceived health, despite achieving comparable relative improvements in pain and function with surgery. Denying THA based on BMI restricts patients from clinically beneficial improvements comparable to those of non-obese patients, though morbidly obese patients may benefit from additional weight loss to achieve maximal functional improvement.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Obesity is a rapidly growing health risk throughout the United States and worldwide [1, 2] and represents a well-established risk factor for the development of symptomatic hip osteoarthritis requiring total hip arthroplasty (THA) [3, 4]. However, obesity increases the risk of postoperative complications including infection, readmission, and revision after THA [5,6,7]. Currently, no consensus exists regarding to what extent arthroplasty surgeons should facilitate preoperative weight loss for obese THA patients, nor is there consensus regarding how body mass index (BMI) should influence patients’ candidacy for THA [8].
Prior research has suggested that BMI cutoff values for THA may reduce the incidence of postoperative complications. By implementing such cutoffs, surgeons may restrict obese patients from experiencing clinically significant improvements in pain and functionality who would otherwise have an uncomplicated postoperative course [9, 10]. Therefore, understanding any differences in quality-of-life improvement based on obesity is critical to formulating a preoperative risk–benefit analysis. Patient-reported outcome measures (PROMs) are commonly used metrics to evaluate patients’ subjective appraisal of surgical success, however prior analyses of PROM scores during THA have yielded heterogeneous results [6, 11,12,13,14,15]. Prior studies have been limited by small sample sizes and poor follow-up, and comparisons between these studies are limited by variations in BMI classification methods, variations in PROM surveys used, and differences in baseline characteristics and comorbidities associated with study groups.
This study aimed to evaluate changes in PROM scores following THA based on patients’ obesity classification across a broad array of PROM metrics for pain, functional status, and global physical and mental health. This study also aimed to assess how diagnoses comorbid with obesity affect PROM scores during THA. We hypothesized that PROM scores assessing pain, function, and overall health would be worse for obese patients preoperatively and postoperatively, and that obese patients would experience relatively less improvement in PROM metrics following surgery when compared to non-obese patients.
Methods
Study design
Consecutive patients undergoing primary, elective THA between 2018 and 2021 at a single academic center were retrospectively reviewed. Patients undergoing bilateral procedures, hemiarthroplasty, revision arthroplasty, or non-elective THA were excluded. PROMs including the hip injury and osteoarthritis, joint replacement (HOOS, JR) score and Patient-Reported Outcome Measurement Information System (PROMIS) measures of pain interference, pain intensity, mobility, physical function, global physical health, and global mental health were captured at patients’ preoperative office visit and at subsequent postoperative office visits [16, 17]. All patient interviews and PROM collections were performed in English.
Demographics and patient stratification
Baseline patient demographics (sex, age, smoking status, BMI, and self-identified race) and comorbidities were collected from the electronic medical record. Patients were stratified into four BMI groups based on the World Health Organization guidelines for obesity classification (Normal Weight: 18.5–24.99 kg/m2, Overweight: 25–29.99 kg/m2, Obese: 30–39.99 kg/m2, Morbidly Obese: > 40 kg/m2) [18]. Only 43 underweight patients with a BMI < 18.5 kg/m2 underwent surgery during the study period, and thus were excluded. Based on a power analysis using the minimally clinically important difference (MCID) (18.0) and standard deviation (18.0) of HOOS, JR [19], we calculated that a minimum of 55 patients would be needed in this group to detect statistically significant differences at an alpha of 0.05 and 80% power. Baseline demographics were compared between BMI groups.
Patient-reported outcome measures
Patients with both preoperative and postoperative PROM scores for at least one outcome during the study period were included in the analysis. To calculate pre-/post-THA changes in PROM scores, we subtracted the most recent postoperative score from the most recent preoperative score during the study period. Mean scores for preoperative, postoperative, and pre-/post-∆ PROMs were compared between BMI groups.
Data analysis
Continuous variables were compared using chi-squared tests. For PROM scores, independent samples t-tests were used to compare the normal weight group to each of the other groups individually, and analysis of variance (ANOVA) was used to compare scores across all four groups. Pairwise t-tests were used to compare preoperative to postoperative PROM score changes within groups before and after surgery. Robust multiple linear regression analyses were conducted to adjust for possible confounders associated with obesity status. The prevalence of comorbid diagnoses was compared between BMI groups using Fisher’s exact tests. Those comorbidities which varied significantly across BMI groups were included as independent variables in regression models along with patient baseline characteristics. Categorical variables are presented as counts (percentages). Date ranges are represented as a median (interquartile range, IQR). PROM scores are presented as mean ± standard deviation. Regression analyses are presented as estimate effect (95% confidence interval, CI). Significance was set at p < 0.05 Statistical analyses were performed using the software R (Version 4.0.2, The R Foundation, 2022) together with RStudio (Version 1.3.959, RStudio Team, 2022).
Power calculations
Power analyses were conducted a-priori using the MCID and standard deviations for HOOS, JR (18.0, 5.3) [19] and PROMIS Global Physical Health (8, 10) [20], as these were the PROMs utilized within our multivariate regressions. The type 1 error rate (alpha) and power (1-beta) were kept fixed at 5% and 80% for all power calculations, respectively. Upon performing power analyses, we found that a minimum sample size of 55 patients would be required in each BMI classification group in order to detect statistically significant differences in HOOS, JR, and 72 patients for the PROMIS Global Physical Health score.
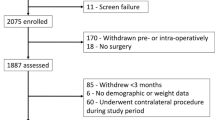
Study population and demographics
In total, 11,276 hip arthroplasties were performed during the study period. Of the included 3,404 patients undergoing 3,903 THAs, 919 (23.5%) were normal weight, 1,374 (%) were overweight, 1,356 (35.2%) were obese, and 254 (6.5%) were morbidly obese (Table 1). Average postoperative follow-up time was 11.2 ± 11.5 months (range 0.2 to 50), and 32.6% of patients had postoperative PROM scores reported from only their initial follow-up visit. The mean BMIs for the normal weight, overweight, obese, and morbidly obese cohorts were 22.6 ± 1.7, 27.4 ± 1.3, 33.7 ± 2.6, and 41.9 ± 5.3 kg/m2, respectively. Patients across all cohorts were predominantly female with the highest preponderance in the normal weight and morbidly obese cohorts (p < 0.0001). The morbidly obese and obese cohorts were younger at the time of surgery than other cohorts (p < 0.0001). The obesity classes showed a higher proportion of non-white patients (p < 0.0001). Of the comorbidities evaluated, congestive heart failure (p = 0.023), dementia (p = 0.016), chronic pulmonary disease (p = 0.001), diabetes without chronic complications (p < 0.001), diabetes with chronic complications (p = 0.007), leukemia or lymphoma (p = 0.031), and HIV/AIDs (p = 0.037) demonstrated significant differences among BMI cohorts, and thus were included as independent variables in regression models. A full analysis of comorbidities can be found in Table 2.
Results
Patient-reported outcome measures
Patients in higher BMI cohorts displayed significantly lower preoperative HOOS, JR scores: 53.7 ± 15.4, 50.9 ± 15.3, 48.3 ± 15.1, and 49.1 ± 17.3 for the normal weight, overweight, obese, and morbidly obese cohorts, respectively (p < 0.0001). Similarly, postoperative HOOS, JR scores were lower for obese (p < 0.0001) and morbidly obese patients (p = 0.001) (Table 3). Within-group analyses of HOOS, JR scores before and after surgery revealed significant score improvements in all BMI groups (normal weight p < 0.0001, overweight p < 0.0001, obese p < 0.0001, and morbidly obese p < 0.0001). No between-group difference was observed for pre-/post-∆ HOOS, JR score among BMI cohorts (p = 0.822).
Across all preoperative PROMIS measures, obese and especially morbidly obese patients reported worse scores in pain intensity (p < 0.0001), pain interference (p < 0.0001), physical function (p < 0.001), mobility (p < 0.0001), global mental health (p < 0.0001), and global physical health (p < 0.0001) (Table 4). Similarly, obese and morbidly obese patients reported worse postoperative PROMIS outcomes for pain intensity (p < 0.0001), pain interference (p < 0.0001), physical function (p = 0.001), mobility (p < 0.0001), global mental health (p < 0.0001), and global physical health (p < 0.0001). No between-group differences were observed for pre-/post-∆ in PROMIS measures of pain intensity (p = 0.626), pain interference (p = 0.799), physical function (p = 0.412), mobility (p = 0.210), global mental health (p = 0.391), and global physical health (p = 0.845) (Table 4). Within-group comparisons revealed significant preoperative to postoperative improvements in PROMIS global physical health scores in all BMI cohorts (normal weight p < 0.0001, overweight p < 0.0001, obese p < 0.0001, morbidly obese p < 0.0001).
Multiple linear regression analysis
Regression analysis showed that morbid obesity was associated with lower postoperative HOOS, JR scores after adjusting for other variables (−3.74, 95% CI −6.69 to −0.79, p = 0.013). Both the overweight (2.91, 95% CI 0.34 to 5.48, p = 0.27) and the obese BMI cohorts (3.52, 95% CI 0.88 to 6.17, p < 0.01) were associated with higher pre-/post-∆ in HOOS, JR scores (Table 5). African American race was associated with lower postoperative HOOS, JR scores (3.66, 95% CI −5.72 to −1.60, p < 0.001), as was identifying as other non-white race (4.62, 95% CI −6.86 to −2.39, p < 0.0001). Analysis of comorbidities demonstrated strong negative associations between patients with HIV/AIDs (−7.73, 95% CI −12.68 to −2.77, p < 0.01) or diabetes with chronic complications (−7.51, 95% CI −13.46 to −1.55, p = 0.014) and postoperative HOOS, JR scores. None of the comorbidities analyzed were associated with significantly decreased pre-/post-∆ improvement in HOOS, JR. Full regression results for HOOS, JR scores are presented in Table 5.
Regression analysis for PROMIS global physical health scores showed elevated BMI was associated with worse postoperative PROMIS global physical health scores (overweight −1.30, 95% CI −2.07 to −0.52, p < 0.01; obese −2.88, 95% CI −3.65 to −2.10, p < 0.0001; morbidly obese −4.71, 95% CI −5.90 to −3.51, p < 0.0001). No association was observed between BMI and pre-/post-∆ in PROMIS global physical health scores (overweight p = 0.49, obese p = 0.94, and morbidly obese p = 0.24). African American race was associated with lower postoperative PROMIS global physical health scores (−1.66, 95% CI −2.50 to −0.82, p < 0.001), as was identifying as other non-white race (−1.72, 95% CI −2.65 to −0.80, p < 0.001). Infection with HIV and diabetes with chronic complications demonstrated similarly negative relationships with postoperative PROMIS global physical health scores (HIV/AIDs: −4.55, 95% CI −6.68 to −2.42, p < 0.0001; diabetes with chronic complications: −2.81, 95% CI −5.29 to −0.33, p = 0.024). None of the comorbidities analyzed were associated with significantly decreased pre-/post-∆ improvement in PROMIS global health. Full regression results for PROMIS global physical health are presented in Table 6.
Outcomes and complications
The morbidly obese group demonstrated the greatest mean surgical time (132.4 min), followed by the obese (108.3), overweight (99.8) and normal weight groups (94.4) (p < 0.001 for all comparisons). Similarly, the morbidly obese group had a significantly longer mean LOS (52.1 h) compared to the obese (41.6), overweight (38.5) and normal weight (40.4) groups (p < 0.001for all comparisons). Discharge disposition rates were comparable between groups (p = 0.738). The morbidly obese group demonstrated significantly higher rates of 90-day readmissions (8.3) when compared to the obese (4.1), overweight (2.8) and normal weight (3.0%) groups (p < 0.001, for all comparisons). All-cause revision rates and mean days to revision were comparable between groups (p = 0.232, p = 0.133, respectively). A full account of perioperative and clinical outcomes can be found in Tables 7 and 8.
Discussion
This study analyzed the association between BMI classification and PROM scores following THA and reports several important findings: (1) obese and morbidly obese patients consistently report worse preoperative and postoperative scores for pain, functional status, and health; (2) improvements in PROMIS measures of pain, function, mobility, global mental health, and global physical health were comparable across BMI cohorts; (3) obesity is independently associated with a greater pre-/post-∆ improvement in HOOS, JR scores, but not global health scores; (4) HIV/AIDS, chronic diabetes, and being of non-white race are independently associated with lower HOOS,JR and PROMIS global physical health scores postoperatively.
Present literature regarding the influence of BMI on PROMs following THA has shown mixed results [6, 11,12,13, 15, 21]. Jameson et al. analyzed 2,656 THA patients stratified by BMI finding that obese and morbidly obese patients experienced a smaller, though still significant postoperative increase in hip pain and function and health-related quality of life (HRQoL) compared to non-obese patients [6]. Similarly, Mukka et al. demonstrated a smaller postoperative increase in HRQoL in overweight and obese patients. In contrast, Li et al. reported on a cohort of 2,040 THA patients which showed that while more obese patients experienced lower function and physical health scores postoperatively, they showed a greater pre-/postoperative decrease in pain scores leading to no difference in postoperative pain among BMI classes [11]. Moreover, Peters et al. investigated data from the Dutch Arthroplasty Register observing that obesity was associated with a greater pre-/postoperative increase in hip-specific and HRQoL measures [13].
Bilateral and non-elective THA patients were excluded from our study as they represent possible sources of heterogeneity. Studies have demonstrated a tendency for higher preoperative pain scores in bilateral THA patients as compared to unilateral THA [22]. Additionally, differential improvements in physical function and mental health scores have been shown for bilateral and unilateral THAs [23], while substantial differences in clinical outcomes between elective and non-elective THAs have been reported [24].
We found that obese and morbidly obese patients consistently scored worse both preoperatively and postoperatively on the HOOS, JR and across PROMIS measures. However, there were no differences in pre-/post-∆ among any BMI cohorts for any measure, suggesting that patients achieve a similar relative degree of clinical improvement regardless of obesity. For all BMI classes, average improvements in HOOS, JR scores and all PROMIS scores–except for global mental health–reached the established minimal clinically important difference (MCID) [25, 26]. This suggests that on average patients obtained a similar and clinically meaningful difference following THA, though obese patients consistently report relatively worse pain, functional status, and overall health.
After adjusting for comorbid conditions, regression analysis demonstrated an independent negative effect of obesity on PROMIS global physical health scores. This effect was largest in the morbidly obese cohort, though no differences were observed among BMI cohorts in the pre-/post-∆ in PROMIS global physical health measures. Interestingly, we observed an independent negative effect of morbid–though not moderate–obesity, on postoperative HOOS, JR scores. It is possible that additional functional limitations and health challenges associated with morbid obesity limit the degree of improvement that these patients can achieve. This is important in counseling patients preoperatively about their weight. Rather than restricting access to care to all obese patients, providing resources and education for morbidly obese patients to achieve weight loss with the goal of achieving a BMI at least < 40 kg/m2 may have positive functional implications.
African American or other non-white race were also independently linked to lower postoperative HOOS, JR and PROMIS global physical health scores. Current literature has shown associations between non-white race and inferior preoperative, postoperative, and pre-/post-∆ in PROMs [27,28,29]. Identifying as African American or other race was associated with moderately decreased postoperative HOOS, JR and PROMIS global physical health scores without a concomitant decrease in pre-/post-∆ in either measure. These results suggest that while racial disparities persist in patients undergoing THA, they likely do not diminish the benefit these patients derive from surgery. These trends highlight the importance of understanding cultural perceptions of weight and tailoring the surgical discussion toward acceptable ways to optimize weight prior to arthroplasty.
Regression analysis showed a strong negative relationship between diagnoses of advanced diabetes and HIV/AIDs and PROMs. Literature regarding the effect of comorbidities on PROMs has yielded heterogeneous results [5, 26]. Leiss et al. reported that diabetes was linked to lower pre- and postoperative functional and pain scores in a cohort of 109 patients [27]. Our results show similarly decreased postoperative scores for HOOS, JR and PROMIS global physical health, however patients with diabetes experienced similar, if not increased pre-/post-∆ in their PROMs, suggesting they still derive therapeutic benefit from the procedure. Limited research has examined PROMs outcomes in HIV positive patients; Graham et al. described improvements in patient-reported functional and pain scores for 102 THAs, though they did not compare to HIV negative patients [28, 29]. Regression results show that while HIV positive patients have lower postoperative PROMs, they demonstrate no difference in pre-/post-∆ in PROMs, suggesting they still derive clinical benefit from THA. None of the comorbidities analyzed were associated with an inferior degree of improvement in HOOS, JR or PROMIS global physical health measures.
The lack of agreement in literature concerning the association between BMI and PROMs following THA may be explained by multiple factors including variations in the criteria used to classify obesity, specific PROM measures employed by researchers, and insufficient data on patient comorbidities [15]. In addition, reduced follow-up and lack of survey response further exacerbate the limited sample sizes across various BMI classes needed to achieve adequate power for analyses of PROMs [30]. Our study included a large sample size of patients who completed PROMs across categories of function, pain, and general health generated by institutional initiatives to gather PROM data for all patients undergoing THA. We also conducted a robust regression analysis that adjusted for baseline demographic factors and patient comorbidities related to BMI. Despite the relation of diabetes and HIV/AIDs diagnoses with lower postoperative HOOS, JR or PROMIS global physical health scores, no comorbidities were linked to worse pre-/post-∆ in PROMs.
Limitations
Inherent to the study’s retrospective design are risks of selection bias resulting from lack of PROM survey adherence and lost follow-up. While patients completed all PROM measures during the period of study, we could not obtain PROM measures from patients on a standardized schedule, and 32.6% of patients had postoperative PROM scores captured only once. This variability in the follow-up timeline may not have allowed us capture complete improvement data for all subjects. Furthermore, PROMs are a subjective outcome that measure patients experience and self-perceived outcome, but do not assess objective outcomes such as readmission and revision rates. PROM questionnaires are also subject to recall bias, and the inclusion of several different PROMs may have introduced a source of heterogeneity within our study, while possibly increasing our generalizability. In addition, inherent baseline differences across BMI groups existed and may have influenced results, though we attempted to account for this by conducting regression analyses. Finally, though we captured comorbidity data for all patients, the low absolute prevalence of specific comorbidities limits our power to adequately adjust for their confounding effects during analysis.
Conclusion
Obese and morbidly obese patients undergoing THA demonstrate worse preoperative and postoperative outcomes for measures of pain, functional status, and overall health, though they attain similar therapeutic benefit across PROMIS measures. Moderate, but not severe, obesity is independently associated with more substantial improvement in HOOS, JR scores following THA. While lower postoperative PROMs are associated with advanced diabetes, HIV/AIDs and non-white race, these factors do not affect the therapeutic benefit of THA. Patient-reported improvements following THA are consistent and clinically significant across BMI groups, however there may be a role for weight loss in morbidly obese THA patients to attain maximum functional status based on HOOS, JR scores.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available as they contain protected health information from within our institution, but de-identified data can be made available from the corresponding author on reasonable request.
References
Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL (2016) Trends in obesity among adults in the United States, 2005 to 2014. JAMA 315:2284–2291. https://doi.org/10.1001/JAMA.2016.6458
Bentham J, Di Cesare M, Bilano V, Bixby H, Zhou B, Stevens GA et al (2017) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 390:2627–2642. https://doi.org/10.1016/S0140-6736(17)32129-3
Lohmander LS, De Verdier MG, Rollof J, Nilsson PM, Engström G (2009) Incidence of severe knee and hip osteoarthritis in relation to different measures of body mass: a population-based prospective cohort study. Ann Rheum Dis 68:490–496. https://doi.org/10.1136/ARD.2008.089748
Bourne R, Mukhi S, Zhu N, Keresteci M, Marin M (2007) Role of obesity on the risk for total hip or knee arthroplasty. Clin Orthop Relat Res 465:185–188. https://doi.org/10.1097/BLO.0B013E3181576035
Podmore B, Hutchings A, Van Der Meulen J, Aggarwal A, Konan S (2018) Impact of comorbid conditions on outcomes of hip and knee replacement surgery: a systematic review and meta-analysis. BMJ Open 8(7):e021784. https://doi.org/10.1136/BMJOPEN-2018-021784
Jameson SS, Mason JM, Baker PN, Elson DW, Deehan DJ, Reed MR (2014) The impact of body mass index on patient reported outcome measures (PROMs) and complications following primary hip arthroplasty. J Arthroplasty 29:1889–1898. https://doi.org/10.1016/J.ARTH.2014.05.019
Verhaegen JCF, Wei R, Kim P, Beaulé PE, Corten K, Grammatopoulos G (2023) The safety and efficacy of the anterior approach total hip arthroplasty as per body mass index. J Arthroplasty 38:314–322. https://doi.org/10.1016/J.ARTH.2022.08.021
Vasarhelyi EM, MacDonald SJ (2012) The influence of obesity on total joint arthroplasty. J Bone Joint Surg Br 94:100–102. https://doi.org/10.1302/0301-620X.94B11.30619
Adhikary SD, Liu WM, Memtsoudis SG, Davis CM, Liu J (2016) Body Mass Index More Than 45 kg/m(2) as a cutoff point is associated with dramatically increased postoperative complications in total knee arthroplasty and total hip arthroplasty. J Arthroplasty 31:749–753. https://doi.org/10.1016/J.ARTH.2015.10.042
Arnold N, Anis H, Barsoum WK, Bloomfield MR, Brooks PJ, Higuera CA et al (2020) Preoperative cut-off values for body mass index deny patients clinically significant improvements in patient-reported outcomes after total hip arthroplasty. Bone Joint J 102:683–692. https://doi.org/10.1302/0301-620X.102B6.BJJ-2019-1644.R1
Li W, Ayers DC, Lewis CG, Bowen TR, Allison JJ, Franklin PD (2017) Functional gain and pain relief after total joint replacement according to obesity status. J Bone Joint Surg Am 99:1183. https://doi.org/10.2106/JBJS.16.00960
Sniderman J, Stark RB, Schwartz CE, Imam H, Finkelstein JA, Nousiainen MT (2021) Patient factors that matter in predicting hip arthroplasty outcomes: a machine-learning approach. J Arthroplasty 36:2024–2032. https://doi.org/10.1016/J.ARTH.2020.12.038
Peters RM, van Steenbergen LN, Stewart RE, Stevens M, Rijk PC, Bulstra SK et al (2021) Which patients improve most after total hip arthroplasty? Influence of patient characteristics on patient-reported outcome measures of 22,357 total hip arthroplasties in the Dutch Arthroplasty Register. Hip Int 31:593–602. https://doi.org/10.1177/1120700020913208
Wu ES, Cherian JJ, Jauregui JJ, Robinson K, Harwin SF, Mont MA (2016) Patient-reported outcomes following total hip arthroplasty stratified by body mass index. Orthopedics 39:e572–e577. https://doi.org/10.3928/01477447-20160404-09
Mukka S, Rolfson O, Mohaddes M, Sayed-Noor A (2020) The effect of body mass index class on patient-reported health-related quality of life before and after total hip arthroplasty for osteoarthritis: registry-based cohort study of 64,055 patients. JB JS Open Access 5(4):e20.00100. https://doi.org/10.2106/JBJS.OA.20.00100
Lyman S, Lee YY, Franklin PD, Li W, Mayman DJ, Padgett DE (2016) Validation of the HOOS, JR: a short-form hip replacement survey. Clin Orthop Relat Res 474:1472–1482. https://doi.org/10.1007/S11999-016-4718-2
Gruber-Baldini AL, Velozo C, Romero S, Shulman LM (2017) Validation of the PROMIS® measures of self-efficacy for managing chronic conditions. Qual Life Res 26:1915–1924. https://doi.org/10.1007/S11136-017-1527-3
Haeuser E, Serfes AL, Cork MA, Yang M, Abbastabar H, Abhilash ES et al (2022) Mapping age- and sex-specific HIV prevalence in adults in sub-Saharan Africa, 2000–2018. BMC Med 20(1):488. https://doi.org/10.1186/S12916-022-02639-Z
Hung M, Bounsanga J, Voss MW, Saltzman CL (2018) Establishing minimum clinically important difference values for the Patient-Reported Outcomes Measurement Information System Physical Function, hip disability and osteoarthritis outcome score for joint reconstruction, and knee injury and osteoarthritis outcome score for joint reconstruction in orthopaedics. World J Orthop 9:41–49. https://doi.org/10.5312/WJO.V9.I3.41
Franovic S, Gulledge CM, Kuhlmann NA, Williford TH, Chen C, Makhni EC (2019) Establishing “Normal” patient-reported outcomes measurement information system physical function and pain interference scores: a true reference score according to adults free of joint pain and disability. JB JS Open Access 4(4):e0019. https://doi.org/10.2106/JBJS.OA.19.00019
Singh V, Yeroushalmi D, Lygrisse KA, Schwarzkopf R, Davidovitch RI (2021) Impact of obesity on the forgotten joint score following primary total hip arthroplasty. J Arthroplasty 36:1342–1347. https://doi.org/10.1016/J.ARTH.2020.10.027
Temporiti F, Zanotti G, Furone R, Loppini M, Molinari S, Zago M et al (2019) Functional and postural recovery after bilateral or unilateral total hip arthroplasty. J Electromyogr Kinesiol 48:205–211. https://doi.org/10.1016/J.JELEKIN.2019.08.002
Yoshii H, Oinuma K, Tamaki T, Miura Y, Kaneyama R, Shiratsuchi H (2016) Comparison of patient satisfaction after unilateral or simultaneous bilateral total hip arthroplasty through a direct anterior approach: evaluation using the Japanese orthopaedic association hip disease evaluation questionnaire. J Orthop Sci 21:332–335. https://doi.org/10.1016/J.JOS.2016.01.008
Anis HK, Sodhi N, Coste M, Ehiorobo JO, Newman JM, Garbarino LJ, Gold P, Freund B, Piuzzi N, Mont MA (2019) A comparison of peri-operative outcomes between elective and non-elective total hip arthroplasties. Ann Transl Med. 7(4):78. https://doi.org/10.21037/atm.2019.01.64
Lyman S, Lee YY, McLawhorn AS, Islam W, MacLean CH (2018) What are the minimal and substantial improvements in the HOOS and KOOS and JR versions after total joint replacement? Clin Orthop Relat Res 476:2432–2441. https://doi.org/10.1097/CORR.0000000000000456
Terwee CB, Peipert JD, Chapman R, Lai JS, Terluin B, Cella D et al (2021) Minimal important change (MIC): a conceptual clarification and systematic review of MIC estimates of PROMIS measures. Qual Life Res 30:2729–2754. https://doi.org/10.1007/S11136-021-02925-Y
Cohen-Levy WB, Lans J, Salimy MS, Melnic CM, Bedair HS (2022) The significance of race/ethnicity and income in predicting preoperative patient-reported outcome measures in primary total joint arthroplasty. J Arthroplasty 37:S428–S433. https://doi.org/10.1016/J.ARTH.2022.02.041
Rubenstein WJ, Harris AHS, Hwang KM, Giori NJ, Kuo AC (2020) Social determinants of health and patient-reported outcomes following total hip and knee arthroplasty in veterans. J Arthroplasty 35:2357–2362. https://doi.org/10.1016/J.ARTH.2020.04.095
Singh V, Realyvasquez J, Kugelman DN, Aggarwal VK, Long WJ, Schwarzkopf R (2021) Does racial background influence outcomes following total joint arthroplasty? J Clin Orthop Trauma 19:139. https://doi.org/10.1016/J.JCOT.2021.05.017
Judge A, Batra RN, Thomas GE, Beard D, Javaid MK, Murray DW et al (2014) Body mass index is not a clinically meaningful predictor of patient reported outcomes of primary hip replacement surgery: prospective cohort study. Osteoarthritis Cartilage 22:431–439. https://doi.org/10.1016/J.JOCA.2013.12.018
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was approved by our institutional review board (IRB) prior to any study procedures (IRB #i17-01223).
Availability of data
The datasets generated and/or analyzed during the current study are not publicly available as they contain protected health information from within our institution, but de-identified data can be made available from the corresponding author on reasonable request.
Conflict of interests
WS: Nothing to disclose. KWL: Nothing to disclose. MAH: Nothing to disclose. JT: Nothing to disclose. RS: AAOS: Board or committee member. American Association of Hip and Knee Surgeons: Board or committee member. Arthroplasty Today: Editorial or governing board. Gauss surgical: Stock or stock Options. Intelijoint: Paid consultant; Stock or stock Options. Journal of Arthroplasty: Editorial or governing board. PSI: Stock or stock Options. Smith & Nephew: IP royalties; Paid consultant; Research support. Zimmer: Paid consultant. JCR: Zimmer: Paid consultant. DePuy, Johnson & Johnson: Paid consultant Aerobiotix: Paid consultant.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sobba, W., Lawrence, K.W., Haider, M.A. et al. The influence of body mass index on patient-reported outcome measures following total hip arthroplasty: a retrospective study of 3,903 Cases. Arch Orthop Trauma Surg 144, 2889–2898 (2024). https://doi.org/10.1007/s00402-024-05381-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-024-05381-8