Abstract
Background
Total hip arthroplasty (THA) is the gold standard procedure for patients with end-stage osteoarthritis after failed conservative therapy. Digital templating is commonly employed in preoperative preparation for THA and contributes positively to its outcome. However, the impact of coxa valga and antetorta (CVA) configurations on stem size prediction accuracy remains not reported. Previous studies demonstrated that the size of the lesser trochanter (LT) can be used to determine femoral anteversion on pelvis radiographs. This study investigates the accuracy of preoperative digital templating in predicting stem size in patients with CVA undergoing cementless THA.
Methods
Preoperative radiographs of 620 patients undergoing cementless THA were retrospectively investigated. Radiographs were standardized with patients standing and the leg internally rotated by 15°. A CVA group was established including patients with a CCD angle greater than 140° and a lesser trochanter (LT) size of at least 10 mm for men and 8 mm for women. For the control group, radiographs with a CCD angle ranging from 125–135° and LT size 3–10 mm for men and 3–8 mm for women were selected. Preoperative templating was performed using mediCAD. To reduce confounding factors, case-control matching was carried out for BMI and body height.
Results
After case-control matching, a total of thirty-one matches were analyzed. Stem size was underestimated in 74% (23/31) in the CVA and 13% (4/31) in the control group (p < 0.001). Moreover, patients with CVA were more likely to be underestimated by two sizes compared to controls (p < 0.004). In contrast, the exact stem size was predicted more frequently in the control group (p < 0.001).
Conclusion
Stem size in patients with a CVA configuration are at high risk of being underestimated when using digital templating. These findings can be valuable for guiding in intraoperative decisions and lowering the risk of complications associated with an undersized femoral component.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Total hip arthroplasty (THA) is one of the most successful procedures in orthopaedic surgery and was even described as ‘the operation of the century’ by Learmonth et al. [1]. THA remains the gold standard for patients suffering from advanced osteoarthritis of the hip after failed conservative therapy [2] and is performed million times a year throughout the world [3]. Due to demographic changes, the frequency of both primary and revision THA is expected to increase in the coming decades, underscoring the importance of precise THA [4]. The correct positioning of implants is related to better outcome, longevity, and complication rate [4, 5]. Preoperative templating, routinely performed on anteroposterior radiographs of the pelvis, has been shown to enhance the accuracy of implant placement in THA. The goal is to simulate the restoration of key biomechanical factors such as the center of rotation, implant size, leg length, and offset [4, 6]. Consequently, digital templating has become a routine procedure during preoperative preparation in THA [7]. However, despite the use of digital templating software, the current literature reports a certain discrepancy regarding predicted and implanted component size [8, 9]. Recently identified causes leading to inaccurate prediction include malpositioning of the measuring ball, obesity and experience of surgeon [8, 10]. Another factor contributing to incorrect size prediction could be excessive femoral antetorsion which is often accompanied by coxa valga in patients undergoing THA. The assessment of femoral antetorsion is challenging [11] and mostly performed using three-dimensional imaging but previous studies have demonstrated that femoral anteversion can also be assessed by the projected size of the lesser trochanter (LT) on anterior-posterior pelvic radiographs [12, 13]. Patients with a coxa valga and antetorta (CVA) configuration may constitute a group of interest when performing digital templating using two-dimensional imaging. To the best of the authors’ knowledge, this specific group has not been investigated in the existing literature.
The aim of this study was to assess whether patients with a coxa valga and antetorta configuration demonstrate a higher degree of inaccuracy during digital templating of the femoral component using pelvic radiographs in comparison to a control group.
Methods
Patient selection
For the CVA group, we retrospectively examined a total of 620 patients with end-stage hip osteoarthritis who underwent cementless THA at our institution between October 2022 and December 2023. For the control group, a total of 224 patients with end-stage hip osteoarthritis between January 2023 and July 2023 undergoing cementless THA were examined. Demographic data, predicted as well as implanted stem size, centrum collum diaphysis (CCD) angle, and size of the LT were documented for all patients included in this study. Exclusion criteria included poor bone quality (Dorr-C), acute or previous fractures, prior osteotomy/osteosynthesis of the proximal femur, malaligned (valgus/varus > 1°), and undersized implanted stems. All surgical procedures were performed using the dorsal approach. The study protocol received approval from the local ethics committee (2024-300433-WF) and was conducted in accordance with the principles of the Declaration of Helsinki.
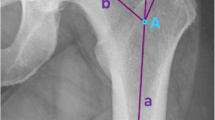
Radiographic analysis
All radiographs adhered to a standardized protocol, with imaging conducted in a standing position and the legs internally rotated by 15°. Calibration was performed using a 25 mm measuring ball. Patients with a CCD angle of more than 140° and an anteverted femur, characterized by a size of the LT of at least 10 mm in men and 8 mm in women, were selected for the CVA group. Former studies have investigated the assessment of femoral anteversion by measuring the size of the lesser trochanter [12, 13]. The control group comprised patients with a CCD angle ranging from 125° to 135°, absence of rotation of the greater trochanter, and a size of the LT with a range from 3 to 10 mm for men and 3 to 8 mm for women. Sex-dependent differences in the size of the LT [12] and the methodology for LT size measurement [13] used in this study have been reported elsewhere.
Preoperative templating on pelvis radiographs was carried out using mediCAD (Hectec GmbH, Altdorf/Landshut, Germany) by two trained orthopaedic surgeons (CS & MJ) independently. Any disagreements regarding component size were resolved by a senior orthopaedic surgeon (ON). In all patients, the cementless Corail femoral stem (DePuy Synthes, Warsaw, Indiana, USA) was used. Figure 1 illustrates an example for preoperative and postoperative pelvic x-rays along with digital templating for both groups.
After applying inclusion and exclusion criteria, 38 patients were identified for the CVA group, and 60 patients for the control group. To minimize magnification error and differences in LT size dependent on body height, case-control matching was performed for the variables BMI and body height, allowing a tolerance of 3 BMI points and 5 cm, respectively. Following casecontrol matching, 31 pairs of patients were successfully matched, yielding a total of 62 patients for further analysis. Demographic characteristics for both groups are presented in Table 1.
Statistical analysis
Differences between the two groups were assessed using an independent t-test and Chisquare test, or Fisher’s exact test when appropriate. A one-way analysis of variance (ANOVA) was employed when comparing the means of more than two groups. Post hoc analysis for Chi-squared test with the Bonferroni-Holm correction was applied for adjustment of multiple testing. P-values of less than 0.05 were considered statistically significant. All statistics analyses were carried out using IBM SPSS statistics® (version 29.0.1).
Results
In the CVA group, there were 19 right and 12 left hips, whereas in the control group, there were 22 right and 9 left hips, respectively. Notably, there were no differences in weight, BMI, or body height between the two groups. A significant difference in age was observed, with the CVA group displaying a lower age compared to the control group (60.5 ± 9.2 vs. 66.8 ± 13.9; p = 0.041). The CVA and control group showed a mean CCD angle of 147.3° ± 5.0 and 131.8° ± 2.5, and a mean size of the LT of 11.5 mm ± 1.8 vs. 6.4 mm ± 1.3, respectively.
In the control group, the stem size was exactly predicted in 77% (24/31), whereas 23% (7/31) were one size above or below the actual stem size. When predicting stem size in the CVA group, 26% (8/31) were exact, 42% (13/31) were one size below, and 32% (10/31) were two sizes below compared to the actual stem size. Overall, stem size was underestimated in 74% (23/31) of patients in the CVA and 13% (4/31) of patients in the control group (p < 0.001). Notably, no stem size was predicted to be larger than the implanted size in the CVA group.
In further analysis, subgroups were formed within both groups based on the degree of difference between preoperatively predicted and implanted stem sizes (Fig. 2). Post hoc analysis for the Chi-square test revealed a significantly higher number of patients with exactly predicted stem sizes in the control group compared to the CVA group (p < 0.001). Of note, patients with a CVA hip configuration showed a significant underestimation by two sizes compared to controls (p = 0.004). Although there were more patients underestimated by one size in the CVA group, this difference was not significant (p = 0.075). Demographic and radiological characteristics within the subgroups of the CVA group did not show any significant differences, as presented in Table 2.
Control (green) versus CVA group (yellow) shown in subgroups regarding difference in stem size between the predicted and the implanted size (Δ-1 = overestimation; Δ0 = exact; Δ1, Δ2 = underestimation, when comparing predicted to implanted stem size). The percentages of patients for both groups are displayed within the columns, with corresponding p-values indicated above. CVA = Coxa valga and antetorta
* Statistically significant
Discussion
Preoperative digital templating plays an essential role in the success of THA. Apart from its valuable assistance to surgeons, templating has proven effective in reducing major complications, including leg length inequality [14], peri-prosthetic fractures [15], and aseptic loosening [16]. The primary aim of this study was to examine accuracy of the predicted stem size in patients with CVA. The results indicate a clear underestimation of the predicted stem size in this anatomical variation compared to a control group. Presumably, increased femoral anteversion causes the femur to rotate externally in standardized pelvic radiographs, leading to a narrower mediolateral width of the oval diameter of the femoral shaft on two-dimensional images, thereby resulting in an underestimation of the stem size during digital templating. Similarly, Hananouchi et al. [17] observed an underestimation in stem size when virtually rotating the femur externally using synthetic x-rays of the hip derived from CT-scans. The results of this study revealed that within the CVA group, 74% were predicted to have a smaller stem size compared to the size implanted, with 32% being underestimated by two stem sizes. Undersizing the femoral component increases the risk of severe complications, including aseptic loosening [18, 19], periprosthetic fractures [16], and early subsidence [20]. Considering the significant younger age of the CVA group in comparison to the controls, preventing these complications is of high importance. Moreover, the findings of this study provide valuable guidance for surgeons during intraoperative decision-making and underscore the need for further enhancement of preoperative templating methods for patients with this anatomical variation.
Although preoperative templating leads to an improved outcome of THA, significant size deviations between preoperative planning and implanted component sizes are described in the literature. With the prediction of the femoral component within one size our study revealed a 100% accuracy in the control group. In contrast, Holzer et al. [8] reported an accuracy of 87% in predicting stem size within one size in 632 patients who had primary uncemented THA. There can be many reasons for this including increased BMI, malpositioning of the ball and the experience of surgeon [10, 21]. No differences in BMI were observed within the subgroups of the CVA group, suggesting that underestimation of stem size in this group was unrelated to BMI. The topic of three-dimensional templating has gained increasing attention in recent years, with literature suggesting that size prediction is more accurate compared to digital twodimensional templating [22, 23]. However, higher radiation exposures and higher costs for radiologic equipment and templating software must be considered when implementing three-dimensional templating. It is unclear whether certain anatomic variations such as CVA could benefit from three-dimensional templating before THA. This issue is complicated by significant differences among three-dimensional measurement results of femoral anteversion depending on the method used [11]. The findings of this study may indicate that three-dimensional templating could be advantageous for patients with a CVA configuration. Nevertheless, additional research is warranted to thoroughly explore this matter, with specific attention to determining the potential benefits of three-dimensional templating for the patients’ outcome.
Femoral anteversion is a frequent anatomic variation in THA and often associated with dysplasia of the hip as well as coxa valga [24]. Three-dimensional imaging such as MRI or CT are widely accepted as reliable procedures to measure femoral anteversion [25, 26]. However, three-dimensional imaging is not a standard procedure prior to primary THA. Only a limited number of studies have investigated femoral rotation based on the visible size of the LT on radiographs while simultaneously measuring anteversion using three-dimensional imaging [12, 13]. In this study, the observed mean size of the LT in the control group was 6.4 mm, consistent with the findings of Marchand et al. [12] for normally rotated femora using CT scans. This consistency underscores the reliability of the control group in our study. However, current data suggests that the LT size cannot be used alone as it only accounts for femoral rotation in about two thirds of cases [12, 13]. In other words, in about one-third of patients, the size of the LT may be misinterpreted regarding femoral rotation, which could explain why underestimation did not occur in about one-third (26%) of patients in the CVA group. Future studies are needed to further address the reliability of the lesser trochanters’ profile on pelvic radiographs as an indicator for excessive femoral anteversion and explore whether other morphological criteria can contribute to additional assessment.
This study has several limitations. One is evident in its retrospective design. Furthermore, this study did not use three-dimensional methods for measuring femoral anteversion, which are considered the gold standard for assessing femoral rotation. Additionally, preoperative templating was not carried out by a senior orthopaedic surgeon, which may have potentially influenced the accuracy of templating. Moreover, the small number of cases, comprising only 31 included patients in each group, may affect the validity of the results.
Conclusion
This study is the first to examine the accuracy of stem size prediction using digital templating in patients with a CVA configuration. Our findings revealed a significant underestimation of the predicted stem size in the CVA group compared to controls. These results offer valuable insights for surgeons to assist in intraoperative decision-making and may help reduce the risk of complications associated with an undersized femoral component in a significant younger population with CVA undergoing cementless THA. Furthermore, future research should explore the advantages of three-dimensional over two-dimensional templating in patients with CVA and evaluate its clinical relevance.
Change history
03 June 2024
The street name of affiliation address is depicted with question marks. It has been updated from “K?sterbergstra?e” to “Kösterbergstraße”.
Abbreviations
- ANOVA:
-
Analysis of Variance
- BMI:
-
Body Mass Index
- CCD:
-
Centrum Collum Diaphysis
- CT:
-
Computer Tomography
- CVA:
-
Coxa Valga and Antetorta
- LT:
-
Lesser Trochanter
- MRI:
-
Magnetic Resonance Imaging
- THA:
-
Total Hip Arthroplasty
References
Learmonth ID, Young C, Rorabeck C (2007) The operation of the century: total hip replacement. Lancet (London England) 370:1508–1519. https://doi.org/10.1016/S0140-6736(07)60457-7
Kong L, Chen L, Sun L, Tian X (2020) Direct anterior approach or posterior approach in total hip arthroplasty: a direct comparative study protocol. Med (Baltim) 99:e22717. https://doi.org/10.1097/MD.0000000000022717
Maradit Kremers H, Larson DR, Crowson CS et al (2015) Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am 97:1386–1397. https://doi.org/10.2106/JBJS.N.01141
Girgis SF, Kohli S, Kouklidis G et al (2023) The Accuracy of Digital Preoperative Templating in primary total hip replacements. Cureus 15:e43046. https://doi.org/10.7759/cureus.43046
Della Valle AG, Padgett DE, Salvati EA (2005) Preoperative planning for primary total hip arthroplasty. J Am Acad Orthop Surg 13:455–462. https://doi.org/10.5435/00124635-200511000-00005
Colombi A, Schena D, Castelli CC (2019) Total hip arthroplasty planning. EFORT open Rev 4:626–632. https://doi.org/10.1302/2058-5241.4.180075
Aubert T, Galanzino G, Gerard P et al (2023) Accuracy of preoperative 3D vs 2D Digital Templating for Cementless Total Hip Arthroplasty using a direct Anterior Approach. Arthroplast Today 24:101260. https://doi.org/10.1016/j.artd.2023.101260
Holzer LA, Scholler G, Wagner S et al (2019) The accuracy of digital templating in uncemented total hip arthroplasty. Arch Orthop Trauma Surg 139:263–268. https://doi.org/10.1007/s00402-018-3080-0
Efe T, El Zayat BF, Heyse TJ et al (2011) Precision of preoperative digital templating in total hip arthroplasty. Acta Orthop Belg 77:616–621
Sinclair VF, Wilson J, Jain NPM, Knowles D (2014) Assessment of accuracy of marker ball placement in pre-operative templating for total hip arthroplasty. J Arthroplasty 29:1658–1660. https://doi.org/10.1016/j.arth.2014.03.013
Schmaranzer F, Meier MK, Lerch TD et al (2022) Coxa valga and antetorta increases differences among different femoral version measurements: potential implications for derotational femoral osteotomy planning. Bone Jt open 3:759–766. https://doi.org/10.1302/2633-1462.310.BJO-2022-0102.R1
Marchand LS, Todd DC, Kellam P et al (2018) Is the lesser Trochanter Profile a Reliable means of restoring anatomic Rotation after Femur fracture fixation? Clin Orthop Relat Res 476:1253–1261. https://doi.org/10.1007/s11999.0000000000000226
Worlicek MC, Wörner ML, Craiovan BS et al (2017) Lesser Trochanter size on plain anteroposterior radiographs correlates with native femoral anteversion. J Arthroplasty 32:2892–2897. https://doi.org/10.1016/j.arth.2017.03.054
Desai AS, Dramis A, Board TN (2013) Leg length discrepancy after total hip arthroplasty: a review of literature. Curr Rev Musculoskelet Med 6:336–341. https://doi.org/10.1007/s12178-013-9180-0
Haddad FS, Masri BA, Garbuz DS, Duncan CP (1999) The prevention of periprosthetic fractures in total hip and knee arthroplasty. Orthop Clin North Am 30:191–207. https://doi.org/10.1016/s0030-5898(05)70074-2
Kelmer G, Stone AH, Turcotte J, King PJ (2021) Reasons for revision: primary total hip arthroplasty mechanisms of failure. J Am Acad Orthop Surg 29:78–87. https://doi.org/10.5435/JAAOS-D-19-00860
Hananouchi T, Sugano N, Nakamura N et al (2007) Preoperative templating of femoral components on plain X-rays. Rotational evaluation with synthetic X-rays on ORTHODOC. Arch Orthop Trauma Surg 127:381–385. https://doi.org/10.1007/s00402-007-0349-0
Streit MR, Innmann MM, Merle C et al (2013) Long-term (20- to 25-year) results of an uncemented tapered titanium femoral component and factors affecting survivorship. Clin Orthop Relat Res 471:3262–3269. https://doi.org/10.1007/s11999-013-3033-4
Fottner A, Woiczinski M, Kistler M et al (2017) Influence of undersized cementless hip stems on primary stability and strain distribution. Arch Orthop Trauma Surg 137:1435–1441. https://doi.org/10.1007/s00402-017-2784-x
Kim YH, Kim VE (1993) Early migration of uncemented porous coated anatomic femoral component related to aseptic loosening. Clin Orthop Relat Res 146–155
Dammerer D, Keiler A, Herrnegger S et al (2022) Accuracy of digital templating of uncemented total hip arthroplasty at a certified arthroplasty center: a retrospective comparative study. Arch Orthop Trauma Surg 142:2471–2480. https://doi.org/10.1007/s00402-021-03836-w
Brenneis M, Braun S, van Drongelen S et al (2021) Accuracy of Preoperative Templating in Total Hip Arthroplasty with Special Focus on Stem morphology: a randomized comparison between Common Digital and three-Dimensional Planning using biplanar radiographs. J Arthroplasty 36:1149–1155. https://doi.org/10.1016/j.arth.2020.10.016
Schiffner E, Latz D, Jungbluth P et al (2019) Is computerised 3D templating more accurate than 2D templating to predict size of components in primary total hip arthroplasty? Hip Int J Clin Exp Res hip Pathol Ther 29:270–275. https://doi.org/10.1177/1120700018776311
Lerch TD, Todorski IAS, Steppacher SD et al (2018) Prevalence of femoral and Acetabular Version Abnormalities in patients with symptomatic hip disease: a controlled study of 538 hips. Am J Sports Med 46:122–134. https://doi.org/10.1177/0363546517726983
Wells J, Nepple JJ, Crook K et al (2017) Femoral morphology in the dysplastic hip: three-dimensional characterizations with CT. Clin Orthop Relat Res 475:1045–1054. https://doi.org/10.1007/s11999-016-5119-2
Hesham K, Carry PM, Freese K et al (2017) Measurement of femoral version by MRI is as Reliable and reproducible as CT in Children and adolescents with Hip disorders. J Pediatr Orthop 37:557–562. https://doi.org/10.1097/BPO.0000000000000712
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conradin Schweizer: Conceptualization, Investigation, data curation, formal analysis, writing—original draft, writing—review & editing Oliver Niggemeyer: writing—review & editing, supervision Jan-Hauke Jens: writing—review & editing Marius Junker: Conceptualization, methodology, investigation, data curation, writing—original draft, writing—review& editing, visualization, project administration. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the local ethics committee (2024-300433-WF).
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schweizer, C., Niggemeyer, O., Jens, JH. et al. Coxa valga and antetorta configuration leads to underestimation of the femoral component size: a matched case-control study of patients undergoing cementless total hip arthroplasty. Arch Orthop Trauma Surg 144, 2859–2864 (2024). https://doi.org/10.1007/s00402-024-05373-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-024-05373-8