Abstract
Introduction
This study evaluated the correlation between postoperative knee joint line obliquity after medial open-wedge high tibial osteotomy and patient-reported outcome measures excluding excessively overcorrected knees. This study further identified preoperative radiological factors related to the increased postoperative knee joint line obliquity.
Materials and methods
We retrospectively evaluated patients who underwent medial open-wedge high tibial osteotomy between March 2013 and March 2021. Postoperative excessively overcorrected knees with hip-knee-ankle angle > 7° were excluded. We investigated radiological parameters and patient-reported outcome measures preoperatively and at the last follow-up. The following radiologic parameters were measured: hip-knee-ankle angle, weight-bearing line ratio, mechanical medial proximal tibial angle, mechanical lateral distal femoral angle, lateral distal tibial angle, joint line convergent angle, knee joint line obliquity, ankle joint line obliquity, hip abduction angle, tibial posterior slope, Carton-Deschamps index, and patella tilting angle. Clinical outcomes were evaluated using Japanese knee outcome measures. This assessment criterion is based on the Western Ontario McMaster Universities Arthritis Index and MOS Short Form 36. Multiple regression analysis was performed to evaluate the association between postoperative knee joint line obliquity and patient-reported outcome measures or preoperative radiological factors (P < .05).
Results
A total of 52 knees were included. The mean age at the time of the surgery was 61.6 ± 9.0 years and the mean follow-up period was 30.6 ± 10.1 months. Increased postoperative knee joint line obliquity was associated with lower Japanese knee outcome measures. The preoperative hip-knee-ankle angle was significantly associated with postoperative knee joint line obliquity.
Conclusions
Increased knee joint line obliquity after medial open-wedge high tibial osteotomy is associated with inferior clinical outcomes. Care should be given to the center of the rotational angulation in around-knee osteotomy to avoid postoperative increased knee joint line obliquity.
Level of evidence
Retrospective comparative study, Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Medial open-wedge high tibial osteotomy (MOWHTO) is a well-established treatment for symptomatic medial unicompartmental knee osteoarthritis (OA) with varus deformity [1]. However, single-level osteotomy of the tibia may result in pathological knee joint line obliquity (KJLO) [2, 3].
An excessively high KJLO elicits problems, such as unfavorable knee kinematics and increased articular cartilage shear stress [4,5,6]. Whether excessive KJLO leads to poor clinical outcomes remains controversial. Goshima et al. reported that mechanical medial proximal tibial angle (mMPTA) > > 95° did not affect clinical outcomes [7]. Conversely, Akamatsu et al. reported that patients with KJLO > 4° had a higher risk of short survivorship [8]. Additionally, Babis et al. stated that patients with mMPTA > 95° had inferior clinical outcomes [2]. Most studies that reported a negative effect of excessive KJLO included overcorrected knees leading to poor clinical outcomes. MOWHTO changes not only the coronal inclination of the tibia, but also sagittal and axial alignments [9, 10]. Many reports investigated the relationship between coronal alignment factors and the KJLO. However, no study indicated a relationship between postoperative KJLO and postoperative 3-dimensional geometric changes, including the tibial posterior slope (TPS), Carton-Deschamps index (CDI), and patella tilting angle (PT).
Thus, this present novel study: (1) evaluated the correlation between postoperative KJLO and patient-reported outcome measures (PROMs) excluding excessively overcorrected knees, (2) identified preoperative radiological factors related to increased postoperative KJLO, and (3) evaluated the relationship between postoperative KJLO and three-dimensional geometric changes. Our hypotheses were as follows: (1) an increased postoperative KJLO was correlated with inferior PROMs; (2) an increased postoperative KJLO was associated with preoperative hip-knee-ankle (HKA), mechanical lateral distal femoral angle (mLDFA), and joint line convergent angle (JLCA); and (3) a postoperative KJLO was correlated with postoperative TPS, CDI, and PT.
Materials and methods
Patients
A total of 78 patients (84 knees) who underwent MOWHTO between March 2013 and March 2021 at a single institution were enrolled in this study. The exclusion criteria were a history of inflammatory arthritis, ligament surgery, concurrent distal femoral osteotomy (DFO), follow-up of < 2 years, insufficient data, and excessive overcorrection. We defined postoperative HKA > 7° as excessive overcorrection because postoperative HKA 2° to 7° valgus was considered ideal alignment after MOWHTO, and the HKA value in non-osteoarthritis knees ranged from 7.6° varus to 7.1° valgus [11, 12]. The surgical indications for MOWHTO were symptomatic OA and ON of the medial compartment with varus malalignment and active patients who complied with the post-operating rehabilitation program. The contraindications for MOWHTO were a history of joint infection, symptomatic OA of the lateral compartment or patella femoral (PF) joint, and flexion contracture of > 15°. Additionally, we performed closed wedge osteotomy or double-level osteotomy (DLO) with expected postoperative correction angle > 15°or postoperative mMPTA > 95°preoperatively.
Radiographic and clinical evaluations
We retrospectively reviewed anteroposterior (AP) long-standing HKA radiographs with the patella facing forward at shoulder width, lateral view, and skyline view, with the knee flexed to 45° both preoperatively and during follow-up. The following radiological parameters were measured: HKA, Weight-bearing line ratio (WBLR), mMPTA, mLDFA, lateral distal tibial angle (LDTA), JLCA, KJLO, ankle joint line obliquity (AJLO), hip abduction angle (HAA), TPS, CDI, and PT. TPS and CDI were measured using the lateral view and PT in the skyline view. Other parameters were deliberated using long-standing HKA radiographs (Fig. 1). All radiological parameters for 30 randomly selected knees were measured twice by two orthopedic surgeons (xx and yy), with a 2-week interval between each measurement (Appendix Table). The observers were blinded to previous observations using a picture archiving and communication system (SYNAPSE Enterprise-PACS; Fujifilm).
Radiographic assessment. A HKA: HKA is the angle formed between the mechanical femoral and mechanical tibial axes (varus, negative). B Weight-bearing line ratio (WBLR): WBLR is defined as the horizontal distance from the WBL to the medial edge of the tibial plateau divided by the width of the tibial plateau. C Mechanical medial proximal tibial angle (mMPTA): The mMPTA is the medial angle formed between the mechanical tibial axis and the joint line of the proximal tibia. Mechanical lateral distal femoral angle (mLDFA): The mLDFA is the lateral angle formed between the mechanical femoral axis and the joint line of the distal femur. Lateral distal tibial angle (LDTA): LDTA is the lateral angle formed between the mechanical tibial axis and the joint line of the distal tibia. Joint line convergent angle (JLCA): JLCA is the angle between the tangents to the femoral condyles and the tibial plateau, with a positive value for JLCA denoting lateral joint opening. D Knee joint line obliquity (KJLO): KJLO is the angle between a line parallel to the ground and the tangent to the proximal tibia with a lateral tilt defined as a positive value. Ankle joint line obliquity (AJLO): AJLO is the angle between a line parallel to the ground and the tangent to the talar dome with lateral tilt defined as a positive. Hip abduction angle (HAA): HAA is the angle between the femoral mechanical axis and a line perpendicular to the ground, with abduction defined as a positive value. E Tibial posterior slope (TPS): TPS is the angle between the line perpendicular to the mid-diaphysis of the tibia and the posterior inclination of the tibial plateau. The Canton-Deschamps index (CDI): CDI was calculated. The distance from the inferior aspect of the patellar articular surface to the anterior edge of the tibial plateau was divided by the patellar articular surface length. F Patellar tilting angle (PT): PT is the angle between the line intersecting the widest bony structures of the patella and the line tangential to the anterior surface of the femoral condyles
PROMs were evaluated using the Japanese knee osteoarthritis measure (JKOM) [13] preoperatively and at the last follow-up. The JKOM is an assessment criterion based on the Western Ontario McMaster Universities Arthritis Index (WOMAC), the MOS Short Form 36 (SF-36) [14], and a patient-based self-answered evaluation scoring system to reflect the specific Japanese cultural lifestyle: pain and stiffness (8 questions, 0–30 points), activities of daily living (10 questions, 0–40 points), participation in social activities (5 questions, 0–20 points), and general health conditions (2 questions, 0–10 points), with a maximum score of 100 points (0 indicating no symptoms and 100 indicating extreme symptoms). Based on previous studies [2], we also divided postoperative KJLO into two groups: normal group, KJLO≦4° (n = 47), pathological group, KJLO > 4° (n = 6), and the subgroup analysis was performed.
Surgical procedure and postoperative rehabilitation
Preoperative planning was done using AP long-standing HKA radiographs by the method described by Miniaci et al. [15]. The target WBLR was 62.5% [16]. Arthroscopy was routinely performed before HTO, and additional intra-articular lesions were treated accordingly based on a previously reported standing procedure [17, 18]. The medial proximal tibia was exposed through an oblique incision. The semitendinosus and gracilis tendons were preserved, and the superficial medial collateral ligament was released distally. Under fluoroscopic guidance, two K-wires were inserted 4 cm below the medial joint line, just proximal to the tibiofibular joint. Biplanar ascending osteotomy of the tuberosity was performed within 1 cm of the lateral cortex. Several chisels were used to gradually open the osteotomy and a lamina spreader was used for the final opening. Two β-tricalcium phosphate wedges (Olympus Terumo Biomaterial) were inserted into the osteotomy site. A fixed-angle plate with locking screws (TomoFix Osteotomy System; DePuy Synthes, Tris medial HTO plate system; Olympus Terumo Biomaterial, Puddu spacer plate; Arthlex Inc., HTO plate system; Teijin Nakashima Medical, Japan) was used to fix the proximal tibia. Passive and active range of motion exercises, isometric exercises of the quadriceps, and straight leg raising were started on postoperative day 1. The patients were allowed partial weight-bearing at 1 week postoperatively, and full weight-bearing at 2 weeks.
Ethical approval
The study protocol was approved by an appropriate Ethics review board, and all patients provided informed consent for the surgical procedures.
Statistical analyses
All statistical analyses were performed using EZR ver1.60 (Saitama Medical Centre, Jichi Medical University), a graphical user interface for R (The R Foundation for Statistical Computing) [19], which is a modified version of R Commander, designed to add statistical functions frequently used in biostatistics. The Wilcoxon signed-rank sum test compared the radiological parameters and JKOM preoperatively and at the last follow-up. The Mann–Whitney U test assessed demographics, JKOM, and radiological parameters between the normal and pathological KJLO groups. Stepwise multivariable linear regression analysis identified the independent factors associated with JKOM, such as patient age, sex, BMI, KL grade, postoperative mMPTA, postoperative KJLO, postoperative TPS, postoperative CDI, and postoperative PT. Multivariable linear regression analysis examined the radiological preoperative risk factors for postoperative increased KJLO. We chose preoperative HKA, mMPTA, mLDFA, LDTA, and JLCA from previous studies [20, 21]. Spearman’s rank correlation analysis identified the correlation between postoperative KJLO, JKOM, and postoperative TPS, CDI, and PT. Statistical significance was set at p < 0.05. A priori power analysis calculated the minimum sample size necessary for correlating postoperative KJLO and PROMs (moderate effect size [r], 0.5; α value; 0.05, and power; 0.9) using G*Power (Version 3.1. 9.6; Franz Faul, Christian-Albrechts-Universitätzu Kiel). The analysis indicated that the required sample size was 34 knees. Furthermore, for multiple regression analysis, a posthoc statistical power calculation was performed (effect size [f2]; observed R2, α value; 0.05, total sample size, and number of predictors) using G*Power 21 [22].
Results
Patient demographics, PROMs, and pre-postoperative radiological parameters
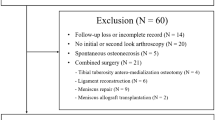
A total of 53 knees (51 patients, two bilateral knees) met the inclusion criteria. Figure 2 shows the inclusion process. The mean age at the time of the surgery was 61.6 ± 9.0 years and the mean BMI was 27.4 ± 4.1. The mean follow-up period was 30.6 ± 10.1 months. No nonunion/malunion or conversion to arthroplasty was observed during follow-up. The patient demographics, radiological parameters, and PROMs preoperatively at the last follow-up are summarized in Table 1. There were significant differences in all radiological parameters between the preoperative and last follow-up except for the mLDFA and JLCA (p = 0.417 and p = 0.84, respectively). KJLO changed from mean – 1.7 ± 2.0° (medial tilt) to mean 2.0 ± 2.8° (lateral tilt) after MOWHTO (Fig. 3). No significant differences were noted in preoperative demographic and radiological data between the subgroups. The pathological KJLO group (KJLO > 4°) had a lower postoperative HKA (p = 0.02). Postoperative JLCA was larger in the pathological KJLO group than in the normal, although the difference was not significant (p = 0.097). Regarding clinical outcomes, there was a significant difference only in the JKOM subscale: participation in social activities (p = 0.04); the pathological group tended to have inferior clinical outcomes overall Tables 2, 3 and 4.
Correlation between postoperative KJLO and PROMs
There was a correlation between postoperative KJLO and JKOM subscales: general health condition (r = 0.378, p = 0.014) and total score (r = 0.317, p = 0.041) (Table 5). In the multiple regression analysis, postoperative increased KJLO and decreased CDI were correlated with the inferior JKOM subscale: general health conditions (adjusted R2 = 0.5318). Additionally, increased BMI, postoperative increased KJLO, and increased TPS were correlated with an inferior JKOM total score (adjusted R2 = 0.4632) (Table 4). These multiple regression analyses revealed good power in the post hoc calculation (0.99; observed R2 = 0.4632[or = 0.5318], α = 0.05, total sample size = 53, and number of predictors = 9).
Multivariable regression analysis of the preoperative factors with postoperative KJLO
In the multivariate regression analysis, preoperative HKA was significant (Adjusted R2 = 0.186). This multiple regression analysis revealed good power in the post hoc calculation (0.87; observed R2 = 0.1896, α = 0.05, total sample size = 53, and number of predictors = 5). Our regression model also revealed that the preoperative HKA > – 9.8° predicted postoperative KJLO > 4°, when mMPTA, mLDFA, JLCA, and LDTA were our mean values. The preoperative mLDFA and JLCA scores were not correlated. Moreover, multivariate logistic regression analysis between the subgroups revealed no significant factors (Table 5).
Correlation between postoperative KJLO and TPS, PF alignment factors (CDI, PT)
There was no correlation between postoperative KJLO and TPS, CDI, or PT (Appendix Table).
Discussion
The main finding of this study was that increased postoperative KJLO was correlated with inferior PROMs, although excessively overcorrected knees were excluded. The preoperative decreased HKA (varus alignment) was defined as a risk factor for postoperative KJLO increase. The postoperative KJLO did not correlate with postoperative TPS, CDI, or PT. In the subgroup analysis, there was no significant difference in radiological parameters and PROMs.
Recently, excessive postoperative KJLO has received substantial attention [21, 23,24,25,26]. Studies indicated that pathological KJLO following MOWHTO leads to abnormal knee kinematics and joint incongruence [4, 6]. Excessive shear stress on the tibial articular cartilage was induced in the knee with KJLO > 5° in a three-dimensional finite element analysis model [5]. However, the correlation between postoperative KJLO and clinical outcomes after MOWHTO is not proven.
Many studies stated that a postoperative MPTA > 95° is associated with inferior clinical outcomes [1, 8]. A postoperative mMPTA > 95.2° would lead to an excessive KJLO increase [25]. Patients with postoperative KJLO > 4° had inferior KSS objective and functional scores in multivariable regression analysis [27]. In contrast, some studies indicated that postoperative mMPTA > 95° is not associated with inferior clinical outcomes [7, 21, 24] as compensatory changes would occur in the hip and ankle joints [7]. However, patients with overcorrection are at risk of experiencing lateral compartment pain [24].
Most studies that reported a negative effect of postoperative increased KJLO on clinical outcomes and survivorship included knees with overcorrection. Hence, it was challenging to determine whether these adverse outcomes were caused by excessive valgus alignment or increased KJLO. In this study, although postoperative overcorrection knees were excluded, an increased postoperative KJLO was correlated with an inferior JKOM total score and subscale of general health conditions. Clinical outcome evaluations differed based on the study. Many studies reported that an excessive KJLO was associated with clinical outcomes; “functional,” “sports activities,” “QOL,” and “mental health.” However, few studies reported a correlation between “pain” and “symptom.” Postoperative pain or stiffness is mainly associated with the lateral tibiofemoral compartment or patellofemoral compartment caused by excessive valgus overcorrection or patellar height change [9, 10, 28]. Shear stress caused by excessive KJLO may not cause these problems, although abnormal kinematics negatively influence function, sports activities, QOL, and mental health. The JKOM is a PROM that strongly reflects the Japanese lifestyle. Japanese people prefer postures such as sitting on their knees and rising from the floor to a standing position. Hence, kinematic change with increased KJLO may have resulted in inferior JKOM.
Previous studies have reported that increased postoperative KJLO was correlated with preoperative HKA, mLDFA, and JLCA [20, 21, 29]. The KJLO would increase after MOWHTO when surgeons corrected the femoral deformity or intra-articular deformity only with the tibia or due to a technical error resulting in excessive valgus overcorrection of the lower limb. In this study, only preoperative HKA was associated with postoperative KJLO, whereas mLDFA and JLCA were not. Moreover, in the multivariable logistic regression analysis, there was no correlation between the subgroups, whereas preoperative HKA tended to predict postoperative pathological KJLO. Preoperative decreased HKA with slightly varus mMPTA and slightly valgus mLDFA would be a risk factor for increased postoperative KJLO. The first reason was that we excluded postoperative excessive valgus HKA and performed a closed wedge osteotomy or DLO if a correction angle > 15°or postoperative MPTA > 95° was expected preoperatively. Few patients had preoperative excessive varus lower limb alignment, femoral varus deformity, or increased JLCA. The second reason could be due to soft-tissue laxity such as varus-valgus laxity. Several studies have reported that preoperative varus-valgus laxity caused over- or under-correction after HTO [30,31,32]. As the KL grade increases, the degree of deformity and soft-tissue laxity increases [33]. Ogawa et al. reported that varus laxity was associated with the deference between the preoperative and postoperative JLCA values [30]. Our results showed a higher tendency for the deference in the JLCA value in the pathological KJLO group than in the normal. To avoid correction errors, a varus-valgus stress radiograph was recommended to assess and classify soft-tissue laxity [31, 32]. However, we did not take a varus-valgus stress radiograph, so further studies are needed to investigate the soft-tissue laxity.
MOWHTO leads not only to coronal changes in the tibia but also to sagittal and axial changes in the proximal and distal tibia. These three-dimensional geometric changes may affect postoperative WBL formation [24], thereby influencing postoperative KJLO. However, there was no significant correlation between postoperative KJLO and TPS, CDI, or PT in this study, as compensation in the hip and ankle joints may have affected the results. Moreover, changes in sagittal and axial alignment should be studied further.
It is important to correct limb alignment at the center of rotational angulation (CORA) [34]. When a large correction with varus deformity of both the femur and tibia is necessary, DLO may be considered to avoid postoperative pathological KJLO. Recent studies indicated good clinical outcomes after DLO [23, 35,36,37]. In a long-standing HKA radiographic study with varus malalignment patients, two-thirds of the patients were corrected with isolated MOWHTO, and the others required DLO if postoperative mMPTA < 95° was target [3]. Nakayama et al. recommended DLO when mMPTA > 95° or KJLO > 5° was estimated after MOWHTO [5]. In a study comparing MOWHTO and DLO during 2 years of follow-up, KJLO changed from 1.4° to 6.3° postoperatively in the MOWHTO group, while it changed only from 1.0° to 1.3° in the DLO group [23]. Iseki et al. compared MOWHTO with DLO for severe varus malignment when preoperative HKA > -10°. They showed that DLO could prevent postoperative pathological joint line [36]. Our findings were similar to theirs. Preoperative HKA > – 9.8°was the cut-off value for postoperative KJLO > 4°, when preoperative mMPTA and mLDFA were within the range of normal value. Thus, DLO could be recommended for severe varus malalignment. However, there was no significant difference in the clinical outcomes between the MOWHTO and DLO groups. As DLO is more invasive and costly, further investigations regarding mid to long-term clinical outcomes are mandated [23].
This study had several limitations. First, it was a retrospective study with a short follow-up period. Second, the number of patients in the postoperative pathological KJLO group was small. However, post hoc analysis was powerful in detecting multiple regression analysis differences. Third, the cut-off value between postoperative pathological KJLO and preoperative radiological factors was not determined. Fourth, we did not fully investigate soft-tissue laxity. Fifth, patients who were older and had low activity levels were included which influenced clinical outcomes. Future studies should exclude such patients. The strengths of our study are as follows: we excluded patients with mechanical axis overcorrection, which represents a confounding factor often associated with increased KJLO and inferior clinical outcomes. Additionally, several radiological parameters were examined.
Conclusions
Increased KJLO after MOWHTO is associated with inferior clinical outcomes. Preoperative decreased HKA is a preoperative risk factor for increased postoperative KJLO. Hence, care of the CORA in the surrounding knee osteotomy is necessary to avoid postoperative increased KJLO. Further studies should investigate the effect of soft-tissue laxity.
Data availability
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
Abbreviations
- AJLO:
-
Ankle joint line obliquity
- CDI:
-
Carton-Deschamps index
- CORA:
-
Center of the rotational angulation
- DFO:
-
Distal femoral osteotomy
- HAA:
-
Hip abduction angle
- HKA:
-
Hip-knee-ankle
- JLCA:
-
Joint line convergent angle
- LDTA:
-
Lateral distal tibial angle
- MOWHTO:
-
Medial open-wedge high tibial osteotomy
- mLDFA:
-
Mechanical lateral distal femoral angle
- mMPTA:
-
Mechanical medial proximal tibial angle
- OA:
-
Osteoarthritis
- PROMs:
-
Patient-reported outcome measures
- PT:
-
Patella tilting angle
- TPS:
-
Tibial posterior slope
- WBLR:
-
Weight-bearing line ratio
- WOMAC:
-
Western Ontario McMaster Universities Arthritis Index
References
Schuster P, Geßlein M, Schlumberger M, Mayer P, Mayr R, Oremek D, Frank S, Schulz-Jahrsdörfer M, Richter J (2018) Ten-year results of medial open-wedge high tibial osteotomy and chondral resurfacing in severe medial osteoarthritis and Varus malalignment. Am J Sports Med 46:1362–1370. https://doi.org/10.1177/0363546518758016
Babis GC, An KN, Chao EY, Rand JA (2002) Double level osteotomy of the knee: a method to retain joint-line obliquity. J Bone Joint Surg Am 84:1380–1388. https://doi.org/10.2106/00004623-200208000-00014’
Feucht MJ, Winkler PW, Mehl J, Bode G, Forkel P, Imhoff AB, Lutz PM (2021) Isolated high tibial osteotomy is appropriate in less than two-thirds of varus knees if excessive overcorrection of the medial proximal tibial angle should be avoided. Knee Surg Sports Traumatol Arthrosc 29:3299–3309. https://doi.org/10.1007/s00167-020-06166-3
Amis AA (2013) Biomechanics of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21:197–205. https://doi.org/10.1007/s00167-012-2122-3
Nakayama H, Schröter S, Yamamoto C, Iseki T, Kanto R, Kurosaka K, Kambara S, Yoshiya S, Higa M (2018) Large correction in opening wedge high tibial osteotomy with resultant joint-line obliquity induces excessive shear stress on the articular cartilage. Knee Surg Sports Traumatol Arthrosc 26:1873–1878. https://doi.org/10.1007/s00167-017-4680-x
Wang D, Willinger L, Athwal KK, Williams A, Amis AA (2021) Knee joint line obliquity causes tibiofemoral subluxation that alters contact areas and meniscal loading. Am J Sports Med 49:2351–2360. https://doi.org/10.1177/03635465211020478
Goshima K, Sawaguchi T, Shigemoto K, Iwai S, Fujita K, Yamamuro Y (2019) Comparison of clinical and radiologic outcomes between normal and overcorrected medial proximal tibial angle groups after open-wedge high tibial osteotomy. Arthroscopy 35:2898-2908.e1. https://doi.org/10.1016/j.arthro.2019.04.030
Akamatsu Y, Nejima S, Tsuji M, Kobayashi H, Muramatsu S (2022) Joint line obliquity was maintained after double-level osteotomy, but was increased after open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 30:688–697. https://doi.org/10.1007/s00167-020-06430-6
Lee SS, So SY, Jung EY, Kim HJ, Lee BH, Wang JH (2019) Predictive factors for patellofemoral degenerative progression after opening-wedge high tibial osteotomy. Arthroscopy 35:1703–1710. https://doi.org/10.1016/j.arthro.2019.01.032
Yang JH, Lee SH, Nathawat KS, Jeon SH, Oh KJ (2013) The effect of biplane medial opening wedge high tibial osteotomy on patellofemoral joint indices. Knee 20:128–132. https://doi.org/10.1016/j.knee.2012.09.019
Hirschmann MT, Hess S, Behrend H, Amsler F, Leclercq V, Moser LB (2019) Phenotyping of hip–knee–ankle angle in young non-osteoarthritic knees provides better understanding of native alignment variability. Knee Surg Sports Traumatol Arthrosc 27:1378–1384. https://doi.org/10.1007/s00167-019-05507-1
So SY, Lee SS, Jung EY, Kim JH, Wang JH (2020) Difference in joint line convergence angle between the supine and standing positions is the most important predictive factor of coronal correction error after medial opening wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 28:1516–1525. https://doi.org/10.1007/s00167-019-05555-7
Doi T, Akai M, Fujino K, Hoshino Y, Iwaya T, Sunami Y (2010) Effect of nonsteroidal anti-inflammatory drug plasters for knee osteoarthritis in Japanese: a randomized controlled trial. Mod Rheumatol 20:24–33. https://doi.org/10.1007/s10165-009-0227-4
Tsuji T, Yoon J, Aiba T, Kanamori A, Okura T, Tanaka K (2014) Effects of whole-body vibration exercise on muscular strength and power, functional mobility and self-reported knee function in middle-aged and older Japanese women with knee pain. Knee 21:1088–1095. https://doi.org/10.1016/j.knee.2014.07.015
Miniaci A, Ballmer FT, Ballmer PM, Jakob RP (1989) Proximal tibial’ osteotomy A new fixation device. Clin Orthop Relat Res 246:250–259
Fujisawa Y, Masuhara K, Shiomi S (1979) The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin North Am 10:585–608. https://doi.org/10.1016/S0030-5898(20)30753-7
Staubli AE, de Simoni C, Babst R, Lobenhoffer P (2003) TomoFix: A new LCP-concept for open wedge osteotomy of the medial proximal tibia - Early results in 92 cases. Injury 34(Supplement 2):B55–B62. https://doi.org/10.1016/j.injury.2003.09.025
Takeuchi R, Ishikawa H, Aratake M, Bito H, Saito I, Kumagai K, Akamatsu Y, Saito T (2009) Medial opening wedge high tibial osteotomy with early full weight bearing. Arthroscopy 25:46–53. https://doi.org/10.1016/j.arthro.2008.08.015
Kanda Y (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48:452–458. https://doi.org/10.1038/bmt.2012.244
Hiramatsu K, Yamada Y, Nakamura N, Mitsuoka T (2022) Factors associated with postoperative knee joint line obliquity after medial open wedge high tibial osteotomy. Am J Sports Med 50:1651–1658. https://doi.org/10.1177/03635465221079343
Rosso F, Rossi R, Cantivalli A, Pilone C, Bonasia DE (2022) Joint line obliquity does not affect the outcomes of opening wedge high tibial osteotomy at an average 10-year follow-up. Am J Sports Med 50:461–470. https://doi.org/10.1177/03635465211059811
Cohen J, Cohen P, West SG, Aiken LS (2003) Applied multiple regression/ correlation analysis for the Behavioral Sciences. Lawrence Erlbaum Associates
Akamatsu Y, Kumagai K, Kobayashi H, Tsuji M, Saito T (2018) Effect of increased coronal inclination of the tibial plateau after opening-wedge high tibial osteotomy. Arthroscopy 34:2158-2169.e2. https://doi.org/10.1016/j.arthro.2018.01.055
Kim GW, Kang JK, Song EK, Seon JK (2021) Increased joint obliquity after open-wedge high tibial osteotomy induces pain in the lateral compartment: a comparative analysis of the minimum 4-year follow-up outcomes using propensity score matching. Knee Surg Sports Traumatol Arthrosc 29:3495–3502. https://doi.org/10.1007/s00167-020-06342-5
Kim JS, Lim JK, Choi HG, Jeong HW, Park SB, Shim SJ, Lee YS (2022) Excessively increased joint-line obliquity after medial opening-wedge high tibial osteotomy is associated with inferior radiologic and clinical outcomes: what is permissible joint-line obliquity. Arthroscopy 38:1904–1915. https://doi.org/10.1016/j.arthro.2021.11.004
Park JG, Han SB, Jang KM (2021) Association of preoperative tibial Varus deformity with joint line orientation and clinical outcome after open-wedge high tibial osteotomy for medial compartment osteoarthritis: A propensity score–matched analysis. Am J Sports Med 49:3551–3560. https://doi.org/10.1177/03635465211044146
Song JH, Bin SI, Kim JM, Lee BS (2020) What is an acceptable limit of joint-line obliquity after medial open wedge high tibial osteotomy? Analysis based on midterm results. Am J Sports Med 48:3028–3035. https://doi.org/10.1177/0363546520949552
Lee SS, Kim JH, Kim S, Jung EY, Ryu DJ, Lee DK, Wang JH (2022) Avoiding overcorrection to increase patient satisfaction after open wedge high tibial osteotomy. Am J Sports Med 50:2453–2461. https://doi.org/10.1177/03635465221102144
Oh KJ, Ko YB, Bae JH, Yoon ST, Kim JG (2016) Analysis of knee joint line obliquity after high tibial osteotomy. J Knee Surg 29:649–657. https://doi.org/10.1055/s-0036-1571430
Ogawa H, Matsumoto K, Ogawa T, Takeuchi K, Akiyama H (2016) Preoperative varus laxity correlates with overcorrection in medial opening wedge high tibial osteotomy. Arch Orthop Trauma Surg 136:1337–1342. https://doi.org/10.1007/s00402-016-2521-x
Kim JE, Kim DH, Lee JI, Choi HG, Jung YS, Lee SH, Lee YS (2021) Difference of preoperative varus-valgus stress radiograph is effective for the correction accuracy in the preoperative planning during open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 29:1035–1044. https://doi.org/10.1007/s00167-020-06076-4
Kim MS, Koh IJ, Sung YG, Park DC, Han SB, In Y (2021) Alignment adjustment using the valgus stress technique can increase the surgical accuracy of novice surgeons during medial opening-wedge high Tibial osteotomy. BMC Musculoskelet Disord 22:585. https://doi.org/10.1186/s12891-021-04475-3
Lee OS, Lee ES, Lee YS (2019) Disparity between preoperative target correction amount and postoperative correction amount in open wedge high tibial osteotomy. Knee Surg Relat Res 31:126–131. https://doi.org/10.5792/ksrr.18.034.10.5792/ksrr.18.034
Paley D (2002) Principles of deformity correction around the knee. Springer-Verlag. https://doi.org/10.1007/s001320050004
Iseki T, Onishi S, Kanto M, Kanto R, Kambara S, Yoshiya S, Tachibana T, Nakayama H (2021) Double-level osteotomy for severe varus osteoarthritic knees can prevent change in leg length and restore physiological joint geometry. Knee 31:136–143. https://doi.org/10.1016/j.knee.2021.04.011
Nakayama H, Iseki T, Kanto R, Kambara S, Kanto M, Yoshiya S, Schröter S (2020) Physiologic knee joint alignment and orientation can be restored by the minimally invasive double level osteotomy for osteoarthritic knees with severe varus deformity. Knee Surg Sports Traumatol Arthrosc 28:742–750. https://doi.org/10.1007/s00167-018-5103-3
Schröter S, Nakayama H, Yoshiya S, Stöckle U, Ateschrang A, Gruhn J (2019) Development of the double level osteotomy in severe varus osteoarthritis showed good outcome by preventing oblique joint line. Arch Orthop Trauma Surg 139:519–527. https://doi.org/10.1007/s00402-018-3068-9
Acknowledgements
The authors have no potential conflicts of interest, including financial interests, activities, relationships, and affiliations.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
KH and SO study design. KH collected the data, interpreted the data, and wrote the paper. KH data collection. All authors provided critical feedback and helped to shape the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no potential conflicts of interest, including financial interests, activities, relationships, and affiliations.
Ethical approval
The study protocol was approved by the Ethics Committee of Sapporo Medical University Hospital (Institutional Review board No. 3320-3064).
Informed consent
All patients involved in the study have received and approved an informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Horita, K., Okimura, S., Hamaoka, K. et al. Relationship between increased knee joint line obliquity after medial open-wedge high tibial osteotomy and patient-reported outcome measures. Arch Orthop Trauma Surg 144, 1751–1762 (2024). https://doi.org/10.1007/s00402-024-05203-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-024-05203-x