Abstract
Introduction
Intramedullary (IM) nailing is the treatment of choice for femoral shaft fractures, but nonunion rates have been reported to be as high as 12%. Surgical interventions for nonunion involve exchange nailing or plate augmentation. Recently, a combined treatment of exchange nailing and plate augmentation has demonstrated good results, but its comparative effectiveness remains unclear. This study aimed to compare the clinical and radiographic outcomes of three different surgical interventions for atrophic femoral shaft nonunion, and investigate the factors that affect bone healing after reoperation.
Materials and methods
A retrospective study was conducted at five university hospitals involving 149 patients with aseptic atrophic nonunion after IM nailing. These patients underwent reoperation with plate augmentation, exchange nailing, or combined treatment. Clinical and radiographic outcomes were assessed and compared according to reoperation procedure. Logistic regression analysis was performed to identify factors affecting persistent nonunion after reoperation.
Results
Of the cohort, 57 patients underwent plate augmentation, 64 underwent exchange nailing, and 28 received combined treatment. There were no significant differences in patient demographics among the groups. Exchange nailing produced a significantly lower union rate than did the combined treatment (82.8% vs. 100%, p = 0.016), whereas no significant difference was observed in the union rate and time to the union between plate augmentation and the combined treatment. Combined treatment showed the longest operative time and the greatest transfusion requirements. The risk factors for persistent nonunion included age, absence of autogenous bone grafts, and use of an exchange nailing technique.
Conclusions
Exchange nailing as a treatment for atrophic femoral shaft nonunion after IM nailing resulted in a lower union rate. The efficacy of the combined treatment requires further study, and persistent nonunion may be influenced by age, bone grafting, and surgical techniques. A comprehensive approach targeting both biological environment and mechanical stability is crucial in the treatment of atrophic femoral shaft nonunion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intramedullary (IM) nailing is the preferred treatment for femoral shaft fractures [1,2,3,4]. IM nailing can achieve indirect bone healing with minimal soft tissue disruption and preservation of blood supply to the fracture site and is resistant to axial compression and bending forces, resulting in high treatment success rates [3,4,5,6]. However, approximately 4.1–12% of nonunion cases after IM nailing in femoral shaft fractures have been recently reported [2, 7]. Exchange nailing or plate augmentation is the main surgical interventions recommended to treat nonunion after IM nailing [8, 9]. The type of nonunion (hypertrophic or atrophic) should be considered for treating nonunion. For atrophic nonunion caused by impaired vascularity at the fracture site, plate augmentation with autogenous bone grafting has produced better outcomes than did exchange nailing [10, 11]. Recently, a single-stage combined treatment of exchange nailing and plate augmentation has been utilized for treating atrophic femoral shaft nonunion with good results [12]; however, the differences in union rate and other clinical outcomes between the combined treatment and the other two interventions are unknown. Therefore, in this study, we aimed to compare the clinical and radiographic outcomes of exchange nailing, plate augmentation, and exchange nailing with plate augmentation for atrophic nonunion after IM nailing in femoral shaft fractures and to investigate the factors that affect bone healing after reoperation for femoral shaft atrophic nonunion.
Materials and methods
Study design and patient selection
The medical records of patients who developed atrophic nonunion after IM nailing for femoral shaft fractures and underwent plate augmentation, exchange nailing, or combined treatment between June 2011 and June 2021 at five university hospitals were analyzed retrospectively after receiving institutional review board approval. Informed consent was waived due to the retrospective nature of the study. Femoral shaft fractures were defined as fractures corresponding to the Orthopedic Trauma Association (OTA) classification 32 area [13]. Atrophic nonunion was defined using Weber and Cech's classification [14]. The inclusion criteria were age ≥ 18 years and skeletal maturity. The exclusion criteria were any procedure other than IM nailing at the time of the initial surgery, concomitant fractures beyond the shaft area (OTA 31 or 33), bilateral femoral fractures, skeletal immaturity, presence of neurovascular injury at the initial visit, pathologic fractures other than osteoporotic fractures, hypertrophic nonunion, septic nonunion, insufficient radiographic data, and a follow-up period of < 1 year.
Nonunion after the initial operation was defined as insufficient callus formation or a persistent fracture line observed in more than one cortices on anteroposterior (AP) and lateral femoral plain radiographs by 9 months postoperatively or failure of progressive bone healing based on consecutive plain radiographs for more than 3 months [15]. In patients diagnosed with nonunion, deep tissue cultures were performed from the nonunion site if a fracture-related infection was suspected based on medical history and clinical examination; patients were excluded from the study if culture results confirmed septic nonunion [16].
Surgical procedure and postoperative management protocol
Revision surgery was performed by six orthopedic trauma specialists with more than 10 years of experience. The revision procedures included plate augmentation, exchange nailing, or plate augmentation with exchange nailing, and the attending surgeon decided which procedure to perform for each patient. All reoperations were performed under C-arm guidance using a radiolucent table. For plate augmentation, a lateral incision was made on the center of the nonunion, and the nonunion site was exposed using a subvastus approach while leaving the existing IM nail in situ. Debridement and decortication of the nonunion site were performed, and a 4.5 mm locking compression plate (LCP, DePuy Synthes, West Chester, PA) was applied after autogenous cancellous iliac bone grafting. Bone grafting was not performed after debridement if the nonunion was limited to a single cortex and the size of the nonunion was minimal. During plate fixation, at least four cortices were fixed on each side of the fracture site, and if necessary, unicortical screws were used to avoid interference with the nail. For exchange nailing, the existing nail was removed, the medullary canal was reamed, and a nail with a diameter of 2 mm larger than that of the existing nail was inserted (Fig. 1). The attending surgeon determined the nail type, and all nails were statically locked. Bone grafting was performed selectively depending on the size of the bone defect at the nonunion site. In the combined plate augmentation and exchange nailing procedure, the existing nail was removed and replaced with a larger nail after reaming. Plate augmentation was performed using a lateral approach (Fig. 2). Bone grafting was performed according to the surgeon's assessment.
A, B Anteroposterior (AP) and lateral plain radiographs of a femoral shaft fracture corresponding to OTA 32-A3 in a 55-year-old male patient following a motorcycle accident. Intramedullary nailing was performed for the femoral shaft fracture. C, D AP and lateral radiographs at 9 months following the initial surgery. Atrophic nonunion with limited callus formation and persistent fracture gap is noted. E, F AP and lateral radiographs following reoperation for atrophic nonunion, which was addressed with exchange nailing. G, H AP and lateral radiographs obtained 14 months after exchange nailing. Note that while the callus formation has increased, cortical bridging has not occurred, and the fracture site gap is still visible
A, B Anteroposterior (AP) and lateral plain radiographs of a 40-year-old male patient who sustained a fall and developed a comminuted femoral shaft fracture corresponding to OTA 32-B3. Retrograde intramedullary nailing was performed for this fracture. C, D AP and lateral radiographs obtained 9 months after the initial surgery. A visible fracture gap and little amount of callus formation were observed. E, F AP and lateral radiographs after reoperation for atrophic nonunion. Atrophic nonunion was treated with a combination of exchange nailing and plate augmentation. G, H AP and lateral radiographs obtained 6 months after reoperation. Note the pronounced callus formation in all four cortices, with no visible fracture gap
Patients began range-of-motion exercises the day after surgery and partial weight-bearing with crutches or a walker within 1 week after surgery. Partial weight-bearing was gradually increased within the patient's pain-tolerable range. If the patient was judged to be able to walk independently, walking aids were removed, and full weight-bearing was permitted. There were no significant differences in postoperative rehabilitation protocols across the participating institutions. Patients were followed up at 1, 2, 3, 6, and 9 months and 1 year postoperatively and then at 6-month intervals thereafter. Plain radiographs of the femur were obtained at each follow-up.
Data collection and assessment of outcomes
Patients were divided into a plate augmentation group (Group P), exchange nailing group (Group N), and combined treatment group (Group C) according to the type of reoperation performed for the nonunion. Data on patients' age, sex, American Society of Anesthesiologists score, diabetes status, smoking status, body mass index, osteoporosis, the ambulatory level before reoperation, nonunion site, and follow-up time were collected. The nonunion sites were divided into isthmic and non-isthmic sites.
Data on initial trauma included injury mechanism, OTA fracture classification, open fractures, Gustilo-Anderson classification [17], and the type of IM nail used during the initial operation. The IM nail types were classified as antegrade and retrograde, and the antegrade nails were subdivided into standard interlocking or cephalomedullary according to the proximal fixation method. Reoperation data included the bone graft procedure and operative time.
Clinical outcomes included transfusion rate, transfusion volume, length of hospital stay, and ambulatory level at the final follow-up. Intraoperative and postoperative transfusions were performed. Postoperative transfusion was performed if the patient exhibited clinical symptoms or a hemoglobin level < 8 g/dL on examination, and hematological evaluations were routinely performed postoperatively at all participating institutions.
Radiographic outcomes included union, delayed union, and time to union. Union was defined as the presence of adequate callus bridging at the nonunion site in a minimum of three cortices on AP and lateral plain femur radiographs without the need for additional surgery after reoperation. Persistent nonunion was defined as the failure to achieve union after reoperation, requiring additional surgery [18, 19]. Delayed union was defined as the time to union exceeding 6 months among patients who achieved union.
Statistical analysis
Comparative analysis was performed among the three groups. For continuous variables, normality was tested using the Shapiro–Wilk test, and a one-way analysis of variance (ANOVA) was used when normality was satisfied. For non-parametric data, the Kruskal–Wallis test was used. Categorical variables were compared using the chi-square test or Fisher’s exact test. Logistic regression analysis was performed to identify the factors affecting persistent nonunion after reoperation for atrophic nonunion. Univariate analysis was performed to evaluate the association between candidate factors and persistent nonunion. Backward stepwise multivariate analysis was then performed using a threshold of P = 0.05 to enter and retain factors significantly associated with persistent nonunion in the model. Logistic regression analysis models were presented as odds ratios (OR) and 95% confidence intervals (95% CI). All statistical analyses were performed using SPSS (version 27.0; IBM Corp., Armonk, NY). Statistical significance was set at P < 0.05, and Bonferroni correction was applied where required.
Results
A total of 231 patients were identified, and 149 (104 male and 45 female patients) were included in the study after excluding 82 patients based on the exclusion criteria (7 with concomitant OTA 31 or 33 fractures, 3 with bilateral femoral shaft fracture, 4 with skeletal immaturity, 2 with initial neurovascular injury, 5 with septic nonunion, 12 with insufficient radiographic data, and 49 with follow-up < 1 year). The final cohort had a mean age of 52.7 years (range 20–88 years) and a mean follow-up of 39.9 months (range 12–207 months). Of the 149 patients, 57 were included in Group P, 64 in Group N, and 28 in group C. No significant differences were observed in patient demographics, comorbidities, ambulatory level before reoperation, nonunion site, or follow-up period between the three groups (Table 1). Also, no significant differences were observed in the mechanism of injury, OTA classification, open fractures, Gustilo-Anderson classification, and type of IM nail used among the three groups in the initial trauma analysis (Table 2).
Autogenous iliac bone grafting was performed in 46 patients (80.7%) in Group P, 6 (9.4%) in Group N, and 25 (89.3%) in Group C at the time of reoperation, with a significantly lower bone graft rate in Group N than in other groups (P < 0.001) (Table 3). The mean operative time was 127.9 ± 56.6 min in Group P, 139.4 ± 45.2 min in Group N, and 178.2 ± 50.8 min in Group C, with a significantly longer operative time in Group C than in other groups (P < 0.001).
Group C had a significantly higher transfusion rate of 64.3% than did Groups P (19.3%) and N (35.9%) (P < 0.001). The mean transfusion volume was also significantly higher in Group C (331.4 ± 403.6 ml) than Group P (140.4 ± 308.5 ml) and N (215.0 ± 403.4 ml) (P = 0.003). The mean length of stay was 15.4 days in Group P, 12.3 days in Group N, and 13.6 days in Group C, and no significant difference was observed among the three groups (P = 0.108). At the final follow-up, 37 patients (64.9%) in Group P, 50 patients (78.1%) in Group N, and 20 patients (71.4%) in Group C were able to walk independently, and there was no significant difference in the final ambulatory level and decline in the ambulatory level among the three groups (P = 0.434 and 0.820, respectively) (Table 3).
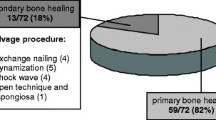
Radiographic union, delayed union, and time to union significantly differed among the three groups (P = 0.032, 0.033, and 0.023, respectively) (Table 3). Group P had a 91.2% union rate after reoperation, Group N had an 82.8% union rate, and Group C had a 100% union rate, with a significantly lower union rate in Group N than in Group C (P = 0.016). The rates of delayed union were 53.8%, 66.0%, and 35.7% in Groups P, N, and C, respectively, with significantly higher rates in Group N than in Group C (P = 0.001). The average time to union were 35.0, 42.5, and 31.7 weeks in Groups P, N, and C, respectively, with Group N exhibiting a significantly longer time to union than did Group C (P = 0.013). However, the radiographic outcomes were not significantly different between Groups P and C.
Logistic regression analysis of the effect of variables on the likelihood of persistent nonunion revealed that in the univariate logistic models, increasing age was associated with a higher risk of persistent nonunion. Patients who did not undergo autogenous bone grafting had a higher risk of persistent nonunion than did patients who received autogenous bone grafts, and patients who underwent exchange nailing had a higher risk of persistent nonunion than did patients who were treated with plate augmentation or combined treatment (age, OR = 1.09, 95% CI 1.02–1.17, P = 0.016; without bone graft, OR = 95.51, 95% CI 4.19–2179.2, P = 0.004; exchange nailing, OR = 115.76, 95% CI 4.01–3342.6, P = 0.006) (Table 4). Multivariate logistic models based on univariate predictors of persistent nonunion showed that age, absence of autogenous bone grafts, and exchange nailing all independently predicted persistent nonunion (age, OR = 1.08, 95% CI 1.03–1.13, P = 0.002; without bone graft, OR = 15.76, 95% CI 2.13–116.80, P = 0.007; exchange nailing, OR = 18.34, 95% CI 2.24–150.46, P = 0.007) (Table 4).
Discussion
In our study on reoperation for atrophic nonunion of the femoral shaft after IM nailing, exchange nailing demonstrated a significantly lower union rate than the combined treatment, whereas no significant difference was observed in the union rate and time to union between plate augmentation and combined treatment. Among the three procedures, the combined treatment had the longest operative time and necessitated more transfusions. Also, it showed a 100% union rate, the shortest mean time to union, and the lowest delayed union rate among the three groups.
High union rates and short union times have been reported in a previous study on combined treatment for femoral shaft nonunion, consistent with the results of this study, making it a promising treatment for nonunion [12]. Nevertheless, radiographic outcomes were not significantly different between the combined treatment and plate augmentation, and the combined treatment had the longest operative time and the highest transfusion volume among the three treatments. This suggests that the additional benefit of combined treatment for union may not be significant, with the trade-off being a longer operative time and greater blood loss.
Exchange nailing alone resulted in lower union rates than did exchange nailing with plate augmentation. Reaming at the time of exchange nailing decreases the endosteal blood supply but increases the periosteal blood supply, increasing in overall blood flow [20, 21]. However, in the case of atrophic nonunion, the increase in blood flow due to reaming was minimal because the periosteal blood supply at the fracture site was already impaired and may have contributed to the low union rate after exchange nailing in atrophic nonunion.
The risk factors for persistent nonunion were age, absence of bone graft, and exchange nailing. Fracture healing potency decreases, comorbidities increase with age, and osteoporosis can develop, affecting fracture occurrence and healing [22, 23]. In a previous study on risk factors for failure after revision femoral shaft nonunion, age was not reported as a risk factor; however, the study included both hypertrophic and atrophic nonunion and only included patients up to age 66 [18]. In our analysis, which focused on atrophic nonunion and included older patients, age was a risk factor for persistent nonunion, suggesting the importance of biological healing potency in atrophic nonunion. Autogenous iliac bone grafts possess osteoconductive, osteoinductive, and osteogenic properties and can effectively restore the impaired biological healing potency of atrophic nonunion [24,25,26]. In the multivariate analysis, the risk of persistent nonunion increased by more than 15-fold without bone grafting, indicating the importance of improving the biological environment to address atrophic nonunion.
Exchange nailing was also an independent risk factor for persistent nonunion after reoperation for atrophic femoral shaft nonunion. The IM nail is highly resistant to axial compression and bending forces but less resistant to torsional forces [6]. Previous studies on bone healing and instability in rats have reported that rotational instability adversely affects bone healing [27, 28]. In a human cadaveric biomechanical study, plate augmentation after femur IM nailing increased rotational stability by 3.3 times than by IM nailing alone [6]. Another biomechanical study that compared exchange nailing and plate augmentation using a synthetic femoral bone model showed that augmentation with a 4.5-mm LCP resulted in significantly less torsional displacement compared to that with nail exchange [29]. Taken together, these studies suggest the importance of increasing rotational stability from a biomechanical perspective to address nonunion after IM nailing and that plate augmentation is more favorable than is exchange nailing for increasing rotational stability. The risk factor analysis for persistent nonunion after reoperation for atrophic nonunion indicates that restoration of the biological environment and enhancement of mechanical stability, especially rotational stability, are important.
The risk factors for nonunion can be categorized into patient-related factors, fracture characteristics, surgery, and implant-related factors [30, 31]. Of the reported risk factors for nonunion, the majority were not identified as risk factors for persistent nonunion, with age being the only patient-related factor and other factors being surgery- and implant-related factors, such as bone graft status and exchange nailing. This suggests that the risk factors for regular nonunion and persistent nonunion after reoperation may differ, and that persistent nonunion may be driven more by surgery- and implant-related factors than by patient factors or initial fracture characteristics.
In this study, different types of IM nails were used during reoperation; they were intentionally selected to avoid overlap with the interlocking screw holes of previous IM nails and to increase the fixation stiffness. Lai et al. reported no difference in union rate and time to the union using different types of IM nails for reoperation of femoral shaft nonunion [10]. Therefore, the effect of the type of IM nail used during reoperation on the union rate may be minimal.
The limitations of this study include its retrospective nature and the potential for surgical bias owing to the participation of multiple surgeons. Due to the retrospective design, we were unable to collect patient-reported outcomes. Future prospective studies are needed to evaluate subjective patient outcomes following different treatments for atrophic nonunion. As for surgical bias, all surgeons were orthopedic trauma specialists, operated according to the principles of modern fracture management, and shared similar rehabilitation protocols; therefore, bias was likely to be minimal. We believe that the inclusion of multiple surgeons contributes to the generalizability of this study. Another limitation was that we were unable to measure other factors that may affect union, such as a quality of reduction or malalignment. Further research is needed to include other factors that may affect union. In addition, randomized studies are needed to have a better understanding of the effectiveness of combined treatment and the risk factors for a persistent nonunion.
In conclusion, exchange nailing as a treatment for atrophic femoral shaft nonunion demonstrated a lower union rate. The efficacy of the combined treatment requires further study. Persistent nonunion after reoperation may be influenced by age, bone grafting, and surgical technique. A comprehensive approach targeting both restoration of the biological environment and enhancement of mechanical stability should be considered in the treatment of atrophic femoral shaft nonunion.
Data availability
Data on this research are available from the corresponding author, K-CP, upon reasonable request.
References
Ricci WM, Gallagher B, Haidukewych GJ (2009) Intramedullary nailing of femoral shaft fractures: current concepts. J Am Acad Orthop Surg 17(5):296–305. https://doi.org/10.5435/00124635-200905000-00004
Ricci WM, Bellabarba C, Evanoff B, Herscovici D, DiPasquale T, Sanders R (2001) Retrograde versus antegrade nailing of femoral shaft fractures. J Orthop Trauma 15(3):161–169. https://doi.org/10.1097/00005131-200103000-00003
Wolinsky PR, McCarty E, Shyr Y, Johnson K (1999) Reamed intramedullary nailing of the femur: 551 cases. J Trauma 46(3):392–399. https://doi.org/10.1097/00005373-199903000-00007
Winquist RA, Hansen ST Jr, Clawson DK (1984) Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Jt Surg Am 66(4):529–539
Garnavos C (2017) Treatment of aseptic non-union after intramedullary nailing without removal of the nail. Injury 48(Suppl 1):S76-81. https://doi.org/10.1016/j.injury.2017.04.022
Park K, Kim K, Choi YS (2011) Comparison of mechanical rigidity between plate augmentation leaving the nail in situ and interlocking nail using cadaveric fracture model of the femur. Int Orthop 35(4):581–585. https://doi.org/10.1007/s00264-010-0983-y
Vaishya R, Agarwal AK, Gupta N, Vijay V (2016) Plate augmentation with retention of intramedullary nail is effective for resistant femoral shaft non-union. J Orthop 13(4):242–245. https://doi.org/10.1016/j.jor.2016.06.003
Hak DJ, Lee SS, Goulet JA (2000) Success of exchange reamed intramedullary nailing for femoral shaft nonunion or delayed union. J Orthop Trauma 14(3):178–182. https://doi.org/10.1097/00005131-200003000-00005
Bellabarba C, Ricci WM, Bolhofner BR (2001) Results of indirect reduction and plating of femoral shaft nonunions after intramedullary nailing. J Orthop Trauma 15(4):254–263. https://doi.org/10.1097/00005131-200105000-00004
Lai PJ, Hsu YH, Chou YC, Yeh WL, Ueng SWN, Yu YH (2019) Augmentative antirotational plating provided a significantly higher union rate than exchanging reamed nailing in treatment for femoral shaft aseptic atrophic nonunion - retrospective cohort study. BMC Musculoskelet Disord 20(1):127. https://doi.org/10.1186/s12891-019-2514-3
Çimen O, Öner A, Köksal A, Dırvar F, Mert M, Kargın D (2023) A comparison of exchange nailing and plate augmentation over a retained intramedullary nail in aseptic oligotrophic and atrophic femoral shaft pseudoarthrosis. Jt Dis Relat Surg 34(1):121–129. https://doi.org/10.52312/jdrs.2023.788
Khalifa AA, Fadle AA, Elsherif ME et al (2022) Concomitant intramedullary nailing and plate augmentation as a single-stage procedure in treating complicated nonunited femoral shaft fractures. Trauma 24(4):286–293. https://doi.org/10.1177/14604086211007037
Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF (2018) Fracture and dislocation classification compendium-2018. J Orthop Trauma 32(1 Suppl):1s–170s. https://doi.org/10.1097/bot.0000000000001063
Weber BG, Brunner C (1981) The treatment of nonunions without electrical stimulation. Clin Orthop Relat Res 161:24–32
Wittauer M, Burch MA, McNally M et al (2021) Definition of long-bone nonunion: a scoping review of prospective clinical trials to evaluate current practice. Injury 52(11):3200–3205. https://doi.org/10.1016/j.injury.2021.09.008
Govaert GAM, Kuehl R, Atkins BL et al (2020) Diagnosing fracture-related infection: current concepts and recommendations. J Orthop Trauma 34(1):8–17. https://doi.org/10.1097/bot.0000000000001614
Gustilo RB, Mendoza RM, Williams DN (1984) Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma 24(8):742–746. https://doi.org/10.1097/00005373-198408000-00009
Ru J-y, Chen L-x, Hu F-y et al (2018) Factors associated with development of re-nonunion after primary revision in femoral shaft nonunion subsequent to failed intramedullary nailing. J Orthop Surg Res 13(1):180. https://doi.org/10.1186/s13018-018-0886-y
Cone R, Roszman A, Conway Y, Cichos K, McGwin G, Spitler CA (2023) Risk factors for nonunion of distal femur fractures. J Orthop Trauma 37(4):175–180. https://doi.org/10.1097/bot.0000000000002553
Reichert IL, McCarthy ID, Hughes SP (1995) The acute vascular response to intramedullary reaming. Microsphere estimation of blood flow in the intact ovine tibia. J Bone Jt Surg Br 77(3):490–493
Greksa F, Tóth K, Boros M, Szabó A (2012) Periosteal microvascular reorganization after tibial reaming and intramedullary nailing in rats. J Orthop Sci 17(4):477–483. https://doi.org/10.1007/s00776-012-0222-z
Clark D, Nakamura M, Miclau T, Marcucio R (2017) Effects of aging on fracture healing. Curr Osteoporos Rep 15(6):601–608. https://doi.org/10.1007/s11914-017-0413-9
Nicholson JA, Makaram N, Simpson A, Keating JF (2021) Fracture nonunion in long bones: a literature review of risk factors and surgical management. Injury 52(2 Suppl):3s–11s. https://doi.org/10.1016/j.injury.2020.11.029
Jhunjhunwala HR, Dhawale AA (2016) Is augmentation plating an effective treatment for non-union of femoral shaft fractures with nail in situ? Eur J Trauma Emerg Surg 42(3):339–343. https://doi.org/10.1007/s00068-015-0534-8
Jones CB, Mayo KA (2005) Nonunion treatment: iliac crest bone graft techniques. J Orthop Trauma 19(10 Suppl):S11-13. https://doi.org/10.1097/00005131-200511101-00004
Myeroff C, Archdeacon M (2011) Autogenous bone graft: donor sites and techniques. J Bone Jt Surg Am 93(23):2227–2236. https://doi.org/10.2106/jbjs.J.01513
Grundnes O, Reikerås O (1993) Effects of instability on bone healing. Femoral osteotomies studied in rats. Acta Orthop Scand 64(1):55–58. https://doi.org/10.3109/17453679308994529
Mølster AO (1984) Effects of rotational instability on healing of femoral osteotomies in the rat. Acta Orthop Scand 55(6):632–636. https://doi.org/10.3109/17453678408992411
Walcher MG, Day RE, Gesslein M, Bail HJ, Kuster MS (2023) Augmentative plating versus exchange intramedullary nailing for the treatment of aseptic non-unions of the femoral shaf—a biomechanical study in a SawboneTM model. J Pers Med 13(4):650
Rupp M, Biehl C, Budak M, Thormann U, Heiss C, Alt V (2018) Diaphyseal long bone nonunions—types, aetiology, economics, and treatment recommendations. Int Orthop 42(2):247–258. https://doi.org/10.1007/s00264-017-3734-5
Quan K, Xu Q, Zhu M, Liu X, Dai M (2021) Analysis of risk factors for non-union after surgery for limb fractures: a case-control study of 669 subjects. Front Surg 8:754150. https://doi.org/10.3389/fsurg.2021.754150
Funding
No funding or other support was offered or received from any organization.
Author information
Authors and Affiliations
Contributions
C-WO, O-JS, Joon-Woo Kim, Ji-Wan Kim, and KTH contributed to the study conception and design. IK organized and interpreted the data, wrote the manuscript, and performed the statistical analysis. C-WO, O-JS, Joon-Woo Kim, Ji-Wan Kim, and KTH contributed in the revision process. K-CP conceptualized the study and participated in its design and helped to modify the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was obtained from the ethics committee of Hanyang university Guri hospital (Approval no.: 2023-02-030).
Informed consent
Informed consent was waived due to the retrospective study design.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kook, I., Oh, CW., Shon, OJ. et al. Comparing outcomes of plate augmentation, nail exchange, and nail exchange with plate augmentation in the treatment of atrophic femoral shaft nonunion after intramedullary nailing: a multicenter retrospective study. Arch Orthop Trauma Surg 144, 1259–1268 (2024). https://doi.org/10.1007/s00402-023-05183-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-05183-4