Abstract
Background
Tourniquet use during total knee arthroplasty (TKA) remains controversial. The purpose of this study is to determine the impact of tourniquet use only during cementation compared with its use throughout the entire surgery concerning early outcomes in functional recovery, pain, quadriceps function, and rehabilitation.
Methods
Between November 2019 and March 2020, 118 patients were enrolled in this study, with 59 patients undergoing TKA with a tourniquet during the entire surgery (group 1) and 59 patients with a tourniquet only during cementation (group 2). Twenty-eight patients were unable to complete follow-up leaving fifty in group 1 and forty in group 2. Primary endpoints were surgical time, postoperative knee and thigh pain, and functional recovery. Secondary endpoints were 6-month clinical scores and blood loss.
Results
Patients in group 1 had statistically significantly increased knee pain on postoperative day 3 (p = 0.004), and thigh pain on postoperative day 1 (p < 0.001), 2 (p < 0.001), and 3 (p = 0.027), and longer time intervals to achieve straight leg raise maneuver (p = 0.006) compared to group 2.
However, it did not affect overall narcotic consumption, knee pain (day 1–2), functional recovery, ROM, ability to do the first walk, Oxford knee score, length of stay, and complication rate.
There was no statistically significant difference in terms of 6-month postoperative knee score, surgical time, and blood loss between the two groups.
Conclusion
Tourniquet use diminishes quadriceps function and increases postoperative thigh pain and, to a lesser extent, knee pain. We, therefore, recommend the use of a tourniquet only during cementing.
Level of evidence
1; prospective randomized study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) is an effective treatment for end-stage knee osteoarthritis. In the United States, a vast majority of TKA are performed with a tourniquet but their use remains controversial [1]. Studies show that tourniquet use improves cement penetration depth, intraoperative visibility, may improve mid-term implant stability, decreases intraoperative blood loss, and surgical time [2,3,4,5,6,7,8,9,10,11]. However, some studies show that their eviction is associated with improved postoperative functional recovery, lower risks of thromboembolic complications, and less narcotic consumption [6, 8, 9, 12,13,14].
The literature is divisive on how tourniquet use during TKA can affect all of the abovementioned endpoints which motivated the current randomized control study.
The purpose of the study is to determine the impact in the early postoperative period of tourniquet just during cementation (8–12 min) compared with a tourniquet use during the entire surgery. Primary outcomes were surgical time, postoperative range of motion (ROM), pain, quadriceps function and functional recovery.
Our primary hypothesis was that the use of tourniquet during the entire surgery would increase postoperative pain and delay postoperative functional recovery as compared to tourniquet used only during cementation.
Material and methods
Patients
This prospective, randomized study was conducted at an academic hospital and was approved by the institution’s ethic committee.
Between November 2019 and March 2020, patient aged between 45 and 90 years with end-stage knee osteoarthritis of grade four according to Kellgren–Lawrence classification requiring unilateral TKA were considered eligible for this prospective study.
Exclusion criteria were patients (1) not willing and able to comply with follow-up requirements, (2) with chronic pain management issues, (3) neuromotor conditions, (4) loss to follow-up, (5) antecedent of knee arthrotomy and/or hardware implantation around the knee joint.
One hundred eighteen patients meeting study criteria were enrolled. Before the surgery, patients were randomized into two groups through a computer-randomization system.
Fifty-nine patients were included in group 1 (tourniquet during the entire surgery) and fifty-nine in group 2 (tourniquet only during component cementation).
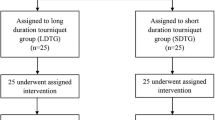
Twenty-eight patients were lost to follow-up. These patients were consequently excluded. Finally, 50 patients in group 1 and 40 patients in group 2 were eligible for the study (Fig. 1, flowchart). The high rate of loss to follow-up is explained by the COVID-19 pandemic. Following governments’ recommendations, many patients canceled their 6-month follow-up visit because of the virus outbreak.
Patients’ baseline characteristics were compared between the two groups.
Demographics included age and gender. Comorbidities comprised body mass index (BMI), diabetes, hypertension, and rheumatoid arthritis. Laboratory values included preoperative and postoperative hemoglobin (Hb) and hematocrit (Hc). Preoperative blood tests were done in the month preceding the surgery. Operative variables included tourniquet time, laterality, and type of anesthesia.
Primary endpoints were surgical time, postoperative knee and thigh pain, and functional recovery. Secondary endpoints were 6-month Oxford knee score (OKS) and blood loss.
Pain assessment
The pain was assessed by patient-controlled analgesia (PCA) morphine pump consumption 24 h after the surgery. Knee pain was also measured via visual analog scale (VAS) on 1–2–3 days, and 6 months after the surgery (0–10, with 10 being severe). Thigh pain was also documented.
Functional assessment
Passive range of motion (ROM) was assessed manually with a goniometer preoperatively and 1–2–3 days, and 6 months after the surgery.
The first walk, on day 1, with crutches was rated by one physiotherapist into four categories: easy, normal, difficult or impossible.
Time intervals for patients to achieve straight leg raise maneuver after the TKA, length of stay (LOS), and complications were also recorded.
Clinical scores
OKS (worst 0; best 48) was collected preoperatively and postoperatively at a follow-up of 6 months for every patient.
The difference in preoperative and postoperative Hb and Hc was used to evaluate blood loss.
Surgical technique
All operations were performed by two senior knee surgeons under general or spinal anesthesia.
A cruciate retaining mobile bearing, fully cemented TKA (Attune knee CR RP system DePuy Synthes, Warsaw, IN, USA) without patellar resurfacing was implanted through a medial subvastus approach for all cases.
The components were aligned following the mechanical alignment principles.
All patients received 1 g of IV TXA 30 min prior to the incision and intraoperative pericapsular local anesthetics injections. No nerve blocks were performed.
No suction drains were used.
After exsanguination of the leg, the tourniquet was either inflated before skin incision (group 1) or just before cementing the implant (group 2) and released before closing of the arthrotomy. The tourniquet was inflated to a pressure that was based on the systolic pressure value recorded (100 mmHg above the baseline systolic pressure).
The postoperative care included multimodal analgesia as a combination of acetaminophen, nonsteroidal anti-inflammatory agents, and tramadol.
A patient-controlled analgesia (PCA) morphine pump was placed for 24 h and the patient was trained to how to use it. The consumption was recorded. After removal of the PCA pump, the patient only received the above described multimodal analgesia. No other narcotics than tramadol were given.
With the guidance of one physiotherapist, patients were encouraged to perform exercises from day 1.
All patients received low-molecular-weight heparin at a prophylactic dose for 30 days following the surgery.
Follow-up
Clinical follow-up was done every day until their discharge from the hospital and at 6-month postoperative.
Participants, physiotherapist, statisticians, and the resident doctor in charge of the follow-up were blinded in order to enable unbiased collection and analysis of patient-reported and functional outcomes.
Statistical analysis
Descriptive statistical analysis was performed, and normality of the data was evaluated using the Kolmogorov–Smirnov test. Chi-square test was performed to compare differences between categorical variables. However, if more than 20% of cells have expected frequencies < 5, a Fisher’s exact test was performed. Continuous variables were compared using an independent t test or the Mann–Whitney U test. Ordinal variables were compared using a Mann–Whitney U test for independent samples. All statistical analyses were conducted using SPSS software (version 28.0.1.0; IBM Corp, Armonk, NY, USA).
Statistical significance was set at p < 0.05.
Results
Patients’ baseline characteristics were compared between the two groups (Table 1).
Except for the tourniquet time, there was no significant difference in terms of demographics, comorbidities, operative and preoperative values between the two groups.
Primary outcomes
Concerning postoperative pain, patients in group 1 (tourniquet during the entire surgery) had statistically significantly increased knee pain on postoperative day 3 (p = 0.004), and thigh pain on postoperative day 1 (p < 0.001), 2 (p < 0.001), and 3 (p = 0.027) compared to group 2 (tourniquet only during cementation). However, no significant difference in opioid consumption and knee pain on postoperative day 1–2 was observed (Table 2).
About functional outcomes, no statistically significant difference was found between the two groups in terms of ROM, ability to do the first walk, and LOS.
Time intervals for patients to achieve straight leg raise maneuver was significantly longer in group 1 (2.4 ± 1.2 days vs 1.8 ± 1 days, p = 0.006).
There was a trend but no statistically significant difference toward an easier first walk in group 2 (p = 0.055) (Table 3).
There was no significant difference regarding surgical time (56.9 ± 9.2 min in group 1 vs 55.4 ± 4.7 min in group 2, p = 0.297), and postoperative complications (6 in group 1 versus 4 in group 2, p = 0.294) between the groups.
Secondary outcomes
There was no statistically significant difference in terms of 6-month postoperative knee score (45.1 ± 4.4 vs 45.1 ± 3.6, p = 0.998), delta hematocrit (6.4 ± 3.2 vs 7.1 ± 2.9, p = 0.309), and delta hemoglobin (2 ± 1 g/dl vs 2.3 ± 0.9 g/dl, p = 0.074) between group 1 and 2, respectively (Table 4).
Discussion
This study was motivated by the lack of consensus and ongoing debates about the use of tourniquet for TKA. Articles with opposite conclusions can be found in the literature and authors disagree [2, 3, 13, 14].
The most important finding of this study was that limited use of a tourniquet could improve postoperative thigh pain and quadriceps function.
Diminished quadriceps strength is associated with tourniquet use for TKA [15, 16].
We came to a similar conclusion and our study showed that tourniquet has a statistically significant impact on the quadriceps. Indeed patients of group 2 were able to perform a straight leg raise maneuver earlier (group 1: 2.4 ± 1.2 days vs group 2: 1.8 ± 1 days) and had significantly less thigh pain on postoperative day 1–2–3 compared to group 1.
However, it did not affect overall narcotic consumption, postoperative range of motion, and ability to do the first walk. The latter keeps the tourniquet debate alive and invites us to question the benefit of not using it if the patient’s functional recovery is not compromised.
Some authors showed that the use of tourniquet was not associated with either early-stage pain or 1-year postoperative functional outcomes [17]. For others, the impact on postoperative pain and opioids is minimal [18]. Finally, some studies found no difference in pain and functional outcomes [19,20,21,22].
Regarding knee pain, there was no significant difference in postoperative knee pain on day 1–2 and opioid consumption. We found that long-duration tourniquet had significantly more knee pain on postoperative day 3. The latter could be explained by the increased patient activity (longer walk, improved ROM, stairs), and soft tissue swelling, solicitating the traumatized quadriceps.
But, to the contrary of what we expected to find, there was no significant difference in postoperative ROM, ability to walk, and OKS in this study’s dataset.
For many, using a tourniquet allows a better surgical field visualization [6, 7]. Therefore, we expected longer surgical time and higher blood loss in group 2. In our cohort, our hypothesis could not be validated. This could be explained by the use of TXA and local infiltration of analgesia, which significantly reduces intraoperative blood loss [23,24,25], therefore limiting the influence of the tourniquet between the groups.
The strengths of our study are its prospective randomized double-blinded design, its relatively large sample size, and large number of data collected. Furthermore, all patients were followed by the same resident doctor and physiotherapist on day 1–2–3 and 6-month postoperatively, both unaware of the patients’ group allocation.
Limitations of this study include the short follow-up (6 months); however, the aim of this study was to investigate the effects of a tourniquet on early postoperative pain and functional outcome. Second, in our study, the surgeons were experienced and the overall tourniquet and surgery time was short. Adverse effects of the long-duration tourniquet versus short-duration tourniquet might increase for more junior surgeons with longer surgical time. Third, this study’s design allows an analysis of the impact of the tourniquet on functional outcomes and pain. However, cement penetration depth, intraoperative visibility, mid-term implant stability, etc., were not addressed.
Lastly, all TKA were implanted using a medial subvastus approach which is quadriceps sparing. We believe that using a more traumatic approach might increase adverse effects of the tourniquet by summing muscle traumatism.
Conclusion
Tourniquet use increases postoperative thigh pain and diminishes quadriceps function. It also increased knee pain on postoperative day 3. However, it did not affect overall narcotic consumption, knee pain (day 1–2), functional recovery, ROM, ability to do the first walk, OKS, LOS, or complication rate.
In our opinion, any decrease in postoperative pain is beneficial for the patient’s rehabilitation process.
We, therefore, recommend limited use of tourniquet to be quadriceps sparing.
Data availability
The data that support the findings of this study are available from the corresponding authors upon reasonable request.
References
Berry DJ, Bozic KJ (2010) Current practice patterns in primary hip and knee arthroplasty among members of the american association of hip and knee surgeons. J Arthroplasty 25(6):2–4
Yi S, Tan J, Chen C, Chen H, Huang W (2014) The use of pneumatic tourniquet in total knee arthroplasty: a meta-analysis. Arch Orthop Trauma Surg 134(10):1469–1476
Migliorini F, Maffulli N, Aretini P, Trivellas A, Tingart M, Eschweiler J et al (2021) Impact of tourniquet during knee arthroplasty: a bayesian network meta-analysis of peri-operative outcomes. Arch Orthop Trauma Surg 141(6):1007–1023
Zak SG, Tang A, Pivec R, Meftah M, Austin MS, Schnaser E et al (2022) The effects of tourniquet on cement penetration in total knee arthroplasty. Arch Orthop Trauma Surg 143:2877–2884
Hegde V, Bracey DN, Johnson RM, Dennis DA, Jennings JM (2021) Tourniquet use improves cement penetration and reduces radiolucent line progression at 5 years after total knee arthroplasty. J Arthroplasty 36(7):S209–S214
Ejaz A, Laursen AC, Kappel A, Laursen MB, Jakobsen T, Rasmussen S et al (2014) Faster recovery without the use of a tourniquet in total knee arthroplasty. Acta Orthop 85(4):422–426
Goel R, Rondon AJ, Sydnor K, Blevins K, O’Malley M, Purtill JJ et al (2019) Tourniquet use does not affect functional outcomes or pain after total knee arthroplasty. J Bone Jt Surg 101(20):1821–1828
Ledin H, Aspenberg P, Good L (2012) Tourniquet use in total knee replacement does not improve fixation, but appears to reduce final range of motion. Acta Orthop 83(5):499–503
bin AbdRazak HR, Tan HCA (2014) The use of pneumatic tourniquets is safe in Asians undergoing total knee arthroplasty without anticoagulation. Knee 21(1):176–179
Hasanain MS, Apostu D, Alrefaee A, Tarabichi S (2018) Comparing the effect of tourniquet vs tourniquet-less in simultaneous bilateral total knee arthroplasties. J Arthroplasty 33(7):2119–2124
Alcelik I, Pollock RD, Sukeik M, Bettany-Saltikov J, Armstrong PM, Fismer P (2012) A comparison of outcomes with and without a tourniquet in total knee arthroplasty. J Arthroplasty 27(3):331–340
Rames RD, Haynes J, Hellman M, Barrack T, Barrack R (2020) Impact of tourniquet strategy on perioperative results of modern TKA. J Knee Surg 33(10):987–991
Zhang W, Li N, Chen S, Tan Y, Al-Aidaros M, Chen L (2014) The effects of a tourniquet used in total knee arthroplasty: a meta-analysis. J Orthop Surg Res 9(1):13
Tai TW, Lin CJ, Jou IM, Chang CW, Lai KA, Yang CY (2011) Tourniquet use in total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 19(7):1121–1130
Dennis DA, Kittelson AJ, Yang CC, Miner TM, Kim RH, Stevens-Lapsley JE (2016) Does tourniquet use in TKA affect recovery of lower extremity strength and function? A randomized trial. Clin Orthop Relat Res 474(1):69–77
Ayik O, Demirel M, Birisik F, Ersen A, Balci HI, Sahinkaya T et al (2021) The effects of tourniquet application in total knee arthroplasty on the recovery of thigh muscle strength and clinical outcomes. J Knee Surg 34(10):1057–1063
Çamur S, Bayram S, Kara A, Seçkin MF, Sağlam N, Batibay SG (2021) Tourniquet use does not affect pain and function after total knee arthroplasty: patient evaluation according to pain threshold. J Knee Surg 36:562–568
Zak SG, Yeroushalmi D, Long WJ, Meftah M, Schnaser E, Schwarzkopf R (2021) Does the use of a tourniquet influence outcomes in total knee arthroplasty: a randomized controlled trial. J Arthroplasty 36(7):2492–2496
Rathod P, Deshmukh A, Robinson J, Greiz M, Ranawat A, Rodriguez J (2014) Does tourniquet time in primary total knee arthroplasty influence clinical recovery? J Knee Surg 28(04):335–342
Bressi E, Longo UG, Mangiacapra F, Candela V, Berton A, Salvatore G et al (2020) Impact of tourniquet use on systemic inflammatory parameters, functional physical recovery, and cardiovascular outcomes of patients undergoing knee arthroplasty: a case–control study. J Knee Surg 33(08):762–767
Andrade MAP, Monte LFR, Lacerda GC, Dourado TR, Lei P, Abreu-e-Silva GM (2022) Are cementation quality and clinical outcomes affected by the use of tourniquet in primary total knee arthroplasty? Arch Orthop Trauma Surg 142(5):845–850
Smith AF, Usmani RH, Wilson KD, Smith LS, Malkani AL (2021) Effect of tourniquet use on patient outcomes after cementless total knee arthroplasty: a randomized controlled trial. J Arthroplasty 36(7):2331–2334
Schwab PE, Yombi J, Lavand’homme P, Thienpont E (2019) Comparison of local infiltration analgesia with single injection femoral nerve block in total knee arthroplasty. Acta Orthop Belg 85(1):122–129
Tzatzairis T, Drosos GI, Vogiatzaki T, Tilkeridis K, Ververidis A, Kazakos K (2019) Multiple intravenous tranexamic acid doses in total knee arthroplasty without tourniquet: a randomized controlled study. Arch Orthop Trauma Surg 139(6):859–868
Padala P, Rouholamin E, Mehta R (2010) The role of drains and tourniquets in primary total knee replacement—a comparative study of TKR performed with drains and tourniquet versus no drains and adrenaline and saline infiltration. J Knee Surg 17(01):24–27
Acknowledgements
We would like to acknowledge the essential collaboration of the physiotherapist involved in patient rehabilitation.
Funding
No financing was received for this study.
Author information
Authors and Affiliations
Contributions
Study design, BG, EM, and GB; data collection, DM and GB; data analysis, DM and GB; writing of manuscript, GB; editing of manuscript, BG, EM, DM, and GB; surgeons, BG and EM; revision and final approval of the manuscript BG, EM, DM, and GB.
Corresponding author
Ethics declarations
Conflict of interest
Bernard Geulette, Eric Manche, David Mazy, and Gautier Beckers: None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Beckers, G., Mazy, D., Manche, E. et al. Impact of tourniquet use in total knee arthroplasty on functional recovery and postoperative pain: a prospective study. Arch Orthop Trauma Surg 144, 1361–1367 (2024). https://doi.org/10.1007/s00402-023-05158-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-05158-5