Abstract
Purpose
To follow-up the non-operated hips of patients who underwent unilateral rotational acetabular osteotomy (RAO) for bilateral developmental dysplasia of the hip (DDH) for a minimum of 20 years to clarify (1) the timing of onset of hip osteoarthritis (OA) in DDH, and (2) factors associated with the development of OA.
Methods
This study included 92 non-operated hips of patients who underwent unilateral RAO for bilateral DDH. We examined the timing of OA onset and total hip arthroplasty (THA) and the joint survival rate in the studied hips. Furthermore, the patients were divided into those with OA onset (progression group) and those without OA onset and compared in terms of lateral center–edge angle (LCEA), sharp angle, acetabular head index (AHI), acetabular roof obliquity (ARO), joint congruity, and the presence or absence of OA progression on the RAO side.
Results
The progression group experienced OA onset 12 years after RAO and underwent THA 6 years after OA onset. The 20-year joint survival rate was 73% with the endpoint of OA onset and 81% with the endpoint of THA. The progression group had significantly smaller LCEA and AHI and larger ARO. The risk of developing OA was 8.2 times greater in patients with LCEA ≤ 7° than in those with LCEA > 7°.
Conclusion
The patients with OA progression group experienced OA onset at an average age of 55 years. A small LCEA (≤ 7°) was identified as a risk factor for the development of OA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Developmental dysplasia of the hip (DDH) is a known risk factor for the development of secondary hip osteoarthritis (OA) [1,2,3]. Recent large studies in Western populations have also demonstrated the association between hip OA and DDH. Rotterdam study [4] found a 4.3-fold increased risk of developing hip OA in patients with a lateral center–edge angle (LCEA) of < 25°, while CCHSIII study [5] demonstrated a correlation between CEA and joint space narrowing.
Various pelvic osteotomy techniques have been proposed for joint-preserving treatment of DDH [6,7,8]. Rotational acetabular osteotomy (RAO) has provided good long-term outcomes in patients followed for more than 20 years [9, 10], but has been associated with learning curve effects and the risk of complications [11]. Arthroscopic surgery for DDH has also been discussed in recent years, although some cases with poor outcomes have been reported [12, 13]. Many surgeons are therefore cautious about performing arthroscopic surgery alone for DDH.
Knowing the long-term course of untreated DDH is important for planning treatment strategies, including surgery. Despite its usefulness in predicting the development of OA, there have been few reports of long-term follow-up of DDH [14,15,16], and furthermore, these studies have limitations such as no description of the follow-up period, a short follow-up period of around 10 years, no stated definition of DDH, inclusion of elderly patients, and inclusion of patients with pre-existing OA changes. It also remains unclear when OA develops in patients with DDH and what the risk factors are for developing OA secondarily.
Thus, the objective of this study was to longitudinally follow the non-operated hips of patients who underwent unilateral RAO for bilateral DDH for a minimum of 20 years in order to clarify the following:
-
1.
the 20-year course of DDH (timing of OA onset), and
-
2.
factors associated with the development of OA.
Patients and methods
This retrospective study was approved by the ethics committee at our hospital. Informed consent was obtained by an opt-out approach.
Patients treated at Kanagawa Rehabilitation Hospital before 1999 who underwent unilateral RAO for bilateral DDH were included in this study, and their non-operated hips were the subjects of this study. The eligibility criteria were as follows: (1) LCEA as a measure of severity of DDH was ≤ 25°; (2) no pre-existing OA, defined as no symptoms at the start of follow-up and a Kellgren-Lawrence grade [17] of 0; and (3) patients who could be followed for at least 20 consecutive years after surgery. The exclusion criteria were as follows: (1) a history of surgery on the studied hip in childhood; (2) a history of prior RAO or THA; (3) a history of trauma, Perthes’ disease, skeletal dysplasia, or cerebral palsy; (4) distal transfer of the greater trochanter, femoral osteotomy, or muscle release simultaneously with RAO; or (5) RAO performed on the studied hip during the follow-up period.
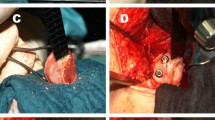
The following information was collected at the time of unilateral RAO defined as the baseline: age at surgery, sex, and studied side (left or right). In addition, an anteroposterior (AP) plain X-ray of the pelvis taken immediately before RAO was examined to determine the LCEA, Sharp angle, acetabular head index (AHI), acetabular roof obliquity (ARO), and joint congruity [18] of the studied hip. The pelvic AP X-rays were performed with the patient in supine, centered 2 finger breadth from the pubic symphysis, which was aligned to the center of the sacrum, at a distance of 110 cm from the X-ray film. And X-ray were taken at follow-up to determine whether OA had progressed on the RAO-treated side (Figs. 1 and 2). X-rays were also taken every one-two years over time after unilateral RAO to determine when OA developed and when THA was performed on the studied hip. For joint congruity, a Yasunaga’s classification [18] of “excellent” or “good” was defined as good congruity, and Yasunaga’s classification of “fair” or “poor” was defined as poor congruity (Fig. 2). The onset of OA was defined as a change in the Kellgren-Lawrence grade from 0 to 1 or higher.
92 hips were evaluated by 2 observers (HS: more than 40 years of experience, AA: more than 10 years of experience). In order to assess the interobserver reliability, intraclass correlation coefficient of LCEA, Sharp angle, AHI, ARO were measured in 20 randomly selected hips. The results were 0.86 (95% CI 0.74–0.95), 0.77 (95% CI 0.52–0.90), 0.81 (95% CI 0.60–0.92) and 0.74 (95% CI 0.42–0.89) respectively, suggesting a good interobserver reliability.
Statistics
Patients’ baseline characteristics are reported as the mean and standard deviation. For comparison, patients were divided into those with and those without OA onset in the studied hip during the follow-up period, referred to as the progression group and the non-progression group, respectively.
The Mann–Whitney U test was used to compare continuous variables, and the chi-square test was used to compare categorical variables. For multivariate analysis with the presence or absence of OA onset as the outcome variable, explanatory variables were selected by univariate analysis, and Cox proportional hazards regression analysis was performed to calculate the hazard ratio. For significant factors, the cutoff values for OA onset were determined by ROC analysis. The joint survival rate was estimated using the Kaplan–Meier method. All statistical analyses were performed with a significance level of 5% using JMP version 15.2 (SAS Institute, Cary, NC, USA).
Results
Of the 579 patients who underwent RAO at our hospital before 1999, 229 met the eligibility criteria for this study. When the exclusion criteria were applied, we excluded 11 patients with a history of surgery on the studied hip in childhood; six patients with a history of trauma, Perthes’ disease, skeletal dysplasia, or cerebral palsy; 96 patients who underwent transposition of the greater trochanter, femoral osteotomy, or muscle release simultaneously with RAO; and 24 patients who underwent RAO of the studied hip during the follow-up period. Thus, 92 patients were eventually included in the study (Fig. 3).
Mean age of the patients at the time of RAO was 42.7 ± 9.7 years. The mean follow-up period after RAO was 24.0 ± 3.7 years. There were 90 women and two men.
Postoperative course
There were 27 patients (29.3%) in the progression group and 65 (70.7%) in the non-progression group. The patients in the non-progression group were younger than those in the progression group (P = 0.005), while there were no significant differences in terms of sex ratio or laterality of the studied side (Table 1). The 27 patients in the progression group had OA onset at a mean of 11.7 ± 6.1 years after RAO, and 17 of them underwent THA at a mean of 5.7 ± 4.9 years after OA onset (15.8 ± 8.1 years after RAO).
The 10- and 20-year joint survival rates with the endpoint of OA onset were 83.7% (95% confidence interval (CI) 76–91) and 72.7% (95% CI 64–82), respectively (Fig. 4a), while those with the endpoint of THA were 86.9% (95% CI 80–94) and 81.0% (95% CI 73–89), respectively (Fig. 4b).
Radiographic evaluation
Significant differences were found between the progression and non-progression groups in LCEA, AHI, and ARO (Table 1). In the progression group, LCEA and AHI are significantly smaller (8.3 ± 12.4 degrees vs. 15.9 ± 5.6 degrees, P < 0.001, and 62.9 ± 11.3% vs. 69.6 ± 5.6%, P < 0.001, respectively), while ARO is significantly larger (17.9 ± 9.5 degrees vs. 12.6 ± 4.5 degrees, P < 0.001). There was no significant difference between the Sharp angles between the two groups (P = 0.142). Good joint congruity was seen in 11 patients in the progression group and 32 in the non-progression group, with no significant difference between the two groups (P = 0.46). OA progression in the RAO-treated hip occurred in 21 patients in the progression group and 31 in the non-progression group, which was a significant difference (P = 0.008) (Table 1).
Multivariate analysis
In Cox proportional hazards regression analysis of the factors that showed significant differences between the two groups (i.e., age, LCEA, AHI, and ARO) with the presence or absence of OA onset as the outcome variable, LCEA was identified as an independent risk factor (Table 2). By ROC analysis, the cutoff value of LCEA for OA onset was determined as LCEA ≤ 7° (R2 = 0.125, AUC = 0.666, P < 0.001). Estimation of HRs by Cox proportional hazards regression analysis showed that patients with LCEA ≤ 7° had an about 8.2 times higher risk of developing OA compared to those with LCEA > 7° (HR: 8.212, 95% CI 3.78–17.82, P < 0.001) (Table 2).
Discussion
DDH is a known risk factor for OA [1,2,3,4,5], and previous studies have reported that DDH is involved in 20–40% of OA cases [2, 3]. A Japanese multicenter study [19] showed that DDH was responsible for 80% of OA cases. However, it remains unclear what proportion of DDH patients develop OA, when DDH progresses to OA, and what factors predispose to OA. The present study attempted to clarify these issues through long-term follow-up of DDH.
The 10- and 20-year join survival rates with the endpoint of OA onset were 83.7% and 72.7%, respectively, while those with the endpoint of THA were 86.9% and 81.0%, respectively. To our knowledge, there are only two studies examining joint survival rate exclusively in DDH. Hisatome et al. [20] studied the non-operated hips of patients who underwent RAO and reported a 10-year joint survival rate of 92.9% with OA progression as the endpoint in 35 hips with pre-hip OA, with no hip requiring THA. Wyles et al. [21] studied 48 non-operated hips of patients who underwent unilateral THA with a Tönnis grade of 0 and reported 10- and 20-year joint survival rates of 96.0% and 67% with endpoints of Tönnis grade 3 or THA, respectively. The high 10-year survival rate reported by Hisatome et al. may have been due to the young age of the included patients (mean 38.2 years). Our results confirm previous reports of relatively good 10- and 20-year joint survival rates in DDH, and revealed that joint preservation can be expected in about 70% of DDH patients even after 20 years.
Next, we would like to discuss the general course of DDH. In the present study, the mean age of the patients at the start of follow-up was 43 years, and the mean follow-up period was 24 years. The results suggest that about 70% of asymptomatic DDH patients, which corresponded to the non-progression group in this study, do not develop OA until their late 60 s. In contrast, the patients in the progression group began to experience joint space narrowing after 12 years of follow-up and underwent THA in another six years. Thus, asymptomatic DDH patients who developed OA typically experienced OA onset around 55 years of age and underwent THA around 61 years on average. The age at which OA is most likely to occur has not been clarified. In terms of age of OA onset, a multicenter study of new outpatients in Japan [19] reported that the most common age at initial diagnosis of OA was 50–59 years (27%), followed by 60–69 years. The present study provides valuable data that the onset of radiological OA in DDH is most common around the age of 55 years. The results also suggest that even DDH patients can achieve joint preservation into their late 60 s if they do not develop OA.
From the above, the following question arises: which patients are more likely to develop OA? There are several reports on radiological indicators of DDH and development of OA (Table 3). Hasegawa et al. [14] studied 86 hips with pre- or early-stage hip OA with acetabular dysplasia or subluxation and found that in 39 pre-stage hips, LCEA, AHI, slope of acetabular roof, acetabular depth ratio were significantly smaller in those with subsequent OA progression, compared to those without OA progression. Jacobsen et al. [15] compared 81 DDH hips and 136 normal hips and found a correlation between LCEA and joint space narrowing. Wyles et al. [21] studied 48 hips that underwent unilateral THA for DDH with a Tönnis grade of 0 and identified LCEA < 25°, Tönnis angle > 8°, femoral head lateralization > 8 mm, femoral head extrusion index > 0.2, and acetabular depth-to-width index < 0.3 as risk factors for OA onset. Consistent with these reports, the present study also showed a significantly higher degree of DDH in the progression group, suggesting an association between the severity of DDH and the development of OA. Among the DDH indicators evaluated, LCEA was identified as an independent risk factor for OA onset, with patients with LCEA ≤ 7° having an about 8.2-fold increased risk of developing OA compared to those with LCEA > 7°.
Two explanations can be considered for the association between LCEA and the development of OA: one relating to the stress applied to the joint surfaces and the other to joint instability. Evidence has suggested that a reduced load transfer area in DDH may lead to premature degeneration of cartilage (1). Pompe et al. [22] reported that a smaller LCEA leads to a higher acetabular contact stress gradient and that a LCEA of less than 20° is associated with increased stress on the lateral acetabular rim. Other authors have also reported that smaller LCEA results in a correspondingly smaller joint surface area, which in turn increases joint stress [23]. Sato et al. [24] postulated that in DDH hips, greater component forces acting on the superior lateral aspect of the femoral head would induce instability of the femoral head. An evaluation of joint instability during gait using an accelerometer also demonstrated a correlation between the degree of instability and LCEA [25]. LCEA is a measure of the relative coverage of the femoral head by the acetabulum. Among several DDH indices, LCEA is the one that can adequately assess hip coverage and is the most influential factor in the development of OA.
The present results also suggest that DDH progression on the RAO-treated side predisposes to OA on the non-operated side. Unilateral RAO for bilateral DDH has been shown to provide adequate support on the operated side and reduce the burden on the non-operated side [20]. In other words, if the leg on the RAO-treated side has impaired function as a supporting leg, the burden on the non-operated side increases, resulting in the progression of OA on the non-operated side as well. Regular observation of the RAO-treated hip may allow for early detection of OA progression on the non-operated side. Even when the condition of the RAO-treated hip deteriorates, appropriate therapeutic intervention on the non-operated side may allow for joint preservation.
To determine whether RAO can prevent OA progression and THA, the survival rate of RAO itself was also investigated. Of the 92 hips that had RAO performed, 56 hips were graded as KL grade0 prior to surgery. Survival rate with OA progression as the endpoint were 84.0% (95% CI 74–94) and 55.4% (95% CI 42–68), respectively (Fig. 5a), which showed a significantly lower survival rate in the RAO group (Log-rank test, P = 0.02). With THA as the endpoint, the survival rates were 98.2% (95% CI 95–100) and 82.1% (95% CI 72–92) (Fig. 5b), respectively, which did not show a significant difference. From these results, RAO did not necessarily prevent OA progression. However, the survival rate for the RAO-treated sided was higher than the non-treated side up until 20 years, therefore RAO may be an effective method for prolonging survival until THA.
There are several limitations with this study. First, radiologic evaluation was performed using only AP plain radiographs of the pelvis. Unfortunately, the only images available for longitudinal follow-up from before RAO to the last observation point were the AP pelvic X-rays. However, X-rays can be taken at any medical facility immediately upon the initial presentation. Simply checking X-rays at initial presentation may therefore be a simple way to predict the development of OA and the prognosis of DDH. The second limitation is that this was a retrospective study. It is very difficult to prospectively follow patients with untreated DDH for a long period of time. We believe that the present study is valuable in that it is the only report of a longitudinal follow-up of exclusively DDH patients over a period of more than 20 years. Third, the study did not include a pain assessment. It is not possible to extract only OA-related pain from the medical record entries because the possibilities of lumbar spine disease or lesions outside the hip cannot be ruled out. Instead, relying solely on radiological evaluation allowed for objective assessment of OA. And finally, the current study is based on an Asian population. In Western countries, primary osteoarthritis is higher than in Asian countries. However, in the Asian population, the incidence of secondary osteoarthritis due to DDH is higher than in the Western population. This does not change the fact that DDH is a risk factor for osteoarthritis, but the age of onset and long-term survival may differ between the different population groups.
Conclusion
In patients with DDH, the joint survival rate with the onset of OA as the endpoint was 72.7% and Joint preservation can be expected in about 70% of DDH patients even after 20 years. However, DDH patients were most likely to develop OA around age 55 and LCEA ≤ 7° was a risk factor for the development of OA. RAO for DDH may be effective in buying time until THA, but patients with LCEA ≤ 7° are at high risk of developing OA and should be followed-up frequently.
Data availability
Data is available by the corresponding author.
Code availability
Not applicable.
References
Wiberg G (1939) Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteo-arthritis. Acta Chir Scand 83:5–135
Harris WH (1986) Etiology of osteoarthritis of the hip. Clin Orthop Relat Res 213:20–33
Murray RO (1965) The aetiology of primary osteoarthritis of the hip. Br J Radiol 38:810–824. https://doi.org/10.1259/0007-1285-38-455-810
Reijman M, Hazes JM, Pols HA, Koes BW, Bierma-Zeinstra SM (2005) Acetabular dysplasia predicts incident osteoarthritis of the hip: the Rotterdam study. Arthritis Rheum 52:787–793. https://doi.org/10.1002/art.20886
Jacobsen S, Sonne-Holm S, Søballe K, Gebuhr P, Lund B (2005) Hip dysplasia and osteoarthritis a survey of 4151 subjects from the Osteoarthrosis Substudy of the Copenhagen City Heart Study. Acta Orthop 76:149–158. https://doi.org/10.1080/00016470510030517
Ganz R, Klaue K, Vinh TS, Mast JW (1988) A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res 232:26–36
Ninomiya S, Tagawa H (1984) Rotational acetabular osteotomy for the dysplastic hip. J Bone Joint Surg Am 66A:430–436
Chiari K (1974) Medial displacement osteotomy of the pelvis. Clin Orthop Relat Res 98:55–71. https://doi.org/10.1097/00003086-197401000-00008
Yasunaga Y, Ochi M, Yamasaki T, Shoji T, Izumi S (2016) Rotational acetabular osteotomy for pre- and early osteoarthritis secondary to dysplasia provides durable results at 20 years. Clin Orthop Relat Res 474:2145–2153. https://doi.org/10.1007/s11999-016-4854-8
Kaneuji A, Sugimori T, Ichiseki T, Fukui K, Takahashi E, Matsumoto T (2015) Rotational acetabular osteotomy for osteoarthritis with acetabular dysplasia. Conversion rate to total hip arthroplasty within twenty years and osteoarthritis progression after a minimum of twenty years. J Bone Joint Surg Am 97A:726–732. https://doi.org/10.2106/JBJS.N.00667
Zaltz I, Baca G, Kim YJ, Schoenecker P, Trousdale R, Sierra R et al (2014) Complications associated with the periacetabular osteotomy: a prospective multicenter study. J Bone Joint Surg Am 96:1967–1974. https://doi.org/10.2106/JBJS.N.00113
McQuivey KS, Secretov E, Domb BG, Levy BA, Krych AJ, Neville M et al (2020) A multicenter study of radiographic measures predicting failure of arthroscopy in borderline hip dysplasia. Beware of the Tönnis angle. Am J Sports Med 48(7):1608–1615. https://doi.org/10.1177/0363546520914942
Shah A, Kay J, Memon M, Simunovic N, Uchida S, Bonin N et al (2020) Clinical and radiographic predictors of failed hip arthroscopy in the management of dysplasia: a systematic review and proposal for classification. Knee Surg Sports Traumatol Arthrosc 28:1296–1310. https://doi.org/10.1007/s00167-019-05416-3
Hasegawa Y, Iwata H, Mizuno M, Genda E, Sato S, Miura T (1992) The natural course of osteoarthritis of the hip due to subluxation or acetabular dysplasia. Arch Orthop Trauma Surg 111:187–191. https://doi.org/10.1007/BF00571474
Jacobsen S, Sonne-Holm S, Søballe K, Gebuhr P, Lund B (2005) Joint space width in dysplasia of the hip. A case-control study of 81 adults followed for ten years. J Bone Joint Surg Br 87B:471–477. https://doi.org/10.1302/0301-620X.87B4.15522
Murphy SB, Ganz R, Müller ME (1995) The prognosis in untreated dysplasia of the hip: a study of radiographic factors that predict the outcome. J Bone Joint Surg Am 77A:985–989. https://doi.org/10.2106/00004623-199507000-00002
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthritis. Ann Rheum Dis 16:494–502. https://doi.org/10.1136/ard.16.4.494
Yasunaga Y, Ikuta Y, Kanazawa T, Takahashi K, Hisatome T (2001) The state of the articular cartilage at the time of surgery as an indication for rotational acetabular osteotomy. J Bone Joint Surg Br 83:1001–1004. https://doi.org/10.1302/0301-620x.83b7.12171
Jingushi S, Ohfuji S, Sofue M, Hirota Y, Itoman M, Matsumoto T et al (2010) Multiinstitutional epidemiologic study regarding osteoarthritis of the hip in Japan. J Orthop Sci 15(5):626–631. https://doi.org/10.1007/s00776-010-1507-8
Hisatome T, Yasunaga Y, Tanaka R, Yamasaki T, Ishida O, Ochi M (2005) Natural course of the minimally symptomatic nonoperated hip in patients with bilateral hip dysplasia treated with contralateral rotational acetabular osteotomy. J Orthop Sci 10:574–580. https://doi.org/10.1007/s00776-005-0949-x
Wyles CC, Heidenreich MJ, Jeng J, Larson DR, Trousdale RT, Sierra RJ (2017) The John Charnley award: redefining the natural history of osteoarthritis in patients with hip dysplasia and impingement. Clin Orthop Relat Res 475:336–350. https://doi.org/10.1007/s11999-016-4815-2
Pompe B, Daniel M, Sochor M, Vengust R, Kralj-Iglič V, Iglič A (2003) Gradient of contact stress in normal and dysplastic human hips. Med Eng Phys 25:379–385. https://doi.org/10.1016/s1350-4533(03)00014-6
Iwasa M, Ando W, Uemura K, Hamada H, Takao M, Sugano N (2021) Pelvic incidence is not associated with the development of hip osteoarthritis. Bone Joint J 103B:1656–1661. https://doi.org/10.1302/0301-620X.103B11.BJJ-2021-0472.R1
Sato T, Tanino H, Nishida Y, Ito H, Matsuno T, Banks SA (2017) Dynamic femoral head translations in dysplastic hips. Clin Biomech 46:40–45. https://doi.org/10.1016/j.clinbiomech.2017.05.003
Maeyama A, Naito M, Moriyama S, Yoshimura I (2008) Evaluation of dynamic instability of the dysplastic hip with use of triaxial accelerometry. J Bone Joint Surg Am 90:85–92. https://doi.org/10.2106/JBJS.G.00029
Funding
The authors declare that no funds, grands, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
AA: Conceptualization, Resources, Investigation, Writing—original draft. HS: Resources, Project administration, Supervision. HT: Resources, Formal analysis. MS: Formal analysis, Writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
This retrospective study was approved by the ethics committee at Kanagawa Rehabilitation Hospital (krh-2020-23).
Consent to participate
Informed consent was obtained by an opt-out approach.
Consent to publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Amagami, A., Sugiyama, H., Tonotsuka, H. et al. Long-term course of developmental dysplasia of the hip: follow-up of the non-operated hips of patients undergoing unilateral rotational acetabular osteotomy for twenty-four years. Arch Orthop Trauma Surg 144, 997–1004 (2024). https://doi.org/10.1007/s00402-023-05140-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-05140-1