Abstract
Introduction
With the success of uncemented fixation in younger patients undergoing total hip arthroplasty and the growing demand for total knee arthroplasty (TKA) in a younger cohort of patients, there has been an increasing interest in cementless tibial baseplate fixation. We sought to determine whether there was a clear advantage to the use of three different forms of tibial baseplate fixation. The primary outcome of this study was survivorship and secondary outcomes were functional and radiological outcomes, up until 10 years.
Materials and methods
We conducted a randomised controlled trial and recruited 224 patients with 274 knees. Patients underwent TKA by a single surgeon utilising a standard surgical technique. All patients received a cruciate retaining TKA with a cementless femoral component, and were randomised to receive either a cemented tibial component, a pegged porous coated cementless tibial component with screws or a cementless tantalum monoblock tibial component with pegs. Patient reported outcome measures (PROMS), radiological data and survivorship were assessed until 10 years post-operatively.
Results
Pre-operative range of motion, alignment and PROMS were similar between the three groups. The use of cemented, cementless with screws or cementless with pegs fixation options, lead to differences in functional outcomes. There was greater improvement in the Oxford score and Knee Society Score in patients who received a cemented baseplate compared to tantalum and the pegged porous groups. However, radiological and survival outcomes were similar in all three groups. Overall survivorship was 99.6%, with one knee with cementless tibial fixation and screws revised for subsidence at 3 years. There were no cases of venous thromboembolism, periprosthetic fracture or infection.
Conclusions
Irrespective of tibial fixation method, functional and radiological outcomes remain similar at follow-up at 10 years, with no clear difference in outcome between each group. Each method of fixation also had excellent survivorship over this period and should reassure surgeons that whichever method of fixation they choose, long-term outcomes are likely to be satisfactory.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) has been shown to provide good function and pain relief for most patients with advanced arthritis of the knee. Consequently, TKA is being performed more frequently and on younger patients who have an expectation of a higher postoperative activity level. In this group, polyethylene wear and aseptic loosening of the tibial baseplate remains a concern and irrespective of patient demographics is the major cause of failure in TKA [28]. This has stimulated debate around the best option to minimise the likelihood of revision surgery.
Cementation of tibial baseplate fixation in TKA has been a reliable method of fixation in long term studies and confirmed by Australian joint registry data [18, 19, 26]. This technique provides the twin advantages of immediate fixation of the baseplate to the underlying bone [7] at a lower cost than their cementless counterparts which rely on bony ingrowth. However, radiostereometric studies have shown failure of cemented tibial baseplates in younger patients with baseplate migration and loosening due to bone resorption at the cement–bone interface leading to subsequent revision [22].
With the success of uncemented fixation in younger patients undergoing total hip arthroplasty and the growing demand for knee replacement in a younger cohort of patients, there has been an increasing interest in cementless tibial baseplate fixation [11, 12, 14, 25, 29]. Highly porous surfaces have been shown to promote bony ingrowth [3], and cementless fixation with components made from trabecular metal (a porous biomaterial made from tantalum) such as augments, sleeves and cones are commonly utilised in revision TKA. Their potential benefits include bone stock preservation, ease of use, a lower operating time, reduced micromotion and possibly improved long term survivorship when compared to cemented tibial components [16, 30]. In the past there has been some concerns with the design of cementless tibial components [6, 8] and reports of catastrophic early failure following baseplate fracture [8, 27]. The use of modular implants with the generation of added polyethylene debris from backside wear is a further issue that requires consideration. However, the belief that a cementless tibial baseplate will provide a long-term biological fixation with bony ingrowth remains an attractive prospect, in particular with implants utilising highly porous metals.
The primary goal of this study was to determine whether there was a clear survivorship advantage to the use of three different forms of tibial baseplate fixation including cemented, uncemented modular and uncemented monoblock at 10 years. The secondary outcomes were to assess any functional or radiological differences between the three groups.
Methods
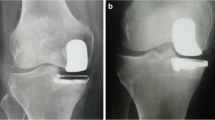
Between November 2005 to March 2012, 313 patients underwent TKA by a single surgeon and were recruited into a randomised controlled trial (RCT) to compare three different types of tibial baseplate fixation (Fig. 1). Each patient underwent a cruciate retaining (CR) TKA with a cementless femoral component (NexGen CR, Zimmer, Warsaw, IN, USA) with all patients having the patella resurfaced. Block randomisation was carried out with patients receiving one of three different tibial baseplates: Group 1 had a cemented tibial component (Zimmer, Warsaw, IN, USA), Group 2 received a pegged porous cementless tibial component coated with hydroxyapatite (HA) and fixed with four screws (Zimmer, Warsaw, IN, USA), and Group 3 received a cementless tantalum monoblock porous tibial component with two pegs (Zimmer, Warsaw, IN, USA). The patients were randomised and both patient and surgeon blinded as to which group each patient would be in, where an envelope was opened in the operating room immediately prior to surgery. Written informed consent was obtained from all the participants and the study was approved by an ethics committee.
Participants
Patients who agreed to participate in the study had knee osteoarthritis in either one or both knees with a clinically intact posterior cruciate ligament (PCL). Patients were not excluded based upon pre-operative deformity but were excluded if they had previous implants in situ, previous osteotomy, or lower limb neurological symptoms (such as Charcot arthropathy). Patients with inflammatory arthritis (such as rheumatoid arthritis) or diseases affecting bone quality (apart from cancer) were not excluded.
From 313 patients, 224 were included in the analysis with 89 being excluded due to incomplete data, death in the first 2 years or loss to follow-up. This left a population of 224 patients with 274 knees. There were 97 knees in Group 1, 87 in Group 2 and 90 in Group 3. Unilateral joint replacement was done in 175 knees (Group 1–67, Group 2—53 and Group 3–55) and bilateral (sequential) joint replacement was done in 49 knees (Group 1–16, Group 2–16, and Group 3–17).
Surgical methods
A standard tourniquet-less surgical technique was used, with a longitudinal midline incision and medial parapatellar approach. Navigation (Zimmer Orthosoft) was used in each case to position implants and achieve mechanical alignment with the femur cut at 90 degrees to the mechanical axis and three degrees of flexion, whilst the tibia was cut on zero degrees varus/valgus with a six degree posterior slope. If required, soft tissue releases were performed as follows: pie-crusting of the medial collateral ligament as necessary for knees with non-correctable varus; iliotibial band release from Gerdy’s tubercle in continuation with the fascia over tibialis anterior for knees with non-correctable valgus. The PCL was left intact. In all cases a cementless femoral component was used and the patella was resurfaced with an all-polyethylene component (Zimmer, Warsaw, IN, USA). Palacos bone cement (Heraeus Medical) was used for Group 1, whilst for Groups 2 and 3, CMW2 was utilised, where the only component cemented was the patella. Tibial component cement technique included applying cement first to the implant including the under surface as well as the central stem and then to the stem hole followed by insertion and impaction. Patients in Group 2 had a cementless baseplate inserted with the addition of four screws through the baseplate prior to polyethylene insertion and those in Group 3 had a cementless tantalum monoblock tibial baseplate with two pegs impacted until fully seated. When cement had cured, the final range, alignment and stability were recorded with navigation and the wound was closed in layers whilst in flexion. A waterproof dressing followed by a compression dressing was applied with the knee in extension. This was removed after 24 h and a fresh waterproof dressing applied if necessary. Drains were not utilised. The patient was mobilised under the supervision of physiotherapists from the day of surgery or the first postoperative day and discharge from hospital occurred when the patient’s function was considered satisfactory. Approximately half the cohort went directly home and the remainder to inpatient rehabilitation. Thromboprophylaxis was standardised utilising Enoxaparin 20 mg twice daily with those patients who had a history of venous thromboembolic disease or significant risk factors having Warfarin with a target INR of 2–2.5 until 6 weeks post-operatively. Patients were followed up at 2 weeks post-operatively for a wound check and then at 6 weeks and 3 months for clinical review.
Patient reported outcomes measures (PROMs)
Patient reported outcome measures (PROMS) were collected preoperatively and 1, 5 and 10 years after joint replacement. These questionnaires included the Oxford Knee Score (OKS), Knee Society Score (KSS) for Knee and Function, and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC).
Radiological assessment
Standing AP, lateral and skyline radiographs were taken at 6 weeks, 12 months, and 5 and 10 years and analysed by each author according to the Modern Knee Society Radiographic Evaluation System (Fig. 2) [20]. Those patients who were unable to attend for follow-up in person were contacted by telephone to collect PROMS and arrange radiographs.
Radiological assessment according to the modern knee society radiographic evaluation system [20]. Alpha (distal femoral valgus), gamma (femoral flexion), beta (tibial varus) or phi (tibial slope) angles
Statistical analysis
Descriptive data have been described as means and standard deviations (SD). Differences in demographical characteristics, PROMS and radiological evaluations at all timepoints were assessed using t tests and two-way analysis of variance (ANOVA). Regression analyses were utilized to assess cross-sectional and longitudinal associations between tibial baseplate fixation methods and study outcomes. Survival analyses were calculated using the Kaplan–Meier estimates. All statistical tests were two-sided and p < 0.05 were considered significant. All statistical analysis was conducted using Stata 17 (Stata Corp., College Station, TX, USA).
Power analysis
A total of 313 participants were recruited in the study. An ANOVA repeated measures test within–between interaction showed a patient count of 313 as being sufficient to detect a small effect (Table 1).
Results
At last review, 46 patients had died (18 in Group 1, 15 in Group 2, and 13 in Group 3) all of causes unrelated to their knee surgery. In terms of the differences between the groups, both median follow-up and gender distribution were significantly different. Median follow-up for Group 1 was 9.51 years (range 1.00–14.9), in Group 2 it was 7.27 years (range 1.10–15.2) and in Group 3 was 6.0 years (range 1–14). Overall median follow-up was 8.76 years (range 1–15.2) across all groups (Table 2) and the overall mean follow-up was 7.27 years (SD 3.03). In terms of gender, females, were more common in group 3 in comparison with group 1.
All participants were of similar age with normal BMI. There was no statistical difference in pre-operative range of motion or alignment between the groups. No differences in the PROMs pre-operatively were found and participants in group 1 had a lower Alpha angle in comparison with participants in group 2.
Patient reported outcomes (PROMS)
Tables 3 and 4 describe changes in PROMs from baseline to follow up in all the three groups. Oxford score improved overtime in all the groups, and the difference was statistically significant. Although participants in group 2 had highest delta for KSS scores, and statistically significant differences were found in all groups. At the end of 10 years of follow-up, improvement in WOMAC scores and KSS function was noted in all groups; however, a limited number of participants completed pre and post-surgery KSS questionnaires..
After data were stratified by gender, men who received Tantalum pegs were found to have poorer pre-operative Oxford scores (β: 4.60, p = 0.02) than women. Ten years after surgery there was a significant improvement in the Oxford score of the men (β: − 5.10, p = 0.005); however, no such change in scores were seen in women.
Radiological
Radiographs were assessed utilizing the Modern Knee Society Radiographic Evaluation System [20]. There were no significant differences between groups in the alpha (distal femoral valgus), gamma (femoral flexion), beta (tibial varus) or phi (tibial slope) angles with the standard deviations being very small as would be expected. Computer navigation was utilized with a consistent attempt to achieve mechanical alignment in all cases (Table 5). There were no differences noted in zonal osteolysis between each of the groups nor was there detection of any radiolucent lines. Furthermore, cross-sectional analysis demonstrated that alpha was higher in Group 2. This association remained significant after adjusting for age, sex and body mass index (β: 0.60, p < 0.01). However, at the end of 10 years this association was no longer significant (β: 0.58, p < 0.10).
Survivorship
Overall survivorship was 99.6% with one knee requiring revision for aseptic loosening of the tibial baseplate. There was no significant difference in survivorship between the three groups (Fig. 3). At the end of 10 years, cumulative survivorship was 88% taking into account those patients who were lost to follow up, revision TKA and mortality. Out of 274 knees, 247 completed the study and 27 were lost to follow up.
Complications
One patient required a revision performed at 3 years. The patient was from Group 2 (Fig. 5) and was revised for subsidence at 3 year post-primary TKA. The baseplate was revised from an uncemented prosthesis with screws to a cemented tibial baseplate, without further complication at 5 year post-revision at the time of this publication. None of the femoral components required revision.
Discussion
Our study reports functional, radiological and survival data for three different methods of tibial baseplate fixation over 10 years. The use of cemented, cementless with screws or cementless with pegs fixation options, lead to differences in functional outcomes. However, radiological and survival outcomes were similar in all the groups: there were no difference in zonal osteolysis or the development of radiolucent lines; overall survivorship was 99.6%, with one knee in Group 2 with cementless fixation and screws being revised to a cemented tibial baseplate for bony subsidence and aseptic loosening, as shown in Fig. 4. As such there was no clear difference in either primary or secondary outcomes as to which of the three groups performed better at 10 years.
There are few similar RCTs published in the literature, most reporting no significant differences between each type of fixation [2, 9, 10, 15, 17, 22]. Meta-analyses comparing cemented and cementless TKA have shown similar outcomes between the two types of fixation methods, but a trend toward better all-cause survivorship in cementless TKA [13, 21]. Of the 12 studies included in these two meta-analyses, only two followed patients for 10 years or more, which is a clear difference between our study as compared to others in the literature. In a recent comparative study of 109 knees by Pacoret et al. [24], patients were allocated to either a cementless or cemented tibial component. Contrary to our results, the survivorship of the cementless group was higher at 100% and was 97.1% in the cemented group at approximately 8 years.
Despite the above studies and meta-analyses revealing little difference between fixation types, registry data from both Australia and New Zealand registries shows superior outcomes for cemented prostheses [1, 23]. The Australian Orthopaedic Association National Joint Replacement Registry has shown that both all-cemented and hybrid methods of fixation have a lower revision rate than cementless fixation at both 10 and 19 years, (10 years: 4.4% and 4.5% vs 6.0%, respectively; 19 years: 7.9% and 7.9% vs 10.3%, respectively).
Evidence of loosening on radiographic analysis did not show any difference between methods of fixation in our study. However, the literature shows mixed results on this outcome with some studies describing higher rates of radiographic loosening in cementless groups [9, 25], whilst others reporting higher rates amongst cemented prostheses [17, 22, 24].
Greater improvement in PROMs was found in all groups. Unadjusted analyses showed that over the period of 10 years, patients Oxford, WOMAC, KSS scores improved and were statistically significant. Although an improvement was noted in the KSS function, the number of participants in these analyses was low. On adjusting the data, these differences were no longer significant. However, in men, there was a significant improved noted in the Oxford score postoperatively. This association was not found in women. Most published studies have demonstrated no difference in PROMS [2, 5, 9, 10, 15, 21, 22]. Conversely, some studies do show statistically significant differences in PROMS favouring cementless fixation; however, this difference is not clinically significant [4, 13, 17, 24]. In this study, statistical differences were found in scores evaluating pain and function.
A limitation of our study was the number of patient’s recruited but not included in the final analysis, either due to incomplete data, death or being lost to follow-up. These patients totaled just under 30% of the initial patient population and is likely in part a result of the patient’s age at the commencement of the study. Another limitation of the study was that median follow-up time and gender distribution were significantly different between the three groups of patients. The strengths of our trial were that it was conducted at a single institution by the same surgeon, with a standardized surgical technique. We believe this led to a significantly better survivorship as compared to other similar studies. With larger numbers, we may have been able to demonstrate statistical significance in PROMS between patients who received a cemented or tantalum peg baseplate as compared to those who received one with HA coating and screws.
Conclusion
This RCT has shown that irrespective of tibial fixation method, functional and radiological outcomes remain similar up to 10 years. Each method of fixation had excellent survivorship over this period and should reassure surgeons that whichever method of fixation they choose, long-term outcomes are likely to be satisfactory.
Data availability
All data used in this study was included in the manuscript.
References
AOA (2020) Australian Orthopaedic Association National Joint Replacement Registry. Annual Report 2020(ed)^(eds). AOA, Adelaide, Australia
Baker PN, Khaw FM, Kirk LM, Esler CN, Gregg PJ (2007) A randomised controlled trial of cemented versus cementless press-fit condylar total knee replacement: 15-year survival analysis. J Bone Jt Surg Br 89(12):1608–1614
Barrack RL, Nakamura SJ, Hopkins SG, Rosenzweig S (2004) Winner of the 2003 James A. Rand Young Investigator’s Award. Early failure of cementless mobile-bearing total knee arthroplasty. J Arthroplasty 19(7 Suppl 2):101–106
Bassett RW (1998) Results of 1,000 Performance knees: cementless versus cemented fixation. J Arthroplasty 13(4):409–413
Beaupre LA, al-Yamani M, Huckell JR, Johnston DW (2007) Hydroxyapatite-coated tibial implants compared with cemented tibial fixation in primary total knee arthroplasty. A randomized trial of outcomes at five years. J Bone Jt Surg Am 89(10):2204–2211
Bloebaum RD, Bachus KN, Mitchell W, Hoffman G, Hofmann AA (1994) Analysis of the bone surface area in resected tibia. Implications in tibial component subsidence and fixation. Clin Orthop Relat Res 309:2–10
Cawley DT, Kelly N, McGarry JP, Shannon FJ (2013) Cementing techniques for the tibial component in primary total knee replacement. Bone Jt J 95-B(3):295–300
Chatterji U, Ashworth MJ, Smith AL, Brewster N, Lewis PL (2005) Retrieval study of tibial baseplate fracture after total knee arthroplasty. J Arthroplasty 20(1):101–107
Choy WS, Yang DS, Lee KW, Lee SK, Kim KJ, Chang SH (2014) Cemented versus cementless fixation of a tibial component in LCS mobile-bearing total knee arthroplasty performed by a single surgeon. J Arthroplasty 29(12):2397–2401
Dunbar MJ, Wilson DA, Hennigar AW, Amirault JD, Gross M, Reardon GP (2009) Fixation of a trabecular metal knee arthroplasty component. A prospective randomized study. J Bone Jt Surg Am 91(7):1578–1586
Fernandez-Fairen M, Hernandez-Vaquero D, Murcia A, Torres A, Llopis R (2013) Trabecular metal in total knee arthroplasty associated with higher knee scores: a randomized controlled trial. Clin Orthop Relat Res 471(11):3543–3553
Fricka KB, Sritulanondha S, McAsey CJ (2015) To cement or not? Two-year results of a prospective, randomized study comparing cemented vs. cementless total knee arthroplasty (TKA). J Arthroplasty 30(9 Suppl):55–58
Hu B, Chen Y, Zhu H, Wu H, Yan S (2017) Cementless porous tantalum monoblock tibia vs cemented modular tibia in primary total knee arthroplasty: a meta-analysis. J Arthroplasty 32(2):666–674
Kamath AF, Lee GC, Sheth NP, Nelson CL, Garino JP, Israelite CL (2011) Prospective results of uncemented tantalum monoblock tibia in total knee arthroplasty: minimum 5-year follow-up in patients younger than 55 years. J Arthroplasty 26(8):1390–1395
Kim YH, Park JW, Lim HM, Park ES (2014) Cementless and cemented total knee arthroplasty in patients younger than fifty five years. Which is better? Int Orthop 38(2):297–303
Laende EK, Richardson CG, Dunbar MJ (2019) Predictive value of short-term migration in determining long-term stable fixation in cemented and cementless total knee arthroplasties. Bone Jt J 101-B(7_Supple_C):55–60
Lizaur-Utrilla A, Miralles-Munoz FA, Lopez-Prats FA (2014) Similar survival between screw cementless and cemented tibial components in young patients with osteoarthritis. Knee Surg Sports Traumatol Arthrosc 22(7):1585–1590
Lombardi AV Jr, Berasi CC, Berend KR (2007) Evolution of tibial fixation in total knee arthroplasty. J Arthroplasty 22(4 Suppl 1):25–29
Long WJ, Bryce CD, Hollenbeak CS, Benner RW, Scott WN (2014) Total knee replacement in young, active patients: long-term follow-up and functional outcome: a concise follow-up of a previous report. J Bone Joint Surg Am 96(18):e159
Meneghini RM, Mont MA, Backstein DB, Bourne RB, Dennis DA, Scuderi GR (2015) Development of a modern knee society radiographic evaluation system and methodology for total knee arthroplasty. J Arthroplasty 30(12):2311–2314
Newman JM, Sodhi N, Dekis JC et al (2020) Survivorship and functional outcomes of cementless versus cemented total knee arthroplasty: a meta-analysis. J Knee Surg 33(3):270–278
Nilsson KG, Karrholm J, Carlsson L, Dalen T (1999) Hydroxyapatite coating versus cemented fixation of the tibial component in total knee arthroplasty: prospective randomized comparison of hydroxyapatite-coated and cemented tibial components with 5-year follow-up using radiostereometry. J Arthroplasty 14(1):9–20
NZOA (2019) The New Zealand Joint Registry Twenty-One Year Report (ed)^(eds). NZOA, Christchurch
Pacoret V, Kalk E, Labattut L, Girardot G, Baulot E, Martz P (2020) Survival rate of cemented versus cementless tibial component in primary total knee arthroplasty over 5 years of follow-up: comparative study of 109 prostheses. SICOT J 6:36
Park JW, Kim YH (2011) Simultaneous cemented and cementless total knee replacement in the same patients: a prospective comparison of long-term outcomes using an identical design of NexGen prosthesis. J Bone Joint Surg Br 93(11):1479–1486
Ritter MA, Keating EM, Sueyoshi T, Davis KE, Barrington JW, Emerson RH (2016) Twenty-five-years and greater, results after nonmodular cemented total knee arthroplasty. J Arthroplasty 31(10):2199–2202
Scully WF, Deren ME, Bloomfield MR (2019) Catastrophic tibial baseplate failure of a modern cementless total knee arthroplasty implant. Arthroplast Today 5(4):446–452
Sharkey PF, Lichstein PM, Shen C, Tokarski AT, Parvizi J (2014) Why are total knee arthroplasties failing today–has anything changed after 10 years? J Arthroplasty 29(9):1774–1778
Unger AS, Duggan JP (2011) Midterm results of a porous tantalum monoblock tibia component clinical and radiographic results of 108 knees. J Arthroplasty 26(6):855–860
van Hamersveld KT, Marang-van de Mheen PJ, Tsonaka R, Valstar ER, Toksvig-Larsen S (2017) Fixation and clinical outcome of uncemented peri-apatite-coated versus cemented total knee arthroplasty : five-year follow-up of a randomised controlled trial using radiostereometric analysis (RSA). Bone Jt J 99-B(11):1467–1476
Funding
The authors did not receive support or funding from any organization for the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial conflicts of interests to disclose.
Ethical approval
The authors obtained ethics approval for this study from the Northern Sydney Local Health District Human Research Ethics Committee, and written informed consent was obtained from all the participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Awwad, G.E.H., Ahedi, H., Angadi, D. et al. A prospective randomised controlled trial of cemented and uncemented tibial baseplates: functional and radiological outcomes. Arch Orthop Trauma Surg 143, 5891–5899 (2023). https://doi.org/10.1007/s00402-023-04831-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04831-z