Abstract
Introduction
Discoid lateral meniscus (DLM) is an anatomic knee variant associated with increased tears and degeneration. This study aimed to quantify meniscal status with magnetic resonance imaging (MRI) T2 mapping before and after arthroscopic reshaping surgery for DLM.
Materials and methods
We retrospectively reviewed the records of patients undergoing arthroscopic reshaping surgery for symptomatic DLM with ≥ 2-year follow-up. MRI T2 mapping was performed preoperatively and at 12 and 24 months postoperatively. T2 relaxation times of the anterior and posterior horns of both menisci and of the adjacent cartilage were assessed.
Results
Thirty-six knees from 32 patients were included. The mean age at surgery was 13.7 years (range 7–24), and the mean follow-up duration was 31.0 months. Saucerization alone was performed on five knees and saucerization with repair on 31 knees. Preoperatively, the T2 relaxation time of the anterior horn of the lateral meniscus was significantly longer than that of the medial meniscus (P < 0.01). T2 relaxation time significantly decreased at 12 and 24 months postoperatively (P < 0.01). Assessments of the posterior horn were comparable. The T2 relaxation time was significantly longer in the tear versus non-tear side at each time point (P < 0.01). There were significant correlations between the T2 relaxation time of the meniscus and that of the corresponding area of the lateral femoral condyle cartilage (anterior horn: r = 0.504, P = 0.002; posterior horn: r = 0.365, P = 0.029).
Conclusions
The T2 relaxation time of symptomatic DLM was significantly longer than that of the medial meniscus preoperatively, and it decreased 24 months after arthroscopic reshaping surgery. The meniscal T2 relaxation time of the tear side was significantly longer than that of the non-tear side. There were significant correlations between the cartilage and meniscal T2 relaxation times at 24 months after surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Discoid lateral meniscus (DLM) is a congenital anatomical knee variant [1]. In a histomorphologic study, Papadopoulos showed that in DLM, the circular collagen network is markedly less organized than a normal meniscus. This means a higher probability of tearing injuries and degeneration [2]. Because the residual meniscus tissue is abnormal, total and subtotal meniscectomy are the standard surgical treatment [3,4,5]. The long-term surgical outcomes after these procedures include high rates of osteoarthritic changes, as seen on postoperative radiographs [5,6,7].
An alternative intervention is the saucerization procedure, in which only the central area of the DLM is removed, leaving an intact cartilage rim [8, 9]. More recent methods allow for repair and stabilization of the peripheral rim of the meniscus [10,11,12,13]. Reshaping procedures cannot avert knee joint degeneration. However, less degeneration results than that after total or subtotal meniscectomy [10, 14,15,16]. Therefore, joint cartilage can still be overloaded even after saucerization. A DLM is structurally fragile; therefore, it is important to evaluate the status of the meniscus before and after surgery.
Magnetic resonance imaging (MRI) is the most effective and a less invasive procedure to assess knee joint morphology [17, 18]. While the sensitivity and specificity of an MRI diagnosis of primary meniscal tears are high [19,20,21,22], these values are lower when assessing for degeneration and healing of repaired menisci [23,24,25,26,27]. In contrast, quantitative MRI techniques have recently been implemented for the detailed qualitative evaluation of meniscal condition [28,29,30,31], including T2 mapping, which measures the T2 relaxation time by detecting the water content, composition, and anisotropic change in the collagen fibers of cartilage [32,33,34,35]. There is limited currently available data regarding the state of the meniscus before and after DLM surgery. MRI T2 mapping was found to be a useful tool for assessing meniscus status after DLM surgery, which would be helpful in determining the effectiveness of future treatment and in evaluating its relevance to the qualitative assessment of cartilage.
The purpose of this study was to quantify meniscal status with MRI T2 mapping before and after arthroscopic surgery for DLM. We hypothesized that the T2 value would be high preoperatively and decrease after reshaping surgery for DLM.
Methods
This study was approved by the hospital ethics committee and the internal review board of our institution (2728). Informed consent was obtained from all study participants.
We reviewed the records of all patients who underwent arthroscopic treatment by a single surgeon for symptomatic DLM between September 2013 and March 2019 and were followed up for at least 2 years. The only inclusion criterion was symptomatic DLM requiring surgery. Exclusion criteria were (1) history of meniscus surgery, (2) follow-up of less than 2 years, and (3) missing medical records, including the MRI scans of patients who could not be followed up.
The diagnosis of DLM was suspected when there were subjective symptoms such as knee pain, locking, catching, and other physical examination findings (e.g., loss of extension, effusion, snapping, or clunking when extending from flexion), tenderness at the lateral joint space, and a positive McMurray test. It was confirmed by MRI findings [36]. The final criteria for surgery were the combination of the symptoms above and imaging findings indicating that the situation had been difficult to treat conservatively for ≥ 3 months.
Surgical procedure and rehabilitation
Portals were created anterolaterally and anteromedially. Arthroscopic examination was initiated with a 30° oblique arthroscope. After confirming DLM, saucerization was started at the free edge of the meniscus with a standard arthroscopic punch or forceps, referring to the circumferential fibers at the anterior part of the DLM. To restore normal peripheral rim width, the center of the DLM was then removed piecewise [11]. The remaining meniscal rim was probed after saucerization to evaluate stability. If meniscal instability (defined as a longitudinal tear in the vascular meniscus region) was observed, meniscal repair was added to the procedure to stabilize the meniscus to the capsule. All knees with anterior instability were treated with outside-in techniques, and all of those with posterior instability were treated with inside-out techniques. Sutures were placed at 3-mm intervals with 2–0 non-absorbable suture material.
The postoperative rehabilitation schedule depended on the type of surgery. Weight-bearing and knee range-of-motion exercises were begun immediately for patients who underwent DLM saucerization alone. At two months postoperatively, they began jogging, and sports activity could be resumed at three months. Patients who underwent saucerization with stabilization were immobilized in a knee brace for 1 week postoperatively. Subsequently, they performed restricted knee range-of-motion exercises from 0 to 90° for 3 weeks. For the initial 3 weeks, they were non-weight-bearing. At 3 weeks postoperatively, they began partial weight-bearing. Full weight-bearing began at 6 weeks, jogging at 3 months, and return to previous sports at 6 months postoperatively.
Clinical evaluation
The Lysholm knee score was used to evaluate patients preoperatively, when they first had symptoms, and at final follow-up. The scores were compared afterward and evaluated with a minimum clinically important difference (MCID) of 8.9 points to assess whether changes were clinically significant [37].
Radiographic evaluation
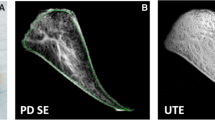
MRI examinations were conducted preoperatively and at 12 and 24 months postoperatively using a 3.0-T scanner (Achieva 3.0 T TX; Philips, Best, The Netherlands). For the examination, patients lay supine on the MRI table. Triangular wedges were placed beneath each knee with a thigh strap to maintain knee flexion of 10°. The knee joint was placed at the center of an eight-channel SENSE knee coil (Philips). MRI analysis was performed by two qualified orthopedic surgeons with experience reading knee MRI, including T2 mapping and imaging analysis. MRI was performed routinely and periodically during the postoperative recovery phase for all DLM patients.
The morphology of each meniscus was assessed with a proton density-weighted multislice turbo spin-echo sequence with fat saturation and the following settings: repetition time (TR) 3462 ms; echo time (TE) 10 ms; receiver band width (RBW) 217.4 Hz; echo train length (ETL) 18; field of view (FOV) 16 × 16 cm; matrix 416 × 416; slice thickness 3 mm; slice gap 0.3 mm; number of slices 26; and number of excitations (NEX).
Sequence used for image interpretation was sagittal T2 mapping (TR 2100; TEs 10, 20, 30, 40, 50, and 60 ms; RBW 290.7 kHz; ETL 18; FOV 16 × 16 cm; matrix size 352 × 352; slice thickness 3.0 mm; slice gap 0.3 mm; number of slices 26; NEX 1; scan time 14 min).
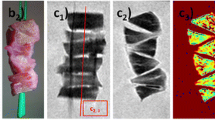
The region of interest was measured in the mid-sagittal plane reflecting the midline of the medial or lateral femoral condyle [38]. Measurements were recorded by manually plotting the outlines of the meniscus and cartilage, and T2 values within the created range were evaluated (Fig. 1). Preoperatively and at 12 and 24 months postoperatively, the T2 transverse relaxation times were assessed for both anterior and posterior horns of the lateral meniscus. For the preoperative MRI, the area at 8 mm from the margin, which is to be preserved by surgery, was evaluated as the anterior and posterior horns, respectively. As a control, the T2 relaxation time of the anterior and posterior horns of the medial meniscus was also assessed preoperatively. To evaluate cartilage status, T2 relaxation time of the lateral and medial femoral condyle and tibial plateau were evaluated at 24 months postoperatively. The lateral femoral condyle was further distinguished into anterior, medial, and posterior sub-compartments [39]. These sub-compartments were the area over the anterior and posterior meniscal horns (the anterior and posterior sub-compartments, respectively) and the area between the 2 horns (the medial sub-compartment). We used Virtual Place Advance software (AZE, Tokyo, Japan) to calculate the T2 relaxation time for each pixel. The longer the T2 relaxation time, the warmer the colors displayed on the color map. T2 relaxation time was set between 75 and 0 ms.
The preoperative meniscal shift was also classified with sagittal and coronal MRI, according to the specifications of Ahn et al. [11]. The categories were characterized as follows: no shift, anterocentral shift, posterocentral shift, and central shift. Preoperative meniscus shift suggests meniscus tear and is an important demographic data for the study group.
The residual meniscal width of the anterior horn, mid-body, and posterior horn, and the extrusion of the mid-body were measured on MRI (mid-sagittal and coronal view) at 24 months after surgery, as previously described [40]. Postoperative meniscus width is also necessary to determine whether the intended reshaping surgery was performed appropriately. In addition, a small postoperative meniscus width can also affect articular cartilage degeneration [16].
Statistical analysis
T2 relaxation times were compared across all time points with Friedman and post hoc Wilcoxon tests. From the surgical record, the anterior and posterior horns were re-sorted into the tear side and non-tear side, and the T2 relaxation times of the tear and non-tear sides were compared using paired t test at each time point. Pearson’s correlation test was used to assess the relationship between the T2 relaxation time of the anterior or posterior horn and that of the corresponding area of the lateral femoral condyle cartilage and between the T2 relaxation time of the tear side meniscus and the Lysholm score at 24 months after surgery. Intraclass correlation coefficients were evaluated by two orthopedic surgeons to determine the intra- and inter-observer reliabilities of the T2 relaxation times of the meniscus. Measurements were performed at two separate times, 2 months apart. The strength of agreement was interpreted as: > 0.80, almost perfect agreement; 0.61–0.80, substantial agreement; 0.41–0.60, moderate agreement; 0.21–0.40, fair agreement; and ≤ 0.20, slight agreement. The intra- and inter-observer reliabilities of the T2 relaxation time measurements were 0.890 and 0.837, respectively.
All hypotheses were tested assuming a 0.05 significance level and a two-sided alternative hypothesis. A power analysis was performed with the power (α) difference and standard deviations set at 0.8, 0.05, 5.5, and 7.0, respectively, according to the T2 relaxation time of the meniscus. The analysis revealed that a minimum of 15 patients were required for Wilcoxon test to detect a difference between the preoperative value and that at 24 months after surgery. EZR software version 1.38 (Saitama Medical Center, Jichi Medical University, Saitama, Japan) was used for all analyses.
Results
Data of 44 knees from 40 consecutive patients with symptomatic DLM were retrospectively collected for this study. Eight patients were excluded because of missing MRI data or less than 2 years of follow-up. Ultimately, 36 knees from 32 patients were included in this study. The mean patient age at the time of surgery was 13.7 years (range, 7–24 years), including 14 men and 18 women. Four patients had bilateral knee involvement. Postoperative follow-up lasted a mean of 31.0 months (range, 24–60 months). Complete discoid meniscus was present in 35 knees and incomplete in one knee. Of the 35 complete discoid menisci, 11 demonstrated no shift, while 10 had anterocentral, 11 had posterocentral, and three had central shifts. Intraoperative arthroscopy identified peripheral longitudinal tears in 31 knees, and horizontal tears with stable peripheral rims in the remaining five knees. Saucerization alone was performed for these five knees, and saucerization plus stabilization was conducted for 31 knees. Subtotal meniscectomy was not performed. The mean Lysholm score increased from 65.3 (range, 45–83) preoperatively to 96.8 (range, 83–100) at final follow-up (P < 0.01) (Table 1). The patients in this study met the MCID for the patient reported outcome measures (PROMs) used in the investigation. The residual meniscal width of the anterior horn, mid-body, and posterior horn, and the extrusion of the mid-body at 2 years after surgery were 8.4 ± 1.9 mm, 5.5 ± 1.6 mm, 8.3 ± 1.8 mm, and 2.0 ± 0.6 mm, respectively.
Preoperatively, the T2 relaxation time of the anterior horn of the lateral meniscus was significantly longer than that of the medial meniscus (lateral vs. medial: 42.3 ± 7.0 ms vs. 34.9 ± 1.9 ms, P < 0.01). The T2 relaxation time significantly decreased at 12 and 24 months postoperatively (38.9 ± 4.5 ms at 12 months and 36.8 ± 3.5 ms at 24 months, P < 0.01), and there was no significant difference between T2 relaxation time of the medial meniscus and lateral meniscus at 24 months (P = 0.063). As for the posterior horn, the T2 relaxation time was significantly longer than that of the medial meniscus preoperatively (lateral vs. medial: 40.9 ± 6.4 ms vs. 34.1 ± 1.9 ms, P < 0.001) and decreased at 12 and 24 months (37.2 ± 3.6 ms at 12 months and 36.2 ± 3.2 ms at 24 months, P < 0.001). There was no significant difference between 12 and 24 months (P = 0.101), and the T2 relaxation time at 24 months was significantly longer than that of the medial meniscus (P = 0.005) (Fig. 2).
In the assessment of the tear and non-tear sides, T2 relaxation time of the tear side was significantly longer than that of the non-tear side preoperatively (44.4 ± 7.1 ms in the tear side and 39.6 ± 5.2 ms in the non-tear side, P < 0.001), at 12 months (39.7 ± 3.9 ms in the tear side and 36.4 ± 3.4 ms in the non-tear side, P < 0.001), and 24 months (37.9 ± 3.9 ms in the tear side and 35.3 ± 2.7 ms in the non-tear side, P < 0.001) after surgery, though the difference seemed to be smaller at 24 months (Fig. 3).
The cartilage T2 relaxation time at 24 months after surgery was 48.1 ± 2.9 ms in the lateral femoral condyle and 41.9 ± 2.3 ms in the lateral tibial plateau. The cartilage T2 relaxation time at 24 months after surgery was 46.8 ± 2.9 ms in the medial femoral condyle and 41.2 ± 3.8 ms in the medial tibial plateau. There were no significant differences in cartilage T2 values between the medial and lateral compartments. In the sub-compartment of the lateral femoral condyle, the T2 relaxation time was 45.3 ± 4.2 ms in the anterior, 47.1 ± 3.0 ms in the middle, and 50.7 ± 3.5 ms in the posterior compartment. There were significant correlations between the T2 relaxation time of the meniscus and that of the corresponding area of the lateral femoral condyle cartilage at 24 months after surgery (anterior horn: r = 0.504, P = 0.002; posterior horn: r = 0.365, P = 0.029) (Fig. 4). Representative images are shown in Fig. 5. No significant correlation was found between T2 relaxation time of the tear side meniscus and Lysholm score at the final follow-up or between T2 relaxation time and the residual meniscal width.
Magnetic resonance imaging (MRI) of a mid-sagittal slice of the right knee. The top row (a–d) shows fat-saturated images, and the bottom row (e–h) shows T2 color mapping images. a, e Preoperative medial compartment. b, f Preoperative lateral compartment. The discoid lateral meniscus showed an anterocentral shift. c, g Lateral compartment at 12 months after surgery. d, h Lateral compartment at 24 months after surgery
Discussion
The most important finding in the present study is that the T2 relaxation time of symptomatic DLM was significantly longer than that of the medial meniscus preoperatively, and decreased 24 months after arthroscopic reshaping surgery. The meniscal T2 relaxation time of the tear side was significantly longer than that of the non-tear side. There were significant correlations between the cartilage and meniscal T2 relaxation time at 24 months after surgery. These findings indicate that MRI T2 mapping could be a useful quantitative evaluation tool to assess the healing status of DLM.
Saucerization with or without concomitant repair has now taken over from subtotal meniscectomy as the treatment of choice for symptomatic DLM [11, 12]. Meniscus preservation prevents worsening degeneration of the articular cartilage in the knee [16]. The main complications after DLM surgery are osteochondritis dissecans and degenerative changes. Increased stress on the articular cartilage is considered as the etiology of both [5, 41]. Even after saucerization, 23–39% of patients have shown degenerative changes [10], although the procedure is more effective at preventing these complications than is subtotal meniscectomy [15]. The assessment of the healing status of the meniscus is one of the most important factors in preventing postoperative degenerative changes. Kai et al. reported that a high meniscal signal change on MRI was associated with an elevated T2 relaxation time of adjacent articular cartilage [42].
T2 mapping with MRI can be used to evaluate the arrangement of collagen and the water content of the articular cartilage, and can assess cartilage changes quantitatively [33, 43, 44]. This evaluation tool is reliable and non-invasive for detecting stress on articular cartilage before degenerative changes appear on plain radiographs [45]. Nishino et al. reported the cartilage T2 relaxation time of DLM before and after surgery [46]; the T2 relaxation time of the lateral femorotibial joint cartilage increased at 3 and 6 months postoperatively and then decreased at 12 and 24 months. In our study, MRI measurements enabled us to quantify the substantial early postoperative changes of the cartilage after DLM reshaping and the recovery changes that developed later.
A few studies have reported meniscal T2 mapping to evaluate the healing of meniscal tears [28, 47, 48]. Yamasaki et al. investigated meniscal healing status using MRI T2 mapping. They evaluated the meniscal T2 relaxation time before and after surgery and confirmed its healing status using second-look arthroscopy. They showed that the T2 relaxation time was significantly shorter in healed menisci than that in incompletely/not healed menisci [48]. Some previous reports have used meniscal T2 mapping to assess meniscal degeneration of osteoarthritic knees [49,50,51]. Eijgenraam et al. evaluated the correlation between T2 mapping of the human meniscus, which was obtained during total knee replacement surgery, and histological degeneration. They reported that there was a strong correlation and that T2 mapping of the meniscus was a biomarker of early osteoarthritis [50]. In the present study, T2 relaxation time of symptomatic DLM was significantly longer than that of the medial meniscus preoperatively and gradually decreased at 24 months after surgery. The meniscal T2 relaxation time of the tear side was significantly longer than that of the non-tear side. DLM is characterized by a decrease in the number of collagen fibers and a heterogeneous course in the fibers compared with the normal meniscus [52]. In addition, symptomatic DLM has abnormal movement caused by tears or degeneration. The increased T2 relaxation time reflects these tears or degeneration of the meniscus, and the recovery of T2 relaxation time allowed us to differentiate the healing status of DLM.
The present study also found positive correlations between cartilage and meniscal T2 relaxation time at 24 months after surgery. This result indicates that an incompletely or unhealed meniscus or degenerated meniscus was associated with degenerative changes in the knee articular cartilage, even in such a young patient group. Rauscher et al. evaluated the differences in meniscal T1ρ and T2 mapping in patients with varying degrees of osteoarthritis and healthy control participants. They reported that meniscal T1ρ and T2 relaxation time significantly correlated with Western Ontario and McMaster Osteoarthritis (WOMAC) scores [51]. Zarins et al. also reported an association between meniscal T2 mapping and cartilage degeneration in healthy participants and patients with osteoarthritis. They concluded that early detection of meniscal damage represented by an elevation in the relaxation time might identify participants with an increased risk for osteoarthritis [53]. The correlations in this study were relatively weak because the causes of cartilage degeneration are multifactorial (e.g., patient activity, duration of symptoms, etc.). Nevertheless, the results of the present study supported those of the previous reports and emphasized the importance of meniscal damage assessment.
There were no correlations between meniscal T2 relaxation time, residual meniscal width, and clinical score. Lee et al. conducted a systematic review and meta-analysis of the clinical and radiographic outcomes of partial versus total meniscectomy in patients with symptomatic DLM. Compared to total meniscectomy, partial meniscectomy yielded significantly more cases with normal cartilage status or mild chondral wear. However, the clinical results between the two groups were comparable [54]. One possible explanation for this is that the surgical procedure was stable and there was minimal variation in width and clinical score. In addition, there were some cases with a large amount of residual meniscus with meniscal degeneration. As for the clinical score, symptoms such as pain derived from osteoarthritis appear on the surface after degenerative changes progress on plain radiographs. Internal meniscal degeneration of the meniscus has also been implicated to increase the postoperative risk for decreased residual meniscus volume [40]. Such factors could contribute to long-term cartilage degeneration.
This study has several limitations. First, it was difficult to gather complete medical records, including serial MRI findings, and thus, the sample size was small. Second, the retrospective design of this study had inherent limitations. Third, the follow-up period was relatively short to assess postoperative degenerative changes. Finally, the current study did not have a reference for meniscal status by second-look arthroscopy. Nevertheless, MRI T2 mapping was useful in differentiating meniscal status and degeneration of the knee articular cartilage at an early stage.
Conclusion
The T2 relaxation time of symptomatic DLM was significantly longer than that of the medial meniscus preoperatively and decreased at 24 months after arthroscopic reshaping surgery. The meniscal T2 relaxation time of the tear side was significantly longer than that of the non-tear side. There were significant correlations between the cartilage and meniscal T2 relaxation time at 24 months after surgery.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Young RB (1889) The external semilunar cartilage as a complete disc. In: Cleland J, Mackay JY, Young RB (eds) Memoirs and memoranda in anatomy. Williams & Norgate, London, UK, p 179
Papadopoulos A, Kirkos JM, Kapetanos GA (2009) Histomorphologic study of discoid meniscus. Arthroscopy 25(3):262–268. https://doi.org/10.1016/j.arthro.2008.10.006
Habata T, Uematsu K, Kasanami R, Hattori K, Takakura Y, Tohma Y, Fujisawa Y (2006) Long-term clinical and radiographic follow-up of total resection for discoid lateral meniscus. Arthroscopy 22(12):1339–1343. https://doi.org/10.1016/j.arthro.2006.07.039
Ikeuchi H (1982) Arthroscopic treatment of the discoid lateral meniscus: technique and long-term results. Clin Orthop Relat Res 167(167):19–28. https://doi.org/10.1097/00003086-198207000-00005
Okazaki K, Miura H, Matsuda S, Hashizume M, Iwamoto Y (2006) Arthroscopic resection of the discoid lateral meniscus: long-term follow-up for 16 years. Arthroscopy 22(9):967–971. https://doi.org/10.1016/j.arthro.2006.04.107
Abdon P, Turner MS, Pettersson H, Lindstrand A, Stenström A, Swanson AJ (1990) A long-term follow-up study of total meniscectomy in children. Clin Orthop Relat Res 257(257):166–170. https://doi.org/10.1097/00003086-199008000-00030
Manzione M, Pizzutillo PD, Peoples AB, Schweizer PA (1983) Meniscectomy in children: a long-term follow-up study. Am J Sports Med 11(3):111–115. https://doi.org/10.1177/036354658301100301
Fujikawa K, Iseki F, Mikura Y (1981) Partial resection of the discoid meniscus in the child’s knee. J Bone Joint Surg Br 63–B(3):391–395. https://doi.org/10.1302/0301-620X.63B3.7263752
Oğüt T, Kesmezacar H, Akgün I, Cansü E (2003) Arthroscopic meniscectomy for discoid lateral meniscus in children and adolescents: 4.5 year follow-up. J Pediatr Orthop B 12(6):390–397. https://doi.org/10.1097/01202412-200311000-00007
Ahn JH, Kim KI, Wang JH, Jeon JW, Cho YC, Lee SH (2015) Long-term results of arthroscopic reshaping for symptomatic discoid lateral meniscus in children. Arthroscopy 31(5):867–873. https://doi.org/10.1016/j.arthro.2014.12.012
Ahn JH, Lee SH, Yoo JC, Lee YS, Ha HC (2008) Arthroscopic partial meniscectomy with repair of the peripheral tear for symptomatic discoid lateral meniscus in children: results of minimum 2 years of follow- up. Arthroscopy 24(8):888–898. https://doi.org/10.1016/j.arthro.2008.03.002
Good CR, Green DW, Griffith MH, Valen AW, Widmann RF, Rodeo SA (2007) Arthroscopic treatment of symptomatic discoid meniscus in children: classification, technique, and results. Arthroscopy 23(2):157–163. https://doi.org/10.1016/j.arthro.2006.09.002
Wasser L, Knörr J, Accadbled F, Abid A, Sales De Gauzy J (2011) Arthroscopic treatment of discoid meniscus in children: clinical and MRI results. Orthop Traumatol Surg Res 97(3):297–303. https://doi.org/10.1016/j.otsr.2010.11.009
Ahn JH, Kang DM, Choi KJ (2017) Risk factors for radiographic progression of osteoarthritis after partial meniscectomy of discoid lateral meniscus tear. Orthop Traumatol Surg Res 103(8):1183–1188. https://doi.org/10.1016/j.otsr.2017.09.013
Lee DH, Kim TH, Kim JM, Bin SI (2009) Results of subtotal/total or partial meniscectomy for discoid lateral meniscus in children. Arthroscopy 25(5):496–503. https://doi.org/10.1016/j.arthro.2008.10.025
Yamasaki S, Hashimoto Y, Takigami J, Terai S, Takahashi S, Nakamura H (2017) Risk factors associated with knee joint degeneration after arthroscopic reshaping for juvenile discoid lateral meniscus. Am J Sports Med 45(3):570–577. https://doi.org/10.1177/0363546516668623
Kinoshita T, Hashimoto Y, Nishida Y, Iida K, Nakamura H (2022) Evaluation of knee bone morphology in juvenile patients with complete discoid lateral meniscus using magnetic resonance imaging. Arch Orthop Trauma Surg 142(4):649–655. https://doi.org/10.1007/s00402-021-03908-x
Kinoshita T, Hashimoto Y, Iida K, Nakamura H (2022) Evaluation of the knee joint morphology associated with a complete discoid lateral meniscus, as a function of skeletal maturity, using magnetic resonance imaging. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04538-7
Challen J, Tang YM, Hazratwala K, Stuckey S (2007) Accuracy of MRI diagnosis of internal derangement of the knee in a non-specialized tertiary level referral teaching hospital. Australas Radiol 51(5):426–431. https://doi.org/10.1111/j.1440-1673.2007.01865.x
Oei EH, Nikken JJ, Verstijnen AC, Ginai AZ, Myriam Hunink MG (2003) MR imaging of the menisci and cruciate ligaments: a systematic review. Radiology 226(3):837–848. https://doi.org/10.1148/radiol.2263011892
Russo A, Capasso R, Varelli C et al (2017) MR imaging evaluation of the postoperative meniscus. Musculoskelet Surg 101(Suppl 1):37–42. https://doi.org/10.1007/s12306-017-0454-3
Hashimoto Y, Nishino K, Yamasaki S, Nishida Y, Takahashi S, Nakamura H (2022) Two positioned MRI can visualize and detect the location of peripheral rim instability with snapping knee in the no-shift-type of complete discoid lateral meniscus. Arch Orthop Trauma Surg 142(8):1971–1977. https://doi.org/10.1007/s00402-021-04148-9
Applegate GR, Flannigan BD, Tolin BS, Fox JM, Del Pizzo W (1993) MR diagnosis of recurrent tears in the knee: value of intraarticular contrast material. AJR Am J Roentgenol 161(4):821–825. https://doi.org/10.2214/ajr.161.4.8372768
Farley TE, Howell SM, Love KF, Wolfe RD, Neumann CH (1991) Meniscal tears: MR and arthrographic findings after arthroscopic repair. Radiology 180(2):517–522. https://doi.org/10.1148/radiology.180.2.2068321
McCauley TR (2005) MR imaging evaluation of the postoperative knee. Radiology 234(1):53–61. https://doi.org/10.1148/radiol.2341031302
Miao Y, Yu JK, Zheng ZZ et al (2009) MRI signal changes in completely healed meniscus confirmed by second-look arthroscopy after meniscal repair with bioabsorbable arrows. Knee Surg Sports Traumatol Arthrosc 17(6):622–630. https://doi.org/10.1007/s00167-009-0728-x
White LM, Schweitzer ME, Weishaupt D, Kramer J, Davis A, Marks PH (2002) Diagnosis of recurrent meniscal tears: prospective evaluation of conventional MR imaging, indirect MR arthrography, and direct MR arthrography. Radiology 222(2):421–429. https://doi.org/10.1148/radiol.2222010396
Berton A, Longo UG, Candela V, Greco F, Martina FM, Quattrocchi CC, Denaro V (2020) Quantitative evaluation of meniscal healing process of degenerative meniscus lesions treated with hyaluronic acid: a clinical and MRI study. J Clin Med 9(7):2280. https://doi.org/10.3390/jcm9072280
Nishioka H, Hirose J, Nakamura E, Oniki Y, Takada K, Yamashita Y, Mizuta H (2012) T1r and T2 mapping reveal the in vivo extracellular matrix of articular cartilage. J Magn Reson Imaging 35(1):147–155. https://doi.org/10.1002/jmri.22811
Regatte RR, Akella SV, Borthakur A, Reddy R (2003) Proton spin-lock ratio imaging for quantitation of glycosaminoglycans in articular cartilage. J Magn Reson Imaging 17(1):114–121. https://doi.org/10.1002/jmri.10228
Tiderius CJ, Olsson LE, Leander P, Ekberg O, Dahlberg L (2003) Delayed gadolinium-enhanced MRI of cartilage (dGEMRIC) in early knee osteoarthritis. Magn Reson Med 49(3):488–492. https://doi.org/10.1002/mrm.10389
Goodwin DW, Zhu H, Dunn JF (2000) In vitro MR imaging of hyaline cartilage: correlation with scanning electron microscopy. AJR Am J Roentgenol 174(2):405–409. https://doi.org/10.2214/ajr.174.2.1740405
Liess C, Lüsse S, Karger N, Heller M, Glüer CC (2002) Detection of changes in cartilage water content using MRI T2-mapping in vivo. Osteoarthr Cartil 10(12):907–913. https://doi.org/10.1053/joca.2002.0847
Mlynárik V, Trattnig S, Huber M, Zembsch A, Imhof H (1999) The role of relaxation times in monitoring proteoglycan depletion in articular cartilage. J Magn Reson Imaging 10(4):497–502. https://doi.org/10.1002/(sici)1522-2586(199910)10:4%3c497::aid-jmri1%3e3.0.co;2-t
Xia Y (2000) Magic-angle effect in magnetic resonance imaging of articular cartilage: a review. Invest Radiol 35(10):602–621. https://doi.org/10.1097/00004424-200010000-00007
Samoto N, Kozuma M, Tokuhisa T, Kobayashi K (2002) Diagnosis of discoid lateral meniscus of the knee on MR imaging. Magn Reson Imaging 20(1):59–64. https://doi.org/10.1016/s0730-725x(02)00473-3
Harris JD, Brand JC, Cote MP, Faucett SC, Dhawan A (2017) Research pearls: the significance of statistics and perils of pooling Part 1: Clinical versus statistical significance. Arthroscopy 33(6):1102–1112. https://doi.org/10.1016/j.arthro.2017.01.053
Murakami K, Arai Y, Ikoma K et al (2018) Total resection of any segment of the lateral meniscus may cause early cartilage degeneration: evaluation by magnetic resonance imaging using T2 mapping. Medicine (Baltim) 97(23):e11011. https://doi.org/10.1097/MD.0000000000011011
Bolbos RI, Link TM, Ma CB, Majumdar S, Li X (2009) T1rho relaxation time of the meniscus and its relationship with T1rho of adjacent cartilage in knees with acute ACL injuries at 3 T. Osteoarthr Cartil 17(1):12–18. https://doi.org/10.1016/j.joca.2008.05.016
Nishino K, Hashimoto Y, Tsumoto S, Yamasaki S, Nakamura H (2021) Morphological changes in the residual meniscus after reshaping surgery for a discoid lateral meniscus. Am J Sports Med 49(12):3270–3278. https://doi.org/10.1177/03635465211033586
Hashimoto Y, Nishino K, Reid JB 3rd et al (2020) Factors related to postoperative osteochondritis Dissecans of the lateral femoral condyle after meniscal surgery in juvenile patients with a discoid lateral meniscus. J Pediatr Orthop 40(9):e853–e859. https://doi.org/10.1097/BPO.0000000000001636
Kai B, Mann SA, King C, Forster BB (2011) Integrity of articular cartilage on T2 mapping associated with meniscal signal change. Eur J Radiol 79(3):421–427. https://doi.org/10.1016/j.ejrad.2010.06.011
Bolbos RI, Zuo J, Banerjee S, Link TM, Ma CB, Li X, Majumdar S (2008) Relationship between trabecular bone structure and articular cartilage morphology and relaxation times in early OA of the knee joint using parallel MRI at 3 T. Osteoarthr Cartil 16(10):1150–1159. https://doi.org/10.1016/j.joca.2008.02.018
Nieminen MT, Rieppo J, Töyräs J et al (2001) T2 relaxation reveals spatial collagen architecture in articular cartilage: a comparative quantitative MRI and polarized light microscopic study. Magn Reson Med 46(3):487–493. https://doi.org/10.1002/mrm.1218
Li H, Chen S, Tao H, Chen S (2015) Quantitative MRI T2 relaxation time evaluation of knee cartilage: comparison of meniscus-intact and -injured knees after anterior cruciate ligament reconstruction. Am J Sports Med 43(4):865–872. https://doi.org/10.1177/0363546514564151
Nishino K, Hashimoto Y, Nishida Y, Yamasaki S, Nakamura H (2021) Magnetic resonance imaging T2 relaxation times of articular cartilage before and after arthroscopic surgery for discoid lateral meniscus. Arthroscopy 37(2):647–654. https://doi.org/10.1016/j.arthro.2020.09.036
Knox J, Pedoia V, Wang A et al (2018) Longitudinal changes in MR T1rho/T2 signal of meniscus and its association with cartilage T1p/T2 in ACL-injured patients. Osteoarthr Cartil 26(5):689–696. https://doi.org/10.1016/j.joca.2018.02.001
Yamasaki S, Hashimoto Y, Nishida Y, Teraoka T, Terai S, Takigami J, Nakamura H (2020) Assessment of meniscal healing status by magnetic resonance imaging T2 mapping after meniscal repair. Am J Sports Med 48(4):853–860. https://doi.org/10.1177/0363546520904680
Baum T, Joseph GB, Karampinos DC, Jungmann PM, Link TM, Bauer JS (2013) Cartilage and meniscal T2 relaxation time as non-invasive biomarker for knee osteoarthritis and cartilage repair procedures. Osteoarthr Cartil 21(10):1474–1484. https://doi.org/10.1016/j.joca.2013.07.012
Eijgenraam SM, Bovendeert FAT, Verschueren J et al (2019) t2 mapping of the meniscus is a biomarker for early osteoarthritis. Eur Radiol 29(10):5664–5672. https://doi.org/10.1007/s00330-019-06091-1
Rauscher I, Stahl R, Cheng J et al (2008) Meniscal measurements of T1rho and T2 at MR imaging in healthy subjects and patients with osteoarthritis. Radiology 249(2):591–600. https://doi.org/10.1148/radiol.2492071870
Atay OA, Pekmezci M, Doral MN, Sargon MF, Ayvaz M, Johnson DL (2007) Discoid meniscus: an ultrastructural study with transmission electron microscopy. Am J Sports Med 35(3):475–478. https://doi.org/10.1177/0363546506294678
Zarins ZA, Bolbos RI, Pialat JB, Link TM, Li X, Souza RB, Majumdar S (2010) Cartilage and meniscus assessment using T1rho and T2 measurements in healthy subjects and patients with osteoarthritis. Osteoarthr Cartil 18(11):1408–1416. https://doi.org/10.1016/j.joca.2010.07.012
Lee DH, D’Lima DD, Lee SH (2019) Clinical and radiographic results of partial versus total meniscectomy in patients with symptomatic discoid lateral meniscus: a systematic review and meta-analysis. Orthop Traumatol Surg Res 105(4):669–675. https://doi.org/10.1016/j.otsr.2019.02.023
Acknowledgements
We thank Editage Group for editing a draft of this manuscript.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
KN: conception and design and drafting of the article. YH: conception, and critical revision of the article for important intellectual content. YN: interpretation of data. SY: critical revision of the manuscript. HN: conception and design, final approval of the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Ethical approval
This study was approved by the hospital ethics committee and the internal review board of our institution (2728). Informed consent was obtained from all study participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nishino, K., Hashimoto, Y., Nishida, Y. et al. Arthroscopic surgery for symptomatic discoid lateral meniscus improves meniscal status assessed by magnetic resonance imaging T2 mapping. Arch Orthop Trauma Surg 143, 4889–4897 (2023). https://doi.org/10.1007/s00402-023-04819-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04819-9