Abstract
Background
To date, there are no systematic reviews on the utility of surgical management for plantar fasciitis to guide best practice. This review aimed to evaluate the operative options for plantar fasciitis and their effectiveness.
Methods
A systematic review and network meta-analysis were carried out in accordance with PRISMA guidelines. A search strategy was conducted on the MEDLINE, EMBASE, and Cochrane databases. Quality was assessed using the ROBINS-I tool.
Results
17 studies involving 865 patients were included. Surgical options considered were open and endoscopic plantar fasciotomy, gastrocnemius release, radiofrequency microtenotomy and dry needling. All interventions resulted in improvement in VAS and AOFAS scores. No major complications were seen from any treatment modality.
Conclusions
Surgical interventions are effective in providing short- to medium-term symptomatic relief for plantar fasciitis refractory to non-operative management. Current evidence is equivocal regarding treatment choice. Further large randomised studies are required to establish long-term outcomes and a management algorithm.
Level of evidence
Level III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Plantar fasciitis, also referred to as plantar fasciopathy, is characterised by heel pain secondary to microtears from repetitive stress resulting in chronic degenerative changes of the plantar fascia at its proximal attachment in the calcaneum [1, 2]. The condition affects one in ten people in their lifetime, with a peak incidence in those aged 45 to 65 years [3].
Approximately 90% of cases will resolve within 12 months with non-operative measures [4]. A recent best practice guide recommends patient education, plantar fascia stretching exercises, and low dye taping in the first instance [5]. Beyond this, adjunctive interventions including foot orthoses and extra-corporeal shockwave therapy can be considered [5, 6]. Additional non-operative options are injections, including corticosteroids, botulinum toxin and platelet-rich plasma, however, evidence for the efficacy of these is lacking at present [5, 6].
In cases where the above measures do not provide adequate symptomatic relief after a period of 9–12 months, surgical management can be considered [7]. Surgical options include plantar fasciotomy, gastrocnemius recession, radiofrequency microtenotomy and dry-needling [8].
At present, there are no systematic reviews on the utility of the surgical treatment options to guide best practice. This aims of this review were to evaluate the surgical options for plantar fasciitis and their effectiveness.
Methods
Protocol and registration
A systematic review of the published literature was carried out in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [9].
Eligibility criteria
Inclusion criteria are outlined in accordance with the PICOS framework in Table 1. Exclusion criteria were non-comparative studies, case series, case reports, reviews, conference abstracts, opinion-based reports, and articles not published in English.
Search strategy
A comprehensive search of the published literature on the MEDLINE, EMBASE and Cochrane databases from inception to 16th April 2021 was carried out. The following search terms were used: (plantar fasc*) AND (surg* OR procedure OR fasciotomy OR fasciectomy OR recession).
Study selection
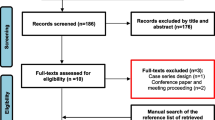
Two reviewers independently performed eligibility assessment of the articles. This was initially carried out through screening of the article titles, followed by the abstracts. The process was completed by full text evaluation. Disagreements between reviewers were resolved via consensus with the senior author. Backward citation searches of papers cited by each article and forward citation searches of other papers that have cited the included articles were carried out to identify any additional papers not picked up from the initial search.
Data collection process
A pilot of the data proforma was initially conducted using three randomly chosen papers to develop a final proforma. Information collected is summarised in Table 2. In cases where there was ambiguity or missing results, the authors were contacted directly for clarification. Two key outcome measures considered were the VAS score, a validated patient-reported outcome measure to assess pain [10, 11], and the AOFAS score, a validated tool to assess pain and function following foot and ankle surgery [12,13,14].
Meta-analysis and network meta-analysis
Mean values and ranges were used to describe continuous variables, and percentages for categorical variables. Narrative synthesis of the results was carried out.
Studies that included a full data set for the VAS or AOFAS score with at least 12 months follow up were included for meta-analysis. For each individual study, we extracted data for patient characteristics, number of patients in each intervention, mean VAS and/or AOFAS score, and the standard deviation of the mean score. Data were recorded and managed on Revman (Version 5.3, property of the Cochrane Collaboration) [15] and MetaXL (Version 5.3, property of EpiGear) [16].
We calculated the absolute mean difference in VAS and AOFAS score between the two interventions described for each study. Not all studies provided a P value for the statistical significance of the difference in means. Therefore, to ensure consistency across all studies we investigated the statistical significance of the absolute mean difference using Welch’s unpaired two-tailed t test. This assumes an unequal variance model between groups (in all studies apart from one there were different numbers of patients for each treatment arm). We compared the P value calculated to the P-value present in the original study (where reported) to check for discrepancies.
Studies suitable for a meta-analysis were grouped by the interventions tested. Five interventions were investigated: proximal medial gastrocnemius release, open plantar fasciotomy, endoscopic plantar fasciotomy, radiofrequency microtenotomy, and non-operative management.
When more than one study reported the same two interventions and comparisons these were pooled into a meta-analysis to calculate a weighted mean difference (WMD) in VAS and AOFAS score between the two interventions. We calculated these with 95% confidence intervals. When performing a meta-analysis we used a DerSimonian Random Effects model due to anticipated high levels of heterogeneity between studies [17]. Clinical and methodological heterogeneity were assessed by author judgement based on patient characteristics and study design while statistical heterogeneity was assessed using Cochranes Q test [17].
To investigate interventions that were not directly compared in the literature, a network meta-analysis was performed to facilitate indirect comparisons. For the network meta-analysis, the Generalized Pairwise Modelling (GPM) method was used [18]. This consists of using multiple adjusted indirect comparisons according to the Bucher method. This was performed on MetaXL v5.3.
Publication bias was assessed using funnel plots, however, we were unable to perform quantitative assessment of asymmetry using Egger's test due to the low number of studies encountered [19].
Risk of bias and quality appraisal
Risk of bias was assessed for each individual study by two independent reviewers. This was carried out in accordance with the Cochrane Collaboration guidelines using the ‘Risk-of-Bias tool’ (RoB 2) for RCTs and ‘Risk Of Bias In Non-Randomised Studies—of Interventions’ (ROBINS-I) for non-randomised studies.
Results
Study selection
A total of 17 papers were included for final analysis. The PRISMA flow diagram of study selection is illustrated in Fig. 1.
Study characteristics
Overall, there were eight RCTs [20,21,22,23,24,25,26,27], three prospective cohort studies [28,29,30] and six retrospective cohort studies [31,32,33,34,35,36]. In total, there were 865 patients included in this systematic review encompassing 903 feet with plantar fasciitis. There was a female preponderance of 64%. In all studies inclusion criteria were a diagnosis of plantar fasciitis (whether clinical or radiological) refractory to non-operative measures, ranging from three to 12 months.
Plantar fasciotomy versus gastrocnemius recession
Two studies compared open plantar fasciotomy with gastrocnemius recession (Table 3). An RCT of 36 patients by Gamba et al. showed significant improvement in both groups in terms of their pain and function over a 12-month period [20]. Whilst there was a trend towards better outcomes following proximal medial gastrocnemius release (PMGR), no statistically significant difference was reached. A retrospective cohort study of 60 patients by Monteagudo et al. similarly showed significant improvement in both groups [34]. However, greater improvement in pain and function was demonstrated following PMGR at 6 and 12 months. This was coupled with higher patient satisfaction rates in this group (good/excellent in 90% following PMGR versus 40% following open plantar fasciotomy).
Endoscopic versus open plantar fasciotomy
Two studies considered endoscopic versus open plantar fasciotomy (Table 3). A prospective cohort study of 62 patients by Feng et al. demonstrated improvement in both groups [28]. Significantly better pain and function was seen in the endoscopic group at 3 months post-operatively, whereas comparable outcomes were seen thereafter up to final follow up at 2 years post-operatively. There was no significant difference in recurrence rates between the two groups. A retrospective cohort study of 38 patients (42 feet) by Chou et al. demonstrated similar results with greater reduction in pain and improvement in function at 3 months post-operatively following endoscopic plantar fasciotomy and no statistically significant difference at 6 and 12 months [31].
An RCT of 41 patients by Catal et al. looking solely at endoscopic plantar fasciotomy, investigated a deep versus superficial fascial approach. Both techniques resulted in significant improvement in pain and function. Whilst there was no statistical difference between the two groups at 3, 6 and 12 months, a significantly greater improvement was seen at 3 weeks post-operatively in the superficial group. Moreover, this group was associated with faster operative time and less complications [27].
Gastrocnemius recession versus non-operative management
An RCT of 40 patients by Molund et al. investigated PMGR and stretching exercises versus stretching exercises alone (Table 3) [21]. This showed significant improvements in pain and function following PMGR at 3 and 12 months post-operatively with no major complications. In contrast, only a moderate improvement was seen following stretching exercises alone at the 3-month time point, which trended back towards pre-intervention results at 12 months.
Endoscopic plantar fasciotomy versus non-operative management
Four studies investigated endoscopic plantar fasciotomy versus various non-operative measures (Table 3). Two RCTs looked at endoscopic plantar fasciotomy versus injections (corticosteroid (CS) and platelet-rich plasma (PRP), respectively). Johannsen et al. demonstrated improvement over time with both fasciotomy and CS injections (up to three monthly injections), however, pain was significantly better at 24 months in the operative group [22]. Furthermore, they considered function using the Foot Function Index (FFI). This showed greater improvement in function in the operative group at 12 months with no significant difference between the two groups by 24 months. Othman et al. showed comparable results from endoscopic plantar fasciotomy and PRP injections [23].
Two studies considered endoscopic plantar fasciotomy versus extracorporeal shockwave therapy (ESWT). An RCT of 65 patients by Radwan et al. showed improvement in pain and function up to 12 months in both groups with no significant difference in the VAS or AOFAS scores at any time point [24]. A higher ‘success rate’, defined as the number of patients who achieved good and excellent scores in the Roles and Maudsley criteria, was seen in the operative group at 12 months (77.4% versus 70.6%), although this did not reach statistical significance. A prospective cohort study of 37 patients showed a similar improvement in pain score between pre-intervention and at final follow up (mean follow up 11 months in the operative group and 7.6 months in the ESWT group). Functional outcomes were not considered in this latter study, however, the mean time to return to work was 6 weeks in the operative group versus 2 weeks in the ESWT group [29].
Radiofrequency microtenotomy
Radiofrequency microtenotomy was investigated against various different interventions in four studies (Table 3). Two retrospective cohort studies considered percutaneous radiofrequency microtenotomy versus open plantar fasciotomy. Yuan et al. showed significant improvement in the VAS and AOFAS scores with both interventions at final follow up [36]. No difference was seen in the scores between the two groups. However, operative time was less in the radiofrequency ablation group (19.73 min versus 36.78 min) and associated with a shorter post-operative recovery time to normal function (13.27 days versus 25.94 days). These findings were replicated by Chou et al., who similarly found no difference in VAS and AOFAS scores between the two groups [32]. Notably, in this latter study, a third arm was included that received both open plantar fasciotomy and radiofrequency microtenotomy. In this group, there was also no statistical difference in outcome measures compared to the individual therapies.
A retrospective cohort study by Wang et al. looked at open radiofrequency microtenotomy versus endoscopic plantar fasciotomy. In their study of 34 patients there was a significantly greater improvement in pain and function at 3 months in the endoscopic plantar fasciotomy group, with no difference between the two groups by 12 months [35].
Huang et al. carried out a retrospective cohort study of 51 patients investigating radiofrequency microtenotomy (either percutaneous or open) versus PMGR [33]. Their study investigated three groups: those that received the individual therapies and a third group that received both. They found significant improvement in pain and function from both treatments, with no statistically significant difference in outcome measures between the groups at 3, 6 or 12 months.
A further prospective cohort study investigated open versus percutaneous radiofrequency microtenotomy, demonstrating a more significant improvement in VAS score at 12 months post-operatively following an open procedure (mean improvement of 6.78 versus 4.48) with no difference in AOFAS score and no complications in either group [30].
Dry needling versus non-operative management
Two RCTs looked at dry needling therapy (Table 3). Uygur et al. investigated dry needling versus CS injections in 96 patients, demonstrating significant improvement in function from the FFI with both therapies at 3 weeks with continued benefit at 6 months in the dry needling group and loss of efficacy at this time point in the injection group [26]. Rahbar et al. investigated dry needling versus ESWT in 72 patients [25]. They found significant improvement in pain as well as function from the FFI at 4 and 8 weeks post-intervention in both groups. Whilst there was no difference between the two groups at 4 weeks, a significantly greater reduction in the VAS score and improvement in the FFI was observed in the dry needling group at 8 weeks.
Network meta-analysis
Nine papers were suitable for network meta-analysis. Two papers were excluded as they investigated variations of the same intervention type. One paper was excluded as they did not include the VAS or AOFAS score in any of their outcome measures. Two papers were excluded due an inadequate follow up period. In five cases, the authors were contacted for additional information. A response was received from two and the remaining three were excluded as sufficient information was not available for meta-analysis.
In one study the mean and standard deviation were not available [21]. These were calculated from the median, range and sample size as described by Hozo et al. [37]. In one study [24] the mean and standard deviation were calculated from the median and interquartile range using the method described by Wan et al. and the Cochrane handbook [38, 39].
Considering the VAS score, direct comparisons showed statistically significant improvement with PMGR compared to non-operative management (absolute mean difference − 2.65 [95% CI − 4.03 to − 1.27], p = 0.0004) and a near significant improvement with PMGR compared to open plantar fasciotomy (absolute mean difference − 1.36 [95% CI − 2.85 to 0.13], p = 0.07). Indirect comparisons using a network meta-analysis suggested an improvement with radiofrequency microtenotomy compared to non-operative management (estimated weighted mean difference − 2.72 [95% CI − 4.84 to − 0.60]). No other significant differences were identified between interventions from direct or indirect comparison (Figs. 2 and 3).
Network graph of included studies for VAS score at 12 months, with thickness of lines and size of circles proportional to number of studies and number of participants, respectively. Black text represents number of studies, and blue text number of participants. OPF open plantar fasciotomy, EPF endoscopic plantar fasciotomy, PMGR proximal medial gastrocnemius release, RMT radiofrequency microtenotomy
Forest plot illustrating weighted mean difference (WMD) and 95% confidence interval (CI) of VAS score at 12 months between each surgical intervention versus non-operative management. Left of solid line indicates lower VAS with operative management; right of solid line indicates higher VAS with operative management. OPF open plantar fasciotomy, EPF endoscopic plantar fasciotomy, PMGR proximal medial gastrocnemius release, RMT radiofrequency microtenotomy. PMGR and EPF based on direct comparisons; RMT and OPF based on indirect comparisons
Regarding the AOFAS score, direct comparison similarly demonstrated statistically significant improvement with PMGR compared to non-operative management (absolute mean difference 19 [95% CI 10.42–27.59], p = 0.0001) and indirect comparisons using a network meta-analysis suggested improvement with radiofrequency microtenotomy versus non-operative management (estimated weighted mean difference 20.54 [95% CI 7.68–33.40]). No other significant differences were identified between interventions from direct or indirect comparison (Figs. 4 and 5).
Network graph of included studies for AOFAS score at 12 months, with thickness of lines and size of circles proportional to number of studies and number of participants, respectively. Black text represents number of studies, and blue text number of participants. OPF open plantar fasciotomy, EPF endoscopic plantar fasciotomy, PMGR proximal medial gastrocnemius release, RMT radiofrequency microtenotomy
Forest plot illustrating weighted mean difference (WMD) and 95% confidence interval (CI) of AOFAS score at 12 months between each surgical intervention versus non-operative management. Left of solid line indicates lower AOFAS score with operative management; right of solid line indicates higher AOFAS score with operative management. OPF open plantar fasciotomy, EPF endoscopic plantar fasciotomy, PMGR proximal medial gastrocnemius release, RMT radiofrequency microtenotomy. PMGR and EPF based on direct comparisons; RMT and OPF based on indirect comparisons
Risk of bias
Risk of bias for all studies is summarised in Fig. 6A, B. All of the RCTs were considered to have “some concerns”, due to an inability to carry out blinding of the participants or healthcare provider. Risk of bias for cohort studies ranged from “low” to “moderate”, with a risk of selection bias, reporting bias and confounding factors in some studies, particularly those that were retrospective in nature.
Discussion
This systematic review suggests that all operative interventions are effective in providing short- to medium-term symptomatic relief for plantar fasciitis refractory to non-operative management. The reported outcomes were up to a follow-up period of 12 months for the majority of the included studies and no more than 24 months in any study, therefore long-term outcomes cannot be determined.
There is indication that PMGR provides better outcomes than plantar fasciotomy. This may be in part due to a strong association between plantar fasciitis and reduced dorsiflexion secondary to gastrocnemius tightness [8], however, the presence of this was not addressed in the current studies. When performing plantar fasciotomy, earlier improvement is seen with an endoscopic procedure due to its minimally invasive nature. Moreover, when performing endoscopic plantar fasciotomy, there appears to be even earlier improvement with a superficial approach.
Radiofrequency tenotomy results in similar outcomes to PMGR and plantar fasciotomy and may be a more attractive option as it can be performed percutaneously in a shorter period of time. Dry needling has greater outcomes when compared to non-operative management. Furthermore, it has the added benefit that it is less invasive and can be performed in the outpatient setting without the need for a specialist foot and ankle surgeon. Therefore, this intervention may prove advantageous in the more resource poor setting. However, to date this procedure has not been compared to alternative operative interventions.
Notably, there were no major complications reported in any study regardless of the intervention performed. The most common complication was recurrence of pain, followed by superficial infection. Moreover, there were three cases of lateral plantar nerve numbness following plantar fasciotomy. No patients in any study required return to theatre for a surgical complication.
The outcome measures considered in this systematic review were the VAS score and AOFAS. The minimal clinically important difference (MCID) in VAS for plantar fasciitis has been reported as between 8 and 9 mm (0.8–0.9 on the scale out of 10) [10, 40], hence significant improvement was seen in all studies regardless of intervention with little clinically significant difference between interventions. MCID of the AOFAS score in plantar fasciitis has not been reported in the literature. Following hallux valgus surgery, it has been demonstrated to be between 7.9 and 30.2 [41]. Based on extrapolation from this data, there was again significant clinical improvement with all surgical options with little clinical difference between interventions.
From the available evidence to date, the authors’ recommendation is that following failure of non-operative management (including use of non-steroidal anti-inflammatories, heel pads, splints, hot and cold compresses, physiotherapy with eccentric Achilles tendon and plantar fascia stretching exercises, and ESWT) surgical management is a viable treatment option. Patients should be examined for gastrocnemius tightness, and if this is present PMGR can be considered. If this is not present, patients should be counselled between the options of percutaneous radiofrequency microtenotomy, dry needling and endoscopic plantar fasciotomy (depending on expertise and equipment availability at the hospital).
This systematic review was limited due to the lack of high-quality evidence available in the literature. Small patient numbers were reported in all studies and nine (53%) of the studies were non-randomised. From these, six were retrospective and thus have an inherent selection and publication bias. Moreover, our network meta-analysis showed only small amount of significance across studies. Whilst this can relate to the minimal difference in efficacy between the surgical treatment options, this may also be influenced by the small numbers of patients and large proportion of indirect comparisons.
Further research with larger high-quality randomised controlled trials is required to provide further information about the efficacy of the different treatment options. Particularly in cases where there has not been any direct comparison.
Conclusion
Surgical interventions may be effective in providing short- to medium-term symptomatic relief for plantar fasciitis refractory to non-operative management. However, due to high study heterogeneity, the evidence is limited. The literature to date suggests minimal clinically significant difference between operative options, therefore we are unable to suggest a management algorithm. Further large randomised studies are required to ascertain the exact indications for the different procedures as well as long-term outcomes.
Availability of data and materials
Not applicable.
References
Monteagudo M, Albornoz PMd, Gutierrez B, Tabuenca J, Álvarez I (2018) Plantar fasciopathy: a current concepts review. EFORT Open Rev 3:485–493. https://doi.org/10.1302/2058-5241.3.170080
Buchanan BK, Kushner D (2021) Plantar fasciitis. In: StatPearls. StatPearls Publishing
Copyright © 2021, StatPearls Publishing LLC., Treasure Island (FL).
Riddle DL, Schappert SM (2004) Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Foot Ankle Int 25:303–310. https://doi.org/10.1177/107110070402500505
Crawford F, Thomson C (2003) Interventions for treating plantar heel pain. The Cochrane database of systematic reviews:Cd000416. https://doi.org/10.1002/14651858.Cd000416
Morrissey D, Cotchett M, Said J’Bari A, Prior T, Griffiths IB, Rathleff MS, Gulle H, Vicenzino B, Barton CJ (2021) Management of plantar heel pain: a best practice guide informed by a systematic review, expert clinical reasoning and patient values. Br J Sports Med. https://doi.org/10.1136/bjsports-2019-101970
Babatunde OO, Legha A, Littlewood C, Chesterton LS, Thomas MJ, Menz HB, van der Windt D, Roddy E (2019) Comparative effectiveness of treatment options for plantar heel pain: a systematic review with network meta-analysis. Br J Sports Med 53:182–194. https://doi.org/10.1136/bjsports-2017-098998%JBritishJournalofSportsMedicine
Neufeld SK, Cerrato R (2008) Plantar fasciitis: evaluation and treatment. J Am Acad Orthop Surg 16:338–346. https://doi.org/10.5435/00124635-200806000-00006
Luffy L, Grosel J, Thomas R, So E (2018) Plantar fasciitis: a review of treatments. 31:20-24.https://doi.org/10.1097/01.Jaa.0000527695.76041.99
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1. https://doi.org/10.1186/2046-4053-4-1
Landorf KB, Radford JA, Hudson S (2010) Minimal important difference (MID) of two commonly used outcome measures for foot problems. J Foot Ankle Res 3:7. https://doi.org/10.1186/1757-1146-3-7
Willis B (2009) Pain scale for plantar fasciitis. Foot Ankle J. https://doi.org/10.3827/faoj.2009.0205.0003
Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M (1994) Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 15:349–353. https://doi.org/10.1177/107110079401500701
SooHoo NF, Vyas R, Samimi D (2006) Responsiveness of the foot function index, AOFAS clinical rating systems, and SF-36 after foot and ankle surgery. Foot Ankle Int 27:930–934. https://doi.org/10.1177/107110070602701111
Ibrahim T, Beiri A, Azzabi M, Best AJ, Taylor GJ, Menon DK (2007) Reliability and validity of the subjective component of the American Orthopaedic Foot and Ankle Society clinical rating scales. J Foot Ankle Surg 46:65–74. https://doi.org/10.1053/j.jfas.2006.12.002
The Cochrane Collaboration (2020) Review manager (RevMan) Version 5.3. In.
EpiGear International (2016) Metal XL Version 5.3.
The Cochrane Collaboration (2011) Cochrane Handbook for Systematic Reviews of Interventions (Version 5.10)
Doi SAR, Barendregt JJ (2018) A generalized pairwise modelling framework for network meta-analysis. Int J Evid Based Healthc 16:187–194. https://doi.org/10.1097/xeb.0000000000000140
Sterne JAC, Sutton AJ, Ioannidis JPA, Terrin N, Jones DR, Lau J, Carpenter J, Rücker G, Harbord RM, Schmid CH, Tetzlaff J, Deeks JJ, Peters J, Macaskill P, Schwarzer G, Duval S, Altman DG, Moher D, Higgins JPT (2011) Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. 343:d4002.https://doi.org/10.1136/bmj.d4002%JBMJ
Gamba C, Serrano-Chinchilla P, Ares-Vidal J, Solano-Lopez A, Gonzalez-Lucena G, Ginés-Cespedosa A (2020) Proximal medial gastrocnemius release versus open plantar fasciotomy for the surgical treatment in recalcitrant plantar fasciitis. Foot Ankle Int 41:267–274. https://doi.org/10.1177/1071100719891979
Molund M, Husebye EE, Hellesnes J, Nilsen F, Hvaal K (2018) Proximal medial gastrocnemius recession and stretching versus stretching as treatment of chronic plantar heel pain. Foot Ankle Int 39:1423–1431. https://doi.org/10.1177/1071100718794659
Johannsen F, Konradsen L, Herzog R, Krogsgaard MR (2020) Endoscopic fasciotomy for plantar fasciitis provides superior results when compared to a controlled non-operative treatment protocol: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 28:3301–3308. https://doi.org/10.1007/s00167-020-05855-3
Othman AM, Hegazy IH (2015) Endoscopic plantar fasciotomy versus injection of platelet-rich plasma for resistant plantar fasciopathy. J Orthop 12:S176-181. https://doi.org/10.1016/j.jor.2015.10.015
Radwan YA, Mansour AM, Badawy WS (2012) Resistant plantar fasciopathy: shock wave versus endoscopic plantar fascial release. Int Orthop 36:2147–2156. https://doi.org/10.1007/s00264-012-1608-4
Rahbar M, Eslamian F, Toopchizadeh V, Aminabad F, Kargar A, Dolatkhah N (2018) A Comparison of the efficacy of dry-needling and extracorporeal shockwave therapy for plantar fasciitis: a randomized clinical trial. Iranian Red Crescent Medical Journal In Press. https://doi.org/10.5812/ircmj.68908
Uygur E, Aktaş B, Eceviz E, Yilmazoğlu EG, Poyanli O (2019) Preliminary Report on the role of dry needling versus corticosteroid injection, an effective treatment method for plantar fasciitis: a randomized controlled trial. J Foot Ankle surg 58:301–305. https://doi.org/10.1053/j.jfas.2018.08.058
Çatal B, Keskinbora M, Uysal MA, Şahin M, Gulabi D, Demiralp B (2017) Endoscopic plantar fasciotomy; deep fascial versus superficial fascial approach: a prospective randomized study. J Foot Ankle Surg 56:1001–1008. https://doi.org/10.1053/j.jfas.2017.04.021
Feng SM, Song RL, Wang AG, Sun QQ, Zhang SC (2021) Endoscopic partial plantar fasciotomy via 2 medial portals vs mini-open procedure for refractory plantar fasciitis. Foot Ankle Int 42:458–463. https://doi.org/10.1177/1071100720964805
Othman AM, Ragab EM (2010) Endoscopic plantar fasciotomy versus extracorporeal shock wave therapy for treatment of chronic plantar fasciitis. Arch Orthop Trauma Surg 130:1343–1347. https://doi.org/10.1007/s00402-009-1034-2
Tay KS, Ng YCS, Singh IR, Chong KW (2012) Open technique is more effective than percutaneous technique for TOPAZ radiofrequency coblation for plantar fasciitis. Foot Ankle Surg 18:287–292. https://doi.org/10.1016/j.fas.2012.05.001
Chou AC, Ng SY, Koo KO (2016) Endoscopic plantar fasciotomy improves early postoperative results: a retrospective comparison of outcomes after endoscopic versus open plantar fasciotomy. J Foot Ankle Surg 55:9–15. https://doi.org/10.1053/j.jfas.2015.02.005
Chou AC, Ng SY, Su DH, Singh IR, Koo K (2016) Radiofrequency microtenotomy is as effective as plantar fasciotomy in the treatment of recalcitrant plantar fasciitis. Foot Ankle Surg 22:270–273. https://doi.org/10.1016/j.fas.2015.11.006
Huang DM, Chou AC, Yeo NE, Singh IR (2018) Radiofrequency microtenotomy with concurrent gastrocnemius recession improves postoperative vitality scores in the treatment of recalcitrant plantar fasciitis. Ann Acad Med Singapore 47:509–515
Monteagudo M, Maceira E, Garcia-Virto V, Canosa R (2013) Chronic plantar fasciitis: plantar fasciotomy versus gastrocnemius recession. Int Orthop 37:1845–1850. https://doi.org/10.1007/s00264-013-2022-2
Wang W, Rikhraj IS, Chou ACC, Chong HC, Koo KOT (2018) Endoscopic plantar fasciotomy vs open radiofrequency microtenotomy for recalcitrant plantar fasciitis. Foot Ankle Int 39:11–17. https://doi.org/10.1177/1071100717732763
Yuan Y, Qian Y, Lu H, Kou Y, Xu Y, Xu H (2020) Comparison of the therapeutic outcomes between open plantar fascia release and percutaneous radiofrequency ablation in the treatment of intractable plantar fasciitis. J Orthop Surg Res 15:55. https://doi.org/10.1186/s13018-020-1582-2
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13. https://doi.org/10.1186/1471-2288-5-13
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135. https://doi.org/10.1186/1471-2288-14-135
JPT H, S G (2008) Cochrane handbook for systematic reviews of interventions.
Landorf KB, Radford JA (2008) Minimal important difference: values for the foot health status questionnaire, foot function index and visual analogue scale. Foot 18:15–19. https://doi.org/10.1016/j.foot.2007.06.006
Chan HY, Chen JY, Zainul-Abidin S, Ying H, Koo K, Rikhraj IS (2017) Minimal clinically important differences for american orthopaedic foot and ankle society score in hallux valgus surgery. Foot Ankle Int 38:551–557. https://doi.org/10.1177/1071100716688724
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by SN and HA. The first draft of the manuscript was written by SN and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nayar, S.K., Alcock, H. & Vemulapalli, K. Surgical treatment options for plantar fasciitis and their effectiveness: a systematic review and network meta-analysis. Arch Orthop Trauma Surg 143, 4641–4651 (2023). https://doi.org/10.1007/s00402-022-04739-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04739-0