Abstract
Introduction
There have been no previous studies comparing serial radiologic results between primary and revision Bankart repair despite the significance of capsulolabral height and slope restoration. The purpose of this study was (1) to compare serially the height and slope of the repaired labrum in the early postoperative period among primary and revision Bankart repair groups, and (2) to compare clinical outcomes between the two groups.
Materials and methods
This study included each 24 patients who underwent arthroscopic primary Bankart repair (Group A) and revision Bankart repair (Group B) matched by age, sex, and glenoid defect ratio. Postoperative serial radiologic assessment of the repaired labral height and slope was proceeded using magnetic resonance imaging (MRI) or computed tomographic arthrography (CTA) at 3 weeks and 6 months.
Results
There were no significant differences in labral height and slope at 3 weeks and 6 months postoperatively in Group A. However, significant reductions in labral height and slope were evident between 3 weeks and 6 months postoperatively in Group B (P < 0.05). Group A yielded superior results to Group B with respect to labral height and slope at each time point (P < 0.05) in between-group analyses. The clinical outcomes were not significantly different between the two groups except for the patients’ return to their premorbid sports activity level (P = 0.024).
Conclusions
The height and slope of the repaired capsulolabral structures in the early postoperative period after arthroscopic revision Bankart repair group were significantly lower than those of the primary Bankart repair group. Also the reduction of labral height and slope was significant in the revision Bankart repair group over time. Nonetheless, clinical outcomes did not differ significantly except return to premorbid sports activity level at final follow-up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The labrum of shoulder is a fibrocartilaginous structure attached to the rim of the glenoid, which functions as a static stabilizer for the shoulder joint [9, 33]. This labrum contributes to shoulder stability by deepening the glenoid fossa [14] and serving as a ‘chock block’ that limits excessive rollback of the humeral head [12, 23]. Detachment of the anteroinferior capsulolabral complex is defined as a ‘Bankart lesion’ in patients with traumatic anterior instability of the shoulder joint [3]. Arthroscopic capsulolabral reattachment or reconstruction (Bankart repair) using suture anchors is regarded as the treatment of choice for this lesion in the setting of anterior shoulder instability when the glenoid bone loss is less than 20–25% [1, 13, 19, 29, 35].
In previous studies, recurrence of instability after primary arthroscopic Bankart repair has been reported to occur in 5–33% of patients [7, 11, 17]. When considering a revision surgery, concomitant pathologies, such as bony glenoid defects, Hill–Sachs lesions, re-injured capsulolabral complex, and residual suture and anchor materials from the primary surgery, are considered potentially problematic [17, 21, 24, 27]. In both primary and revision stabilization surgeries, a definitive bony augmentation procedure is recommended if the anteroinferior glenoid defect is larger than 20–25% [15, 28, 29], but restoration of the labrum buttress and joint congruency with capsulolabral repair is considered the most important factor when the anteroinferior glenoid bone loss is less than 20% [10, 36]. Arthroscopic revision Bankart repair is, therefore, performed in carefully selected cases, and the results have generally been reported to be relatively good [2, 18]. Nonetheless, previous studies reported that revision surgery yielded inferior clinical results compared to primary stabilization surgery [20, 31].
In addition to clinical assessment of surgical outcomes, several studies have evaluated objective (quantitative) postoperative radiologic outcomes in the early postoperative period after primary arthroscopic Bankart repair [26, 36]. These investigations included either assessment of maintenance of the repaired labral height and slope through serial follow-up MRI studies, or comparison of the labral height between the stable and unstable shoulders [26, 36]. However, there has been no report of serial radiologic measurements of changes in the repaired labral height and slope after arthroscopic revision Bankart repair, nor any comparison with the result after arthroscopic primary Bankart repair.
This study aimed (1) to compare serial measurements of the height and slope of the repaired labrum in the early postoperative period among revision and primary Bankart repair patients, and (2) to compare clinical outcomes between the two patient groups during the study period. We hypothesized that (1) the revision Bankart repair group would achieve less complete restoration of labral height and slope, compared to the primary Bankart repair group, and (2) nonetheless, the revision Bankart repair group would have comparable clinical outcomes and recurrence rates to those of the primary Bankart repair group except with respect to the patients’ premorbid sports activity level.
Materials and methods
Study population
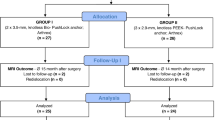
This retrospective study included 249 patients with anterior shoulder instability and 20% or less glenoid bone defects who underwent either arthroscopic primary or revision Bankart repair performed by a single senior surgeon from March 2009 to April 2017. The indication for surgery was a positive apprehension sign in 90° abduction and 90° external rotation of the shoulder as well as discomfort in daily-living activities. Additional remplissage procedure was performed in cases with either an off-track lesion detected on preoperative evaluation or a positive engagement test during arthroscopic examination. The inclusion criteria were (1) 20% or less glenoid bone defect on preoperative enface 3-dimensional computed tomography (CT) imaging, [32] (2) availability of at least 2 years of follow-up data, and (3) serial follow-up magnetic resonance image (MRI) or computed tomography arthrography (CTA) imaging available at 3 weeks and 6 months after surgery. Exclusion criteria were (1) at least two years of follow-up data not available (n = 31), (2) lack of follow-up images (n = 22), (3) combined rotator cuff tear (n = 5), and (4) combined posterior or multi-directional instability (n = 6).
From the pool of 202 patients who met the above inclusion and exclusion criteria, 24 patients who underwent revision arthroscopic Bankart repair were enrolled as Group B. Another 24 patients from among the remaining patients who underwent primary arthroscopic Bankart repair were matched by age, sex, and glenoid defect with Group B, and they were enrolled as Group A. The matching procedure was performed blind to guarantee sorting of patients in accordance with the matching parameters without bias in their outcomes. The criteria for matching are the same gender, the glenoid defect difference was within 3%, and the age difference was within 3 years. The patients’ medical records, including radiologic images, were reviewed. Our institutional review board approved this study after waiving the requirement for the informed consent.
Radiologic assessments
Preoperative radiologic imaging for all patients included true anteroposterior and axillary radiographic views of the shoulder, MRI or MR arthrography, and 3D CT (Somatom Sensation 64; Siemens, Erlangen, Germany). The size of the glenoid bone defect as seen on the en-face view of the glenoid was measured using a picture archiving and communication system (Centricity PACS; GE Medical System Information Technologies, Milwaukee, WI). The estimation of the amount of glenoid bone loss was performed using the method reported by Sugaya et al. [32],
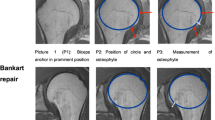
All patients underwent serial postoperative follow-up MRI or CTA at 3 weeks and 6 months after surgery to estimate the labral height and slope and angle on axial and oblique coronal images at the anteroinferior portion of the glenoid (5 mm above the most inferior anchor). [36] Labral height was defined as the distance (in millimeters) between the lowest portion of the glenoid and the tip (i.e., maximum height) of the labrum (Fig. 1) [18, 36]. The slope was defined as the angle formed by a tangential line drawn from the lowest portion of the glenoid (center of the glenoid) to the tip of the labrum (Fig. 2) [18, 36]. All measurement was performed using a picture archiving and communication system (PACS; GE Healthcare, Chicago, Illinois) to complete automated computer calculation of distance and angle using mouse pointer cursors. As a continuous variable of each value, the intraclass correlation coefficient (ICC) for agreement was calculated by the two shoulder fellows for the labral height and labral slope values.
Functional assessments
Functional assessments were performed at each visit using the following metrics: subjective shoulder value (SSV; in which patients estimate the value of the affected shoulder as a percentage of the value of the normal shoulder) and Rowe score [13, 30]. Among them, Rowe score was used to confirm the clinical significance of outcomes in reflection of a minimal clinically important difference (MCID). An independent examiner who was blinded to group assignment rated the pre- and postoperative shoulder functional scores and measured the active range of motion (ROM) for the following: forward flexion in the scapular plane, external rotation with the elbow at the side, and external and internal rotation in 90° of abduction. Recurrence of instability was defined as re-dislocation, a subluxation episode, or finding a positive apprehension sign in 90° of abduction and 90° external rotation of the shoulder.
The level of sports/recreation activity able to be sustained when using the affected shoulder was also evaluated. Patients were asked to rate postoperative activity level as a percentage of the premorbid level using the following rating system: Grade I, no limitations of sports/recreation activity (100% of premorbid level); Grade II, mild limitations in sports/recreation activity (> 90% of premorbid level); Grade III, moderate limitation of sports/recreation activity (> 70% of premorbid level); and Grade IV, severe limitation (< 70% of premorbid level) or inability to return to previous sports/recreation activity. [4]
Operative procedures
Either arthroscopic primary Bankart repair or revision Bankart repair was performed by a senior surgeon under general anesthesia with the patient in the lateral decubitus position with 10-lb longitudinal traction. A standard posterior portal was created first, followed by a low anterior portal. An 8.5-mm cannula (Cleartrac Complete Cannula System; Smith & Nephew, Andover, MA) was placed over the lateral half of the subscapularis tendon. A superior portal was then established around the anterior portion of lateral edge of the acromion after trial with a spinal needle. Viewing from the superior portal, Bankart lesion was identified. An electrocautery device was introduced through the low anterior portal, releasing and mobilizing the detached anteroinferior labrum sufficiently, allowing for identifying the subscapularis muscle and being brought up on the glenoid so as to recreate the labral bumper. The glenoid neck and rim were prepared, and the first suture anchor was inserted onto the glenoid at the 5:00 or 5:30 clock-face position of the glenoid rim in a right shoulder (7:00 or 6:30 clock-face position in a left shoulder). Using a suture passer or hook, a suture was passed through the capsule, about 1 cm inferior to the suture anchor. Then, after shuttle relay, a secure knot was placed on the capsular side of repaired labrum. The subsequent two or three suture anchors were inserted in a row and secured in the same manner.
Postoperative rehabilitation
In Group A (primary Bankart repair), the affected arm was kept in a brace for 4 to 5 weeks after surgery. Pendulum or self-assisted circumduction exercises were initiated on the day after surgery. After brace removal, self-assisted passive range-of-motion exercises and stretching exercises were introduced as tolerated. Self-assisted active range-of-motion exercises were allowed beginning at 6 to 8 weeks after surgery, and isotonic strengthening exercises using an elastic band were added 3 months after surgery. Six months after their surgery, patients were allowed to gradually return to sports/recreation activities. All patients were educated on the risk of recurrence of instability when participating in highly active sports and recreation activities. In Group B (revision Bankart repair), with the exception of absolute immobilization of the affected arm for the first 6 weeks after surgery, the rehabilitation protocol was the same as for Group A.
Statistical analyses
All statistical analyses were performed with the SPSS® program (IBM SPSS Statistics, version 25.0; IBM, Armonk, NY). A Wilcoxon signed rank test was used to compare the postoperative radiologic results at 3 weeks and 6 months within the two groups. The Mann–Whitney U test was used to compare the clinical and radiologic results between the two groups. Categorical data were compared by use of the Chi-squared or Fisher’s exact test. Interobserver reliabilities were calculated using intraclass correlation coefficients. Statistical significance was set at P < 0.05. The Rowe score was used as a primary outcome for sample size calculation. The calculation was performed according to previously determined on the MCID 9.7 in Rowe score [25]. In the setting of effect size of 0.65, a power of 0.8, the calculation showed minimum of 22 patients requiring for each group.
Results
Patient demographics, arthroscopic findings and concomitant procedure
All patients included in either group were male. The mean age was 25.1 years in Group A and 26.8 years in Group B. The mean duration of follow-up after surgical treatment was 51.2 (range, 24–102) months in Group A and 48.4 (range, 24–98) months in Group B. The mean Beighton and Horan score [5] was 2.8 in Group A and 3.2 in Group B. A superior labrum anterior and posterior (SLAP) lesion requiring repair or tenodesis was found in 4 patients (16.7%) from Group A and 6 patients (25%) from Group B. Concomitant SLAP repair was performed using suture anchors. An additional remplissage procedure was performed in 3 patients (12.5%) from Group A and 8 patients (33.3%) from Group B. The mean size of glenoid defects was 14.9% (range, 9.5–17.9%) in patients from Group A and 15.6% (range, 10.2–18.7) in patients from Group B (Table 1). There were no significant differences in any metrics between the two groups.
Radiologic outcomes
The changes in the labral height and slope between 3 weeks and 6 months after surgery were not statistically significant in Group A. On the other hand, in Group B, the mean labral height and slope 6 months after surgery were significantly less than at 3 weeks after surgery (P < 0.05). The mean anterior labral height 3 weeks and 6 months after surgery was 6.1 and 5.7 mm, respectively, in Group A (P = 0.111), and 5.4 mm and 4.3 mm, respectively, in Group B (P < 0.001). The inferior labral height of 3 weeks and 6 months after surgery was 6.7 and 6.3 mm, respectively, in Group A (P = 0.075), and 6.0 and 5.2 mm, respectively, in Group B (P = 0.040). Similarly, the mean anterior labral slopes measured 3 weeks and 6 months after surgery were 21.8° and 20.6°, respectively, in Group A (P = 0.360), and 20.1° and 17.1°, respectively, in Group B (P < 0.001). For the inferior labral slopes, the measured mean values in Group A patients were 22.0° and 21.7° after 3 weeks and 6 months of recovery, respectively (P = 0.059), and 20.2° and 18.2° in Group B patients after 3 weeks and 6 months of recovery, respectively (P < 0.001). Comparing the labral height and slope between the two groups at each time point, the results of Group B were all inferior to those of Group A (P < 0.05). The measured values are summarized in Tables 2 and 3.
Functional outcomes
Recurrent instability occurred in 1 of 24 (4.2%) patients in Group A and 3 of 24 (12.5%) patients in Group B (P = 0.608). The one patient with recurrence in Group A had a positive apprehension sign on examination during the follow-up period, but had no history of a traumatic event. In Group B, 2 patients sustained a dislocation and 1 patient had a positive apprehension sign on examination after a minor traumatic event.
The mean SSV significantly improved from 41.9 to 90.6 in Group A (P < .001), and from 38.8 to 82.5 in Group B (P < 0.001). The mean Rowe score also improved from 47.9 to 91.3 in Group A (P < 0.001) and from 41.3 to 84.2 in Group B (P < 0.001). However, none of these preoperative and postoperative shoulder functional values were significantly different between the groups. (Table 4). In terms of MCID for clinical significance in Rowe score, the minimum change of Rowe score in this study was 10 points and 100% of patients (48/48) achieved the MCID.
Regarding the assessment of the patients’ return to their premorbid activity levels, in Group A, 11 patients reported being able to maintain activity at a Grade I level, 9 patients were Grade II, 3 patients were Grade III, and 1 patient was Grade IV. In Group B, there were 2 patients who reported Grade I activity, 13 with Grade II, 7 with Grade III, and 2 with Grade IV. There was a statistically significant difference between the two groups (P = 0.024; Table 4).
There were no significant differences between the two groups with respect to the measured active ranges of motion of the shoulders at the time of preoperative evaluation and final follow-up (Table 5).
Discussion
The most important findings of the current study were that the reduction in labral height and slope was significant in the revision Bankart repair group. Nonetheless, these differences between the two groups were not correlated with clinical outcomes, except with respect to return to premorbid sports activity level.
Several investigators have indicated that postoperative labral height is correlated with clinical outcomes [20, 26, 36]. Yoo et al. [36] indicated that the repaired buttress was more prominent in stable shoulders than in shoulders with anterior instability, and the restoration of labral height and slope is important in both primary and revision Bankart repair. However, Krueger et al. [20] indicated that the tissue quality in revision cases is likely to be stiff and poor, and it may lead to difficulty in holding and shifting the sufficient tissue and achieving labral height for reconstructing the capsulolabral complex in Bankart repair. In the current study, although there were statistical differences in the labral height and slope when assessed 3 weeks after surgery, these numerical differences of about 1 mm or 1–2° did not seem to be clinically meaningful. In contrast, meticulous and sufficient release of the capsulolabral complex could facilitate the better than expected restoration of the labral height and slope even in revision Bankart repair.
Although there has been no previous study investigating shoulder stiffness induced by a recent dislocation or subluxation episode in patients with anterior shoulder instability, we think that stiffness arising from recent injury may make it difficult to gain sufficient mobility of the capsulolabral complex (namely, Bankart lesion) even after release. Thus, in such cases, we have been working to make the affected shoulder as supple as the contralateral shoulder before surgery, regardless of whether primary or revision surgery is to be undertaken. Also, in case of revision surgery, the release of adhered capsulolabral complex is performed at the 6 o’clock position or over the affected labral lesion to achieve sufficient capsular shift, in addition to completing the Bankart repair. However, in this study, despite absolute immobilization of the affected shoulder in the revision cases during the early postoperative period, the labral height and slope were not maintained in the early postoperative period.
There have been conflicting reports regarding the maintenance of the repaired labral height and slope after surgery.[16, 22, 26, 31] Park et al. [26] reported that the repaired labral height decreased over time on serial CT arthrography from 3 months to 1 year after surgery. Interestingly, the reduction was more significant in the patients with poor tissue quality, although the determination of tissue quality is inevitably subjective and cannot be quantitative. On the other hand, Yoo et al. [36] indicated that the repaired labral height and slope were maintained in the early postoperative period (between 6 weeks and 6 months); in addition, repaired labral height and slope in stable shoulders were significantly more prominent than in shoulders with recurrent instability after surgery. In the current study, labral height and slope were maintained in the primary repair group in the early postoperative period, but not in the revision Bankart repair group. As Park et al. indicated, the tissue quality in the revision group was not robust as in primary group, and this might lead to significant reduction in labral height and slope.
Nonetheless, there was no significant difference in the Rowe score and recurrence of instability between the two groups. The additional remplissage indicated in either positive engagement test at the time of surgery or off-track lesion at preoperative planning was more often in the revision Bankart repair group, but there was no statistical significance. The ROM at final follow-up did not differ significantly between the groups, either. However, regarding return to premorbid sports activity level, the revision Bankart repair group had significantly inferior outcomes.
Our study population was drawn from the general community, and did not include professional athletes or patients with high functional demands, so their physical demands or expectations of participation in sports or strenuous activity were moderate to low. People who have repeatedly experienced dislocations generally tend to modify their level of participation in sports after surgery, due to fear or anxiety about recurrence; patients who experience subjective failure of surgical treatment tend to have increasing lack of confidence in their shoulder function and a negative attitude when answering questions on the evaluation of clinical scores [8]. Likewise, other studies [6, 34] have reported psychological atrophy for return to sports activity and passive attitude toward rehabilitation after surgical repair. Similar psychological concerns may underlie the difference in the percentage of patients reporting they were able to return to the level of sports activity they undertook prior to surgery, despite good clinical functional outcomes.
This study has several limitations to address. First, the study design was retrospective in nature, with a small sample size, which might lead to type II error related to low statistical power. Second, the study findings should be interpreted with care: although not intended, this study included only male community-based patients with moderate to low physical demands, and not females, or professional athletes or other high-demand patients. Third, for the radiologic evaluation modality used in this study periods, MRI and CT arthrography were mixed. Fourth, there was a difference in immobilization period between the two groups.
Conclusions
The height and slope of the repaired capsulolabral structures in the early postoperative period after arthroscopic revision Bankart repair group were significantly lower than those of the primary Bankart repair group. Also the reduction of labral height and slope was significant in the revision Bankart repair group over time. Nonetheless, clinical outcomes did not differ significantly except return to premorbid sports activity level at final follow-up.
References
Ahmed I, Ashton F, Robinson CM (2012) Arthroscopic Bankart repair and capsular shift for recurrent anterior shoulder instability: functional outcomes and identification of risk factors for recurrence. J Bone Joint Surg Am 94:1308–1315
Arce G, Arcuri F, Ferro D, Pereira E (2012) Is selective arthroscopic revision beneficial for treating recurrent anterior shoulder instability? Clin Orthop Relat Res 470:965–971
Bankart ASB (1938) The pathology and treatment of recurrent dislocation of the shoulder-joint. Br J Surg 26:23–29
Bartl C, Scheibel M, Magosch P, Lichtenberg S, Habermeyer P (2011) Open repair of isolated traumatic subscapularis tendon tears. Am J Sports Med 39:490–496
Beighton P, Horan F (1969) Orthopaedic aspects of the Ehlers-Danlos syndrome. J Bone Joint Surg Br 51:444–453
Blonna D, Bellato E, Caranzano F, Assom M, Rossi R, Castoldi F (2016) Arthroscopic Bankart repair versus open Bristow-Latarjet for shoulder instability: a matched-pair multicenter study focused on return to sport. Am J Sports Med 44:3198–3205
Boileau P, Villalba M, Héry JY, Balg F, Ahrens P, Neyton L (2006) Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am 88:1755–1763
Buckup J, Welsch F, Gramlich Y, Hoffmann R, Roessler PP, Schuttler KF, Stein T (2018) Back to sports after arthroscopic revision Bankart repair. Orthop J Sports Med 6:2325967118755452
Burkart AC, Debski RE (2002) Anatomy and function of the glenohumeral ligaments in anterior shoulder instability. Clin Orthop Relat Res 400:32-39
Burkhart SS, Debeer JF, Tehrany AM, Parten PM (2002) Quantifying glenoid bone loss arthroscopically in shoulder instability. Arthroscopy 18:488–491
Cho NS, Hwang JC, Rhee YG (2006) Arthroscopic stabilization in anterior shoulder instability: collision athletes versus noncollision athletes. Arthroscopy 22:947–953
Fehringer EV, Schmidt GR, Boorman RS, Churchill S, Smith KL, Norman AG, Sidles JA, Matsen FA 3rd (2003) The anteroinferior labrum helps center the humeral head on the glenoid. J Shoulder Elbow Surg 12:53–58
Gerber C, Fuchs B, Hodler J (2000) The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am 82:505–515
Howell SM, Galinat BJ (1989) The glenoid-labral socket. A constrained articular surface. Clin Orthop Relat Res 243:122–125
Itoi E, Lee SB, Berglund LJ, Berge LL, An KN (2000) The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am 82:35–46
Kim JY, Chung SW, Kwak JY (2014) Morphological characteristics of the repaired labrum according to glenoid location and its clinical relevance after arthroscopic Bankart repair: postoperative evaluation with computed tomography arthrography. Am J Sports Med 42:1304–1314
Kim SH, Ha KI, Cho YB, Ryu BD, Oh I (2003) Arthroscopic anterior stabilization of the shoulder: two to six-year follow-up. J Bone Joint Surg Am 85:1511–1518
Kim SH, Ha KI, Kim YM (2002) Arthroscopic revision Bankart repair: a prospective outcome study. Arthroscopy 18:469–482
Kim SH, Jung W, Rhee SM, Kim JU, Oh JH (2020) Outcomes of arthroscopic capsulolabral reconstruction for anterior instability with greater than 20% glenoid bone defects: are Latarjet procedures absolutely indicated for these patients? Clin Shoulder Elb 23:62–70
Krueger D, Kraus N, Pauly S, Chen J, Scheibel M (2011) Subjective and objective outcome after revision arthroscopic stabilization for recurrent anterior instability versus initial shoulder stabilization. Am J Sports Med 39:71–77
Lee J-H, Kang J-S, Park I, Shin S-J (2021) Serial changes in perianchor cysts following arthroscopic labral repair using all-suture anchors. Clin Orthop Surg 13:229–236
Lee SJ, Kim JH, Gwak HC, Kim CW, Lee CR, Jung SH, Kwon CI (2020) Influence of glenoid labral bumper height and capsular volume on clinical outcomes after arthroscopic Bankart repair as assessed with serial CT arthrogram: can anterior-inferior volume fraction be a prognostic factor? Am J Sports Med 48:1846–1856
Lippitt S, Matsen F (1993) Mechanisms of glenohumeral joint stability. Clin Orthop Relat Res 291:20–28
Mardani-Kivi M, Alizadeh A, Asadi K, Izadi A, Leili EK, arzpeyma SF, (2022) Can indirect magnetic resonance arthrography be a good alternative to magnetic resonance imaging in diagnosing glenoid labrum lesions?: a prospective study. Clin Shoulder Elbow 25:182–187
Park I, Oh MJ, Shin SJ (2019) Minimal clinically important differences and correlating factors for the Rowe score and the American shoulder and elbow surgeons score after arthroscopic stabilization surgery for anterior shoulder instability. Arthroscopy 35:54–59
Park JY, Lee SJ, Lhee SH, Oh JH (2012) Change in labrum height after arthroscopic Bankart repair: correlation with preoperative tissue quality and clinical outcome. J Shoulder Elbow Surg 21:1712–1720
Patel RV, Apostle K, Leith JM, Regan WD (2008) Revision arthroscopic capsulolabral reconstruction for recurrent instability of the shoulder. J Bone Joint Surg Br 90:1462–1467
Piasecki DP, Verma NN, Romeo AA, Levine WN, Bach BR Jr, Provencher MT (2009) Glenoid bone deficiency in recurrent anterior shoulder instability: diagnosis and management. J Am Acad Orthop Surg 17:482–493
Provencher MT, Bhatia S, Ghodadra NS, Grumet RC, Bach BR Jr, Dewing CB, LeClere L, Romeo AA (2010) Recurrent shoulder instability: current concepts for evaluation and management of glenoid bone loss. J Bone Joint Surg Am 92(Suppl 2):133–151
Rowe CR, Patel D, Southmayd WW (1978) The Bankart procedure: a long-term end-result study. J Bone Joint Surg Am 60:1–16
Stein T, Buckup J, Mehling AP, Hoffmann R, Efe T, von Eisenhart-Rothe R, Welsch F (2014) Restoration of joint congruency and the glenoidal labrum after arthroscopic revision Bankart repair: a MRI match-paired analysis comparing primary Bankart repair and the uninjured labrum. Arch Orthop Trauma Surg 134:1121–1134
Sugaya H, Moriishi J, Kanisawa I, Tsuchiya A (2005) Arthroscopic osseous Bankart repair for chronic recurrent traumatic anterior glenohumeral instability. J Bone Joint Surg Am 87:1752–1760
Turkel SJ, Panio MW, Marshall JL, Girgis FG (1981) Stabilizing mechanisms preventing anterior dislocation of the glenohumeral joint. J Bone Joint Surg Am 63:1208–1217
Warth RJ, Briggs KK, Dornan GJ, Horan MP, Millett PJ (2013) Patient expectations before arthroscopic shoulder surgery: correlation with patients’ reasons for seeking treatment. J Shoulder Elbow Surg 22:1676–1681
Yamamoto N, Itoi E (2015) Osseous defects seen in patients with anterior shoulder instability. Clin Orthop Surg 7:425–429
Yoo JC, Lee YS, Tae SK, Park JH, Park JW, Ha HC (2008) Magnetic resonance imaging appearance of a repaired capsulolabral complex after arthroscopic Bankart repair. Am J Sports Med 36:2310–2316
Funding
This study was supported by a faculty research grant of Yonsei University College of Medicine (6–2016-0179).
Author information
Authors and Affiliations
Contributions
H-ML was involved in writing—original draft, conceptualization, data curation, formal analysis, investigation, resources, visualization, approval of the submitted and final versions. J-RL helped in writing—original draft, writing—review & editing, conceptualization, approval of the submitted and final versions. T-HY contributed to conceptualization, supervision, visualization, approval of the submitted and final versions. W-WL was involved in data curation, resources, visualization, approval of the submitted and final versions. S-JK helped in methodology, supervision, approval of the submitted and final versions. Y-MC contributed to conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, resources, visualization, writing—original draft, writing—review & editing, approval of the submitted and final versions. All authors have read and approved the final submitted manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical approval
IRB (4–2020-0936).
Informed consent
Our institutional review board approved this study after waiving the requirement for the informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, HM., Lim, JR., Lee, WW. et al. Comparison of arthroscopic primary and revision Bankart repair for capsulolabral restoration: a matched-pair analysis. Arch Orthop Trauma Surg 143, 3183–3190 (2023). https://doi.org/10.1007/s00402-022-04651-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04651-7