Abstract
Introduction
Hip fracture patients are fragile, and the majority fail to fully recover to their pre-fracture functional level, resulting in an increase in institutionalization. We aimed to investigate risk factors for being dependent at discharge and for failure to return to independent living 12 months after a hip fracture.
Materials and methods
From 2011 to 2017, all surgically treated hip fracture patients admitted from their own homes were included in this prospective cohort study. Patient characteristics were registered, including age, sex, lifestyle, comorbidities, pre-fracture New Mobility Score (NMS), biochemical measures, fracture type, and surgical method. Dependency was measured at discharge using a cumulated ambulatory score (CAS < 6) and the timed-up-and-go test (TUG > 20 s). At 12 months, patients were interviewed regarding residence, NMS, and care needs. Multivariable logistic regression was used, reporting odds ratio (OR) with 95% confidence intervals (CI).
Results
A total of 2006 patients were included in the study with data regarding their hospital stay and discharge. In all, 1342 patients underwent follow-up at 12 months. The risk factors found to be associated with dependency at discharge were mostly static. Modifiable variables associated with dependency at discharge (CAS < 6) were hypoalbuminemia (OR: 1.94, 95% CI 1.38–2.71), not having been mobilized to standing within 24 h (OR: 1.88, 95% CI 1.12–3.15), and general anesthesia (OR: 1.35, 95% CI 1.07–1.71). Failure to return to independent living at 12 months was found in 10% of the patients, and was primarily associated with patient characteristics and proxy variables for comorbidities, but also with dependency at discharge (CAS < 6).
Conclusions
Mobilizing patients to standing within 24 h from hip fracture surgery was vital in maximizing short-term functional recovery. Failure to return to independent living was seen in the frailest patients. However, the majority remained in their own home with little increase in care needs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The World Health Organization (WHO) and the United Nations have coined 2021–2030 the decade of healthy aging [1]. The WHO defines this as: "the process of developing and maintaining the functional ability that enables wellbeing in older age" [1]. The WHO highlights functional ability, including meeting basic needs and being mobile as key terms [1]. However, for the patient sustaining a hip fracture is a catastrophic event and often associated with adverse outcomes including disability and mortality. Hip fractures often lead to deterioration in function with increased care needs that make independent living impossible and results in institutionalization. In Western countries, 10–36% of patients sustaining a hip fracture are institutionalized within 12 months after their fracture [2,3,4]. Previous studies have identified risk factors for failure to return to independent living, such as age, cognitive status, comorbidities, and pre-fracture functional level [5,6,7]. Additionally, a recent study found that a low functional level at discharge predicted failure to return to independent living 12 months after the hip fracture [4].
Early identification of patients at specific risk of functional loss and long-term institutionalization due to hip fracture is important. However, hip fracture patients’ short-term functional recovery has not previously been in focus, since most studies have investigated only predictors of long-term functional recovery [10,11,12]. One focus of hip fracture treatment should be timely and focused rehabilitation aiming at regaining pre-fracture function, enabling patients to remain in their own homes and preserve their independence. A key element in the improvement of functional recovery after hip fracture surgery is identification of modifiable risk factors that may be targeted by interventions. However, systemic reviews have highlighted the lack of consistent findings regarding risk factors for poor functional recovery [8, 9].
The present study aimed to describe risk factors for dependency at discharge in a hospital setting with a short length of stay (LOS) and subsequent failure to return to independent living at 12 months following hip fracture surgery.
Patients and methods
This was an observational cohort study using prospectively and consecutively collected data from the Holstebro Hip Fracture Database, Denmark. Patients were included in the Hip Fracture Database if they were surgically treated for a hip fracture (femoral neck fracture, intertrochanteric fracture, or subtrochanteric fracture) at our institution between June 2011 and December 2017. All patients in the database who were living independently in their own homes at the time of their hip fracture were considered for inclusion. Excluded were patients with non-fragility hip fracture (e.g., caused by pathology or high-energy trauma), not surgically treated, operated at another hospital, and patients who died during their acute hospital stay. If a patient experienced a second hip fracture during the study period, the second fracture was not included.
Data were gathered prospectively by nurses, physiotherapists, and doctors at four time points; the day of admission, day 1 post-operatively, the day of acute hospital discharge, and 12 months post-operatively. One project nurse double checked the registration papers and the database to ensure the date quality and completeness of data after the patient's discharge. Nurses, physiotherapists, and doctors were continuously trained in reporting to the database, thereby minimizing variation in reporting practices during the study period.
Patient characteristics
Age was categorized into < 75, 75–84, and ≥ 85 years. The patients' gender, residence, smoking status, weekly alcohol consumption, and any visual impairment were documented. Body Mass Index (BMI), derived from the patients' height and weight, was categorized based on the World Health Organization into underweight (< 18.5 kg/cm2), normal weight (18.5–25 kg/cm2), and overweight (> 25 kg/cm2) [13]. Height was primarily patient reported, whereas weight was obtained by weighing the patients. Fractures were grouped into intra- or extracapsular fractures based on pre-operative radiographs [14].
Proxy variables for comorbidities
Using the American Society of Anesthesiologists (ASA) classification system, the treating anesthesiologist assessed the patients' comorbidity status. ASA score was dichotomized into ASA 1–2 and ASA 3–5. Patients were divided into cognitively fit or cognitively impaired based on previous diagnoses of dementia or similar. Blood results included hemoglobin, albumin, and 25-hydroxy-vitamin D, with the lower limit at 10 g/dl for hemoglobin, 35 g/dl for albumin, and 50 µmol/l for 25-hydroxy-vitamin D. The pre-fracture functional level was based on the New Mobility Score (NMS) [15]. The NMS is a self-reported measure that categorizes a patient's ability to complete three functional activities: indoor walking, outdoor walking, and shopping. Each activity is given a score between 0 and 3, yielding a final score between 0 and 9, where 9 represents independent with no aid in all three activities, and 0 represents being unable to perform any of the activities. The NMS has a high inter-tester reliability, and a cut-off point of six has been shown to be predictive of functional recovery [16, 17]. Patients were divided into a high pre-fracture functional level with a score of 6 or above, and a low functional group with a score of 5 or below.
Hospital-related variables
Hospital-related variables included time to surgery, surgical method, type of anesthesia, mobilization to standing within 24 h of surgery, post-operative pain management, discharge destination, LOS, and all-cause readmission within the first year.
Patients were treated with either screws or total hip arthroplasty for femoral neck fractures, while patients with intertrochanteric fractures were treated with dynamic hip screw with or without trochanteric stabilizing plate or intramedullary nails. Subtrochanteric fractures were treated with intramedullary nails.
Physiotherapy was initiated on the first post-operative day on weekdays as well as during weekends with the intention to have the patient standing and with full weight-bearing from the first mobilization. However, if the surgeon assessed the fracture as unstable only partial weight-bearing was achieved. The first mobilization was documented; so was whether the patient was mobilized to standing—including any reason for not being mobilized to standing. Patients were categorized as no indication for mobilization, i.e., if they were without pre-fracture standing ability, had very complex fractures, or were admitted to the intensive care unit after surgery. Hence, these patients were not part of the analyses regarding mobilization.
Time to surgery was calculated from admission and divided into less than 24 h, 24–36 h, or more than 36 h from admission based on national guidelines [14, 18]. All fractures were surgically managed according to a previously published local protocol [19]. After surgery, patients either received only oral pain management with opioids (primarily morphine) and paracetamol or a combination of oral pain management and an epidural catheter in the initial three days.
Patients were primarily rehabilitated in the orthopedic ward and discharged with a rehabilitation plan and an individually assigned number of follow-up sessions with a municipal physiotherapist. Patients requiring extensive rehabilitation were discharged to a rehabilitation facility. Discharge destination was documented; own home, protective living, nursing home, rehabilitation, or transferred to another hospital.
Outcomes
The primary outcome was independence measured by the Cumulated Ambulation Score (CAS) assessed by the physiotherapist immediately before discharge. The CAS is a reliable outcome measure that evaluates a patient's ability to: get in and out of bed, sit down and stand up, and walk with or without a mobility aid [20, 21]. The scores for each task (0–2 points) are combined to provide a total score between 0 and 6, where 6 implies independence in all three tasks and 0 indicates the inability to perform any of the tasks despite assistance. Studies have demonstrated the CAS to be a valid predictor of functional recovery in patients with hip fracture [21, 22]. The total CAS score was dichotomized into whether the patient regained complete independence (CAS = 6) or not (CAS score ≤ 5) [22]. At discharge, patients also had a timed-up-and-go (TUG) test. The TUG test measures the time in seconds that a person requires to rise from a standardized chair, walk 3 m with or without the use of walking aids, and return to the chair and sit down [23]. The TUG test is a reliable outcome measure that has been demonstrated to predict functional outcomes after a hip fracture [24, 25]. Based on previous research, a cut-off point of 20 s was chosen, meaning that a TUG test of less than 20 s indicated independence [23, 26, 27].
All patients who were alive 12 months after surgery received a telephone call by a project nurse; 77% of the surviving patients or their close relatives or caregivers were reached. A standardized questionnaire was completed, and it was documented if the patients had changed residence. Patients had changed residence if they had moved from independent living to either protective living or to a nursing home at the 12-month follow-up, with the hip fracture being the primary reason for the change of residence. Furthermore, the respondent was asked about changes in care needs compared with their care need prior to their hip fracture.
Statistical analysis
Continuous variables were presented as median with interquartile range (IQR). Categorical variables were summarized as frequencies and percentages. A univariable logistic regression analysis was conducted to explore risk factors for dependency at discharge and failure to return to independent living. The independent variables are presented in Table 1. Furthermore, CAS and TUG were used as independent variables in the analysis of failure to return to independent living. The dependent variables were CAS = 6 and TUG < 20 s for dependency at discharge and failure to return to independent living at 12 months. Multivariable logistic regression was conducted adjusting for age, gender, ASA score, cognitive function, pre-fracture functional level, mobilization, and fracture type reporting odds ratio (OR) with 95% confidence intervals (95% CI). All analyses were conducted using the statistical package STATA version 17.
Ethics
The study was registered with the national data protection agency; under national law, there is no requirement for written consent for non-interventional studies. The study was funded by the department only and received no external funding. The authors have no conflicts of interest to declare.
Results
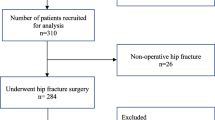
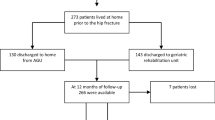
In the study period, 3047 patients were diagnosed with a hip fracture at our institution. Among these, 1047 patients were excluded, and 2006 patients were included in the study of short-term functional recovery (Fig. 1). Clinical characteristics of the 2006 eligible patients are presented in Table 1. Within the first year, 253 patients died and 411 were lost to follow-up, which left 1342 patients for the analyses of risk factors for failure to return to independent living (Fig. 1).
Dependency at discharge
The median CAS was 4 (IQR: 3), with 613 (31%) patients being independent at discharge (CAS = 6). Multiple risk factors were identified for CAS ≤ 5 after adjusting for confounders. For patient characteristics; older age, overweight, extracapsular fractures, and pre-fracture NMS ≤ 5 were associated with an increased risk of being dependent at discharge (Table 2). For proxy variables for comorbidity, high ASA score, cognitive impairment, and hypoalbuminemia were associated with increased risk of being dependent at discharge (Table 2). For hospital-related variables; not having been mobilized to standing within 24 h, displaced intracapsular fracture treated with total hip arthroplasty (THA), transfer to another hospital, and longer LOS were associated with an increased risk for being dependent at discharge (Table 2). Only 398 (20%) patients could perform TUG at discharge, and only 84 (21%) of the patients performed it in less than 20 s. More patients treated with THA were able to perform the TUG test and complete it within 20 s (p < 0.001). Extracapsular fracture and post-operative anemia were associated with an increased risk of dependency measured by TUG > 20 s at discharge (Table 2).
A total of 13 (1%) patients were discharged without walking aids, 90% were discharged with a walking aid, and 9% were discharged without walking ability.
Failure to return to independent living
The 1 year questionnaires were completed via a telephone interview with the patient in 83% (1.114 patient) of the cases. The majority of the patients (1.297 patients (65%)) were discharged directly to their own homes. Failure to return to independent living was reported for 136 (10%) patients. The following risk factors were identified; old age, extracapsular fracture, cognitive impairment, low pre-fracture NMS, discharge to rehabilitation, and being dependent at discharge (CAS = 6) (Table 3). Care needs were reported to have increased in 274 patients (26%); 752 patients (71%) reported the same level as before their hip fracture. Furthermore, 667 (50%) patients regained their pre-fracture NMS at 12 months, whereas 600 (45%) patients experienced a decrease in their NMS; and 75 (5%) patients either had no information on pre-fracture or 12-month NMS.
Discussion
We set out to investigate a vast number of risk factors for both short-term functional recovery and failure to return to independent living following hip fracture surgery. Only one-third of patients gained independence before discharge, based on a CAS value of 6, which was predictive of returning to independent living at 12 months. Multiple risk factors were identified, some of which will be discussed below. In general, patients with poor health (physically, cognitively, and functionally) before their fracture were at higher risk of being dependent at discharge. Even so, some modifiable factors were identified, such as post-operative mobilization and anesthesia type. For failure to live independently at 12 months, pre-fracture health greatly impacted the ability to remain in the patient's own home.
Dependency at discharge
Older patients with multiple comorbidities and low pre-fracture functional level (NMS ≤ 5) had poorer short-term functional outcomes; this observation is in line with the findings reported in other publications [8, 28]. In our study, patients who were not mobilized to standing within 24 h had an increased risk of being dependent at discharge, which shows the importance of getting patients back on their feet quickly after surgery. Likewise, time to mobilization was suggested as an underlying mechanism in the association between functional outcome and static factors, such as comorbidities, cognitive impairment, and fracture [9]. Early mobilization reduces the amount of time spent immobilized, which is important as immobilization carries an increased risk of complications such as pneumonia [29]. Furthermore, early mobilization has been shown to reduce mortality and disability following a hip fracture [30,31,32]. Common causes for not achieving early mobilization may be pain, nausea, and fatigue, which may be targeted with multimodal pain management, rehydration, and medical optimization. We found no association between epidural catheter use as post-operative pain management and independence at discharge. However, this may be due to only 4% of the patients receiving an epidural catheter. Regional nerve blocks have previously been found to reduce time to first-time mobilization, surgical delay, and LOS, influencing outcomes like mortality and readmissions [33,34,35]. Compared with general anesthesia, spinal anesthesia was associated with an improved short-term independence. However, there is a potential selection bias of patients by the anesthesiologist, where healthier patients are more likely to receive spinal anesthesia and, therefore, may be more likely to regain function. We attempted to adjust for this by including ASA score, cognitive function, and pre-fracture NMS in our model. However, some residual confounding may remain. Previous studies have found no differences between general anesthesia and spinal anesthesia regarding functional recovery [36, 37]. However, Fields et al. found more complications post-operatively in patients receiving general anesthesia that could delay mobilization [38].
Patients treated with THA carried an increased risk of being dependent at discharge. However, this is most likely a result of a 3-month movement restriction (hip flexion > 90 degrees, hip adduction > 0 degrees, and hip internal rotation > 0 degrees) following THA surgery. These restrictions hamper activities in the CAS such as getting in and out of bed, and may explain the association found between THA and dependency at discharge in the present study. This is supported by patients treated with THA being more likely to complete the TUG test, which may indicate a better walking ability at discharge.
A longer LOS was associated with dependency measured by the CAS; which is confirmed in a recent study that showed a similar trend [22]. It would have been expected that patients admitted for a longer period of time would display decreased dependency as they would have had a longer period to recover and therefore had more rehabilitation. Likely, the explanation is reverse causality where patients more rapidly regaining function being discharged sooner, rather than early discharge ensuring better functioning. Furthermore, more dependent and frail patients may be admitted for an extra day or 2 after receiving the needed hospital care while awaiting transfer to a rehabilitation facility or nursing home. LOS varies considerably between countries and has been reported to range from 1 to 55 days, which may to some extent be explained by differences in time to surgery and length of in-hospital rehabilitation [9]. Obviously, these factors may influence the short-term in-hospital functional recovery.
A recent study found that the initial functional recovery during the acute hospital stay was a good predictor for functional recovery after a subsequent rehabilitation stay [39]. Furthermore, regaining CAS has previously been shown to predict 30-day readmission and mortality. The study also showed that each additional CAS point patients regained improved their functional recovery even among patients who did not regain total independence upon discharge [22]. Therefore, it is crucial to find ways to improve short-term functional recovery as this may subsequently improve long-term functional recovery, thereby reducing mortality and readmissions.
Only 20% of patients were able to perform the TUG test at discharge, supporting the statement by others that the TUG test may not be the optimal measure for functional assessment in the acute phase following hip fracture surgery [40]. This indicates a need for more objective measurements for functional recovery validated in patients with hip fracture.
Failure to return to independent living
Sustaining a hip fracture can have considerable consequences for the patient, including forgoing independent living due to diminished function and increased care needs. Similar to Dyer et al., we found that 10% of patients became institutionalized due to their hip fracture [3]. Furthermore, our results align with risk factors found for institutionalization and increased care needs among patients with hip fractures identified in the previous studies [4, 5, 7, 41]. Generally, this indicates that patients with good health (cognitive and functional) have a better chance of returning to independent living.
Similar to the results by Gamboa-Arango et al., our results showed that dependence measured by CAS predicted failure to return to independent living at 12 months [4]. Furthermore, a recent study showed that short-term functional recovery predicted long-term functional recovery [39]. As declining function and increased care needs affect the ability to live independently, a focus on improving short-term functional recovery after hip fracture may help maintain pre-operative functions and independency. However, as this is an observational study, no conclusions regarding causality can be made, and it may be argued that the healthiest patients who are mobilized more quickly regain independence at discharge, and continue to live independently.
Strengths and limitations
The strengths of this study were the large study population and the detailed prospective data collection with consecutive inclusion of all admitted patients, including cognitively impaired patients, and with few missing values. On the other hand, this study also carries several limitations. We had no information about patients’ post-surgery weight-bearing limitations, which would influence short-term functional recovery, in particular. Additionally, marital status, cohabitation, and educational level may potentially affect the ability to live independently, along with residual confounding. As the 1 year follow-up relied on a questionnaire, recall bias is inherent.
Conclusion
Most of the risk factors associated with dependency at discharge were static. However, mobilizing patients to standing within 24 h from hip fracture surgery was associated with achieving independency at discharge, as measured by CAS = 6, which, in turn, was associated with return to independent living at 12 months. Patients not returning to independent living following hip fracture surgery were typically frailer than those who did return. However, the prognosis was generally good and the majority of the patients remained in their own home with little increase in care needs.
Availability of data and materials
The study protocol and data analysis files are available upon reasonable request to the corresponding author. For data sharing, relevant local authorities need to grant permission.
References
World Health Organization 2020 Decade of healthy ageing
Osnes EK, Lofthus CM, Meyer HE et al (2004) Consequences of hip fracture on activities of daily life and residential needs. Osteoporos Int 15:567–574. https://doi.org/10.1007/s00198-003-1583-0
Dyer SM, Crotty M, Fairhall N et al (2016) A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr 16:158. https://doi.org/10.1186/s12877-016-0332-0
Gamboa-Arango A, Duaso E, Malafarina V et al (2020) Prognostic factors for discharge to home and residing at home 12 months after hip fracture: an anoia hip study. Aging Clin Exp Res 32:925–933. https://doi.org/10.1007/s40520-019-01273-9
Vochteloo AJH, Van Vliet-Koppert ST, Maier AB et al (2012) Risk factors for failure to return to the pre-fracture place of residence after hip fracture: a prospective longitudinal study of 444 patients. Arch Orthop Trauma Surg 132:823–830. https://doi.org/10.1007/s00402-012-1469-8
Martinez-Reig M, Ahmad L, Duque G (2012) The orthogeriatrics model of care: systematic review of predictors of institutionalization and mortality in post-hip fracture patients and evidence for interventions. J Am Med Dir Assoc 13:770–777. https://doi.org/10.1016/j.jamda.2012.07.011
Uriz-Otano F, Pla-Vidal J, Tiberio-López G, Malafarina V (2016) Factors associated to institutionalization and mortality over three years, in elderly people with a hip fracture—an observational study. Maturitas 89:9–15. https://doi.org/10.1016/j.maturitas.2016.04.005
Xu BY, Yan S, Low LL et al (2019) Predictors of poor functional outcomes and mortality in patients with hip fracture: a systematic review. BMC Musculoskelet Disord 20:568. https://doi.org/10.1186/s12891-019-2950-0
Sheehan KJ, Williamson L, Alexander J et al (2018) Prognostic factors of functional outcome after hip fracture surgery: a systematic review. Age Ageing 47:661–670. https://doi.org/10.1093/ageing/afy057
Ju J, Zhang P, Jiang B (2019) Risk factors for functional outcomes of the elderly with intertrochanteric fracture: a retrospective cohort study. Orhtopaedic Surg 11:643–652. https://doi.org/10.1111/os.12512
Meng D, Bai X, Wu H et al (2019) Patient and perioperative factors influencing the functional outcomes and mortality in elderly hip fractures. J Investig Surg. https://doi.org/10.1080/08941939.2019.1625985
Wong RMY, Qin J, Chau WW et al (2021) Prognostic factors related to ambulation deterioration after 1-year of geriatric hip fracture in a Chinese population. Sci Rep 11:1–8. https://doi.org/10.1038/s41598-021-94199-0
World Health Organization Body mass index—BMI 2021 https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi
Jensen CM, Mainz H, Lamm M, et al. (2008) Reference programme for treatment of patients with proximal femur fractures. Dansk Sygeplejeråd, Danske Fysioterapeuter Dansk Ortopædisk Selskab 1–128.
Parker MJ, Palmer CR (1993) A new mobility after score for predicting mortality. J Bone Jt Surg Br 75:797–798
Kristensen MT, Bandholm T, Foss NB et al (2008) High inter-tester reliability of the new mobility score in patients with hip fracture. J Rehabil Med. https://doi.org/10.2340/16501977-0217
Kristensen MT, Foss NB, Kehlet H (2007) A new mobility score for predicting mortality after hip fracture. Physical 87:24–30
Danish Multidisciplinary Hip Fracture Registry (2019) Annual report 2019.
Frandsen CF, Glassou EN, Stilling M, Hansen TB (2021) Poor adherence to guidelines in treatment of fragile and cognitively impaired patients with hip fracture: a descriptive study of 2804 patients. Acta Orthop. https://doi.org/10.1080/17453674.2021.1925430
Kristensen MT, Kehlet H (2018) The basic mobility status upon acute hospital discharge is an independent risk factor for mortality up to 5 years after hip fracture surgery—survival rates of 444 pre-fracture ambulatory patients evaluated with the cumulated ambulation score. Acta Orthop 89:47–52. https://doi.org/10.1080/17453674.2017.1382038
Foss N, Kristensen M, Kehlet H (2006) Prediction of postoperative morbidity, mortality and rehabilitation in hip fracture patients: the cumulated ambulation score. Clin Rehabil 20:701–708
Kristensen MT, Öztürk B, Röck ND et al (2019) Regaining pre-fracture basic mobility status after hip fracture and association with post-discharge mortality and readmission—a nationwide register study in Denmark. Age Ageing 48:278–284. https://doi.org/10.1093/ageing/afy185
Podsiadlo D, Richardson S (1991) The timed “up & go”: a test of basic functional mobility for frail elderly persons. JAGS 39:142–148
Kristensen MT, Bandholm T, Holm B, Ekdahl C (2009) Timed up & go test score in patients with hip fracture is related to the type of walking aid. Arch Phys Med Rehabil 90:1760–1765. https://doi.org/10.1016/j.apmr.2009.05.013
Kristensen MT, Foss NB, Kehlet H (2007) Timed “up & go” test as a predictor of falls within 6 months after hip fracture surgery. Phys Ther 87:24–30. https://doi.org/10.1016/0308-5953(77)90120-9
Bischoff HA, Stähelin HB, Monsch AU et al (2003) Identifying a cut-off point for normal mobility: a comparison of the timed ‘ up and go ’ test in community-dwelling and institutionalised elderly women. Age Ageing 32:315–320
Tabori-jensen S, Hansen TB, Bøvling S et al (2018) Good function and high patient satisfaction at mean 2. 8 years after dual mobility THA following femoral neck fracture: a cross-sectional study of 124 patients. Clin Interv Aging 13:615–621
Van Der SMPL, Van EM, Tong WH et al (2020) Independent factors associated with long-term functional outcomes in patients with a proximal femoral fracture: a systematic review. Exp Gerontol. https://doi.org/10.1016/j.exger.2020.111035
Kamel HK, Iqbal MA, Mogallapu R et al (2003) Time to Ambulation After Hip Fracture Surgery: Relation to Hospitalization Outcomes. J Gerontol 58:1042–1045. https://doi.org/10.1093/gerona/58.11.M1042
Morri M, Forni C, Marchioni M et al (2018) Which factors are independent predictors of early recovery of mobility in the older adults’ population after hip fracture? a cohort prognostic study. Arch Orthop Trauma Surg 138:35–41. https://doi.org/10.1007/s00402-017-2803-y
Goubar A, Martin FC, Potter C et al (2021) The 30-day survival and recovery after hip fracture by timing of mobilization and dementia : a UK database study. Bone Joint J. https://doi.org/10.1302/0301-620X.103B7.BJJ-2020-2349.R1
Frandsen CF, Glassou EN, Stilling M, Hansen TB (2021) Malnutrition poor function and comorbidities predict mortality up to one year after hip fracture: a cohort study of patients. Eur Geriatr Med. https://doi.org/10.1007/s41999-021-00598-x
Scurrah A, Shiner CT, Stevens JA, Faux SG (2018) Regional nerve blockade for early analgesic management of elderly patients with hip fracture—a narrative review. Anaesthesia 73:769–783. https://doi.org/10.1111/anae.14178
Garlich JM, Pujari A, Debbi EM et al (2020) Time to block: early regional anesthesia improves pain control in geriatric hip fractures. J Bone Jt Surg 102:866–872
Guay J, Kopp S (2020) Peripheral nerve blocks for hip fractures in adults ( Review ). Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD001159.pub3.www.cochranelibrary.com
Fukuda T, Imai S, Nakadera M et al (2018) Postoperative daily living activities of geriatric patients administered general or spinal anesthesia for hip fracture surgery: a retrospective cohort study. J Orthop Surg 26:1–9. https://doi.org/10.1177/2309499017754106
Sieber F, Magaziner J, Marcantonio ER et al (2021) Spinal Anesthesia or general Anesthesia for hip surgery in older adults. N Engl J Med. https://doi.org/10.1056/NEJMoa2113514
Fields AC, Dieterich JD, Buterbaugh K, Moucha CS (2015) Short-term complications in hip fracture surgery using spinal versus general anaesthesia. Injury 46:719–723. https://doi.org/10.1016/j.injury.2015.02.002
Hershkovitz A, Borow Y, Beeri A, Nissan R (2020) Initial functional recovery as a measure for rehabilitation outcome in post- acute hip fractured patients. Arch Gerontol Geriatr. https://doi.org/10.1016/j.archger.2020.104070
Nygard H, Matre K, Fevang JM (2016) Evaluation of timed up and go test as a tool to measure postoperative function and prediction of one year walking ability for patients with hip fracture. Clin Rehabil 30:472–480. https://doi.org/10.1177/0269215515591039
Schulz C, Büchele G, Peter RS et al (2020) Regional variation of care dependency after hip fracture in Germany: a retrospective cohort study using health insurance claims data. PLoS ONE 15:1–17. https://doi.org/10.1371/journal.pone.0230648
Funding
This study was funded by the department only and has not received any external funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Data collection was performed by MS, Torben Bæk Hansen, and Christina Frølich Frandsen. Eva Natalia Glassou and Christina Frølich Frandsen performed the analyses. Christina Frølich Frandsen prepared the first draft of the manuscript, and all authors read, revised, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare relevant to this article's contents.
Ethics approval
The study was registered with the Danish Data Protection Agency (number 2007–58-0010). Under Danish law, no requirement for approval from the National Ethics committee applied.
Consent to participate and for publication
Under Danish law, no requirement for written consent applies.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Frandsen, C.F., Stilling, M., Glassou, E.N. et al. The majority of community-dwelling hip fracture patients return to independent living with minor increase in care needs: a prospective cohort study. Arch Orthop Trauma Surg 143, 2475–2484 (2023). https://doi.org/10.1007/s00402-022-04472-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04472-8