Abstract
We report the long-term results of Bernese periacetabular osteotomy using a dual approach in hip dysplasia. Fifty-three hips (49 patients, mean age 39.9 years: 13–62 years; bilateral hips: four patients) that underwent periacetabular osteotomy using a dual approach (combined Smith–Peterson and Kocher–Langenbeck techniques) between May 1997 and December 2005 were analyzed in this study. The clinical and radiologic outcomes and complications were analyzed and the final survival rates of the operated hips were investigated with survival analysis curves. Forty-nine hips survived until the final follow-up without arthroplasty, and four hips underwent arthroplasty. The average follow-up period was 11.5 years (8–16 years). The pain visual analogue scale improved from 6.3 to 1.1, while the Harris hip score improved from 61.9 to 91.1. Radiologic findings showed that all cases showed improvements in the center edge angle, acetabular angle, acetabular depth, and femoral head coverage. Two patients underwent intraarticular osteotomy due to a complication, and one patient underwent additional osteotomy due to an under-correction. Three cases showed an asymptomatic nonunion of the superior pubic ramus osteotomy site. One patient developed an avulsion fracture of the anterior superior iliac spine, and none of the cases had an infection or permanent neurologic damage. Kaplan–Meier analysis revealed that the 10-year survival rate was 93% (95% confidence interval [CI] 81–98%) with arthroplasty as the endpoint and 86% (95% CI 70–91%) with the progression of osteoarthritis based on Tönnis osteoarthritis rating as the endpoint. Based on the outcomes of a long-term follow-up of more than 10 years on average, Bernese periacetabular osteotomy via a dual approach was found to be a satisfactory method for lowering the incidence of complications while preserving hips.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In hips with acetabular dysplasia, the femoral head is not adequately covered by the acetabulum, and the surface for weight-bearing load decreases. This in turn causes abnormally high stress on the acetabular rim, ultimately leading to secondary degenerative arthritis [1, 2]. Murphy et al. followed the radiographic status of the dysplastic hips. And they reported that some radiographic parameters, a center–edge angle (< 16°), an acetabular index of depth to width (< 38%), an acetabular index of the weight-bearing zone (> 15°), uncovering of the femoral head (31%), or zero peak-to-edge distance, may lead osteoarthritis in dysplastic hip [3]. Jacobsen et al. reported that the center–edge angle, femoral head extrusion index, and acetabular depth index were significantly related to hip osteoarthritis [4].
If left untreated, the probability of developing secondary arthritis by the age of 50 is about 25–50% [2, 5]. Therefore, even if there are no symptoms in childhood and during growth, symptoms may manifest in adulthood and ultimately progress to degenerative arthritis. Generally, the femoral head and acetabulum may maintain a normal relationship until the age of 10–11 years, but after this period, the growth of acetabulum falls considerably short of the growth of the femoral head, causing a relative acetabular dysplasia in adults. Individuals with acetabular dysphasia can carry on daily life without pain for about 10–20 years. However, once degenerative changes occur, they progress rapidly and persistently; therefore, early correction is important for individuals with degenerative changes in the hip or those anticipated developing degenerative changes, to prevent the progression of such changes.
Although arthroplasty is the preferred treatment for older patients or patients with severe osteoarthritis, articular reconstruction should be preferentially considered for young, highly active patients, since there is a high likelihood that arthroplasty will ultimately fail. Since young patients have a long remaining lifespan, the lifetime of the artificial implant is likely to be exceeded [6, 7].
Thus, several pelvic osteotomy techniques based on an understanding of the anatomical structure of the hip as well as rearrangement of abnormal stress distributions have been introduced. Among pelvic osteotomies for hip dysplasia, the Bernese periacetabular osteotomy, introduced in 1983, is a type of re-directional osteotomy. While the technique published by Ganz et al. [1] is difficult, the postoperative outcomes have been reported to be good with benefits that are manifold. The Bernese group has published a 20-years survival rate of about 60% and a 30-years survival rate of about 30% [8]. It can be performed using a single approach, allow substantial correction in all directions, preserve blood supply to the acetabulum, and preserve the posterior column of the unilateral pelvis which enables early ambulation even with a simple internal fixation using screws. It also allows normal delivery in pregnant women, since the true pelvis is not deformed [9]. However, the operative technique is challenging. The challenge associated with the technique of Bernese periacetabular osteotomy is primarily due to it being an osteotomy, where the osteotomy is performed without visualization of the posterior column and ischium area.
The conventional PAO has a flat learning curve [10], which regarding the potential risks, may overwhelm the surgeon. Particularly, when obese patients are involved, osteotomy without the adequate surgical field of view is associated with higher risks of complications like neurovascular injuries [11].
Due to the technical difficulty and the flat learning curve of Bernese osteotomy, several authors [12, 13], including the author of this study [14], introduced periacetabular osteotomy which uses a dual approach and triple osteotomy by Tonnis with a triple approach. Triple osteotomy by Tonnis classically uses three separate incisions; one incision for each individual osteotomy [15]. CU (University of Colorado) periacetabular osteotomy introduced by Mei-Dan et al. is interlocking osteotomy using two- minimally invasive incision [16]. The osteotomy had been successfully done in 200 cases without major neurovascular complication, except injury of lateral femoral cutaneous nerve by direct seeing and protecting the sciatic nerve while ischial osteotomy. They also reported the technique allows early ambulation as rehabilitation by preserving the posterior column. Hussell et al. [17] pointed out that double acetabular osteotomy requires about 1.5 h longer operating time than the single approach. In contrast, Kim et al. [12] reported there was no difference in the operative time between the two methods, and he reported that the dual approach exhibited significant reductions in the amount of bleeding. As described above, the single approach has several disadvantages, but there are only a few reports on the dual approach. Furthermore, there are few studies that have performed long-term follow-ups of patients after periacetabular osteotomy (PAO) [18,19,20,21,22]. The objectives of this study were to analyze the clinical and radiologic outcomes and complications of Bernese periacetabular osteotomy via a dual approach involving combined Smith-Peterson and Kocher-Langenbeck techniques which make the surgeon see the osteotomy site of the posterior column, and examination of the final survival rate (> 10 years) of hips through survival analysis.
Subjects and methods
Subjects
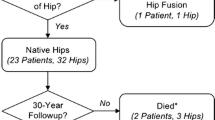
Fifty-three hips (bilateral hips: four patients) of 49 patients diagnosed with acetabular dysplasia, who were followed-up for average more than 11 years (8–16 years) after undergoing Bernese periacetabular osteotomy via a dual approach between May 1997 and December 2005, were enrolled in this study. There were 17 male and 46 female patients, with a mean age of 39.9 years (13–62 years). Fourteen patients have been excluded due to follow-up loss. In all cases, the patients presented to the hospital for hip pain, and four patients underwent osteotomy of both hips. The protocol of this retrospective comparative study was approved by our Institutional Review Board of Chungbuk National University Hospital (CBNUH 2020-09-019).
Methods
Operative technique
A dual approach was used for all cases. The modified Smith-Peterson technique was used for the anterior approach to perform an osteotomy of the pubic bone and ilium, and the Kocher-Langenbeck method was used for the posterior approach to perform an osteotomy of the posterior column and ischium. Moreover, a chest roll positioner was used to rotate the patient to the lateral decubitus position for the posterior incision and to a supine position for the anterior incision.
With the Smith-Peterson approach, a 10 cm longitudinal incision was made along the iliac crest past the anterior superior iliac spine, and the iliac medial periosteum was divided to expose the medial aspect of the ilium. After drilling holes for screw fixation, an osteotomy of the anterior superior iliac spine, which was isolated with the Sartorius muscle attached, was performed in a triangular-shape and medialized. After dissecting and exposing the periosteum of the superior pubic ramus, a K-wire was inserted medially in the iliopubic eminence to examine the osteotomy via X-ray. The K-wire was vertically inserted in the ilium between the anterior superior iliac spine and anterior inferior iliac spine, and then an x-ray was performed to confirm the location of the osteotomy. An osteotomy of the pubic bone was made 1 cm medially from the medial aspect of the iliopubic eminence, in order to avoid nonunion of pubis, being cautious about the damage of the acetabular joint. In addition, the direction of osteotomy was inclined 45° medially to prevent damage to the acetabular joint under fluoroscopy.
An osteotomy of the ilium was performed starting from 3 cm lateral to the sacroiliac joint and 1 cm lateral to the pelvic brim, then to the downward with a 120° turn and through all the visible parts with 1 cm or more posterior column preserved. The osteotomy was performed with an interval of about 1 cm for some females with a narrow posterior column. In general, it extended slightly inferiorly to the pelvic brim. The patient was then rotated to the lateral decubitus position.
For the Kocher-Langenbeck approach, the incision was carried over the greater trochanter parallel with the anterior incision. Short external rotators were detached while preserving 1–2 cm that attaches to the femur to avoid damaging the blood supply to the femoral head and for tendon reattachment. The posterior wall and posterior column of the acetabulum were exposed, and osteotomy was performed along the posterior border to the infracotyloid groove while preserving about 1 cm of the posterior column.
The osteotomy of the ilium was completed by finding the line of osteotomy of the ilium, which was initiated at the anterior part of the proximal line of osteotomy for the posterior column. The osteotomy of the ischium was performed almost perpendicular to the line of osteotomy of the posterior column, medially along the inferior margin of the acetabulum while ensuring the posterior column was not damaged [14].
The patient was rotated back to the supine position, and Schanz pins were inserted in the superior acetabulum (near the anterior inferior iliac spine). The osteotomized ilium was spread using a laminar spreader, and the acetabular fragment was rotated using a Schanz pin to cover the femoral head adequately. The anterior aspect was also covered by medially displacing the distal fragment. After fixing them with Steinmann pins, radiographs were taken. Upon confirming that the fragments adequately covered the femoral head and that the hip joint was medialized, the Steinmann pins were removed and acetabular fragments were fixed using 2–3 long screws. Bone graft, which were obtained from the anterior superior iliac spine, was inserted between the ilium and acetabular fragment.
Rehabilitation
Immobilization was not performed after the surgery. As soon as the pain diminished, the patients were instructed to perform partial weight-bearing walking exercises to the extent tolerable. At about week 10–12, complete weight-bearing was possible. The inserted screws were removed about 1 year after surgery.
Clinical and radiological analysis
The range of motion of the hip joint was measured by an orthopaedic surgeon as well as the radiological parameters. The Harris hip score and the pain visual analogue scale score were measured and compared before and 1 year after surgery.
Before surgery, all patients underwent pelvis radiography to evaluate radiological parameters. In addition, the exact version of the acetabulum was evaluated before surgery through computed tomography.
Immediately after surgery, all patients underwent plain radiography. They visited the outpatient clinic periodically in the following order: 2 weeks, 1 month, 3 months, 6 months and 1 year after the operation, followed by x-ray observation.
The radiological parameters, including center edge angle of Wiberg (CE angle), acetabular angle of Sharp, and acetabular depth, were checked and compared between comparison with the preoperative x-ray, Intraoperative intra-articular fracture and non-union findings were also confirmed through the radiographs. Cross-over sign and ischial spine sign that can infer the acetabular version were evaluated.
Statistical analysis
Statistical analyses were performed using the IBM SPSS Statistics version 24 software (SPSS Institute, IBM Corp.). Preoperative and postoperative HHS and radiographic parameters, as well as postoperative changes, were compared using the Wilcoxon rank-sum test at a significance of p < 0.05. Kaplan–Meier analysis was used to analyze the survival rates, with arthroplasty and Tönnis arthritis progression at year 10 as the endpoints [23].
Results
Radiologic assessment showed that compared to preoperative levels, all patients had significant improvements of the center–edge angle of Wiberg, acetabular angle of sharp, acetabular depth, and femoral head coverage at the final follow-up. The Harris hip score improved from 61.9 before surgery to 91.9 after surgery, while the pain visual analogue scale score improved from 6.3 to 1.1. The center edge angle improved from 2.3° to 24.5°, and the acetabular angle decreased from 54.1° to 40.5°. The acetabular depth improved from 153.1 to 207.4, and the femoral head coverage significantly improved from 49.7% to 74.8% (Table 1; Fig. 1). Flexion showed a reduction of 7.1° at the hip range of motion test, but none of the patients complained of discomfort in daily life due to this reduction (Table 2).
A 30-year-old male patient undergoes left hip PAO. a Anteroposterior radiograph of the pelvis obtained from a 30-year-old man with symptomatic left hip dysplasia and femoral head subluxation, b immediate post-operative pelvic anteroposterior radiograph shows satisfactory correction and fixation (PAO was conducted at 2-week intervals on both hips), c radiograph obtained 5 years after surgery shows excellent clinical results, despite the progression of OA, d Radiograph obtained 12 years after surgery shows that left hip joints progressed in terms of the Tönnis OA grade. HSS = < 70, poor; 70–79, fair; 80–89, good; 90–100, excellent. HSS Harris Hip Score, OA osteoarthritis, PAO periacetabular osteotomy
In terms of complications, intra-articular osteotomy was observed in two cases, and additional osteotomy was scheduled for one case due to under-correction. The fracture was not from direct osteotomy into acetabular joint, but extended from the osteotomy site. There were minimal displacement less than 2 mm in two cases of intra-articular osteotomy. Therefore, for two cases, conservative treatment was performed with non-weight bearing instead of partial weight-bearing for 4 weeks, without additional surgery, and the union was confirmed through follow-up X-ray. Nonunion of the pubic bone was observed in three cases. Cross-over sign and ischial spine sign were found in seven cases. An avulsion fracture of the anterior superior iliac spine occurred in one case during the process of drilling a hole for screw fixation and performing an osteotomy for medialization. However, the displacement of bone fragment was mild and therefore, we only made the observation. There were no complications such as nerve (sciatic nerve, femoral nerve, peroneal nerve, lateral femoral cutaneous nerve, superior and inferior gluteal nerve) palsy, avascular necrosis of bone fragments, and posterior column fracture (Table 3).
Kaplan–Meier analysis with arthroplasty as the end point revealed a survival rate of 93% and progression in terms of osteoarthritis (OA) grade revealed 86% at 10 years (Fig. 2).
Discussion
There are some approaches to periacetabular osteotomy. The Bernese periacetabular osteotomy with a single approach like the ilioinguinal, direct anterior or modified Smith-Peterson approach is a type of challenging technique because of its flat learning curve technically and being related to some complications such as intra-articular extension of the osteotomy, posterior column fracture, and neurovascular injury caused by obscured osteotomy [17, 24]. The dual approach with Kocher–Langenbeck approach had been introduced and allowed surgeons to secure an accurate osteotomy by identifying and protecting the sciatic nerve and exposing the ischial bone. Kocher–Langenbeck approach has a risk that affects the vascularity of the proximal femur by compromising the deep branch of the medial circumflex artery because the deep branch of the femoral circumflex artery crosses posterior to the obturator externus tendon and runs anterior to the other short external rotators [25]. In addition, when conversion to arthroplasty there may be a risk of adhesion around the previous operation site, especially the attachment site of the external rotators, which make surgery difficult. The triple osteotomy technique by Tonnis requires position change from a slightly over-tilted lateral position to a supine position to approach the ischium and pubis separately. Furthermore, multiple incisions have a risk including increased blood loss, operative time as well as pain and cosmetic concerns [15, 26]. With regard to the surgical approach of CU-PAO, there are some advantages for preventing neurovascular injury like sciatic nerve injury and allowing early weight-bearing postoperatively. Even Mei-Dan noted that it has a cosmetic advantage, a smaller incision than that described for the Bernese PAO and triple osteotomy by Tonnis [16].
In the short-term follow-up of this study with a dual approach using both the modified Smith-Peterson technique and the Kocher-Langenbeck method, functional improvement using the Harris hip score improved from 61.9 preoperatively to 91.9 postoperatively, and radiologic findings improved from the preoperative CE angle of 2.3° to postoperative CE angle of 24.5° (Table 1). Compared with the Harris hip score improvement of 18 ~ 33 and CE angle correction of 22 ~ 28° in studies using the anterior single approach, the dual approach also showed sufficient improvement in function and radiological factors (Table 3).
Postoperative complications occurred in seven cases. There were two cases, in which the osteotomy was extended to the joint from the osteotomy site. In this study, conservative treatment was performed because of minimal displacement. In one case, re-operation was chosen due to under correction. The case of under-correction was confirmed on plain radiograph 3 months after the surgery and the patient suffered from pain. In three cases, there was a nonunion due to excessive medial displacement of the pubic bone. These nonunion did not cause symptoms. There was also no case of conversion to arthroplasty. We checked the postoperative plain radiographs to find cross-over sign or ischial spine sign and evaluate the version of the hip including retroversion. Cross-over sign and ischial spine sign were found in seven cases of this study, which suggest retroversion due to over-correction. However, we just checked only plain x-ray not CT scan and it had a limitation for the accurate version analysis of acetabulum postoperatively. In addition, the retroversion of the hip in this study did not cause symptoms such as impingement symptoms or limitation of range of motion.
An avulsion fracture of the anterior superior iliac spine occurred in one case during the process of drilling a hole for screw fixation and performing an osteotomy and medially pushing it aside. The displacement was mild; therefore we only observed the patient’s progress. Contrary to our concern of complications caused by a disturbance of blood flow due to two incisions around the hip joint, skin or soft tissue necrosis did not occur. This is probably because there was an adequate gap and soft tissues present between the modified Smith-Peterson approach on the anterior side and Kocher–Langenbeck approach on the posterior side. As described above, although it was possible that avascular necrosis of femoral head and acetabular fragment, there was no case of avascular necrosis of the femoral head since the medial femoral circumflex artery was preserved by retracting the quadratus femoris muscle without cutting through the posterolateral approach that is familiar to surgeons. There was no case of avascular necrosis of acetabular fragment which is vascularized by the supra-acetabular and acetabular branches of the superior gluteal artery, the obturator artery, and the inferior gluteal artery [27]. Furthermore, there were no complications such as nerve palsy, posterior column fracture, or heterotopic ossification.
Rating the conversion to total hip arthroplasty as the endpoint, 10-year survival of hip joints were 93%. The intermediate to long-term results of young patients under 40 years old were reported to be 90.8% in 10 years [28], and mid-term results [29] were similar to this study (Fig. 2). Ten-year survival rates were reported to be 85–93% in studies using the anterior single approach (Table 4).
Previous studies have reported that older age at the time of operation is a poor prognostic factor for long-term follow-up [19, 21, 22, 30, 31]. However, even though patients enrolled in this study were older than in other studies, the results showed good hip survival.
The other prognostic factors affecting the survival rate of hip joints were the correction of radiological factors including CE angle [30,31,32].
The average range of CE angle reported by Wiberg was between 25° and 35°. Massie and Howarth reported 35° in a study performed on US population [33]. Nakamura and Fuji reported 32.2 ± 6.4° SD and 30 ± 6.2° SD in the Japanese population respectively [34, 35]. Han and associates reported 32.6 ± 5.7° SD which is lower than the average CE angle of US population in their study performed on a Korean population [36]. In this study, the average CE angle correction was 22.2° and the average postoperative CE angle was 24.5°. It can be considered as under coverage, since the dysplasia of the hip was diagnosed by the criteria of CE angle, under 25°. Also, there are patients showing postoperative anterior over coverage. However, in a recent study, Murphy et al. reported that under 16° of center edge angle might lead to osteoarthritis in dysplastic hip [3]. The authors of this study consider that although the CE angle less than 25° were still borderline dysplastic and inferred lateral under coverage, it is significant correction of CE angle. In addition, no patient underwent arthroplasty due to progression of osteoarthritis after PAO with dual approach despite relative high rate of lateral undercoverage and anterior overcoverage in this study. Therefore, this radiological correction may have improved the long-term survival of the hip. Furthermore, intraoperative intraarticular fractures and postoperative heterotopic ossification have been reported as prognostic factors that reduce survival [37]. Visualization of the osteotomy site through the dual approach employed without increasing these complications and this may improve long-term survival.
This study has several limitations. First, no comparisons were made with a control group that had been operated on only by anterior approach. Therefore, it was difficult to compare differences directly according to the approach, and so we compared our results with those of other studies that used a single anterior approach. Second, the skill of the operator varies according to the number of cases. The learning curve of the operator was reflected in results such as the operative time and complications, which decreased according to the time point of the surgeon, so it was difficult to obtain a uniform result. Third, the retrospective nature of this study may have led to selection bias.
Conclusion
All cases showed improvements in the PVAS score including clinical pain, Harris hip score, and hip range of motion, and radiological findings showed improvement on short-term follow-up. Thus, periacetabular osteotomy using a dual approach seems to be an effective treatment for preserving the hip joint, since it enables visualization of all areas of the osteotomy, which does not increase the incidence of complications related to osteotomy without direct seeing the pelvic bone. Furthermore, long-term results (> 10 years) show a high survival rate.
References
Ganz R, Klaue K, Vinh TS, Mast JW (1988) A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res 232:26–36
Cooperman DR, Wallensten R, Stulberg SD (1980) Post-reduction avascular necrosis in congenital dislocation of the hip. J Bone Joint Surg Am 62:247–258
Murphy SB, Ganz R, Müller ME (1995) The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am 77:985–989
Jacobsen S, Sonne-Holm S, Søballe K, Gebuhr P, Lund B (2005) Hip dysplasia and osteoarthrosis: a survey of 4 151 subjects from the osteoarthrosis substudy of the Copenhagen City heart study. Acta Orthop 76:149–158
Cooperman DR, Wallensten R, Stulberg SD (1983) Acetabular dysplasia in the adult. Clin Orthop Relat Res 175:79–85
Bsila RS, Inglis AE, Ranawat CS (1976) Joint replacement surgery in patients under thirty. J Bone Joint Surg Am 58:1098–1104
Chandler HP, Reineck FT, Wixson RL, McCarthy JC (1981) Total hip replacement in patients younger than thirty years old. A five-year follow-up study. J Bone Joint Surg Am 63:1426–1434
Lerch TD, Steppacher SD, Liechti EF, Tannast M, Siebenrock KA (2017) One-third of hips after periacetabular osteotomy survive 30 years with good clinical results, no progression of arthritis, or conversion to THA. Clin Orthop Relat Res 475:1154–1168
Kim HT, Choi SJ, Yoo CI (2005) Bernese periacetabular osteotomy for treatment of acetabular dysplasia. J Korean Orthop Assoc 40:942–948
Novais EN, Carry PM, Kestel LA, Ketterman B, Brusalis CM, Sankar WN (2017) Does surgeon experience impact the risk of complications after Bernese periacetabular osteotomy? Clin Orthop Relat Res 475:1110–1117
Novais EN, Potter GD, Sierra RJ, Kim YJ, Clohisy JC, Schoenecker PL, Trousdale RT, Carry PM, Millis MB (2015) Surgical treatment of adolescent acetabular dysplasia with a periacetabular osteotomy: does obesity increase the risk of complications? J Pediatr Orthop 35:561–564
Kim HT, Woo SH, Lee JS, Cheon SJ (2009) A dual anteroposterior approach to the Bernese periacetabular osteotomy. J Bone Joint Surg Br 91:877–882
Dienst M, Goebel L, Birk S, Kohn D (2018) Bernese periacetabular osteotomy through a double approach: simplification of a surgical technique. Oper Orthop Traumatol 30:342–358
Chang JS, Kwon KD, Shon HC (2002) Bernese periacetabular osteotomy using dual approaches for hip dysplasias. J Korean Orthop Assoc 37:226–232
Tönnis D, Behrens K, Tscharani F (1981) A modified technique of the triple pelvic osteotomy: early results. J Pediatr Orthop 1:241–249
Mei-Dan O, Welton KL, Kraeutler MJ, Young DA, Raju S, Garabekyan T (2019) The CU PAO: a minimally invasive, 2-incision, interlocking periacetabular osteotomy: technique and early results. J Bone Joint Surg Am 101:1495–1504
Hussell JG, Mast JW, Mayo KA, Howie DW, Ganz R (1999) A comparison of different surgical approaches for the periacetabular osteotomy. Clin Orthop Relat Res 363:64–72
Kralj M, Mavcic B, Antolic V, Iglic A, Kralj-Iglic V (2005) The Bernese periacetabular osteotomy: clinical, radiographic and mechanical 7–15-year follow-up of 26 hips. Acta Orthop 76:833–840
Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M (2010) Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome: surgical technique. J Bone Joint Surg Am 92(Suppl 1 Pt 2):115–129
Díaz BA, Pérez RL, Bullón IG, Rodríguez LEM, López-Durán Stern L (2015) Long-term clinical and radiological outcomes in a serie of 26 cases of symptomatic adult developmental dysplasia of the hip managed with Bernese periacetabular osteotomy. Rev Esp Cir Ortop Traumatol 59:421–428
Wells J, Millis M, Kim YJ, Bulat E, Miller P, Matheney T (2017) Survivorship of the Bernese periacetabular osteotomy: what factors are associated with long-term failure? Clin Orthop Relat Res 475:396–405
Lerch TD, Steppacher SD, Liechti EF, Siebenrock KA, Tannast M (2016) Bernese periacetabular osteotomy: indications, technique and results 30 years after the first description. Orthopade 45:687–694
Rich JT, Neely JG, Paniello RC, Voelker CC, Nussenbaum B, Wang EW (2010) A practical guide to understanding Kaplan-Meier curves. Otolaryngol Head Neck Surg 143:331–336
Hussell JG, Rodriguez JA, Ganz R (1999) Technical complications of the Bernese periacetabular osteotomy. Clin Orthop Relat Res 363:81–92
Gautier E, Ganz K, Krügel N, Gill T, Ganz R (2000) Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br 82:679–683
Balakumar B, Racy M, Madan S (2018) Minimally invasive (MIS) Tonnis osteotomy—a technical annotation and review of short term results. J Orthop 15:253–258
Beck M, Leunig M, Ellis T, Sledge JB, Ganz R (2003) The acetabular blood supply: implications for periacetabular osteotomies. Surg Radiol Anat 25:361–367
Ito H, Tanino H, Yamanaka Y, Minami A, Matsuno T (2011) Intermediate to long-term results of periacetabular osteotomy in patients younger and older than forty years of age. J Bone Joint Surg Am 93:1347–1354
Zhu J, Chen X, Cui Y, Shen C, Cai G (2013) Mid-term results of Bernese periacetabular osteotomy for developmental dysplasia of hip in middle aged patients. Int Orthop 37:589–594
Siebenrock KA, Schöll E, Lottenbach M, Ganz R (1999) Bernese periacetabular osteotomy. Clin Orthop Relat Res 363:9–20
Hartig-Andreasen C, Troelsen A, Thillemann TM, Søballe K (2012) What factors predict failure 4 to 12 years after periacetabular osteotomy? Clin Orthop Relat Res 470:2978–2987
Grammatopoulos G, Wales J, Kothari A, Gill HS, Wainwright A, Theologis T (2016) What is the early/mid-term survivorship and functional outcome after Bernese periacetabular osteotomy in a pediatric surgeon practice? Clin Orthop Relat Res 474:1216–1223
Massie WK, Howorth MB (1950) Congenital dislocation of the hip. Part I. Method of grading results. J Bone Joint Surg Am 32-A:519–531
Nakamura S, Ninomiya S, Nakamura T (1989) Primary osteoarthritis of the hip joint in Japan. Clin Orthop Relat Res 241:190–196
Fujii M, Nakashima Y, Jingushi S, Yamamoto T, Noguchi Y, Suenaga E, Iwamoto Y (2009) Intraarticular findings in symptomatic developmental dysplasia of the hip. J Pediatr Orthop 29:9–13
Han CD, Yoo JH, Lee WS, Choe WS (1998) Radiographic parameters of acetabulum for dysplasia in Korean adults. Yonsei Med J 39:404–408
Sambandam SN, Hull J, Jiranek WA (2009) Factors predicting the failure of Bernese periacetabular osteotomy: a meta-regression analysis. Int Orthop 33:1483–1488
Trousdale RT, Ekkernkamp A, Ganz R, Wallrichs SL (1995) Periacetabular and intertrochanteric osteotomy for the treatment of osteoarthrosis in dysplastic hips. J Bone Joint Surg Am 77:73–85
Crockarell J Jr, Trousdale RT, Cabanela ME, Berry DJ (1999) Early experience and results with the periacetabular osteotomy. The Mayo Clinic experience. Clin Orthop Relat Res 363:45–53
Mayo KA, Trumble SJ, Mast JW (1999) Results of periacetabular osteotomy in patients with previous surgery for hip dysplasia. Clin Orthop Relat Res 363:73–80
Trumble SJ, Mayo KA, Mast JW (1999) The periacetabular osteotomy. Minimum 2 year follow up in more than 100 hips. Clin Orthop Relat Res 363:54–63
Peters CL, Erickson JA (2006) Treatment of femoro-acetabular impingement with surgical dislocation and débridement in young adults. J Bone Joint Surg Am 88:1735–1741
Clohisy JC, Nunley RM, Curry MC, Schoenecker PL (2007) Periacetabular osteotomy for the treatment of acetabular dysplasia associated with major aspherical femoral head deformities. J Bone Joint Surg Am 89:1417–1423
Steppacher SD, Tannast M, Ganz R, Siebenrock KA (2008) Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res 466:1633–1644
Troelsen A, Elmengaard B, Søballe K (2009) Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg Am 91:2169–2179
Dahl LB, Dengsø K, Bang-Christiansen K, Petersen MM, Stürup J (2014) Clinical and radiological outcome after periacetabular osteotomy: a cross-sectional study of 127 hips operated on from 1999–2008. Hip Int 24:369–380
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shon, H.C., Park, W.S., Chang, JS. et al. Long-term results of Bernese periacetabular osteotomy using a dual approach in hip dysplasia. Arch Orthop Trauma Surg 143, 591–602 (2023). https://doi.org/10.1007/s00402-021-04090-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-04090-w