Abstract
Objectives
Intertrochanteric femur fractures (ITFF) are frequently fixed with proximal femoral nailing (PFN), and a common cause of fixation failure is cut-out of the lag screws. In the literature, many factors have been defined to determine the failure risk, including the tip–apex distance (TAD), calcar-referenced tip–apex distance (CalTAD), the Cleveland zone and Parker's ratio. In this study, a novel technique is described which favors infero-posterior placement of the lag screw and predicts failure risk for PFN. The purpose of this study was to evaluate the tip–neck distance ratio as a factor for the prediction of cut-out after PFN of ITFF.
Materials and methods
A retrospective evaluation was made of the data of 125 patients applied with PFN for ITFF between October 2016 and September 2019. The occurrence of mechanical complications was analyzed in relation to age, gender, fracture side, American Society of Anaesthesiologists classification, fracture classification, reduction quality, bone quality, Cleveland zone, Parker’s ratio, TAD, CalTAD and the TNDR.
Results
A total of 125 patients, including 16 with mechanical complications, were suitable for full analysis. In the univariate analysis, reduction quality (p = 0.003), the TAD (p = 0.048) and the TNDR (p = 0.030) were statistically associated with mechanical complications (p < 0.05). In the multivariate analysis, good quality of reduction reduced risk of mechanical failure (p = 0.011) and the TNDR (p < 0.001) indicated that these were two independent factors affecting mechanical complications.
Conclusion
The results of this study provide clinical evidence that the TNDR is a predictor for cut-out risk. Placement of the lag screw posterior and inferior reduces the risk of mechanical complications.
Level of evidence
Level 3.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intertrochanteric femur fractures (ITFF), which usually occur as a result of low-energy trauma in the elderly and high-energy trauma in the young, are generally treated with extramedullary and intramedullary fixation methods [1, 2]. Implant failure in elderly patients with an ITFF has a great effect on morbidity and mortality [3]. Intertrochanteric fractures are frequently fixed with proximal femoral nailing (PFN), and a common cause of fixation failure is cut-out of the lag screws [4, 5]. Bone quality, fracture geometry, reduction, implant design and implant placement are the main factors determining success in trochanteric fractures [6, 7]. Consequently, the ability to predict and prevent the causes of cephalomedullery (CM) nail cut-out and cut-in are important.
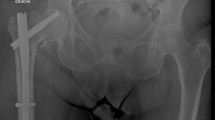
To date, the methods used for the placement of the lag screws are the tip–apex distance (TAD), calcar-referenced tip–apex distance (CalTAD), Cleveland zone and Parker’s ratio [8,9,10]. The tip–apex distance (TAD) has been shown to be an important predictor for cut-out in PFN [11] and favors central–central positioning of the lag screws. In the literature, it has been reported that inferior positioning of lag screws in the AP plane reduces the risk of cut-out with the view that there is better bone stock, and surgeons have tended towards this positioning of lag screws [8, 10, 12,13,14]. Parker’s ratio and CalTAD measurements support this view as predictors. However, CalTAD is based on AP view measurements only and supports infero-central lag screws positioning. Parker’s ratio evaluates measurements on both AP and lateral views separately with lag screws positioned inferiorly in the AP view and central in the lateral view [10]. However, in this technique, the measurements are made independently from lag screw type and the measurement may cause errors in cases with anatomic variations, where the lag screw axis is not parallel to the neck axis for acceptable loss of reduction. Therefore, a novel technique is described in this paper which favors infero-posterior placement of the lag screw and predicts failure risk for PFN. This is the Tip–Neck Distance Ratio (TNDR) (Fig. 1).
a, b Graphical (a) and radiographic (b) presentation of the tip–neck distance ratio distance measurement. The total distance between the inferior of the femoral head–neck junction and the blade tip on the pelvic AP radiograph (a) and the distance between the posterior femoral head–neck junction and the blade tip on the hip lateral radiograph (c) was calculated as the proportion of the total distance between the blade tip and the superior of the femoral head–neck junction on the AP radiograph (b) and the distance between the anterior of the femoral head–neck junction and the blade tip on the lateral radiograph (d).TNDR was calculated as (a + c)/(b + d)
The purpose of this study was to evaluate the TNDR as a factor for the prediction of cut-out after PFN of ITFF [15].
Materials and methods
Local Ethics Committee approval and informed consent from all the patients were obtained. A retrospective evaluation was made of the prospectively collected data of 185 patients, treated with PFN for an intertrochanteric femur fracture between October 2016 and September 2019. All fractures were treated by a single surgeon who had more than 5 years of experience of trauma surgery.
Inclusion criteria of the study were patients aged > 60 years, with an unstable femoral fracture (31-A2, 31-A3) according to the AO/OTA proximal femur classification [16]. Exclusion criteria were defined as a pathological, open, or concomitant lower extremity fracture, death, lack of standard radiographs, and radiological follow-up for at least 3 months postoperatively [8]. According to these criteria, a total of 125 patients were accepted in the study. Cut-out was defined as supero-medial migration of the PFNA lag screw into the femoral head and hip joint [4]. Patients were grouped according to cut-out state, as the cut-out group (n:16) and no cut-out group (n:119). All radiographic measurements were evaluated in both groups.
Patient demographic data and clinical characteristics were obtained from the medical records, including age at the time of operation, gender, side, body mass index (BMI), American Society of Anaesthesiologists (ASA) score, and the severity of osteoporosis at the time of fracture. Osteoporosis was evaluated from the contralateral radiograph according to the Singh Index [17].
Radiographic evaluation
Standard immediate postoperative and follow-up radiographs were taken as pelvic anteroposterior (AP) and Löwenstein lateral views. The pelvic AP view was taken with the patient positioned supine, both lower extremities in 15° internal rotation to accommodate femoral anteversion, distance between the X-ray tube and the film of 1.2 m, and projection towards the middle of the line connecting the upper symphysis pubis and anterior–superior iliac spine. The Löwenstein lateral view was taken with patient turned onto the affected hip at least 45°, with the hip flexion angle of 90° and internal rotation angle of 45° in a supine position and then images of each side were taken vertically from the groin region [18].
The radiological measurements of TNDR, TAD [4], CalTAD [8], Cleveland zone [9], Parker’s ratio (PR) [10], femoral neck-shaft angle difference [8] and reduction quality were evaluated by two independent, experienced orthopaedic surgeons using the hospital picture archiving and communication system (PACS) tool (Fig. 2). Inter-observer reliability for all the measurements was satisfactory with a median value of 0.83 (range 0.78–0.89). The median value of the measurements was calculated as the average of the values measured by the two surgeons. Discrepancies in the classification of the fractures and TNDR measurements were resolved with the observation of the senior author.
TNDR was measured as the proportion of the total distance between the inferior of the femoral head–neck junction and the lag screw tip on AP view (a) and the distance between the posterior femoral head–neck junction and the lag screw tip on lateral view (c) and the total distance between the lag screw tip and the superior of the femoral head–neck junction on the AP view (b) and the distance between the anterior of the femoral head–neck junction and the lag screw tip on lateral view (d) (Fig. 1). The head–neck junction was accepted as the point, where the convexity of the femoral head turns into the concavity of the femoral neck, on both views. The other radiological measurements as mentioned before were evaluated as defined in the literature [4, 8,9,10]. The reduction quality was determined using the Baumgaertner et al. classification, and was evaluated as good, acceptable, or poor [4].
In all the patients, the Hip Fracture Nail System (Trauson Stryker, Changzhou, China) was used as the cephalomedullary nail. The diameter of the lag screws for this device was 10.5 mm. All the operations were performed with closed reduction on a traction table. On the first postoperative day, patients were allowed mobilization as tolerated according to pain. The hip range of motion (ROM) and strengthening exercises protocol was started immediately postoperatively. After the 15th and 30th day controls, we followed the patients up in monthly periods until the 3rd month. After the 3rd month, we continued for 3-month periods. Union and complications were evaluated clinical and radiological in postoperative evaluations. Complications such as varus collapse or implant cut-out were recorded.
Statistical analysis
Statistical analyses and calculations were performed using IBM SPSS Statistics vn. 22.0 software (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY, USA) and MS-Excel 2016 program.
To determine the difference between variables in complication groups, continuous variables were evaluated with the Mann–Whitney U test, and categorical variables with the Chi-square test (Chi-square test—χ2). The Chi-square test results were reported from continuity correction and likelihood ratio test statistics.
In addition to age and gender, the status of no complication and TAD, TNDR, and reduction quality variables which showed significance in the univariate analysis were included in the logistic regression analysis as independent variables. For explanation of the model, – 2 log likelihood and Nagelkerke R2 values were reported, goodness of fit for the model was examined with Hosmer–Lameshow statistics and the odds ratios were given in a 95% confidence interval (95% CI). A value of p < 0.05 was accepted as statistically significant.
Results
Evaluation was made of a total of 125 patients, comprising 85 females and 40 males with a mean age of 78.3 years (range, 65–95 years). Mechanical failure of PFNA was determined in 16 (12.8%) patients. The demographic data of the patients are shown in Table 1. The mean radiological follow-up time for the fractures was 14.6 months (range, 5–40 months). No statistically significant difference was determined between the groups in respect of age, gender, side and BMI (p > 0.05) (Table 1).
In the univariate analysis, ASA, follow-up, and AO classification were not statistically different between the two groups (p > 0.05) (Table 1). No significant difference was determined between the groups in respect of the Singh Osteoporosis Index (p = 0.847) (Table 1). CalTAD, cervical angle difference, Parker’s ratio AP and L were not statistically different between the two groups (p > 0.05) (Table 1). In the TAD, TNDR and good reduction quality measurements, a significant difference was determined between the groups (p < 0.05) (Table 1).
In the multivariate analysis, the multivariate model included age, gender, and all parameters with a value of p < 0.05 in the univariate analysis. Reduction quality (p = 0.011) and the TNDR (p < 0.001) showed significant results, which indicated that reduction quality and the TNDR were two independent factors affecting mechanical complications (Table 2).
Discussion
The place of cephalomedullary nails, particularly in the treatment of unstable ITFF, has been previously proven. The most common cause of fixation failure after CM nailing is cut-out of the lag screw [4, 5, 19]. Lag screw positioning is known to have a strong influence on the incidence of mechanical complications. In this study, a new measurement method of cut-out was proposed, and from the effect and comparisons with other measurement methods, the TNDR value was determined to be high risk in terms of mechanical complications, Table 3.
As the measurement method proposed is a proportional value, it is independent of the patient anatomy and dimensions, providing a combined value in the AP and lateral planes. Current lag-screw placement techniques tend to be inferior–central and inferior–posterior. In the measurement technique described in this study, placement of the lag screw in quadrants, such as superior–anterior, superior–central, and central–anterior, which are risk factors for cut out, is a predictor factor and supports the current literature [14, 20].
Previous studies have stated that TAD > 25 [4, 21, 22], CalTAD [8], Parker’s ratio [10], positioning of lag screw outside the centre–centre or centre–inferior position according to the Cleveland zone [9, 23], varus neck-shaft angle [23, 24] and reduction quality [4] are risk factors for cut-out.
TAD has been reported by many researchers as an important predictor for cut-out [4, 22]. However, lag screw in superior position and inferior position in AP view, and anterior and posterior position in LAT view may have similar results. In a biomechanical study by Kuzyk et al., it was reported that an inferior lag screw provides higher resistance against axial and torsional stresses [13]. Although Goffin et al. suggested lag screw positioning in inferior–central and inferior–posterior, it was stated that TAD > 25 is not a more reliable predictor for cut-out [14]. Kane et al. [25], Mingo-Robinet et al. [26] and Herman et al. [27] stated that TAD was not the main factor in preventing cut-out. In the current study, the average TAD value was 24.71 and in the group with complications, it was 27.02. Although positioning the lag screw inferior increased TAD, it was not found to be more predictive for cut-out.
In a study by Kashigar et al. it was stated that the multivariate analysis result was only a predictor for CalTAD cut-out, and that this was a better predictor compared to traditional TAD [8]. However, CalTAD was different from TAD only in the AP view. It was suggested to position the lag screw more inferior in the AP plane and no measurement for lag screw positioning in the lateral plane was specified. The advantage of CalTAD over TAD is that it detects the difference between inferior and superior positioning in the AP plane but a shortcoming is that it does not evaluate the anterior or posterior position in the lateral plane. In the current study, in the TNDR measurement, a more concrete method of measurement was proposed by evaluating the differences in both the AP and lateral planes.
In the study by Parker et al. the positioning of the lag screw in the superior and posterior planes was reported to increase the cut-out risk [10]. In addition, which points would be used for the measurement were not exactly stated. Through a ratio of 0 to 100 for each view, the Parker’s ratio only describes blade direction in an indirect and cumbersome way [10, 28].
Kyle et al. reported that of the lag screws placed in all nine zones described by Clevand et al. [9], the anterior–superior zone and posterior–inferior zone were the ones with the most frequent cut-out [10, 29]. There is no single opinion regarding the best position of the blade in the femoral head, although studies have generally demonstrated that a centre–centre or an inferior–centre position of the blade protects against mechanical failure of inferior–central positioning of the blade and may provide better support for fractures with comminuted posteromedial cortex and allow fracture surface compaction as well as a shorter lever arm, thereby reducing the risk of mechanical failure [30]. In a study by Turgut A. et al., positioning the lag screw in the inferior–posterior position was suggested [20]. In the current study, placing the lag screw in the inferior–posterior position was found to reduce the risk of cut-out.
An important limitation of this study can be considered to be the retrospective design, despite the sufficient size of the patient groups and length of follow-up.
Conclusion
In the literature, there is a general consensus that superior positioning of the lag screw in the femoral head increases the risk of cut-out. However, discussions on whether positioning of the lag should be deep central or inferior still continue. The results of the current study showed that TNDR is a significant measurement method for the prediction of cut-out risk in ITFF treated with cephalomedullary nailing, and it was, therefore, concluded that positioning the lag screw in posterior–inferior reduces the risk of cut-out.
Availability of data
Data are stored by corresponding author of this manuscript and will be shared whenever required.
References
Bjørgul K, Reikeras O (2007) Incidence of hipfracture in southeastern Norway. Int Orthop 31(5):665–669
Xu Z et al (2015) Redisplacement after reduction with intramedullary nails in surgery of intertrochanteric fracture: cause analysis and preventive measure. Arch Orthop Trauma Surg 135(6):751–758
Van Balen R et al (2001) Hip fracture in elderly patients: outcomes for function, quality of life, and type of residence. Clin Orthop Relat Res 390:232–243
Baumgaertner MR, Solberg BD (1997) Awareness of tip-apex distance reduces failure of fixation of trochanteric fractures of the hip. J Bone Joint Surg Br 79(6):969–971
Davis TR, Sher JL, Horsman A et al (1990) Intertrochanteric femoral fractures. Mechanical Failure after internal fixation. J Bone Joint Surg Br 72-B:26–31
Biber R, Berger J, Bail HJ (2016) The art of trochanteric fracture reduction. Injury 47:S3–S6
Kaufer H (1980) Mechanics of thetreatment of hip injuries. Clin Orthop Relat Res 146:53–61
Kashigar A et al (2014) Predictors of failure for cephalomedullary nailing of proximal femoral fractures. Bone Joint J 96(8):1029–1034
Cleveland M, Bosworth DM, Thompson FR, Wilson HJ, Ishizuka T (1959) A ten-year analysis of intertrochanteric fractures of the femur. JBJS 41(8):1399–1408
Parker MJ (1992) Cutting-out of the dynamic hip screw related to its position. J Bone Joint Surg 74(4):625–625
Rubio-Avila J, Madden K, Simunovic N et al (2013) Tip to apex distance in femoral intertrochanteric fractures: a systematic review. J Orthop Sci 18(4):592–598
Thomas AP (1991) Dynamic hip screws that fail. Injury 22(1):45–46
Kuzyk PR, Zdero R, Shah S et al (2012) Femoral head lag screw position for cephalomedullary nails: a biomechanical analysis. J Orthop Trauma 26(7):414–421
Goffin JM, Pankaj P, Simpson AH (2013) The importance of lag screw position for the stabilization of trochanteric fractures with a sliding hip screw: a subject-specific finite element study. J Orthop Res 31(4):596–600
Mainds CC, Newman RJ (1989) Implant failures in patients with proximal fractures of the femur treated with a sliding screw device. Injury 20(2):98–100
Marsh JL (2007) Fracture and dislocation classification compendium-2007: orthopaedic trauma classification, data-base and outcome committee. J Orthop Trauma 21(10):S47–S50
Singh M, Nagrath A, Maini PS (1970) Changes in trabecular pattern of the upper end of the femur as an index of osteoporosis. JBJS 52(3):457–467
Lim SJ, Park YS (2015) Plain radiography of the hip: a review of radiographic techniques and image features. Hip Pelvis 27(3):125–134
Verettas DAJ, Ifantidis P, Chatzipapas CN et al (2010) Systematic effects of surgical treatment of hip fractures: gliding screw-plating vs intramedullary nailing. Injury 41(3):279–284
Turgut A, Kalenderer O, Karapınar L et al (2016) Which factor is most important for occurrence of cut out complications in patients treated with proximal femoral nail antirotation? Retrospective analysis of 298 patients. Arch Orthop Trauma Surg 136(5):623–630
Fujii T, Nakayama S, Hara M et al (2017) Tip-apex distance is most important of six predictors of screw cutout after internal fixation of intertrochanteric fractures in women. JB JS Open Access 2(4):e0022
Yam M, Chawla A, Kwek E (2017) Rewriting the tip apex distance for the proximal femoral nail anti-rotation. Injury 48(8):1843–1847
Den Hartog BD, Bartal E, Cooke F (1991) Treatment of the unstable intertrochanteric fracture. Effect of the placement of the screw, its angle of insertion, and osteotomy. J Bone Joint Surg Am 73:726–733
Jiamton C, Boernert K, Babst R (2018) The nail-shaft-axis of the of proximal femoral nail antirotation (PFNA) is an important prognostic factor in the operative treatment of intertrochanteric fractures. Arch Orthop Trauma Surg 138(3):339–349
Kane P, Vopat B, Heard W et al (2014) Is tip apex distance as important as we think? A biomechanical study examining optimal lag screw placement. Clin Orthop Rel Res 472(8):2492–2498
Mingo-Robinet J, Torres-Torres M et al (2015) Comparative study of the second and third generation of Gamma nail for trochanteric fractures. Review of 218 cases. J Orthop Trauma 29:e85–e90
Herman A, Landau Y, Gutman G et al (2012) Radiological evaluation of intertrochanteric fracture fixation by the proximal femoral nail. Injury 43:856–863
Güven M, Yavuz U, Kadıoğlu B et al (2010) Importance of screw position in intertrochanteric femoral fractures treated by dynamic hip screw. Orthop Traumatol Surg Res 96(1):21–27
Kyle RF, Gustilo RB, Premer RF (2010) Analysis of six hundred and twenty-two intertrochanteric hip fractures. Orthopedic Trauma Directions 8(06):25–29
Hwang JH, Garg AK, Oh JK et al (2012) A biomechanical evaluation of proximal femoral nail antirotation with respect to helical blade position in femoral head: a cadaveric study. Indian J Orthop 46(6):627–632
Funding
No financial support has been received for this study.
Author information
Authors and Affiliations
Contributions
SÇ: methodology and manuscript writing/editing. OS: methodology, data analysis, and manuscript writing/editing. AF: data collection, data analysis, and manuscript editing. İB: methodology and data analysis. AŞ: data collection. KK: manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interests to declare.
Ethical approval
This retrospective study was carried out at Ankara City Hospital Experimental Medicine Research and Application Center with the approval of the Experimental Ethics Committee numbered 72300690–799.
Consent to participate
All authors consent to participate of the present study.
Consent to publish
All authors consent to publish of this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Çepni, Ş., Subaşı, İ.Ö., Şahin, A. et al. Tip–neck distance ratio as a novel predictor for failure in cephalomedullary nailing of unstable trochanteric fractures (UTF). Arch Orthop Trauma Surg 142, 2619–2626 (2022). https://doi.org/10.1007/s00402-021-03999-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03999-6