Abstract
Background
Different approaches are applied for reconstruction in patients with a musculoskeletal malignancy which require a proximal femoral or total femoral resection. We aimed to evaluate the treatment outcomes of patients who underwent a proximal femoral or total femoral resection due to bone and soft tissue tumors and had an endoprosthetic reconstruction by a bipolar hemiarthroplasty type of hip articulation.
Methods
We retrospectively identified 133 patients who underwent a proximal femoral or total femoral endoprosthetic replacement after resection of a bone or soft tissue malignancy. There were 74 male and 59 female patients, with a mean age of 55.02 ± 16.92 years (range 11–84 years) and a median follow-up of 24.47 ± 24.45 months (range 6–164 months). Patient demographics, surgical, and oncological data were recorded. Acetabular wear was measured using the classification proposed by Baker. Functional assessment was performed using the Musculoskeletal Tumor Society (MSTS) functional score.
Results
There was no statistically significant difference among primary diagnostic groups in terms of gender, prosthesis type, trochanter major resection, local recurrence, complication/revision rate, and MSTS Score (p > 0.05, for each parameter). On the other hand, a statistically significant difference was detected in terms of degree of acetabular erosion among diagnostic groups (p < 0.001); the acetabular erosion rate (AER) was found to be lower in patients with metastatic carcinoma than in patients with a diagnosis of primary bone or soft tissue sarcoma. The univariable analysis revealed that the effect of age, primary diagnosis, localization, follow-up time, and presence and number of distant organ metastasis variables on AER were found to be statistically significant (p = 0.018, p = 0.035, p = 0.002, p = 0.007, p = 0.031, p = 0.040, respectively).
Conclusion
In patients who undergo a proximal femoral or a total femoral resection due to a musculoskeletal tumor, bipolar hemiarthroplasty is an adequate type of hip articulation method, since it does not affect the revision requirements and functional outcomes of patients with acetabular erosion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The modular megaprostheses are widely used for reconstruction in patients who undergo a proximal femoral or a total femoral resection due to musculoskeletal tumors [1,2,3,4]. Depending on the patient’s age, functional status and presence of the acetabulum involvement, bipolar or unipolar head hemiarthroplasty or total hip arthroplasty with acetabular replacement can be used. Although hemiarthroplasty has a lower risk of dislocation than total hip arthroplasty, there are studies showing that acetabular erosion is more common, especially in young patients [1, 3,4,5,6].
Bipolar hemiarthroplasty causes less erosion and less protrusion in the acetabulum than unipolar hemiarthroplasty [7]. There are studies showing that acetabular erosion and proximal migration develops as follow-up time increases in patients with non-tumoral conditions who undergo a standard bipolar and unipolar hemiarthroplasty [4, 8,9,10,11,12,13,14]. In addition, it has been shown that following a proximal femoral resection, the rates of acetabular cartilage erosion and acetabular revision surgery requirement were 18.4–35.7% and 0–10.7%, respectively [6, 15,16,17]. Drexler et al. reported that, on 4.6% of patients who underwent a proximal femoral endoprosthetic reconstruction with a bipolar head hemiarthroplasty, they performed a revision surgery requiring acetabular resurfacing (12.3%) at an average of 36 months due to pain, acetabular protrusion and degenerative changes [15]. The most important reason for revising a hemiarthroplasty by a total hip replacement is hip pain caused by acetabular wear [18].
In patients with musculoskeletal tumors involving the femur and requiring a proximal femoral or a total femoral resection, the bone defect can be reconstructed by an endoprosthesis, and a unipolar/bipolar hemiarthroplasty or a total hip arthroplasty is preferred according to the patient's age, current clinical status, and acetabular involvement [1,2,3].
The current study aimed to evaluate the adequacy and effectiveness of bipolar hemiarthroplasty type of hip articulation in patients who underwent a proximal femoral or a total femoral resection due to a musculoskeletal malignancy, including primary bone and soft tissue sarcoma and metastatic carcinoma. The degree of acetabular erosion was compared among the primary diagnostic groups. In addition, a univariate analysis was done to search for the effect of demographic and oncological variables on acetabular erosion rate (AER).
Patients and methods
This retrospective study was conducted upon the approval of our İnstitution's Ethics Committee (03.04.2020. 444). Between January 2008 and April 2019, 133 patients who were diagnosed as primary bone sarcoma, multiple myeloma, metastatic carcinoma, and soft tissue sarcoma at our institution and underwent a proximal femoral or a total femoral resection and endoprosthetic reconstruction by a bipolar hemiarthroplasty were included in the study. The patients treated for non-oncological indications or benign tumors, and who had acetabular involvement and required an acetabular replacement were excluded. All patients were assigned the same approach and technique by two orthopaedic oncological surgeons. The patient’s demographic features (age, gender), histopathological diagnosis, tumor localization, the primary focus in metastatic patients, distant organ metastasis (present/absent), and number of distant organ metastases were recorded. Additionally, the degree of acetabular erosion, the need for revision, and complications including local recurrence were recorded. Retrospective information was obtained from records, patients files, radiographic imaging, and pathological reports. Extended follow-up consisted of clinical visits, serial radiographs, and routine annual patient questionnaires.
The patients were divided into four groups based on diagnosis as primary bone sarcoma, multiple myeloma, metastatic carcinoma, and soft tissue sarcoma. Statistical differences in operative time, perioperative blood loss, survival, local recurrence, presence of distant metastases, number of organs with distant metastasis, development of complications, revision requirement and acetabular erosion were analyzed. We determined the variables which would have a possible effect on acetabular erosion with univariable analysis.
Intravenous antibiotic prophylaxis (1st generation cephalosporins), calculated by age and weight, was given to patients 30 min before surgery. Lateral incision was used in patients who underwent proximal femur resections. The incision was extended to anterolateral aspect of the patellar tendon in patients who underwent a total femoral resection. Oral antibiotic treatment was continued untill the drains were taken out when the amount of total drainage was < 50 cc in 24 h. Anticoagulant therapy was administered for six weeks in patients older than 16 years. All patients were able to walk with a walker on the second or third postoperative day and a brace was not used in any of them.
The complications and failures were classified according to the International Society of Limb Salvage (ISOLS) Committee's modified system, which sub-classifies all five primary types of failure for limb salvage following endoprosthetic and biological reconstruction [19]; these included structural failure (including dislocation), aseptic loosening, periprosthetic fracture, periprosthetic infection and tumor progression with contamination of prosthesis.
The patients' functional outcomes were calculated according to the Musculoskeletal Tumor Society (MSTS) Scoring System [20]. This scoring system looks at six parameters including pain, function, emotional acceptance, use of walking supports, walking ability and gait. Scoring between 0 and 5 is done for each parameter. Then, a total is calculated by adding all points, up to a maximum of 30.
The patients were followed up at our orthopedic oncology outpatient clinic with intervals of 3 months for the first 2 years, intervals of 6 months for the next 3 years, and once every year afterward; physical examination, laboratory data, and anteroposterior (AP) and lateral plain radiographs (X-rays) were recorded for each patient. The probable rate of erosion in the acetabulum due to bipolar hemiarthroplasty was evaluated by two orthopaedic oncological surgeons on plain radiographs using the criteria defined by Baker et al. [21]; the degree of acetabular erosion was rated between 0 and 3 as follows; Grade 0 (no erosion), Grade 1 (narrowing of articular cartilage, no bone erosion), Grade 2 (acetabular bone erosion and early migration), and Grade 3 (protrusio acetabuli).
Statistical analysis
For statistical analyses, the NCSS (number cruncher statistical system) 2007 (Kaysville, Utah, USA) program was used. Descriptive statistical methods (mean, standard deviation, frequency, ratio, minimum, maximum) were used to evaluate the study data. The normal distribution of the quantitative data was tested using the Shapiro–Wilk test and graphical analysis. One-way analysis of variance and Bonferroni-corrected binary evaluations was used to compare more than two groups between normally distributed quantitative variables. Pearson chi-square test, Fisher’s Exact test and Fisher-Freeman-Halton exact test were used to compare qualitative data. Diagnostic screening tests (sensitivity, specificity, PKD, NKD) and ROC analysis were used to determine the parameters' predictive value. Cox regression analysis was used to determine the factors affecting survival. GLMM (Generalized Linear Mixed Model) with a logit link was used to determine the factors affecting the classification of acetabular erosion. Statistical significance was accepted as p < 0.05.
Results
The study cohort included 74 (55.6%) men and 59 (44.4%) women at a mean age of 55.02 ± 16.92 years (range 11–84 years) at the time of surgery. Patients’ demographics, surgical details, adjuvant treatments, oncological and functional data of the patients were given in Tables 1 and 2. Following resection of the tumors with appropriate surgical margins, the proximal femoral endoprostheses (119 patients, 89.5%) and total femoral endoprostheses (14 patients, 10.5%) were applied with bipolar head. There was no statistically significant difference among the groups in terms of gender. On the other hand, a statistically significant difference was detected among the diagnostic groups in terms of age (p < 0.001); the age of the patients with a primary bone sarcoma was found to be lower than the age of the patients with multiple myeloma, metastatic carcinoma, and soft tissue sarcoma (p < 0.001, p = 0.001, p = 0.002, respectively) (Table 1). Further analysis of the study data revealed that there was no statistically significant difference among the diagnostic groups in terms of prosthesis type, trochanter major resection, local recurrence and complication and revision rates (p > 0.05 for each) (Tables 2 and 3).
There was a statistically significant difference among groups in terms of survival (p < 0.001). The survival of the patients with metastatic carcinoma was found to be shorter than the survival of patients with primary bone sarcoma, multiple myeloma, and soft tissue sarcoma (p = 0.003, p = 0.001, p = 0.001, respectively) (Fig. 1). As a result of the univariable analysis using Cox regression analysis, we found that variables of age, primary diagnosis, presence and number of distant organ metastasis had statistically significant effects on survival (p = 0.004, p < 0.001, p = 0.001, p = 0.007, respectively). Determination of variables affecting survival by Cox regression analysis was given in Table 4.
There was a statistically significant difference among the groups in terms of the degree of acetabular erosion (p < 0.001) (Table 5). The acetabular erosion rate (AER) was found to be lower in patients with metastatic carcinoma than in patients with a diagnosis of primary bone sarcoma and soft tissue sarcoma (p = 0.001, p = 0.001, respectively). As a result of univariable analysis, the effect of age, primary diagnosis, follow-up time, presence of distant organ metastasis, number of distant organ metastases, and localization variables on AER were found to be statistically significant (p = 0.018, p = 0.035, p = 0.007, p = 0.031, p = 0.040, p = 0.002, respectively) (Table 6). When a group with AER equals to Grade 0 is taken as reference, it was found that 1 unit increase in survival time increases the probability of AER Grade 1 to 1.139 times [OR (95% CI) 1.139 (1.079–1.202), p < 0.001]. When the group with AER equals to Grade 0 is taken as reference, it was found that 1 unit increase in survival time increases the probability of AER Grade 2 and 3 to 1.181 times [OR (95% CI) 1.181 (1.109–1.257), p < 0.001].
ROC analyses were carried out to determine the availability of survival time in distinguishing AER groups. Five different analyses were performed in order to be able to determine cut-offs, aiming to distinguish between AER = 0 and AER = 1, AER = 0 and AER = 2&3, AER = 0 and AER = 1&2&3, AER = 0&1 and AER = 2&3, and AER = 1 and AER = 2&3 (Table 7).
A statistically significant difference was found between acetabular lysis and complication rates according to the type of endoprosthesis, proximal femoral or total femoral, applied after resection (p < 0.01, p < 0.05, respectively). While the rate of Grade 0 acetabular erosion was high in the proximal femoral endoprosthesis group, the rate of Grade 1, 2, or 3 acetabular erosion was found to be significantly high in total femoral endoprosthesis group (Table 8). In addition, the complication rate was higher following total femoral replacements (Fig. 2).
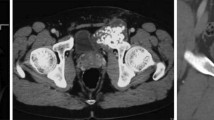
X-rays of the patient who underwent two-stage revision surgery due to infection and erosion. A: A 16-year-old male patient, after proximal femur resection with the diagnosis of Ewing sarcoma in the left proximal femur, a bipolar head and proximal femur prosthesis was applied to the patient. B: In the 56th month of the patient's follow-up, erosion and prosthetic infection developed in the acetabulum C Two-stage revision surgery was performed on the patient.
Accordingly, when life span of the patients was longer than 40 months, sensitivity, specifity, PPV, NPV, accuracy, and Youden index were found to be 100%, 89.43%, 43.5%, 100%, 90.2%, and 0.894, respectively. AuROC value for AER = 1 vs AER = 2&3 was found to be 0.935 [AuROC (95% CI) = 0.935 (0.842–0.982), p < 0.001]. Accordingly, when life span was longer than 40, sensitivity, specifity, PPV, NPV, accuracy, and Youden index were found to be 100%, 74.51%, 43.5%, 100%, 78.7%, and 0.745, respectively. We concluded that these results could be interpreted as "The AER = 0 Group was composed of patients with survival time ≤ 16 months, the AER = 1 Group had a survival time of > 16 and ≤ 40 months, and the AER = 2&3 group had a survival time > 40 months.
In the current study, we did not find any statistical difference among the groups in terms of MSTS Scores. In addition, no statistically significant difference was found among groups based on survival time and of MSTS Scores (p > 0.05) (Table 9).
Discussion
There is an increase in survival of patients with malignant bone and soft tissue tumors due to the advances in chemotherapy and radiotherapy. Limb-sparing surgery has become the standard treatment in many orthopedic oncology centers, partly due to increased patient survival [22]. In limb-sparing surgery, osteochondral allografts, allograft prosthetic composites, and megaprostheses are the preferred reconstruction options after proximal femoral or total femoral resections [22]. Although osteochondral allografts and allograft prosthetic composites are useful in reconstruction of bone defects, they have disadvantages such as non-union, resorption, fracture formation and possible disease transmission [23,24,25]. In their study on 28 patients who received allograft, Jofe et al. stated that the rate of infection was 20%. Nonunion was developed in the graft-host region in two patients, in addition to instability which was observed in one patient [23]. Our study revealed that bipolar hemiarthroplasty is a suitable reconstruction option for patients who underwent proximal femoral and total femoral resections due to a tumoral mass in terms of complication and revision rates, acetabular wear, and functional outcomes. In addition, our study contributes significantly to the literature in revealing the degree of acetabular wear according to the patients' average survival time.
Especially in children, because the acetabulum is not fully developed, superior dysplasia and migration in the lateral acetabulum may develop progressively following bipolar hemiarthroplasty [26]. In adults, insufficiency develops progressively in the superomedial portion of the acetabulum due to cartilage abrasion after hemiarthroplasty which is performed for proximal femoral fractures and degenerative arthritis [10, 12, 14]. Although it has a low dislocation rate, bipolar hemiarthroplasty causes controversy as a treatment option in reconstruction, because it generates acetabular wear in the long-term follow-up [27, 28]. Medial migration with acetabular erosion has been shown in young adults who underwent bipolar hemiarthroplasty after resection with a diagnosis of osteosarcoma in the proximal femur [29]. There are studies reporting that the conversion of bipolar hemiarthroplasty to total hip arthroplasty in the long-term follow-up of orthopedic oncology patients is between 4.6 and 8% [15, 27]. Khodamorad et al. retrospectively analyzed a total of 57 patients with a musculoskeletal malignancy, 29 of whom underwent a bipolar hemiarthroplasty and 28 a total hip prosthesis. The authors stated that the dislocation rate of total hip prosthesis was not higher than the bipolar hemiarthroplasty group and that the functional results were better [30]. There are also studies that do not recommend primary total hip arthroplasty in tumor patients due to the high risk of dislocation [1, 2, 31, 32].
In the current study, we found a statistically significant difference among the diagnostic groups in terms of acetabular wear levels. The degree of acetabular erosion was lower in patients with metastatic carcinoma than patients with primary bone tumor and soft tissue sarcoma. We believe that the low survival rates in metastatic patients was the most important reason for that. The fact that the follow-up time was the only variable which had a significant effect on acetabular wear supported this conclusion. When we searched for effect of survival time on acetabular erosion rates, acetabular erosion was most prevalent, especially in patients with soft tissue sarcoma, because this group had a survival time of longer than 40 months. The least acetabular erosion was observed in the metastatic carcinoma group because the survival time was shorter than 16 months.
Following the reconstruction of proximal femoral tumors with a megaprosthesis, hip dislocation rate ranges from 2 to 28% [25, 33,34,35,36]. In a study comparing the complications seen in two groups with tumor-related hemiarthroplasty and non-tumor hemiarthroplasty, it was stated that the dislocation rate in the tumor group was 3.4% and higher than the non-tumor group [37]. In the current study, total dislocation rate was 3.1% (n = 4). Two patients were in the primary bone tumor group, and one of them had a dislocation accompanied by infection. The remaining two patients were in the multiple myeloma and soft tissue sarcoma groups, and there was no dislocation in the metastatic carcinoma group. We believe that our low dislocation rate was due to our meticulous soft tissue care including capsular repair and abductor mechanism reconstruction after resection. Three out of four dislocations were managed by a one-stage revision of bipolar hemiarthroplasty without a further dislocation. The remaining dislocation which was associated with infection was managed by two-stage revision with a total hip arthroplasty.
Bickels et al. reported that the revision rate due to aseptic loosening was 5% at an average of 6.6 years of follow-up in patients who underwent bipolar hemiarthroplasty after proximal femoral resections [29]. Similarly, Farid et al. stated that the rate of revision due to aseptic loosening was 10% at long-term follow-up in a series of 52 patients who underwent a proximal femur resection [38]. In the current study, the mean follow-up period was 24.47 ± 24.45 months, and we observed aseptic loosening in 2 (1.5%) patients, one in metastatic carcinoma and one in multiple myeloma groups. We believe that the low rate of aseptic loosening was probably due to our relatively short follow-up.
In a study evaluating the functional outcomes of 59 patients who underwent a bipolar hemiarthroplasty, the average MSTS Score was 22 at 21-month postoperative follow-up [1]. Farid et al. reported similar functional outcomes, without a significant difference between metastatic carcinoma and primary bone tumor groups [38]. In the current study, we did not find any statistical difference among the diagnostic groups in terms of MSTS Scores. The results were remarkable in that although there was a difference in degree of acetabular erosion among the diagnostic groups, there was no statistical difference in terms of MSTS Scores.
The limitations of the current study were as follows; (1) it was a retrospective study, (2) the number of patients was not homogeneously distributed among the diagnostic groups, (3) the age distribution among the groups differed and the follow-up period varied depending on the survival time, and (4) there was a low number of patients in soft tissue sarcoma group. On the other hand, the adequacy and effectiveness of bipolar hemiarthroplasty type of hip articulation was investigated extensively in patients who underwent a proximal femoral or a total femoral resection due to a musculoskeletal malignancy.
Conclusion
Considering acetabular erosion was not existent in patients with metastatic carcinoma who had an average survival time of ≤ 16 months, and acetabular erosion was minimal in patients with primary bone tumor and multiple myeloma who had an average survival time of > 16 and ≤ 40 months, we can consider bipolar hemiarthroplasty type of hip articulation is the gold standard for patients who undergo a proximal femoral or total femoral resection for a musculoskeletal malignancy. Even though acetabular erosion was more advanced in soft tissue sarcoma group who had an average survival time of > 40 months, it did not affect the functional outcomes and the need for a revision.
References
Menendez LR, Ahlmann ER, Kermani C, Gotha H (2006) Endoprosthetic reconstruction for neoplasms of the proximal femur. Clin Orthop Relat Res 450:46–51
Ahlmann ER, Menendez LR, Kermani C, Gotha H (2006) Survivorship and clinical outcome of modular endoprosthetic reconstruction for neoplastic disease of the lower limb. J Bone Joint Surg 88-B(6):790–795
Chandrasekar CR, Grimer RJ, Carter SR, Tillman RM, Abudu A, Jeys LM (2009) Unipolar proximal femoral endoprosthetic replacement for tumour: the risk of revision in young patients. J Bone Joint Surg 91-B(3):401–404
Theil C, Möllenbeck B, Gosheger G, Schmidt-Bräkling T, Andreou D, Henrichs MP, Dieckmann R (2019) Acetabular erosion after bipolar hemiarthroplasty in proximal femoral replacement for malignant bone tumors. J Arthroplasty 34(11):2692–2697
Henderson ER, Keeney BJ, Pala E, Funovics PT, Eward WC, Groundland JS et al (2017) The stability of the hip after the use of a proximal femoral endoprosthesis for oncological indications: analysis of variables relating to the patient and the surgical technique. Bone Joint J 99(4):531–537
Van Egmond PW, Taminiau AH, Van der Heide HJ (2013) Hemiarthroplasties in young patients with osteonecrosis or a tumour of the proximal femur; an observational cohort study. BMC Musculoskelet Disord 14(1):31
Bateman JE, Berenji AR, Bayne OMAR, Greyson ND (1990) Long-term results of bipolar arthroplasty in osteoarthritis of the hip. Clin Orthop Relat Res 251:54–66
Bose WJ, Miller GJ, Petty W (1995) Osteolysis of the acetabulum associated with a bipolar hemiarthroplasty. A late complication. JBJS 77(11):1733–1735
Coleman SH, Bansal M, Cornell CN, Sculco TP (2001) Failure of bipolar hemiarthroplasty: a retrospective review of 31 consecutive bipolar prostheses converted to total hip arthroplasty. Am J Orthop 30(4):313–319
Ito H, Matsuno T, Kaneda K (2000) Bipolar hemiarthroplasty for osteonecrosis of the femoral head: a 7-to 18-year followup. Clin Orthop Relat Research 374:201–211
Nakata K, Ohzono K, Masuhara K, Matsui M, Hiroshima K, Ochi T (1997) Acetabular osteolysis and migration in bipolar arthroplasty of the hip: five-to 13-year follow-up study. J Bone Joint Surg 79-B(2):258–264
Vázquez-Vela E, Vázquez-Vela G (1990) Acetabular reaction to the bateman bipolar prosthesis. Clin Orthop Relat Res 251:87–91
Leyshon RL, Matthews JP (1984) Acetabular erosion and the Monk" hard top" hip prosthesis. J Bone Joint Surg 66-B(2):172–174
Houdek MT, Rose PS, Ferguson PC, Sim FH, Griffin AM, Hevesi M, Wunder JS (2019) How often do acetabular erosions occur after bipolar hip endoprostheses in patients with malignant tumors and are erosions associated with outcomes scores? Clin Orthop Relat Res 477(4):777
Drexler M, Gortzak Y, Sternheim A, Kollender Y, Amar E, Bickels J (2015) The radiological evaluation of the hip joint after prosthetic arthroplasty of the proximal femur in patients with a tumour using a bipolar femoral head. Bone Joint J 97(12):1704–1709
Stevenson JD, Kumar VS, Cribb GL, Cool P (2018) Hemiarthroplasty proximal femoral endoprostheses following tumour reconstruction: is acetabular replacement necessary? Bone Joint J 100(1):101–108
Inngul C, Hedbeck CJ, Blomfeldt R, Lapidus G, Ponzer S, Enocson A (2013) Unipolar hemiarthroplasty versus bipolar hemiarthroplasty in patients with displaced femoral neck fractures. A four-year follow-up of a randomised controlled trial. Int Orthop 37(12):2457–2464
Cossey AJ, Goodwin MI (2002) Failure of Austin Moore hemiarthroplasty: total hip replacement as a treatment strategy. Injury 33(1):19–21
Henderson ER, O’connor MI, Ruggieri P, Windhager R, Funovics PT, Gibbons CL et al (2014) Classification of failure of limb salvage after reconstructive surgery for bone tumours: a modified system Including biological and expandable reconstructions. Bone Joint J 96(11):1436–1440
Enneking WF, Dunham WILLIAM, Gebhardt MC, Malawar MARTIN, Pritchard DJ (1993) A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res 286:241–246
Baker RP, Squires B, Gargan MF, Bannister GC (2006) Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck: a randomized, controlled trial. JBJS 88(12):2583–2589
Ilyas I, Pant R, Kurar A, Moreau P, Younge D (2002) Modular megaprosthesis for proximal femoral tumors. Int Orthop 26(3):170–173
Jofe MH, Gebhardt MC, Tomford WW, Mankin HJ (1988) Reconstruction for defects of the proximal part of the femur using allograft arthroplasty. J Bone Joint Surg 70(4):507–516
Mankin HJ, Gebhardt MC, Jennings LC, Springfield DS, Tomford WW (1996) Long-term results of allograft replacement in the management of bone tumors. Clin Orthop Relat Res 324:86–97
Zehr RJ, Enneking WF, Scarborough MT (1996) Allograft-prosthesis composite versus megaprosthesis in proximal femoral reconstruction. Clin Orthop Relat Res 322:207–223
Manoso MW, Boland PJ, Healey JH, Tyler W, Morris CD (2005) Acetabular development after bipolar hemiarthroplasty for osteosarcoma in children. J Bone Joint Surg 87(12):1658–1662
Donati D, Zavatta M, Gozzi E, Giacomini S, Campanacci L, Mercuri M (2001) Modular prosthetic replacement of the proximal femur after resection of a bone tumour: a long-term follow-up. J Bone Joint Surg 83-B(8):1156–1160
Abou Senna WG, Ebeid WA, Moneim MA, Saladin M, Hasan BZ, Badr IT, Karim MA (2020) Long-term outcome of patients with primary or secondary tumors of the proximal femur treated by bipolar modular tumor prosthesis. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03581-6
Kiekens G, Somville J, Taminiau A (2000) Clinical relevance of acetabular erosion in young patients with a bipolar hip prosthesis. Acta Orthop Belg 66(5):455–460
Jamshidi K, Mirkazemi M, Gharedaghi M, Izanloo A, Mohammadpour M, Pisoudeh K et al (2020) Bipolar hemiarthroplasty versus total hip arthroplasty in allograft-prosthesis composite reconstruction of the proximal femur following primary bone tumour resection. Bone Joint J 102(4):524–529
Potter BK, Chow VE, Adams SC, Letson GD, Temple HT (2009) Endoprosthetic proximal femur replacement: metastatic versus primary tumors. Surg Oncol 18(4):343–349
Chandrasekar CR, Grimer RJ, Carter SR, Tillman RM, Abudu AT (2008) Modular endoprosthetic replacement for metastatic tumours of the proximal femur. J Orthop Surg Res 3(1):50
Bickels J, Meller I, Henshaw RM, Malawer MM (2000) Reconstruction of hip stability after proximal and total femur resections. Clin Orthop Relat Res 375:218–230
Ogilvie CM, Wunder JS, Ferguson PC, Griffin AM, Bell RS (2004) Functional outcome of endoprosthetic proximal femoral replacement. Clin Orthop Relat Res 426:44–48
Ward WG, Dorey F, Eckardt JJ (1995) Total femoral endoprosthetic reconstruction. Clin Orthop Relat Res 316:195–206
Calabró T, Van Rooyen R, Piraino I, Pala E, Trovarelli G, Panagopoulos GN et al (2016) Reconstruction of the proximal femur with a modular resection prosthesis. Eur J Orthop Surg Traumatol 26(4):415–421
Schneiderbauer MM, Sierra RJ, Schleck C, Harmsen WS, Scully SP (2005) Dislocation rate after hip hemiarthroplasty in patients with tumor-related conditions. JBJS 87(8):1810–1815
Farid Y, Lin PP, Lewis VO, Yasko AW (2006) Endoprosthetic and allograft-prosthetic composite reconstruction of the proximal femur for bone neoplasms. Clin Orthop Relat Res 442:223–229
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article has ethics committee approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Saglam, F., Baysal, O., Sirin, E. et al. Is bipolar hemiarthroplasty an appropriate type of hip articulation following proximal femoral or total femoral resections for musculoskeletal malignancies?. Arch Orthop Trauma Surg 142, 331–341 (2022). https://doi.org/10.1007/s00402-021-03980-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03980-3