Abstract
Background
The aim of the study is to determine the rate of acute kidney injury (AKI) after hip fracture surgery over the age of 80 and to investigate the factors associated with AKI.
Methods
From January 2015 to January 2020, 589 patients who underwent surgery of hip fractures at our institution were retrospectively reviewed. Serum creatinine (sCr) was analysed daily pre- and postoperatively during the hospital stay. Patients were divided into groups; AKI and non-AKI based on KDIGO (Kidney Disease Global Outcomes) criteria. The incidence, risk factors, and mortality of postoperative AKI were investigated.
Results
Out of 589 patients, 58 developed an AKI (9.8%). Smoking (p: 0.004), pre and postoperative low albumin level (p < 0.05), pre- and postoperative high potassium level (p < 0.05), pre- and postoperative high urea levels (p < 0.05), high amount of intra-operative bleeding (p: 0.003) and prolonged surgery time (p: 0.003) were found to be risk factors associated with AKI. Although the mortality rate was higher in the AKI group, it was not statistically significant (p > 0.05).
Conclusion
AKI is a temporary but common complication following hip fracture surgery, which can also be predicted if risk factors are adequately observed. It typically increases the length of hospital stays, mortality and morbidity.
Level of evidence
Level III evidence, Retrospective comparative study
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Advances in the medical field have contributed significantly to life expectancy, resulting in an ageing population prone to osteoporotic fractures, especially hip fractures [1]. Hip fractures in the elderly are a significant public health problem because they are associated with severe morbidity, mortality and significant socioeconomic burden [2,3,4,5,6,7]. Although excessive mortality following a hip fracture is well-defined in the literature [8, 9], its causes remain largely undefined.
Acute kidney injury (AKI), previously referred to as acute renal failure, has been widely studied among the critically ill [10, 11] and trauma patients [12, 13] and is known to reduce survival significantly. AKI is also a common perioperative complication in surgical patients [14, 15]. Several studies have cited dehydration, blood loss, nephrotoxic drugs [non-steroidal anti-inflammatory drugs (NSAIDs) and antibiotics], and patient comorbidities (such as hypertension, diabetes, and cerebrovascular disease) as significant risk factors for AKI [4, 16]. AKI in surgery can occur under two conditions: (1) hypovolemia due to acute tubular necrosis, pulmonary embolism, heart failure, acute myocardial infarction, sepsis and anaesthesia, while it may present as a prerenal AKI; and (2) renal artery occlusion (thrombus or embolism), drugs and pyelonephritis, while it may present as a renal AKI.
However, postoperative AKI is often unclear in aetiology and is multifactorial. While AKI has been well-studied in elective orthopaedic patients [17,18,19,20], fewer studies are available on low-energy hip fractures [21,22,23]. It is unclear whether current treatment strategies are adequate and effective for AKI, and current concepts emphasise prevention through close monitoring of risk factors for AKI [24, 25]. However, risk factors for AKI after hip fracture surgery remain unclear. Male gender, increased age, diabetes mellitus, pre-existing chronic kidney disease, acute or chronic heart failure, and surgery are risk factors common in patients over 80 years of age; may not be sensitive or specific to these populations [26, 27].
This study’s primary aim was to determine the incidence of postoperative AKI and risk factors in patients over 80 years of age who were operated on for hip fracture. The study’s secondary aim was to compare the postoperative mortality of patients with AKI and patients without AKI.
Patients and methods
A retrospective examination was made of patients hospitalised and treated surgically for proximal femur fractures at the University of Health Sciences, Kanuni Sultan Süleyman Training and Research Hospital Department of Orthopaedics and Traumatology Department, Istanbul, Turkey, between January 1, 2015, and January 1, 2020. All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as amended in 2008. Informed consent was waived due to its retrospective nature. The records of 614 patients over 80 years of age who underwent surgery for femoral neck fracture and intertrochanteric femur fracture were reviewed. Standard diagnosis and treatment were applied to all patients admitted for emergency services with hip fractures and operated on according to the local treatment protocol for various hip fractures under spinal anaesthesia or general anaesthesia.
All surgical procedures were performed in the same institution under a senior surgeon’s supervision (C.E.). As a surgical procedure, cementless bipolar hip arthroplasty, proximal femoral nail, dynamic hip screw, external fixator and proximal femur plate were applied. Criteria for exclusion included a history of renal replacement therapy (RRT), AKI at admission and missing pre or postoperative laboratory data. As a result, 25 patients were excluded (three patients had kidney transplants, 10 patients had AKI at the time of admission, and 12 patients did not have access to their data). Overall, 589 patients operated on for femoral neck fracture or intertrochanteric fracture of the hip joint were included in the final study cohort.
Clinical and laboratory data
Demographic and medical history data of the patients were collected using the Hospital Information System Software, Panates, Istanbul, Turkey. Standard demographic, clinical and physiological data collected included age, sex, time from hospitalisation to surgery, length of hospital stay, primary diagnosis, ASA (American Society of Anesthesiologists) score, smoking status.
All patient medical comorbidities were recorded. These included hypertension, diabetes mellitus, chronic obstructive pulmonary disease, coronary artery disease, chronic renal failure, congestive heart failure, cerebrovascular disease, dementia and malignancy in the body. Reference to an existing disease in the records was considered an adequate definition and used to calculate the Charlson Comorbidity Index.
sCr (serum creatinine) was recorded for up to 7 days after surgery or while the patient was in the clinic. To determine risk factors for the onset of AKI, the following were evaluated:
-
Type of femoral fracture (collum or intertrochanteric).
-
Type of anaesthesia (general or spinal).
-
Surgical treatment method.
-
Length of surgery.
-
Intra-operative blood loss (the amount of bleeding obtained by collecting the amount of blood collected in the aspirator during the operation and the amount of bleeding gauze).
-
Amount of erythrocyte suspension and fresh frozen plasma applied during hospitalisation.
-
Pre-operative and postoperative serum sodium, potassium, albumin, urea, BUN (blood urea nitrogen), haemoglobin, haematocrit, GFR (glomerular filtration rate), and creatinine levels.
Postoperative laboratory evaluations were conducted between 1 and 7 days after surgery. The patients were followed for an average of 23.62 (1–81) months; their mortality in the first 3 months, the first year and total time were compared.
Definition of AKI
The primary goal of the study was to determine the incidence of and factors affecting postoperative AKI. We defined AKI as the change in SCr levels on postoperative days 1 to 7 compared to preoperative levels when admitted to the hospital. According to the criteria in the Improvement of Kidney Disease Global Outcomes (KDIGO), patients were diagnosed with AKI if any of the following conditions were present: ≥ 0.3 mg/dL, (26.5 μmol/L) increase in SCr within 48 h, or an increase in the SCr level of ≥ 1.5 times compared to the baseline value within postoperative 7 days.
Statistics
When evaluating the study’s findings, the IBM SPSS Statistics 22 for statistical analysis (SPSS IBM, Turkey) was used. While analysing the study data, the normal distribution parameters’ suitability was evaluated with the Shapiro–Wilks test. In addition to the descriptive statistical methods (mean, standard deviation, frequency), the Student’s t-test was used to compare normally distributed parameters between the two groups. The Mann–Whitney U test was used to compare abnormally distributed parameters between the two groups. The Chi-squared test was used to compare qualitative data. Fisher’s exact test, the Fisher Freeman Halton test and Continuity (Yates) Correction were also used. A logistic regression analysis was used for multivariate analysis. The Kaplan–Meier analysis and Log Rank test were used for survival analysis. Finally, significance was evaluated at the p < 0.05 level.
Results
Of the 589 patients included in the study, 58 (9.8%) developed AKI. Demographic and clinical characteristics, including laboratory parameters, are presented in Tables 1, 2 and 3.
The incidence of smoking in those patients with AKI (17.2%) was found to be statistically significantly higher than those without AKI (5.8%) (p: 0.004; p < 0.05) (Table 1).
Pre- and postoperative albumin levels in patients with AKI were statistically significantly lower than patients without AKI (p < 0.05). Pre- and postoperative potassium levels were significantly higher in patients with AKI than those without AKI (p < 0.05). In patients with AKI, pre- and postoperative urea values were substantially higher than those without AKI. In addition, the increase in pre- and postoperative urea and BUN levels in the group with AKI was statistically significant (p < 0.05) (Table 3).
The pre-operative and postoperative changes in albumin (p: 0.000; p < 0.05), potassium (p: 0.014; p < 0.05), urea (p: 0.000; p < 0.05), BUN (p: 0.000; p < 0.05), creatinine (p: 0.000; p < 0.05) and GFR (p: 0.000; p < 0.05) values of the patients with AKI were found to be statistically significantly higher than the patients without AKI (Table 3).
In patients with AKI, the amount of intraoperative bleeding (p: 0.003; p < 0.05), length of surgery (p: 0.003; p < 0.05) and length of hospitalisation (p: 0.000; p < 0.05) were found to be statistically significantly higher than patients without AKI (Table 2).
Using logistic regression analysis, we evaluated the effects of smoking, the amount of bleeding, duration of surgery, length of stay, pre–postoperative albumin, pre–postoperative potassium, pre–postoperative urea, postoperative creatinine and postoperative GFR parameters on AKI status. The model results were found to be significant (p: 0.000; p < 0.05); the Negelkerke R square value was 0.731, and the explanatory coefficient of the model (95.2%) was found to be high. While the effect of surgery time was not significant in the model (p > 0.05), the effects of postoperative albumin (p1: 0.000), postoperative potassium (p2: 0.004), pre-operative urea (p3: 0.000), postoperative urea (p4: 0.000) and postoperative GFR (p5: 0.000) were found to be statistically significant (p < 0.05). The effects of surgery time (1.025-fold), postoperative albumin (0.019-fold), postoperative potassium (3.141-fold), pre-operative urea (0.910-fold), postoperative urea (1.055-fold), and postoperative GFR (0.891-fold) were found to have increasing effects on AKI. In the model, the effects of smoking, the amount of bleeding, hospitalisation time, pre-operative albumin, and pre-operative potassium on the incidence of AKI were not statistically significant (p > 0.05) (Table 4).
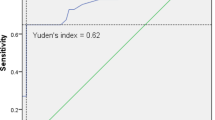
In patients with AKI, 16 (27.6%) of the 58 cases died in the first 3 months (Table 2). The cumulative survival rate for the first-3 months was 72.4%, with a standard error of 5.9%. Of the 531 patients without AKI, 100 (18.8%) died in the first-3 months. For the first-3 months, the cumulative survival rate was 81.2%, with a standard error of 1.7%. When the groups’ survival rates in the first-3 months were evaluated using the Log Rank test, no statistically significant difference was found (p: 0.098; p > 0.05) (Fig. 1).
When the patients’ long-term survival was evaluated, 37 (63.8%) of 58 patients with AKI died (Table 2). The last death occurred in the 64th month; the cumulative survival rate in that period was 32%, with a standard error of 6.6%. The mean life expectancy was 34.67 ± 4.39, and the median was 22 months. Of the 531 patients without AKI, 285 (53.7%) died. The last death occurred in the 64th month, and the cumulative survival rate for the period was 33%, with a standard error of 3.9%. The mean life expectancy was 39.5 ± 1.66, and the median was 31 months. When the groups’ survival rates were evaluated using the Log Rank test, no statistically significant difference was found (p: 0.282; p > 0.05) (Fig. 2).
Discussion
In this study, the rate of AKI was 9.8%. In one of the most extensive studies in the literature on AKI incidence following hip fracture surgery, an incidence of 12.7% was found in 13,529 patients in Denmark [28]. The literature concludes that the AKI rate in high-energy traumas varies between 15 and 40% [12,13,14]; in hip fractures, this rate is between 15 and 24% [4, 21]. We believe the lower rate of AKI in our study compared to the literature is due to fluid supplementation starting in the emergency department, especially in elderly patients, and the severe avoidance of nephrotoxic drugs. In addition, this study observed that the waiting times from trauma to surgery were longer than those in the literature [23, 29]. In our institution, surgery is performed after optimal conditions are achieved for advanced elderly patients; this may contribute to a lower rate of AKI.
Reported risk factors for AKI in hip fracture patients are advanced age, male gender, peripheral vascular diseases, vascular occlusive disease, hypertension, diabetes, chronic obstructive pulmonary disease, chronic kidney disease, congestive heart disease, emergency surgery, and pre-illness use of nephrotoxic drugs [4, 21]. However, the evidence on this subject is not sufficient. In this study, we observed that gender, comorbid diseases, ASA score, and length of emergency surgery were not statistically related to the onset of AKI. However, the rate of smoking was found to be statistically higher in patients with AKI. Still, when evaluated using regression analysis, the effect of tobacco on AKI was not found to be statistically significant. Ritz et al concluded in their study that smoking increased renovascular resistance by 11% and, consequently, there was a 15% reduction in GFR [30].
Ulucay et al found that the amount of intraoperative bleeding is a significant risk factor for the onset of AKI [21]. In this study, we observed that the amount of bleeding and length of surgery, which are among the intraoperative factors, were significantly higher in patients with AKI. However, when this finding was evaluated using regression analysis, the effect of bleeding on the incidence of AKI was not statistically significant. Because the two groups in this study were similar in the amount of perioperative transfusion, we concluded that postoperative AKI might occur in patients with massive bleeding if appropriate blood transfusion is not performed.
The literature has shown that postoperative hypoalbuminemia is an independent risk factor for the onset of postoperative AKI [23, 29]. Available data indicate that albumin maintains colloid osmotic pressure, increases adequate circulating volume, promotes increased renal blood flow, and preserves renal function [31]. Albumin also maintains renal perfusion, glomerular filtration, and medullary fluid reabsorption [31]. In addition, Ulucay et al found that postoperative potassium levels in patients with AKI were higher than in patients without AKI [21]. In this study, when patients with AKI were evaluated using regression analysis, the effects of postoperative albumin, postoperative potassium, pre-operative urea, postoperative urea and postoperative GFR parameters were found to be statistically significant.
Many studies in the literature evaluated early mortality after AKI. Pedersen et al. found that 1717 (12.7%) of 13,529 patients had AKI within 5 days of surgery; the mortality rate in those patients increased 2.8 times in the first-3 months, and the mortality rate beyond 3 months rose by a factor of 1.3 [28]. Rantalaiho et al reported a 3-month mortality rate of 35% in patients with AKI and 12.7% in those without AKI [22]. In this study, although the mortality rate in the first-3 months and long-term was found to be higher in patients with AKI than those without AKI, the difference was not statistically significant.
There are several limitations to this study. The study was a retrospective observational study conducted at a single institution. AKI was defined according to increments in the sCr level only, not in urine output, which correlates with renal function [4, 32]. Due to insufficient analyses, patients with AKI could not be further divided into prerenal, renal, and postrenal groups. Although the drugs used after hospitalisation were prescribed according to their renal functions, and if nephrotoxic drugs, especially NSAIDs, are avoided starting from hospitalisation in this age group, the nephrotoxic effects of the drugs used daily and the drugs prescribed for anaesthesia could not be examined due to the lack of homogeneity. In fact, polypharmacy involving nephrotoxic drugs such as ACE inhibitors, aminoglycoside and NSAIDs were frequently observed in the patient population enrolled in the study. However, due to the multiplicity of drug combinations, it was impossible to determine the effects of these drugs alone. In addition, the cost of AKI to the healthcare system was not evaluated in this study. However, it is not difficult to predict that costs will increase because AKI prolongs the length of stay and creates additional treatment burdens. It is also known that sCr and GFR levels depend on muscle mass. Decrease in muscle mass, especially in elderly patients, has an undeniable effect on kidney functions. Another limitation of the study is that muscle mass in patients is not taken into account. In addition, since most of the patients were referred to our center from an external center, detailed information about the pre-operative functional capacities of the patients could not be provided.
Conclusion
AKI is a temporary but common complication following hip fracture surgery. It typically increases the length of hospital stays, mortality and morbidity. In this study, we determined that basal kidney functions, postoperative albumin and potassium levels are independent factors contributing to the onset of AKI. In addition, smoking, lengthy surgery time and excessive intra-operative bleeding may lead to AKI. Surgeons should be alert to the development of AKI and minimise preventable risk factors. Nephrological consultation should be requested for patients in high-risk groups.
References
Arias E (2014) United States life tables, 2009. Natl Vital Stat Rep 62(7):1–63
Mullen JO, Mullen NL (1992) Hip fracture mortality: a prospective, multifactorial study to predict and minimize death risk. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-199207000-00028
Bass E, French DD, Bradham DD, Rubenstein LZ (2007) Risk-adjusted mortality rates of elderly veterans with hip fractures. Ann Epidemiol. https://doi.org/10.1016/j.annepidem.2006.12.004
Bennet SJ, Berry OMB, Goddard J, Keating JF (2010) Acute renal dysfunction following hip fracture. Injury. https://doi.org/10.1016/j.injury.2009.07.009
Choi HJ, Shin CS, Ha YC, Jang SM, Jang SH, Park CM, Yoon HK, Lee SS (2012) Burden of osteoporosis in adults in Korea: a national health insurance database study. J Bone Miner Metab. https://doi.org/10.1007/s00774-011-0280-x
Stewart NA, Chantrey J, Blankley SJ, Boulton C, Moran CG (2011) Predictors of 5 year survival following hip fracture. Injury. https://doi.org/10.1016/j.injury.2010.12.008
Castronuovo E, Pezzotti P, Franzo A, Di Lallo D, Guasticchi G (2011) Early and late mortality in elderly patients after hip fracture: a cohort study using administrative health databases in the Lazio region. BMC Geriatr, Italy. https://doi.org/10.1186/1471-2318-11-37
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int. https://doi.org/10.1007/s00198-012-1964-3
Panula J, Pihlajamäki H, Mattila VM, Jaatinen P, Vahlberg T, Aarnio P, Kivelä SL (2011) Mortality and cause of death in hip fracture patients aged 65 or older—a population-based study. BMC Musculoskelet Disord. https://doi.org/10.1186/1471-2474-12-105
Gaieski DF, Edwards JM, Kallan MJ, Carr BG (2013) Benchmarking the incidence and mortality of severe sepsis in the United States. Crit Care Med. https://doi.org/10.1097/CCM.0b013e31827c09f8
Wohlauer MV, Sauaia A, Moore EE, Burlew CC, Banerjee A, Johnson J (2012) Acute kidney injury and posttrauma multiple organ failure: the canary in the coal mine. J Trauma Acute Care Surg. https://doi.org/10.1097/TA.0b013e318244869b
Skinner DL, Hardcastle TC, Rodseth RN, Muckart DJJ (2014) The incidence and outcomes of acute kidney injury amongst patients admitted to a level I trauma unit. Injury. https://doi.org/10.1016/j.injury.2013.07.013
Eriksson M, Brattström O, Mårtensson J, Larsson E, Oldner A (2015) Acute kidney injury following severe trauma: risk factors and long-term outcome. J Trauma Acute Care Surg. https://doi.org/10.1097/TA.0000000000000727
Bihorac A, Yavas S, Subbiah S, Hobson CE, Schold JD, Gabrielli A, Layon AJ, Segal MS (2009) Long-term risk of mortality and acute kidney injury during hospitalization after major surgery. Ann Surg. https://doi.org/10.1097/SLA.0b013e3181a40a0b
Harris DG, McCrone MP, Koo G, Weltz AS, Chiu WC, Scalea TM, Diaz JJ, Lissauer ME (2015) Epidemiology and outcomes of acute kidney injury in critically ill surgical patients. J Crit Care. https://doi.org/10.1016/j.jcrc.2014.07.028
de Luise C, Brimacombe M, Pedersen L, Sørensen HT (2008) Comorbidity and mortality following hip fracture: a population-based cohort study. Aging Clin Exp Res. https://doi.org/10.1007/BF03325146
Jämsä P, Jämsen E, Lyytikäinen LP, Kalliovalkama J, Eskelinen A, Oksala N (2017) Risk factors associated with acute kidney injury in a cohort of 20,575 arthroplasty patients. Acta Orthop. https://doi.org/10.1080/17453674.2017.1301743
Perregaard H, Damholt MB, Solgaard S, Petersen MB (2016) Renal function after elective total hip replacement. Acta Orthop. https://doi.org/10.3109/17453674.2016.1155130
Kimmel LA, Wilson S, Janardan JD, Liew SM, Walker RG (2014) Incidence of acute kidney injury following total joint arthroplasty: a retrospective review by RIFLE criteria. Clin Kidney J. https://doi.org/10.1093/ckj/sfu108
Bell S, Dekker FW, Vadiveloo T, Marwick C, Deshmukh H, Donnan PT, Van Diepen M (2015) Risk of postoperative acute kidney injury in patients undergoing orthopaedic surgery-development and validation of a risk score and effect of acute kidney injury on survival: Observational cohort study. BMJ. https://doi.org/10.1136/bmj.h5639
Ulucay C, Eren Z, Kaspar EC, Ozler T, Yuksel K, Kantarci G, Altintas F (2012) Risk factors for acute kidney injury after hip fracture surgery in the elderly individuals. Geriatr Orthop Surg Rehabil. https://doi.org/10.1177/2151458512473827
Rantalaiho I, Gunn J, Kukkonen J, Kaipia A (2019) Acute kidney injury following hip fracture. Injury. https://doi.org/10.1016/j.injury.2019.10.008
Kang JS, Moon KH, Youn YH, Park JS, Ko SH, Jeon YS (2020) Factors associated with postoperative acute kidney injury after hip fractures in elderly patients. J Orthop Surg. https://doi.org/10.1177/2309499019896237
Thiele RH, Isbell JM, Rosner MH (2015) AKI associated with cardiac surgery. Clin J Am Soc Nephrol. https://doi.org/10.2215/CJN.07830814
Waikar SS, Liu KD, Chertow GM (2008) Diagnosis, epidemiology and outcomes of acute kidney injury. Clin J Am Soc Nephrol. https://doi.org/10.2215/CJN.05191107
Kheterpal S, Tremper KK, Heung M, Rosenberg AL, Englesbe M, Shanks AM, Campbell DA (2009) Development and validation of an acute kidney injury risk index for patients undergoing general surgery: results from a national data set. Anesthesiology. https://doi.org/10.1097/ALN.0b013e3181979440
National Clinical Guideline Centre (UK) (2013) Acute kidney injury: prevention, detection and management up to the point of renal replacement therapy [Internet]. London: Royal College of Physicians (UK)
Pedersen AB, Christiansen CF, Gammelager H, Kahlert J, Sorensen HT (2016) Risk of acute renal failure and mortality after surgery for a fracture of the hip: a population-based cohort study. Bone Jt J. https://doi.org/10.1302/0301-620X.98B8.37497
Shin KH, Han SB (2018) Early postoperative hypoalbuminemia is a risk factor for postoperative acute kidney injury following hip fracture surgery. Injury. https://doi.org/10.1016/j.injury.2018.05.001
Ritz E, Benck U, Franek E, Keller C, Seyfarth M, Clorius J (1998) Effects of smoking on renal hemodynamics in healthy volunteers and in patients with glomerular disease. J Am Soc Nephrol. https://doi.org/10.1681/ASN.V9101798
Margarson MP, Soni N (1998) Serum albumin: touchstone or totem? Anaesthesia. https://doi.org/10.1046/j.1365-2044.1998.00438.x
MacEdo E, Malhotra R, Claure-Del Granado R, Fedullo P, Mehta RL (2011) Defining urine output criterion for acute kidney injury in critically ill patients. Nephrol Dial Transplant. https://doi.org/10.1093/ndt/gfq332
Acknowledgements
We thank Sibel Kanat for assistance in the statistical analysis of our data and preparation of table for this article.
Funding
No funding was received for this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Agar, A., Gulabi, D., Sahin, A. et al. Acute kidney injury after hip fracture surgery in patients over 80 years of age. Arch Orthop Trauma Surg 142, 2245–2252 (2022). https://doi.org/10.1007/s00402-021-03969-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03969-y