Abstract
Introduction
This report is the first study to compare the clinical outcomes between cementless and cemented femoral prostheses in total hip arthroplasty (THA) with subtrochanteric femoral shortening osteotomy for Crowe type IV hips.
Materials and methods
We identified 26 hips in 20 patients who had undergone cemented (n = 13) or cementless (n = 13) THA with subtrochanteric femoral shortening osteotomy for Crowe type IV hips with a minimum follow-up period of 2 years. The mean follow-up period was 60.8 ± 33.9 months (24–120 months). We compared radiological findings, postoperative clinical recoveries, postoperative complications, and implant survival rates.
Results
In both groups, there were no cases of aseptic loosening for the acetabular and femoral implant. In terms of bone union at the osteotomy site, the mean duration was significantly longer in the cemented group (9.8 ± 4.2 months) than in the cementless group (5.0 ± 1.9 months). The clinical hip score in gait and pain at 3 months postoperatively was significantly higher in the cemented group than in the cementless group, while there were no significant changes at other timepoints between two groups. The number of postoperative complications was not significantly different between the two groups. The implant survival rate was 92% in the cementless group and 100% in the cemented group at 5 years postoperatively (P = 0.31).
Conclusions
The cemented femoral prosthesis is superior to the cementless femoral prosthesis for early clinical recovery, while the duration required to achieve bone union at the osteotomy site is longer in the cemented femoral prostheses. It is possible for surgeons to perform successful hip reconstructions, regardless of the fixation method used for THA with shortening femoral osteotomy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Developmental dysplasia of the hip (DDH) is well known to be a common cause of secondary osteoarthritis (OA). Total hip arthroplasty (THA) is a successful orthopedic procedure for patients with OA [1]. However, THA for severely dislocated hips, such as Crowe type IV hips, has been extremely challenging because of the poor bone quality and bone stock on the acetabulum, severe femoral canal deformity, abnormal femoral anteversion, and severe limb length discrepancy (LLD) [2]. The insertion of the implant at the correct orientation and angle on the acetabular side is challenging because the acetabular anatomy of patients with Crowe type IV hips is extremely different from that of patients with normal hip OA [3, 4]. Moreover, a subtrochanteric femoral shortening osteotomy during THA is often required for Crowe type IV hips to achieve the restoration of the center of rotation and prevent an excessively lengthened limb that may result in excessive soft tissue tension, abductor impairment, and postoperative nerve palsy [5, 6].
Previous studies have reported the clinical effectiveness of cemented or cementless THA with subtrochanteric femoral shortening osteotomy [7,8,9,10]. We performed cementless THA with subtrochanteric femoral shortening osteotomy for severely dislocated hips until 2013. However, due to the concern for late clinical recovery in patients with a cementless femoral prosthesis, we adopted a hybrid THA with femoral shortening osteotomy technique for Crowe type IV hips. Using the cemented stem may lead to a favorable clinical recovery during the early postoperative period. To our knowledge, no study has compared the clinical outcomes between THA using a cementless femoral prosthesis and THA using a cemented femoral prosthesis with femoral shortening osteotomy for Crowe type IV hips.
The purpose of this retrospective study was to compare the clinical outcomes between cementless and cemented femoral prostheses in THA with subtrochanteric femoral shortening osteotomy for Crowe type IV hips.
Materials and methods
This investigational protocol was conducted with the approval of the institution’s ethics committee. In accordance with the requirements of this study, informed consent was obtained from all patients. This study was conducted according to the principles of the Declaration of Helsinki.
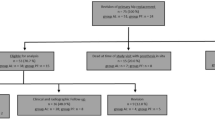
This retrospective study includes a consecutive series of 27 hips in 21 patients (4 men and 17 women) who underwent primary THA with subtrochanteric femoral shortening osteotomy for Crowe type IV hips between January 2009 and March 2017. The patients were followed up for a minimum of 2 years. One patient who was followed up for less than two years was excluded from this study, resulting in a total of 26 hips in 20 patients (4 men and 16 women) in the final analysis. We manually retrieved the patients’ detailed demographic data including sex, age, operative side, body mass index (BMI), follow-up duration, American Society of Anesthesiologist Physical Status (ASA-PS), and etiology of the hip disorder (secondary acetabulum or neglected dislocated hip).
Operative procedure
All operations were performed by the senior surgeon (T.K) via a posterolateral approach with the patients in a lateral decubitus position. After the resection of the femoral head, the tendinous insertion of the gluteus maximus was cut from the femoral shaft to enlarge the acetabular field. The joint capsule and fibrous tissue around the acetabulum were resected carefully and completely to accurately locate the true acetabula. Then, we reamed the true acetabula using a computed tomography (CT)-based navigation system (Stryker Inc., Mahwah, NJ) while confirming the depth or height of the acetabular reaming according to the preoperative plan. When the cementless acetabular component was used, it was press fitted to the true acetabulum according to the CT-based navigation system, and an intraoperative anteroposterior hip radiography was performed to ensure the appropriate inclination or anteversion was achieved. Then, we used augmented screws to achieve an adequate initial fixation. When the cemented acetabular shell was used, we inserted it on the true acetabulum according to the CT-based navigation system after checking the inclination or anteversion of the trial component via an intraoperative hip X-ray image.
Next, we performed a V-shaped subtrochanteric osteotomy at a distance of 2 cm distal to the lesser trochanter using a V-shaped osteotomy device [11]. The amount of intraoperative femoral shortening was determined preoperatively, ensuring that maximum leg lengthening was limited to approximately 35 mm to prevent postoperative nerve palsy. When the cementless hip stem was used we used the S-ROM-A Modular Hip System (DePuy Synthes, Warsaw, IN) in 9 hips and the K-MAX S-LOCK distal interlocking stem (Kyocera, Japan) in 4 hips. When the cemented stem was used, we used the Exeter hip stem (Stryker, Mawhaw, NJ) in all hips. We fixed both fragments with a cerclage in cementless stems to prevent rotational instability after the final femoral stem insertion (Fig. 1). The cementing procedure was performed in the usual manner in cemented stems; however, the proximal and distal femoral fragments were reduced with large bone clamps. We inserted the cemented femoral stem on the femur and then performed an on-lay bone grafting longitudinally to the osteotomy site. The bone graft was acquired from the subtrochanteric bone that was resected during the femoral shortening osteotomy. The on-lay grafts were fixed with a cerclage wire (Fig. 2).
The postoperative rehabilitation schedule in patients with a cementless femoral stem was free weight bearing at 4 weeks postoperatively and full weight bearing at 6 weeks postoperatively. In patients with a cemented femoral stem, free weight bearing was allowed as soon as possible after the operation.
Assessment
To compare the clinical outcomes between the cementless and cemented femoral prostheses, we divided the patients according to the type of prosthesis received (cementless group and cemented group).
We retrieved the operative time, intraoperative bleeding amount, and amount of intraoperative femoral shortening from each patient’s medical records. The preoperative or postoperative vertical and horizontal distances of the center of the femoral head were evaluated on the anteroposterior hip radiographs. The vertical center of the femoral head was defined as the distance between the inter-teardrop reference line and the center of the femoral head, and the horizontal center of the femoral head was defined as the distance between a perpendicular reference line drawn through the teardrop and the center of the femoral head. The amount of leg lengthening was calculated from the preoperative and postoperative anteroposterior hip radiographs, as previously described [12].
We investigated aseptic loosening of the acetabular or femoral implant during the follow-up period for all patients using follow-up hip radiographs. Next, bone union at the osteotomy site was assessed on the postoperative radiographs according to the criteria for bone union described by Masonis et al. [13].
In the clinical evaluation, the hip function was evaluated using the Japanese Orthopaedic Association (JOA) hip score [14]. The JOA hip score includes the scores of pain (40 points), range of motion (20 points), walking (20 points), and activities of daily living (20 points), with a maximum score of 100 points. Clinical hip evaluation was evaluated by the senior surgeon. Each score of JOA hip score at preoperatively, 3 months, 6 months, and 1 year postoperatively and at the final follow-up were compared between the cementless and cemented groups.
Next, we summarized the postoperative complications, including postoperative implant dislocation, aseptic loosening of the implant, vessel or nerve injury, and postoperative infection including surgical site infection (SSI) or periprosthetic joint infection (PJI), using the data from the medical database. Furthermore, we investigated any additional surgeries performed due to these complications.
Finally, a survival analysis was performed with the Kaplan–Meier method to estimate the cumulative probabilities of failure, which were compared between the two groups. The end point was defined as requiring an additional surgery due to any postoperative complications.
Statistical analysis
All statistical analyses were performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria) [15]. The Fisher’s exact probability test was used to assess the differences in sex, operative side, etiology of the hip disorder, ASA-PS, and postoperative complications between the two groups. The Mann–Whitney U test was used to assess the differences in mean age, follow-up duration, BMI, operative information, JOA score, and mean duration of bone union at the osteotomy site between the two groups. A P value < 0.05 was considered statistically significant.
Results
The mean age of all patients was 68.9 ± 6.4 years (range 50–77 years). The patients were followed up for a mean duration of 60.8 ± 33.9 months (range 24–120 months). The demographic characteristics of the cementless and cemented groups are shown in Table 1. Only the mean follow-up duration was significantly different between the two groups (P = 0.01), because we used cemented THA with femoral shortening osteotomy for Crowe type IV hips only after 2014.
The results of the operative assessment are shown in Table 2. There were no statistical differences in the operative time, intraoperative bleeding amount, amount of leg lengthening, and femoral shortening, calculated intraoperative leg lengthening, precenter of rotation, or postcenter of rotation between the two groups.
There were no cases of aseptic loosening of the acetabular and femoral implant. The mean duration to bone union was significantly longer in the cemented group (9.8 ± 4.2 months) than in the cementless group (5.0 ± 1.9 months) (P < 0.001). No patient in either group experienced pseudo-arthrosis or required additional surgery at the osteotomy site (Table 3).
The mean JOA score and mean each JOA score are shown in Figs. 3 and 4. The preoperative JOA score was significantly different between the groups (P = 0.02), while there was no statistical difference in the JOA score at other timepoints (Fig. 3). The recovery of pain and gait were significantly different between both groups at 3 months postoperatively (P < 0.05). (Fig. 4a–d)
The postoperative complications are shown in Table 4. Three hips in the cementless group had postoperative dislocations, all due to neglected dislocated hips. Only one of the dislocated hips required additional surgery. No acetabular or femoral implant loosening, nerve injury, or SSI or PJI were reported. There was no significant difference in the number of postoperative complications between the two groups.
The survival rate, defined as not requiring additional surgery due to any complications, was 92% (95% confidence interval (CI) 78–100%) in the cementless group and 100% (95% CI 100%) in the cemented group at 5 years postoperatively (P = 0.31) (Fig. 5).
Discussion
There are few previous reports regarding the use of a cemented or cementless femoral prosthesis for THA with femoral shortening osteotomy. Wang et al. investigated 76 hips in 62 patients who underwent cementless THA with femoral shortening osteotomy at a mean follow-up duration of 10 years. This study showed that 97% of patients did not require revisions for any reason [16]. Grappiolo et al. investigated 102 hips in 74 patients who underwent cementless THA with femoral shortening osteotomy at a mean follow-up duration of 11.3 years and reported that 96% of patients did not require a stem revision for any reason [17]. Kawai et al. reported that the short-term results of cemented THA with femoral shortening osteotomy are satisfactory and that revisions are not typically required [18]. Charity et al. also reported favorable mid-to-long-term clinical results of a cemented femoral stem for Crowe type IV hips, as none of the patients in their study required revisions for any reason [19]. However, no study has compared the clinical results between cementless and cemented femoral stems. We found that there was no statistical difference in the perioperative complications and mid-term clinical results between the two techniques, suggesting that it is possible to perform a successful hip reconstruction for Crowe Type IV hips using a cementless or a cemented femoral stem.
The disadvantage of using a cemented femoral stem for THA with femoral shortening osteotomy is the late timing of bone union at the osteotomy site, while the disadvantage of using a cementless femoral stem is the risk of intraoperative fracture. Oe et al. reported that the completion of bone union at the osteotomy site in cemented stems required an average of 8 months, while Wang et al. and Hasegawa et al. reported that the average duration required for bone union at the osteotomy site in cementless stems was 3–6 months [8, 16, 20]. Our results also indicate that the average duration of bone union at the osteotomy site in the cemented group is significantly longer than that in the cementless group. This may be related to the reduction of bone supply around the osteotomy site due to the bone cement. We believe that the prevention of the development of pseudoarthrosis around the osteotomy site in cemented stems can be attributed to two factors. Firstly, the V-shaped osteotomy device minimizes bone cement leakage around the osteotomy site due to the correspondence with proximal and distal bone fragments. Secondly, the strut on-lay bone graft of the resected femoral shaft bone to the osteotomy site (which was performed in all cases) prevents pseudoarthrosis around the osteotomy site.
The results of our study show that the clinical recovery of hip function at 3 months postoperatively was more favorable in the cemented group than in the cementless group. This may be due to the fact that postoperative weight bearing was immediately possible in the cemented group as the cement achieves the initial fixation stability around the osteotomy site, subsequently allowing for early walking rehabilitation and a faster recovery. Moreover, using the cemented femoral stem may lead to early clinical recovery due to pain reduction in the postoperative thigh, as previous reports have indicated that the postoperative thigh pain is lower when using the cemented femoral stem than when using the cementless femoral stem [21, 22]. Although our study did not show any statistical difference in the mid-term clinical results between the two femoral fixation methods, the use of the cemented femoral stem for THA with shortening femoral osteotomy may lead to early clinical recovery. Thus, using a cemented femoral stem for this procedure may be indicated for patients with bilateral Crowe type IV hips, as this will minimize the interval of the surgery and postoperative rehabilitation on the contralateral side.
Our study was not without limitations. First, it is a retrospective study, and the number of patients included was relatively small, although this is due to the rarity of Crowe type IV hips. Second, the mean follow-up duration of the cemented group was shorter than that of the cementless group. This could not be avoided as we started using the cemented femoral stem for Crowe Type IV hips only after 2014. Thus, a long-term follow-up of the cemented group is necessary. Third, the method for the assessment of bone union around the osteotomy site was not powerful as we did not use CT or digital tomosynthesis. However, our method of using X-rays to evaluate bone healing around an osteotomy site is consistent with previous reports [8, 13, 16]. Lastly, patients with a cementless femoral stem were permitted full weight bearing after 6 weeks postoperatively in this study. This may influence JOA hip score in gait between preoperative and 3-month postoperatively.
Despite these limitations, we conclude that in terms of early clinical recovery, the cemented femoral stem is superior to the cementless femoral stem. However, the duration required to achieve bone union at the osteotomy site is longer in the cemented femoral stem. Importantly, it is possible for surgeons to perform successful hip reconstructions regardless of the femoral stems used for THA with shortening femoral osteotomy.
References
Devane PA, Wraighte PJ, Ong DCG, Horne JG (2012) Do joint registries report true rates of hip dislocation? Clin Orthop Relat Res 470(11):3003–3006
Charnley J, Feagin JA (1973) Low-friction arthroplasty in congenital subluxation of the hip. Clin Orthop Rel Res 91:98–113
Yoshitani J, Kabata T, Kajino Y, Ueno T, Ueoka K, Nakamura T, Tsuchiya H (2019) Morphometric geometrical analysis to determine the centre of the acetabular component placement in Crowe type IV hips undergoing total hip arthroplasty. Bone Joint J 101(2):189–197
Ueoka K, Kabata T, Kajino Y, Yoshitani J, Ueno T, Tsuchiya H (2019) The accuracy of the computed tomography-based navigation system in total hip arthroplasty is comparable with Crowe type IV and Crowe type I dysplasia: a case–control study. J Arthroplasty 34(11):2686–2691
Bernasek TL, Haidukewych GJ, Gustke KA et al (2007) Total hip arthroplasty requiring subtrochanteric osteotomy for developmental hip dysplasia: 5 to 14year results. J Arthroplasty 22(2):145–150
Lai KA, Shen WJ, Huang LW et al (2005) Cementless total hip arthroplasty and limblength equalization in patients with unilateral Crowe type-IV hip dislocation. J Bone Joint Surg Am 87(2):339–345
Takao M, Ohzono K, Nishii T, Miki H, Nakamura N, Sugano N (2011) Cementless modular total hip arthroplasty with subtrochanteric shortening osteotomy for hips with developmental dysplasia. J Bone Joint Surg Am 93(6):548–555
Oe K, Iida H, Nakamura T, Okamoto N, Wada T (2013) Subtrochanteric shortening osteotomy combined with cemented total hip arthroplasty for Crowe group IV hips. Arch Orthop Trauma Surg 133(12):1763–1770
Rollo G, Solarino G, Vicenti G, Picca G, Carrozzo M, Moretti B (2017) Subtrochantericfemoralshorteningosteotomycombined with cementless total hip replacement for Crowe type IV developmental dysplasia: a retrospective study. J Orthop Traumatol. 18(4):407–413
Akiyama H, Kawanabe K, Yamamoto K, Kuroda Y, So K, Goto K, Nakamura T (2011) Cemented total hip arthroplasty with subtrochanteric femoral shortening transverse osteotomy for severely dislocated hips: outcome with a 3 to 10-year follow-up period. J Orthop Sci 16(3):270–277
Hotokebuchi T, Sonohata M, Shigematsu M, Mawatari M (2006) A new device for a V-shaped subtrochanteric osteotomy combined with total hip arthroplasty. J Arthroplasty 21(1):135–137
Kabata T, Kajino Y, Inoue D, Ohmori T, Yoshitani J, Ueno T, Ueoka K, Tsuchiya H (2019) Safety range for acute limb lengthening in primary total hip arthroplasty. Int Orthop 43(9):2047–2056
Masonis JL, Patel JV, Miu A, Bourne RB, McCalden R, Macdonald SJ, Rorabeck CH (2003) Subtrochanteric shortening and derotational osteotomy in primary total hip arthroplasty for patients with severe hip dysplasia: 5-year follow-up. J Arthroplasty 18(1):68–73
Shima Y (1971) Standard for evaluation of osteoarthritis of the hip. Nippon Seiekeigekagakkai Zasshi 45:813–833 ((in Japanese))
Kanda Y (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48(3):452–458
Wang D, Li LL, Wang HY, Pei FX, Zhou ZK (2017) Long-termresults of cementlesstotal hip arthroplasty with subtrochanteric shortening osteotomy in Crowe type IV developmental dysplasia. J Arthroplasty 32(4):1211–1219
Grappiolo G, La Camera F, Della Rocca A, Mazziotta G, Santoro G, Loppini M (2019) Total hip arthroplasty with a monoblockconicalstem and subtrochanteric transverse shortening osteotomy in Crowe type IV dysplastic hips. Int Orthop 43(1):77–83
Kawai T, Tanaka C, Ikenaga M, Kanoe H (2011) Cemented total hip arthroplasty with transverse subtrochanteric shortening osteotomy for Crowe group IV dislocated hip. J Arthroplasty 26(2):229–235
Charity JA, Tsiridis E, Sheeraz A, Howell JR, Hubble MJ, Timperley AJ, Gie GA (2011) Treatment of Crowe IV high hip dysplasia with total hip replacement using the Exeter stem and shortening derotational subtrochanteric osteotomy. J Bone Joint Surg Br 93(1):34–38
Hasegawa Y, Iwase T, Kanoh T, Seki T, Matsuoka A (2012) Total hip arthroplasty for Crowe type IV developmental dysplasia. J Arthroplasty 27(9):1629–1635
D’Lima DD, Oishi CS, Petersilge WJ, Colwell CW Jr, Walker RH (1998) 100 cemented versus 100 noncemented stems with comparison of 25 matched pairs. Clin Orthop Relat Res 348:140–148
Luo X, He S, Li Z, Huang D (2012) Systematic review of cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures in older patients. Arch Orthop Trauma Surg 132:455–463
Acknowledgements
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Inoue, D., Kabata, T., Kajino, Y. et al. Comparison of mid-term clinical results between cementless and cemented femoral stems in total hip arthroplasty with femoral shortening osteotomy for Crowe type IV hips. Arch Orthop Trauma Surg 141, 1057–1064 (2021). https://doi.org/10.1007/s00402-020-03749-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03749-0