Abstract
Introduction
The recent focus on early surgery for hip fractures to reduce complications and improve morbidity, has led some resource-constrained institutions to perform after hours surgery in a bid to meet these timelines. However, there are concerns about the potential increase in complications and poorer outcomes in after hours surgery. This study aims to evaluate the safety of after hours hip fracture surgery and its related complications.
Materials and methods
This is a retrospective review of hip fracture patients admitted over a 2-year period to a tertiary centre with an established orthogeriatric co-managed hip fracture care pathway. Patients were divided into two groups based on their operating start time: (1) office hours surgery was defined as surgery conducted between 8 am to 5 pm on weekdays and 8 am to 12 noon on Saturdays; and (2) after hours surgery was defined as surgery conducted between 5 pm to 8 am on weekdays, and between Saturday 12 noon to Monday 8 am, as well as those that were conducted on public holidays. Demographic data, comorbidities, fracture details, operative details and outcome measures (complications, mortality and functional scores) were collated.
Results
A total of 903 patients were surgically treated for per- and intertrochanteric or femoral neck fractures. 76.7% (n = 693) of the patients underwent operation during office hours while 23.3% (n = 210) of the patients underwent after hours operation. 12.4% (n = 26) of the after hours group underwent surgery within 24 h of admission, compared with 6.8% (n = 47) in the office hours group (p = 0.009). We did not find any significant difference between the two groups in terms of complications, mortality and functional outcomes (p > 0.05).
Conclusion
In conclusion, our study did not show that after hours surgery increases complication rates in hip fracture surgery and had equivalent functional outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As the world population ages, the rising number of hip fracture patients places a toll on both the healthcare and socioeconomic systems.
It is postulated that by 2050, the incidence of hip fracture worldwide is projected to rise to between 7.3 and 21.3 million [1]. Based on 1997 currency values and the projected incidence, analysts estimated that medical cost could translate to between US $153.5 billion and US $446.3 billion annually by 2050 [2].
There is an urgency to operate on these patients and the reasons are multi-fold. Zuckerman et al. reported doubling of the 1 year mortality rate for patients delaying operation for more than 2 days [3]. Many guidelines recommend early operation to reduce complications and improve mobility [4]. There is also a push by institutions and policymakers to discharge patients due to high hospital bed occupancy rates.
To reduce the time to surgery and hence length of stay, many institutions are setting aside specific trauma operating theatres or operating after hours to ensure hip fracture operations are performed expeditiously.
However, there are concerns about the theoretical increase in operative risk at night due to surgeon fatigue, reduction in nursing staff or decreased familiarity of the surgery among operating staff.
Sugden et al. reported sleep deprivation and fatigue can substantially impair neurocognitive function that lead to the risk of committing serious medical errors [5]. The detrimental effect of wakefulness of more than 24 h impairs cognitive performance equivalent to blood alcohol level of 10% [6, 7].
In a prospective comparative study by Ricci et al. published in 2009, there was an increased frequency for removal of painful hardware in patients undergoing femoral nailing at night, which may be related to technical error [8].
The potential increase in complications and poorer outcomes for operations performed after hours led us to evaluate the safety of this practice. We hypothesise that after hours operation for elderly hip fractures is associated with increased perioperative complications, increased mortality rate and poorer functional outcomes.
Materials and methodology
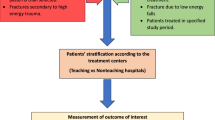
This is a retrospective review of prospectively collected data from a hip fracture registry of patients admitted to a tertiary centre from October 2011 to October 2013. The centre has an established orthogeriatric co-managed hip fracture care pathway.
All patients aged 60 years and older with hip fractures (intertrochanteric or femoral neck fracture) who underwent surgical intervention were included in the study. Polytrauma, open fractures, pathological fractures or revision surgeries were excluded.
Patients were divided into two groups based on their operating start time: (1) office hours surgery was defined as surgery conducted between 8 am to 5 pm on weekdays and 8 am to 12 noon on Saturdays; and (2) after hours surgery was defined as surgery conducted between 5 pm to 8 am on weekdays, and between Saturday 12 noon to Monday 8 am, as well as those that were conducted on public holidays. This differentiation is based on a 5.5-day work week in our institution.
Intertrochanteric hip fractures were treated with proximal femoral nailing, extramedullary fixation or total hip replacement. Femoral neck fractures were treated with fixation, bipolar hemiarthroplasty or total hip replacement.
Demographic data (age, ethnicity, gender), comorbidities (diabetes mellitus, end stage renal failure, ischemic heart disease (IHD), stroke, dementia), and fracture details (type, laterality, type of intervention) were collected. The outcome measures recorded were: (1) Pre-operative (time to surgery); (2) intra-operative (surgical time and intra-operative complications); (3) Post-operative (blood transfusion, weight-bearing status, length of stay, inpatient complications and inpatient mortality); (4) long term outcomes (1 year complications and mortality); and (5) functional outcomes (Modified Barthel Index (MBI) scores pre-fall, at 6 months and 12 months post-op).
MBI is a functional scoring system to assess physical disability based on behaviours relating to activities of daily living. A patient with a higher score has a better functional status.
Length of stay is defined from the time of admission to discharge from hospital either to a step-down care facility or home.
Statistical analysis was performed with SPSS version 19.0 (IBM Corp. Armonk, NY). Categorical variables were presented as numbers and percentages. Values of continuous variables were presented as mean ± standard deviation (SD) or as median with inter-quartile range (IQR). Shapiro–Wilk W test was used to determine data normality. Chi-square test or Fisher’s exact test was used as appropriate to compare categorical variables. Student’s t test or Wilcoxon test was used as appropriate to compare continuous variables in two groups. One way ANOVA or Kruskal–Wallis test was used to compare continuous variables in more than two groups. A two-tailed p value of less than 0.05 was considered significant for all tests.
Results
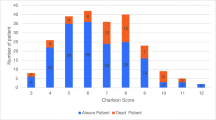
A total of 903 patients were surgically treated for intertrochanteric or femoral neck fractures. 73.0% (n = 659) were female patients and 27.0% (n = 244) were male patients with the mean age of 80.8.
76.7% (n = 693) of the patients underwent operation during office hours while 23.3% (n = 210) of the patients underwent after hours operation. 44.4% (n = 401) of the patients were treated for intertrochanteric fracture and 55.6% (n = 502) of the patients were treated for femoral neck fracture.
Amongst the patients who sustained intertrochanteric fractures, 69.5% (n = 279) underwent intramedullary nail fixation, 29.9% (n = 120) underwent extramedullary fixation, and 0.6% (n = 2) underwent total hip arthroplasty. Amongst the patients who sustained neck of femur fractures, 28.8% (n = 145) underwent cemented bipolar hemiarthroplasty, 56.1% (n = 282) underwent uncemented bipolar hemiarthroplasty, 8.1% (n = 41) underwent surgical fixation procedure, and 6.7% (n = 34) underwent total hip arthroplasty.
Table 1 shows the baseline characteristics of patients in the office hours and after hours groups. There was no significant difference in patient mean age, gender profile, ethnicity as well as fracture laterality. We did not find any significant difference in the fracture type and the surgical procedure performed between the two groups (p > 0.05).
16.2% (n = 112) of patients who underwent office hours operation had underlying ischemic heart disease compared with 10.5% (n = 22) of patients who underwent after hours operation (p = 0.042).
There was no statistically significant difference for the other premorbid medical conditions (diabetics mellitus, end-stage renal disease, stroke disease or dementia) between the two groups (p > 0.05).
The median time to surgery for office hours group was 69.7 h (IQR = 70.3 h) and median time to surgery for after hours group was 63.8 h (IQR = 60.4 h). The difference was not found to be statistically significant (p > 0.05) (Table 2).
However, we found that 12.4% (n = 26) of the after hours group underwent surgery within 24 h of admission, compared with 6.8% (n = 47) in the office hours group (p = 0.009 and CI 0.750–0.807). There was no difference when we compared surgery performed within 48 h (p > 0.05).
The median length of stay was 10.0 days (IQR = 7 days) for the office hours group and 9.3 days (IQR = 6 days) for the after hours group (p > 0.05).
We did not find any significant difference between the office hours and after hours groups in terms of intra-operative complications, blood transfusion, urinary tract infection, wound infection, acute myocardial infarction, venous thrombosis, pulmonary embolism and dislocation. There was also no significant difference for inpatient death and 1-year mortality (p > 0.05).
Pre-operative Modified Barthel Index (MBI) between the two groups were similar with mean of 91.3 for the office hours group and 90.3 for the after hours group (p > 0.05). Mean MBI score for the office hours group at 6 months and 12 months post-operation were 80.6 and 83.3 respectively. Mean MBI score for the after hours group at 6 months and 12 months post-operation were 78.7 and 82.1, respectively. These findings did not reach statistical significance (p > 0.05).
Discussion
Surgery performed after hours has been a safety concern to many surgical disciplines. Many believe that operations carried out at night result in higher peri-operative mortality and complication rates. In hip fracture surgeries, this fear is compounded by the fact that the profile of hip fracture patients is older with multiple comorbidities.
The reduction in surgical and support staff and cross covering of non-Orthopaedic-trained nursing staff during after hours operation potentially increases the occurrence of an adverse outcome.
Foss et al. reported an increase in 5-day and 30-day mortality in hip fracture patients admitted during holidays due to a reduction in staff numbers [9]. Although the staff applied standardised care according to pathway protocol, the quality of practical application of care and early recognition of complications may be compromised. The reduction in staff number was similarly experienced in the operating theatre and may have resulted in poorer surgical outcomes for hip fracture operations.
The adverse effect of performing surgery after hours has also been echoed in other high-risk operations. Kenan et al. reported increased mortality and wound infection in after hours cardiac operations [10]. Komen et al. reported after hours colorectal operation being an independent risk factor for anastomotic leakage [11].
The effect of late night operation is further magnified in our local context where surgeons perform night calls compared to shift work in some other countries. Our surgeons perform day duties and continue throughout the night. This may result in higher unexpected errors and complications.
With all these in mind, our study failed to prove the hypothesis that after hours operation leads to a significant increase in adverse outcomes. Their functional outcome scores were also comparable to patients with office hours surgery.
The push for earlier hip fracture surgeries resulted in a higher rate of after hours operations. However, the earlier time to operation did not translate into shorter length of stay. The median length of stay for patients who underwent after hours surgery was 9.3 days compared to 10.0 days for office hours operation.
When we analysed this further, the office hours group had a median time to surgery of 69.0 h compared to 63.9 h in the after hours group. The time difference is 5.1 h. Hence this difference in hours between the two groups is unlikely to make any significant difference to the eventual length of stay.
Rizwan et al. similarly reported that after hours hip fracture operations showed no difference in post-operative complication and mortality [12]. Likewise, they also showed that there was a trend towards reduction in length of stay for after hours operation (7.7 ± 2.4 days) compared with office hours operation (10 ± 8.9 days) but the results were not statistically significant. However, the study population was relatively younger compared to our study population, with a mean age of 68 years for both groups.
In another study, Leontien et al. evaluated the effect of weekend admissions on hip fracture operations [13]. Similarly, after hours operation is not associated with increased 30-day mortality or 1-year mortality. In this study, there was no comparison between the medical conditions. Instead, ASA (American Society of Anaesthesiologist) score was used as a surrogate in their study.
The strengths of our study include having a large pool of patients in a single tertiary centre managed by an established orthogeriatric co-managed hip fracture care pathway. In addition, functional outcomes were measured in our study utilising the Modified Barthel Index scoring at multiple phases up to 1 year of follow-up.
There are several limitations in this study. Firstly, this is a retrospective study with the inherent risk of selection bias. There was no randomisation performed to allocate the patients into different groups. The decision to operate on patients after hours was based on either the decision from the clinician, anaesthetist or availability of operating theatre. Surgeons may elect to perform office hours operations in patients with ischemic heart disease due to better medical support during office hours.
Conclusion
In conclusion, our study did not show that after hours surgery increases complication rates in elderly hip fracture patients and functional outcomes were comparable to office hours surgery. After hours surgery allows patients to receive their surgeries earlier within 24 h and although not statistically significant, the total length of stay was shorter.
References
Gullberg B, Johnell O, Kanis JA (1997) World-wide projections for hip fracture. Osteoporos Int 7(5):407–413
Johnell O (1997) The socioeconomic burden of fractures: today and in the 21st century. Am J Med 103(2A):20S–S25. https://doi.org/10.1016/s0002-9343(97)90023-1(Discussion 25S-6S)
Zuckerman JD, Skovron ML, Koval KJ, Aharonoff G, Frankel VH (1995) Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Joint Surg Am 77(10):1551–1556. https://doi.org/10.2106/00004623-199510000-00010
Rogers FB, Shackford SR, Keller MS (1995) Early fixation reduces morbidity and mortality in elderly patients with hip fractures from low-impact falls. J Trauma 39(2):261–265
Sugden C, Athanasiou T, Darzi A (2012) What are the effects of sleep deprivation and fatigue in surgical practice? Semin Thorac Cardiovasc Surg 24(3):166–175. https://doi.org/10.1053/j.semtcvs.2012.06.005
Gaba DM, Howard SK (2002) Fatigue among clinicians and the safety of patients. N Engl J Med 347(16):1249–1255. https://doi.org/10.1056/NEJMsa020846
Taffinder NJ, McManus IC, Gul Y, Russell RC, Darzi A (1998) Effect of sleep deprivation on surgeons’ dexterity on laparoscopy simulator. Lancet 352(9135):1191. https://doi.org/10.1016/s0140-6736(98)00034-8
Ricci WM, Gallagher B, Brandt A, Schwappach J, Tucker M, Leighton R (2009) Is after-hours orthopaedic surgery associated with adverse outcomes? A prospective comparative study. J Bone Joint Surg Am 91(9):2067–2072. https://doi.org/10.2106/JBJS.H.00661
Foss NB, Kehlet H (2006) Short-term mortality in hip fracture patients admitted during weekends and holidays. Br J Anaesth 96(4):450–454. https://doi.org/10.1093/bja/ael012
Yount KW, Lau CL, Yarboro LT et al (2015) Late operating room start times impact mortality and cost for nonemergent cardiac surgery. Ann Thorac Surg 100(5):1653–1659. https://doi.org/10.1016/j.athoracsur.2015.04.131
Komen N, Dijk J-W, Lalmahomed Z et al (2009) After-hours colorectal surgery: a risk factor for anastomotic leakage. Int J Colorectal Dis 24(7):789–795. https://doi.org/10.1007/s00384-009-0692-4
Rashid RH, Zubairi AJ, Slote MU, Noordin S (2013) Hip fracture surgery: does time of the day matter? A case-controlled study. Int J Surg 11(9):923–925. https://doi.org/10.1016/j.ijsu.2013.07.003
Nijland LMG, Karres J, Simons AE, Ultee JM, Kerkhoffs GMMJ, Vrouenraets BC (2017) The weekend effect for hip fracture surgery. Injury 48(7):1536–1541. https://doi.org/10.1016/j.injury.2017.05.017
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article was performed with Institutional Review Board (IRB) approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yeo, Q.Y., Kwek, E.B.K. After hours surgery for elderly hip fracture patients: How safe is it?. Arch Orthop Trauma Surg 141, 1183–1187 (2021). https://doi.org/10.1007/s00402-020-03585-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03585-2