Abstract
Introduction
Post-radiation fractures of the femur (PRF) are difficult to treat and are associated with a high risk of delayed union and non-union. We report a series of patients affected by soft tissue sarcoma (STS) of the thigh, treated with limb-sparing surgery and perioperative radiotherapy (RT), to analyse post-radiotherapy femur fracture (FF) rate and its management.
Material and methods
547 patients treated with surgery and RT for a deep primary STS of the thigh were included. “Periosteal stripping” and “bone tangential resection” were performed in case of tumor invasion. In the case of complete bone involvement, the patient received its complete resection and econstruction.
Results
Twenty-three (4.3%) patients underwent surgical procedures involving periosteum and cortical bone. In 11 (2.0%) patients a bone resection was required because of massive bone involvement. Six out of these 11 (54.5%) patients developed major complications (infection and aseptic loosening). At the time of STS excision, 11 patients (2.0%) underwent prophylactic intramedullary nailing (PIN). PRF occurred in 15 patients (3.0%) at a median follow up of 52 months (range 3–151). Among patients who developed PRF, three were treated with a prosthesis (no complications) and eight nailing (7/8, 87.5% did not heal and developed a non-union).
Conclusions
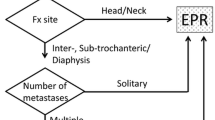
Given the potentially devastating complication of a PRF, PIN should be considered. We suggest prophylactic IM nail in patients at higher risk the time of STS excision. In other cases, IM nail can be postponed in the following years considering the prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The combination of radiation therapy (RT) and limb-salvage surgery is effective for decreasing the rate of local recurrence in soft tissue sarcomas (STS) [1,2,3]. However, several deleterious consequences have been described including post-radiation fractures (PRF) [4], which is particularly evident in the femur (rates from 1.2 to 22%) [5,6,7]. Despite awareness of radiation bone toxicity, it is less clear whether radiation dose, timing of radiation (preoperative versus postoperative), and the circumference of the femur involved in the radiation field are risk factors for the development of a femur fracture [4, 6]. Other risk factors such as age and chemotherapy have been identified; however, there is no uniform consensus on that [5, 8, 9].
Fractures that occur following radiation therapy are difficult to treat and are associated with a high risk of delayed union and non-union despite aggressive therapy [4, 9, 10]. Most patients require multiple surgeries to fix these fractures, consequently increasing their risk of a deep infection. If non-union persists, total endoprosthetic replacement or amputation may be eventually required [4, 11].
To prevent PRF, prophylactic intramedullary nailing (PIN) has been suggested as an attractive preventive measure [4, 9, 11]
We report a mono Institutional series of patients treated for STS of the thigh with limb-sparing surgery and perioperative RT. We specifically analyse the cumulative risk of PRF and the outcome of patients who developed a PRF; we also provide a review of the literature on this topic.
Materials and methods
A total of 547 patients who were treated between 2000 and 2017 for a deep primary STS of the thigh using limb-sparing surgery and RT were included.
Tumor size was assessed on surgical specimens using the larger diameter as a reference according to preoperative imaging (computerized tomography CT-scan or magnetic resonance imaging -MRI). The site of the STS was classified as proximal, diaphysis or distal with respect to the region of the femur.
On antero-posterior pre-operative radiographs, cortical-shaft index was evaluated according to Barnett and Nordin [12]. “Periosteal stripping” and “bone tangential resection” were performed in case of tumor invasion. In the case of bone tangential resection, cortical-shaft index was evaluated on post-operative radiographs. Overall, 493 patients had radiographs available for analysis.
Prophylactic intramedullary nail was performed using a long Gamma nail (Stryker, Mahwah, NJ) The nail is available in 240 mm up to 480 mm lengths, with 20 mm increments. Reaming was performed in 0.5 mm steps, up to 2 mm larger than the nail distally. Distal static locking was performed [13, 14]
In the case of complete bone involvement by the tumour, the patient received its complete resection and reconstruction.
All patients received RT according to STS guidelines [15]. The use of chemotherapy (ChT) was decided at the discretion of a multidisciplinary team.
PRF was defined as a fracture occurring in the previous radiation field and associated with minimal energy trauma.
Patients’ characteristics are presented by frequencies and percentages for categorical variables, mean and range for continuous variables.
The Kaplan–Meier method was used to estimate PRF.
PRF interval was defined as the time between the date of surgery and the date of the femur fracture or last follow-up, whichever came first.
Differences in survival rates were assessed by the log-rank test.
All analysis was completed using the Statistical Package for Social Science (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.).
Results
Mean age at the time of diagnosis was 54.8 years (range 18–92). 241 (44.5%) patients were female and 306 (55.5%) were male. Fifty-five (10.2%) STS were localized in the proximal region, 406 (75.0%) involved the diaphyseal region and 86 (15.8%) the distal region. Histological diagnosis was heterogeneous: most represented histotypes were liposarcoma (n = 186), undifferentiated pleomorphic sarcoma (n = 72), myxofibrosarcoma (n = 66), synovial sarcoma (n = 56) and leiomiosarcoma (n = 40). Twenty-four (4.4%) tumours were < 5 cm, 203 (36.9%) between 5 and 10 cm, 264 (48.2%) between 10 and 20 cm and 56 (10.5%) > 20 cm.
Mean cortical-shaft index was 58 (range 29–74).
Eighty-five (15.7%) patients had metastasis at the time of the diagnosis.
Chemotherapy was administered to 272 (50.3%) patients.
All patients received RT: 153 (27.5%) had exclusively pre-operatory EBRT, 359 (66.0%) post-operatory radiotherapy alone and 35 (6.5%) both pre plus post-operatory EBRT.
Twenty-three (4,3%) patients underwent surgical procedures involving periosteum and cortical bone: 16 periosteal stripping and seven a tangential femur resection. Periosteal procedures were mostly performed in tumours larger than 10 cm (p = 0.019).
In 11 patients a bone resection was required because of massive bone involvement. Reconstructions included megaprosthesis in seven patients, total hip arthroplasty in one patient, diaphyseal prosthesis in one patient, one saddle prosthesis and one intercalary graft reconstruction. Six out of these 11 (54.5%) patients developed major complications. Two patients with distal femur megaprosthesis suffered from an infection; they were treated with a staged revision and healed. An infection was observed also in the patients with a THA who finally was amputated. The patient with the intercalary reconstruction suffered of an infection, which required hardware removal. Another patient with diaphyseal prosthesis had an aseptic loosening and was then converted into a distal femur megaprosthesis.
At the time of STS excision, 11 patients (2.0%) underwent PIN. Most of these patients (eight) had associated periosteal procedures (p < 0.001). Despite the nail, one of these developed a fracture with breakage of the nail 37 months after surgery.
Excluding 22 patients with PIN and bone resection, PRF occurred in 15 patients (3.0%) at a median follow up of 52 months (range 3–151). Femur fracture estimated rate was 1.9% at 5 years, 3.5% at 10 years and 12.3% at 15 years (Fig. 1).
An increased risk of PRF was observed in female (p = 0.007) (Fig. 2). No significance was observed among the size of the tumour, the timing of RT and age. A higher incidence of PRF was observed among patients who had procedures on periosteum during the 1st years after surgery (p < 0.001) (Fig. 3).
No differences were observed regarding pre-operative cortical-shaft index among patients who suffered PRF and those who did not (mean 56 and 59, respectively, p = 0.876)
Among patients who developed PRFs four refused (Table 1) surgery. Three patients were treated with a prosthesis. None of these developed major complications. Eight patients underwent intramedullary nailing. Seven out of 8 (87.5%) patients treated with a nail did not heal and developed a non-union. Five of these required a megaprosthesis.
Discussion
Post radiation fractures are rare but serious complications of combined modality treatment of STS. Current data addressing the occurrence and risk of PRF is sparse, likely due to the difficulty in standardizing a treatment group [16]. Previous studies have reported very heterogeneous fracture rates (from 1.2 to 22%) [5,6,7]. We found a very low PRF rate up to 10 years (3.5%), which raises up to 12.3% at 15 years follow up (Table 2) Several risk factors for PRF have been described in the previous series [4,5,6, 8, 9, 17, 18]. In this study, we found that women had a significant increase risk of PRF. Patients who underwent periosteal stripping had an increased risk of PRF only during the 1st years after surgery. However, neither the age of the patient nor the timing of RT (pre or post surgery) were found to affect fracture risk.
Treatment of post-radiation fractures is typically more complicated than that of post-traumatic fractures because radiation-induced damage to the vasculature and osteoblast cells impairs bone union. We found no differences in the cortical-shaft index in patients who suffered PRF.
Photon radiation produce grater damage to trabecular network than to cortical bone [19] and minimal changes in bone composition (tissue mineral density, mineral/matrix ratio) [20]. Even though mice models may vary severely compared to humans, these data suggest that we are still lacking a radiological tool to assess PRF.
The non-union rate is high (generally > 50%) in all previous series [11, 21], and healing times are often quite long for fractures that eventually unite. In addition, multiple procedures are often required, including supplemental bone grafting, vascularized fibula grafting, exchange nailing, and potential resection of the fracture site and conversion to a large oncologic endoprosthesis [4, 6, 9, 11, 22].
In our series, the majority of patients (87.5%) treated with intramedullary nailing for PRF developed a pseudoarthrosis, thus requiring additional procedures. Eventually, most of them (five out of eight) required a megaprosthesis.
On the other hand, none of the three patients treated with a prosthesis for PRF developed any complication.
Differently, most of the prosthesis performed at the same stage of STS excision developed major complications, thus resulting in amputation in some of them. Additional bone resection is very rarely required as only a few sarcomas are able to penetrate cortical bone. A careful evaluation should be done to limit the need for a bone resection.
Because of the difficulties in the management of the fracture once it has occurred, fracture prevention is the most important intervention [10]. Prophylactic femoral intramedullary nail (PIN) was suggested in higher-risk patients. With this policy, the femoral fracture rates of Pak et al. [7] was lower than fracture rates for similar patients who had periosteal excision and RT in other series [4, 9]. However, it has been suggested that PIN should not be contemplated on a regular basis because the fracture risk is low [4, 9] Moreover, due to the heterogeneity of risk factors, it is very hard to select those patients who may benefit from PIN. In the present series, PIN was performed in 11 patients, approximately 50% of those who received any periosteal procedure.
Prophylactic stabilization does not entirely preclude subsequent fracture of the femur, because one out of 11 patients developed a fracture with breakage of the nail.
Also, the timing to perform PIN is debated. Gortzak et al. [8] found that approximately 30% of fractures occurred within 2 years after surgery. Nonetheless, in the present series most of PRF occurred after more than 5 years from STS excision. Based on our results, we believe that in most of the patients a PIN may be reserved to medium- to long-term survivors, either at index surgery or even delayed [23]
One of the limitations of this study is the lack of precise data about RT doses. The dose of radiation may influence the rate of femoral fracture, with 9% rate being reported for lower extremity STS treated to > 60 Gy compared to 1% for those treated to 50 Gy. However, all patients were treated for a STS of the extremities, thus receiving a similar dose of RT (approximately 55–60 Gy). Additionally, there was perhaps a selection bias in the way patients with fractures were identified, as in this series fracture was identified through retrospective chart review. Moreover, 54 patients did not have pre-operative radiographs to assess cortical-shaft index. In addition, data regarding the localisation of the tumour were not available. According to the literature, within the thigh, there is a higher rate of fracture in anterior compartment tumors compared to medial or posterior compartments [18]. This might have partially affected our findings. However, this is one of the series with a longest follow up and, because fractures may occur many years after the completion of therapy, follow up is important.
Conclusions
It is still impossible to predict when prophylactic intramedullary nailing should be performed. A case-by-case decision should be taken. We suggest PIN in patients at higher risk (women with associated periosteal procedures) at the time of STS excision. In other cases, PIN can be postponed in the following years considering the prognosis. The goal is to prevent the fracture. Therefore, patients with no prophylactic osteosynthesis should be followed more carefully even after oncologic follow up is over (> 10 years) to detect early any sign of femur fracture.
In case of late PRF, bone resection and reconstruction is recommended. Fewer complications are expected than after osteosynthesis in irradiated bone.
References
O'Sullivan B, Davis AM, Turcotte R, Bell R, Catton C, Chabot P, Wunder J, Kandel R, Goddard K, Sadura A, Pater J, Zee B (2002) Preoperative versus postoperative radiotherapy in soft-tissue sarcoma of the limbs: a randomised trial. Lancet 359(9325):2235–2241
Alektiar KM, Brennan MF, Healey JH, Singer S (2008) Impact of intensity-modulated radiation therapy on local control in primary soft-tissue sarcoma of the extremity. J Clin Oncol 26(20):3440–3444
Wilson AN, Davis A, Bell RS, O'Sullivan B, Catton C, Madadi F, Kandel R, Fornasier VL (1994) Local control of soft tissue sarcoma of the extremity: the experience of a multidisciplinary sarcoma group with definitive surgery and radiotherapy. Eur J Cancer 30(6):746–751
Lin PP, Schupak KD, Boland PJ, Brennan MF, Healey JH (1998) Pathologic femoral fracture after periosteal excision and radiation for the treatment of soft tissue sarcoma. Cancer 82(12):2356–2365
Blaes AH, Lindgren B, Mulrooney DA, Willson L, Cho LC (2010) Pathologic femur fractures after limb-sparing treatment of soft-tissue sarcomas. J Cancer Surviv 4(4):399–404
Holt GE, Griffin AM, Pintilie M, Wunder JS, Catton C, O'Sullivan B, Bell RS (2005) Fractures following radiotherapy and limb-salvage surgery for lower extremity soft-tissue sarcomas. A comparison of high-dose and low-dose radiotherapy. J Bone Joint Surg Am 87(2):315–319
Pak D, Vineberg KA, Griffith KA, Sabolch A, Chugh R, Ben-Josef E, Biermann JS, Feng M (2012) Dose–effect relationships for femoral fractures after multimodality limb-sparing therapy of soft-tissue sarcomas of the proximal lower extremity. Int J Radiat Oncol Biol Phys 83(4):1257–1263
Gortzak Y, Lockwood GA, Mahendra A, Wang Y, Chung PW, Catton CN, O'Sullivan B, Deheshi BM, Wunder JS, Ferguson PC (2010) Prediction of pathologic fracture risk of the femur after combined modality treatment of soft tissue sarcoma of the thigh. Cancer 116(6):1553–1559
Helmstedter CS, Goebel M, Zlotecki R, Scarborough MT (2001) Pathologic fractures after surgery and radiation for soft tissue tumors. Clin Orthop Relat Res 389:165–172
Duffy GP, Wood MB, Rock MG, Sim FH (2000) Vascularized free fibular transfer combined with autografting for the management of fracture nonunions associated with radiation therapy. J Bone Joint Surg Am 82(4):544–554
Lin PP, Boland PJ, Healey JH (1998) Treatment of femoral fractures after irradiation. Clin Orthop Relat Res 352:168–178
Barnett E, Nordin BE (1960) The radiological diagnosis of osteoporosis: a new approach. Clin Radiol 11:166–174
Edwards SA, Pandit HG, Clarke HJ (2000) The long gamma nail: a DGH experience. Injury 31(9):701–709
Edwards SA, Pandit HG, Clarke HJ (2001) The treatment of impending and existing pathological femoral fractures using the long gamma nail. Injury 32(4):299–306
Casali PG, Abecassis N, Bauer S, Biagini R, Bielack S, Bonvalot S, Boukovinas I, Bovee J, Brodowicz T, Broto JM, Buonadonna A, De Alava E, Dei Tos AP, Del Muro XG, Dileo P, Eriksson M, Fedenko A, Ferraresi V, Ferrari A, Ferrari S, Frezza AM, Gasperoni S, Gelderblom H, Gil T, Grignani G, Gronchi A, Hannu A, Hassan B, Hohenberger P, Issels R, Joensuu H, Jones RL, Judson I, Jutte P, Kaal S, Kasper B, Kopeckova K, Krakorova DA, Le Cesne A, Lugowska I, Merimsky O, Montemurro M, Pantaleo MA, Piana R, Picci P, Piperno-Neumann S, Pousa AL, Reichardt P, Robinson MH, Rutkovski P, Safwat AA, Schoffski P, Sleijfer S, Stacchiotti S, Sundby Hall K, Unk M, Van Coevorden F, Van der Graaf W, Whelan J, Wardelmann E, Zaikova O, Blay JY (2018) Soft tissue and visceral sarcomas: ESMO-EURACAN clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 2:67
Pacheco R, Stock H (2013) Effects of radiation on bone. Curr Osteoporos Rep 11(4):299–304
Davis AM, O'Sullivan B, Turcotte R, Bell R, Catton C, Chabot P, Wunder J, Hammond A, Benk V, Kandel R, Goddard K, Freeman C, Sadura A, Zee B, Day A, Tu D, Pater J (2005) Late radiation morbidity following randomization to preoperative versus postoperative radiotherapy in extremity soft tissue sarcoma. Radiother Oncol 75(1):48–53
Folkert MR, Casey DL, Berry SL, Crago A, Fabbri N, Singer S, Alektiar KM (2019) Femoral fracture in primary soft-tissue sarcoma of the thigh and groin treated with intensity-modulated radiation therapy: observed versus expected risk. Ann Surg Oncol. 26(5):1326–1331
Bandstra ER, Pecaut MJ, Anderson ER, Willey JS, De Carlo F, Stock SR, Gridley DS, Nelson GA, Levine HG, Bateman TA (2008) Long-term dose response of trabecular bone in mice to proton radiation. Radiat Res 169(6):607–614
Bartlow CM, Mann KA, Damron TA, Oest ME (2018) Limited field radiation therapy results in decreased bone fracture toughness in a murine model. PLoS ONE 13(10):e0204928
Green N, French S, Rodriquez G, Hays M, Fingerhut A (1969) Radiation-induced delayed union of fractures. Radiology 93(3):635–641
Cannon CP, Ballo MT, Zagars GK, Mirza AN, Lin PP, Lewis VO, Yasko AW, Benjamin RS, Pisters PW (2006) Complications of combined modality treatment of primary lower extremity soft-tissue sarcomas. Cancer 107(10):2455–2461
Brennan MF, Antonescu CR, Moraco N, Singer S (2014) Lessons learned from the study of 10,000 patients with soft tissue sarcoma. Ann Surg. 260(3):416–421
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflicts of interest to disclose and approved the manuscript and this submission.
Ethical approval
Not required for retrospective studies.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sambri, A., Gardini, L., Dalla Rosa, M. et al. Femoral fracture in primary soft-tissue sarcoma of the thigh treated with radiation therapy: indications for prophylactic intramedullary nail. Arch Orthop Trauma Surg 141, 1277–1282 (2021). https://doi.org/10.1007/s00402-020-03544-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03544-x