Abstract
Introduction
Trabecular metal cones are a relatively new option for reconstruction of major bone defects during revision total knee arthroplasty (TKA). The purpose of the present study was to retrospectively assess medium-term results for tibial cones in revision TKA with a severe proximal tibial bone defect. We hypothesized that revision TKA patients with bone defects treated with trabecular metal cones have excellent medium-term clinical and radiological results.
Patients and methods
A single-center retrospective review included all consecutive cases of tibial revision using trabecular metal cones. All patients with a minimum 2-year follow-up were included in the study. There were no exclusion criteria. The primary endpoint was tibial cone survivorship. The secondary endpoints were revision TKA all-cause survivorship, patient-reported outcome measures with a Knee injury and Osteoarthritis Outcome Score (KOOS), SF 12, and radiographic analysis.
Results
Five of the 57 patients alive at last follow-up (8.77%) had undergone revision (4 for infection and 1 for instability). Complications comprised four cases (7.02%) of infection, 2 cases (3.51%) of tibial and femoral implant aseptic loosening that did not require revision surgery, 1 of which (1.75%) with associated patellar loosening, and 1 case (1.75%) of instability. Kaplan–Meier estimates showed 100% 5-year survivorship with tibial cone revision for aseptic loosening and 93.44% (95% CI 83.47–97.49%) for all-cause revision.
Discussion
The present study of cones used for tibial revision supports shows excellent results; however, longer and larger follow-up is needed to better assess results in revision TKA.
Level of evidence
4, retrospective study
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Revision total knee arthroplasty (TKA) is the primary treatment for failed primary TKA. The anticipated volume and cost of revision TKA are forecasted to significantly increase in the near future [1]. Results after revision TKA are less predictable than after primary surgery [2]. Assessment and management of bone defects in revision TKA is a challenging problem [3]. Depending on defect severity, improved distal fixation may be needed. Many treatment options are available, without any evidence of superiority [4]. Trabecular metal (TM) cones are a relatively new option for reconstruction of major bone defects during revision TKA and have recently been studied, showing good primary fixation in cadaver [5] and biomechanical models [6]. TM is well described for femoral cones and tibial sleeves [7]. The purpose of a tibial cone is to enable metaphyseal fixation secondary to the high porosity and low elasticity modulus of TM [8, 9]. Some authors have reported good preliminary results with femoral cones, but further study is needed [8, 10, 11]. Medium-term results on the tibial side have not yet been studied.
Sandiford et al. compared femoral head allograft and tibial cones in revision TKA and did not find any difference [12], but there were only 15 patients in the cone group. Bohl et al. reported that metaphyseal cones were not associated with better short-term results [13]. Few studies have assessed medium-term results for tibial cones in revision TKA [14,15,16]. Longer follow-up studies are necessary to determine whether outcomes and survivorship differ over time. The purpose of the present study was to retrospectively assess medium-term results for trabecular metal tibial cones in revision TKA. We hypothesized that revision TKA patients with bone defect treated with trabecular metal tibial cones have excellent medium-term clinical and radiological results.
Material and methods
A single-center retrospective review included all consecutive cases of tibial revision using trabecular metal cones. Since early 2010, all revision TKA procedures with tibial bone defects used porous metal cones. The study protocol was reviewed and accepted by our institutional review board.
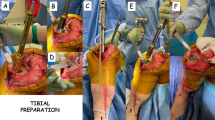
The inclusion criteria were: patients undergoing revision TKA with a revision of the tibial component. Tibial metaphyseal cones were used in all cases. The metaphyseal tibial cone was made of highly porous tantalum biomaterial (Trabecular Metal, Zimmer®) Fig. 1. All patients with a minimum of 2 years follow-up were included. There were no exclusion criteria. Patients were seen for radiographic and clinical follow-up as necessary. All surgeries were performed by one of the authors (WP), a senior fellowship-trained arthroplasty surgeon, between January 1, 2010 and December 31, 2016.
Demographic data included age, gender, weight, height, body mass index, comorbidities, and perioperative variables (complications, operative time, implant records, etc.). Pre- and post-operative clinical scores included Knee injury and Osteoarthritis Outcome Scores (KOOS) and SF-12. Ambulation ability of all patients was evaluated with the Postel Merle d’Aubigné score. Devane activity level, Charnley class and range of motion were also recorded for all patients. Preoperative and postoperative X-rays were analyzed for cone integration, fracture, mechanical axis, and loosening. The primary endpoint was tibial cone survivorship. The secondary endpoints were revision TKA all-cause survivorship, patient-reported outcome measures with KOOS, SF-12, and radiographic analysis.
Reasons for revision TKA in our study comprised: second stage after infection (2 cases), aseptic loosening (55 cases), instability (3 cases) and rotational problem (1 case). There were no cases of implant failure or fracture as a cause for revision. All revision procedures for infection were performed in 2 stages. The first stage was implant removal with antibiotic spacer placement and the second stage was reimplantation with revision components and the tibial cone. Preoperative radiographic review and intraoperative assessment identified bone defect according to the AORI Anderson Bone Defect Classification [17]. Type 2B and 3 defects were identified intraoperatively [18]. Defect status comprised: no defect in 5 cases (8.20%), type 1 in 4 cases (6.56%), type 2A in 22 cases (36.07%), type 2B in 24 cases (39.34%) and type 3 in 6 cases (9.84%).
A medial parapatellar approach and tourniquet were used in all cases. Trial sizes for the appropriate tibial cone were used to press-fit the tibial cone into the final position. Any remaining voids around the implant were not grafted. All patients had hybrid fixation of the tibial components with cement only between the cone and the tibial component and press-fit stems. Concomitant femoral revision was performed in 31 patients (50.82%) and femoral cones were used in 5 cases (8.20%). One patient (1.64%) had no prior patellar component and primary patellar resurfacing was performed; 56 patients (91.80%) had a prior patellar component, which was left in place; 4 patients (6.56%) had a prior patellar component that was revised during surgery (1 for loosening, 3 for malposition). Posterior-stabilized components were used in 43 cases (70.49%), varus-valgus constrained components in 12 cases (19.67%) and hinged constructs in 6 cases (9.84%). The level of constraint was dictated by ligamentous and soft-tissue status. The minimal necessary level of constraint was utilized. Mean polyethylene thickness was 13.97 ± 3.44 mm (range, 10–26).
The immediate postoperative and all subsequent radiographs were analyzed by 2 observers for implant alignment, migration, osseointegration and any complications such as fracture or loosening. Full-length and standard knee radiographs were analyzed for radiolucency around the components, reconstruction of the joint line, HKA angle, alpha angle, tibial slope, joint-line height, patellar tilt and patellar lateral translation in sunrise view. Final follow-up radiographs were available and used for assessment of all patients. Criteria for radiological loosening of the tibial component were progressive lysis between bone, cone and implant.
Statistical analyses used Stata software, v12 (StataCorp, Texas, USA). Descriptive statistics were reported as numbers and percentage for categorical data and continuous data as mean ± standard deviation, or median and interquartile range in case of non-normal distribution checked graphically and on Shapiro–Wilk test. Continuous variables were compared before versus after surgery on paired Student’s t test (or Wilcoxon matched-pairs signed-rank test in case of non-normal distribution). Inter-rater concordance was analyzed on Pearson’s correlation coefficient (or Spearman’s in case of non-normal distribution) and Bland and Altman plot. Complications (all causes, infection, loosening and instability) were analyzed by survivorship, considering the complication as the event, and time from surgery to complication or censoring at last news (last consultation, or death without previous complication). Survival curves were plotted according to Kaplan–Meier. Results were reported as complication rates at different time-points, with 95% confidence intervals. We chose the 0.05 threshold statement for statistical significance.
Results
Clinical outcomes
Thirty-one of the 61 patients (50.82%) were female. Mean age at revision TKA was 60.35 ± 9.09 years (range, 34.71–80.66 years). Four patients (6.56%) died for reasons unrelated to the revision TKA, but had been followed up for at least 2 years and were, therefore, included in the study. Two patients (3.28%), who had undergone revision TKA at least 2 years previously, were not seen after their 6-month appointment and were thus lost to follow-up. The study flowchart is shown in Fig. 2.
Clinical examination at final follow-up found 1 patient (1.82%) who could not walk at all, 1 patient (1.82%) walking with 2 canes, 3 patients (5.45%) walking 1 cane, 5 patients (9.09%) walking with a cane only outside the home, 13 patients (23.64%) using a cane only for long distances, and 32 (58.18%) walking without any assistive device. Devane activity level was 1 for 2 patients (3.64%), 2 for 26 patients (47.27%), 3 for 18 patients (32.73%), 4 for 8 patients (14.55%), and 5 for 1 patient (1.82%). Charnley class was A for 9 patients (16.36%), B for 31 patients (56.36%) and C for 15 patients (27.27%). Mean KOOS improved from 56.32 ± 10.84 (range 36.93–65.99) preoperatively to 71.84 ± 22.56 (range 24.88–100) at final follow-up (p = 0.013). Mean Mental SF-12 score improved from 52.70 ± 8.93 (39.57–70.40) to 54.96 ± 6.80 (40.93–64.67) (p = 0.50), and mean Physical SF-12 score increased from 32.31 ± 11.66 (18.87–57.65) to 39.58 ± 11.94 (21.43–57.84) (p = 0.083). At final follow-up, mean flexion contracture was 0.33 ± 1.54° (− 5° hyperextension to 5° flexion contracture) and mean maximum flexion was 117.51 ± 10.92° (80–135°). These results are described in Table 1.
Radiographic results
Inter-observer reliability was good: correlation coefficient r = 0.93 (p < 0.001) for alpha angle, r = 0.98 (p < 0.001) for beta angle, r = 0.99 (p < 0.001) for HKA angle, r = 0.85 (p < 0001) for HKS angle, r = 0.98 (p < 0.001) for interline height, r = 0.98 (p < 0.001) for patellar translation, r = 0.98 (p < 0.001) for patellar tilt, and r = 0.99 (p < 0.001) for tibial slope.
Mean HKA angle improved from 172.66 ± 6.82° to 178.96 ± 2.85° (p < 0.001). Prior to surgery, 47 patients (77.05%) were outside the 180 ± 3° HKA range, with 45 patients below 177° and 2 patients above 183°. Post-operatively, only 12 patients (21.05%) were outside the 180 ± 3° HKA range, with 9 patients below 177° and 3 patients above 183°. Mean alpha angle changed from 95.50 ± 2.10° to 95.40 ± 1.47° (p = 0.72). Mean beta angle changed from 84.77 ± 5.15° to 89.58 ± 1.70° (p < 0.0001). Mean tibial slope changed from 6.25 ± 5.09° to 4.84 ± 2.50° (p = 0.034). Mean joint-line height relative to the fibular head changed from 15.93 ± 4.87 mm to 17.19 ± 5.91 mm (p = 0.035). Mean patellar tilt progressed from 5.90 ± 4.57° to 3.80 ± 3.51° (p = 0.0005). Mean patellar lateral translation on sunrise view progressed from 4.32 ± 3.26 mm to 3.31 ± 3.35 mm (p = 0.031).
Survivorship and complications
Five of the 57 patients alive at last follow-up (8.77%) had undergone revision (4 for infection and 1 for instability). Complications comprised 4 cases (7.02%) of infection, 2 cases (3.51%) of tibial and femoral loosening, 1 of which (1.75%) with associated patellar loosening, and 1 case (1.75%) of instability. The two patients with tibial and femoral aseptic loosening are asymptomatic and have not undergone revision surgery. Kaplan–Meier estimates showed 100% 5-year survivorship with tibial cone revision for aseptic loosening as an event, and 93.44% (95% CI 83.47–97.49%) for all-cause revision (Fig. 3).
Discussion
The primary conclusion of our study is the excellent medium-term results of tibial cones used for management of tibial bone defect and metaphyseal fixation in revision total knee arthroplasty. On the primary endpoint of survivorship for aseptic loosening of the revision TKA, clinical results at minimum 2 years follow-up were excellent. These results were similar to those reported for cones used in a femoral defect in revision TKA [8], with 5-year survivorship of 96% for cone revision due to aseptic loosening. To our knowledge, no other studies specifically reported medium-term results for cones used for tibial defect, although short-term results were good in Bohl et al. [13] with no subsequent complications or revision. Denehy [15] found similar results with 90.2% survival rate for any reason at 27 months mean follow-up with the Stryker cone for femoral and tibial defect. Backstein et al. found satisfactory results using allograft in revision TKA but results in our study are slightly improved compared to these findings [19]. As described by Denehy, the second-generation metaphyseal cones used in this study were produced from titanium powder using 3-dimensionally printed technology and were prepared for insertion with a simplified cannulated technique with markings on the reamers to identify the depth and size of the cone required to meet the surgical objectives. It makes the surgery easier than with the previous generation [15]. Moreover, the high number of trials and different sizes available help facilitate the use of these cones during surgery.
The secondary endpoint was all-cause survivorship. Compared to the recent literature, the current study results for tibial cones are comparable to the results for cones in septic revision reported by Burastero and by Agarwal, although these studies included both tibial and femoral defects [20, 21]. Our results are also comparable to those reported in systematic reviews by Divano et al. and Zanirato et al. [10, 22]. Klim et al. reported a lower survivorship rate but focused specifically using metaphyseal sleeves in septic revision TKA [23]. Sandiford et al. found no difference between femoral head allograft and trabecular metal cones for severe bone defects in revision TKA, and advocated that both may be used to address these defects in revision TKA [12]. Kim found no difference between cones and sleeves with severe bone defects in revision TKA, but the analysis included only a few studies and patients [24]. Stambough reported satisfactory results using acetabular wedge augments in uncontained tibial plateau defects [25]. These studies as well as the current study support the use of tibial cones as a viable option in revision TKA to aid with both primary and secondary fixation of the tibial component.
Complications with tibial cones are rare but do include risk of intraoperative fracture [22, 26]. Infection rate does not appear to be increased when using a tibial cone but larger and longer-term studies are needed to validate these conclusions [27]. In our study the complication rate was low, may be due to our patient population. Nevertheless, all patients requiring a tibial revision were included in our analysis.
Our study does have a number of limitations. First, it was a retrospective single-center study with a small number of patients and without a control group. However, we did not exclude any patients undergoing revision TKA with a tibial cone during the study period and data were extracted from a prospective database. Thus our results may be a good reflection of reality. The length of follow-up is relatively short but these are newer implants and longer-term follow-up is unavailable at this point. We have used these tibial cones in many types of bone defects because we believe the cones help anchor the implant improving primary and secondary fixation. Defect-oriented differentiation of the survivorship according to primary and secondary endpoints based on the bone defects T1-T3 could be useful but type 1 and 3 were rare with no statistical value. Despite these limitations, the present study results are encouraging for the use of tibial cones in revision TKA.
Conclusion
The present study of tibial cones shows excellent clinical results and survivorship and supports their use in revision TKA. However, longer and larger follow-up studies are needed to better assess long-term clinical outcomes in revision TKA.
References
Kurtz S, Ong K, Lau E et al (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 89:780–785. https://doi.org/10.2106/JBJS.F.00222
Hardeman F, Londers J, Favril A et al (2012) Predisposing factors which are relevant for the clinical outcome after revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 20:1049–1056. https://doi.org/10.1007/s00167-011-1624-8
Sheth NP, Bonadio MB, Demange MK (2017) bone loss in revision total knee arthroplasty: evaluation and management. J Am Acad Orthop Surg 25:348–357. https://doi.org/10.5435/JAAOS-D-15-00660
Mancuso F, Beltrame A, Colombo E et al (2017) Management of metaphyseal bone loss in revision knee arthroplasty. Acta Bio-Medica Atenei Parm 88:98–111
Meijer MF, Boerboom AL, Stevens M et al (2017) Tibial component with and without stem extension in a trabecular metal cone construct. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 25:3644–3652. https://doi.org/10.1007/s00167-016-4271-2
Faizan A, Bhowmik-Stoker M, Alipit V et al (2017) Development and verification of novel porous titanium metaphyseal cones for revision total knee arthroplasty. J Arthroplasty 32:1946–1953. https://doi.org/10.1016/j.arth.2017.01.013
Watters TS, Martin JR, Levy DL et al (2017) Porous-coated metaphyseal sleeves for severe femoral and tibial bone loss in revision TKA. J Arthroplasty 32:3468–3473. https://doi.org/10.1016/j.arth.2017.06.025
Potter GD, Abdel MP, Lewallen DG, Hanssen AD (2016) Midterm results of porous tantalum femoral cones in revision total knee arthroplasty. J Bone Joint Surg Am 98:1286–1291. https://doi.org/10.2106/JBJS.15.00874
Maslaris A, Layher F, Bungartz M et al (2019) Sagittal profile has a significant impact on the explantability of well-fixed cemented stems in revision knee arthroplasty: a biomechanical comparison study of five established knee implant models. Arch Orthop Trauma Surg 139:991–998. https://doi.org/10.1007/s00402-019-03160-4
Divano S, Cavagnaro L, Zanirato A et al (2018) Porous metal cones: gold standard for massive bone loss in complex revision knee arthroplasty? A systematic review of current literature. Arch Orthop Trauma Surg 138:851–863. https://doi.org/10.1007/s00402-018-2936-7
Fink B, Mittelstädt A (2019) Treatment of periprosthetic fractures of the knee using trabecular metal cones for stabilization. Arthroplasty Today 5:159–163. https://doi.org/10.1016/j.artd.2018.10.007
Sandiford NA, Misur P, Garbuz DS et al (2017) No difference between trabecular metal cones and femoral head allografts in revision TKA: minimum 5-year followup. Clin Orthop 475:118–124. https://doi.org/10.1007/s11999-016-4898-9
Bohl DD, Brown NM, McDowell MA et al (2018) Do porous tantalum metaphyseal cones improve outcomes in revision total knee arthroplasty? J Arthroplasty 33:171–177. https://doi.org/10.1016/j.arth.2017.07.033
Wirries N, Winnecken HJ, von Lewinski G et al (2019) Osteointegrative sleeves for metaphyseal defect augmentation in revision total knee arthroplasty: clinical and radiological 5-year follow-up. J Arthroplasty. https://doi.org/10.1016/j.arth.2019.04.024
Denehy KM, Abhari S, Krebs VE et al (2019) Excellent metaphyseal fixation using highly porous cones in revision total knee arthroplasty. J Arthroplasty. https://doi.org/10.1016/j.arth.2019.03.045
Abdelaziz H, Jaramillo R, Gehrke T et al (2019) Clinical survivorship of aseptic revision total knee arthroplasty using hinged knees and tantalum cones at minimum 10-year follow-up. J Arthroplasty 34:3018–3022. https://doi.org/10.1016/j.arth.2019.06.057
Engh GA, Ammeen DJ (1998) Classification and preoperative radiographic evaluation: knee. Orthop Clin North Am 29:205–217. https://doi.org/10.1016/s0030-5898(05)70319-9
Scuderi GR, Tria AJ (2006) Knee arthroplasty handbook: techniques in total knee and revision arthroplasty. Springer Science and Business Media https://www.springer.com/gp/book/9780387307305
Backstein D, Safir O, Gross A (2006) Management of bone loss: structural grafts in revision total knee arthroplasty. Clin Orthop Relat Res 446:104. https://doi.org/10.1097/01.blo.0000214426.52206.2c
Burastero G, Cavagnaro L, Chiarlone F et al (2018) The use of tantalum metaphyseal cones for the management of severe bone defects in septic knee revision. J Arthroplasty 33:3739–3745. https://doi.org/10.1016/j.arth.2018.08.026
Agarwal S, Neogi DS, Morgan-Jones R (2018) Metaphyseal sleeves in revision total knee arthroplasty: minimum seven-year follow-up study. Knee. https://doi.org/10.1016/j.knee.2018.09.010
Zanirato A, Cavagnaro L, Basso M et al (2018) Metaphyseal sleeves in total knee arthroplasty revision: complications, clinical and radiological results. A systematic review of the literature. Arch Orthop Trauma Surg 138:993–1001. https://doi.org/10.1007/s00402-018-2967-0
Klim SM, Amerstorfer F, Bernhardt GA et al (2018) Septic revision total knee arthroplasty: treatment of metaphyseal bone defects using metaphyseal sleeves. J Arthroplasty. https://doi.org/10.1016/j.arth.2018.08.017
Kim HJ, Lee O-S, Lee SH, Lee YS (2018) Comparative analysis between cone and sleeve in managing severe bone defect during revision total knee arthroplasty: a systematic review and meta-analysis. J Knee Surg 31:677–685. https://doi.org/10.1055/s-0037-1606564
Stambough JB, Haynes JA, Barrack RL, Nunley RM (2018) Acetabular wedge augments for uncontained tibial plateau defects in revision total knee arthroplasty. Arthroplasty Today 4:313–318. https://doi.org/10.1016/j.artd.2018.02.005
Barnett SL, Mayer RR, Gondusky JS et al (2014) Use of stepped porous titanium metaphyseal sleeves for tibial defects in revision total knee arthroplasty: short term results. J Arthroplasty 29:1219–1224. https://doi.org/10.1016/j.arth.2013.12.026
Mortazavi SMJ, Schwartzenberger J, Austin MS et al (2010) Revision total knee arthroplasty infection: incidence and predictors. Clin Orthop 468:2052–2059. https://doi.org/10.1007/s11999-010-1308-6
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
RE: none; RT: none; AM: none; WP: consultancy fees and speaker fees from Zimmer-Biomet, Stryker, Intellijoint and Medtronic.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Oral consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Erivan, R., Tracey, R., Mulliez, A. et al. Medium term clinical outcomes of tibial cones in revision knee arthroplasty. Arch Orthop Trauma Surg 141, 113–118 (2021). https://doi.org/10.1007/s00402-020-03532-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03532-1