Abstract
Introduction
The posterolateral approach is used in most cases of surgical treatment of ankle fractures involving the posterior and lateral malleoli. However, this approach does not allow access to the anterolateral structures of the ankle, which represent important landmarks to allow an anatomical reduction in case of complex ankle fracture.
Our objective is to propose a novel surgical approach for optimal management of injuries including both a fracture of the posterior malleolus and a complex lesion of the lateral and/or anterolateral portions of the ankle.
Methods
Cadaveric dissection, including a vascular study, was performed on eight specimens. Assessment included density of the vascular supply around the lateral malleolus, identification of the structures at risk, quality of exposure of the bony structures, and convenience of hardware fixation.
Results
The cutaneous flap benefits from a rich interconnected arterial supply. Structures at risk, including the superficial peroneal and sural nerves, the lesser saphenous vein, and the peroneal artery are easily identified and protected. The interval between the peroneal tendons and the flexor hallucis longus muscle provides optimal access to the posterior malleolus. The lateral malleolus is exposed by retracting the peroneal tendons medially. An anterolateral arthrotomy, respecting the anterior talofibular and tibiofibular ligaments, offers a sharp view on the talo-tibio-fibular junction. Hardware placement can be done with optimal access to any exposed surfaces.
Conclusions
The PAMELA opens a new perspective in the optimal management of complex fractures of the ankle. The approach allows optimal exposure to address fractures of the posterior malleolus, of the lateral malleolus, and of the anterolateral portion of the ankle through a single incision. Application in clinical practice is the subject of a future study in our institution.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Comprehensive anatomical reduction of ankle fractures optimizes the clinical and radiological outcome [1,2,3] even if several other factors also influence the long term results [4]. Clear visualization of anatomical landmarks is mandatory for precise fracture reduction. Furthermore, several recent publications recommend the use of pre-operative CT scan for identification and classification of the fracture pattern and for determining the best surgical approach [5,6,7,8,9]. These studies particularly focused on posterior malleolar fractures. A posterolateral approach has been found to give adequate access to posterolateral tibial fragments, which account for more than 60% of posterior malleolar fractures [6, 8] while a posteromedial approach is recommended for fractures of the posterior malleolus extending into the medial malleolus [8].
The posterolateral approach is carried out through the interval between the peroneal tendons and the flexor hallucis longus muscle belly to access the posterior malleolus. The fibula is accessed by retracting the peroneal tendons medially or laterally [10,11,12,13,14]. Although this approach allows visualization of both the posterior malleolus and the fibula, it does not give access to the anterolateral portion of the ankle, including, the anterior syndesmosis, the Chaput tubercle, and the tibio-talo-fibular junction. In case of complex ankle injuries, as after high energy trauma or in elderly patients with poor bone quality, diaphyseal and metaphyseal bony landmarks become less reliable. Therefore, exposure of the tibio-talo-fibular junction provides substantial additional information to achieve anatomical reduction. Surgical experience shows that access to the posterior aspect of this junction is difficult due to the strong transverse ligaments and also to the posterior position of the fibula. Conversely, clear visualization of the anterior tibio-talo-fibular junction is easy. Therefore, a surgical approach allowing simultaneous access to the posterior malleolus, to the fibula, and to the anterolateral portion of the joint could be advantageous in the setting of complex ankle injury.
The aim of our study is to describe a surgical approach, considering local vascularization and structures at risk that provides optimal access to the posterior, lateral, and anterolateral portion of the joint.
Methods
Eight fresh frozen cadaveric paired lower limbs from Caucasian voluntary donor specimens were used, provided by the Anatomy and Morphology Faculty Unit of the University of Lausanne (Switzerland). Four specimens (two pairs) were amputated at the level of distal diaphyseal tibia and used for the preliminary vascular study. The other four specimens (two pairs) were used for the study of the surgical approach and were above-knee amputated to preserve muscular tension at the ankle. All limbs were examined for the absence of signs of previous surgery.
Vascular study
The anterior tibial, posterior tibial and peroneal arteries were identified on each specimen and catheterized with an 18 Gauge venous catheter secured with a clamp. After copious irrigation with water and manual draining, colored liquid latex (Plastylate, Latex milk, Glorex Inspirations® with Universal colorant, Abtönen®) was injected simultaneously in all three arteries (blue latex for the posterior tibial artery, pink latex for the peroneal artery and green latex for the anterior tibial artery). Forty-eight hours after injection, dissection was performed on the four specimens. The presence of cutaneous color was recorded, as well as the abundance of subcutaneous blood network and the distribution according to the three main arteries.
Surgical approach
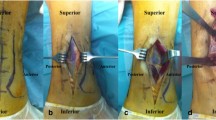
The four above-knee amputated specimens were placed in a lateral decubitus position, and dissection was performed by a senior orthopedic surgeon. A cartography was established defining the safe zone for skin incision. A standardized l-shaped incision pattern (Fig. 1) was then defined in relationship with both this cartography and three anatomical landmarks including: the lateral malleolus; the lateral edge of the Achilles tendon; the sinus tarsi. The longitudinal part of the incision was placed at the junction between the anterior third and the posterior two thirds of the interval between the posterior edge of the fibula and the lateral edge of the Achilles tendon, and measured about 10 cm, ending at the level of the tip of the malleolus. The distal part of the incision continued obliquely on a straight line defined by the sinus tarsi and the tip of the lateral malleolus. Both parts of the incision crossed behind the lateral malleolus at an angle of 110°. At first, the position of the sural and peroneal superficial nerves was assessed. The peroneal tendons were retracted posteriorly to expose the distal fibula. To visualize the posterior malleolus, two ways of deepening the incision were compared: the first retracting the peroneal tendons medially; the second, incising the fascia at the posterior border of the peroneal tendons and deepening through the interval between the peroneal tendons and the flexor hallucis longus muscle belly. To access the anterior syndesmosis, a thick cutaneous flap was prepared anteriorly, exposing the inferior extensor retinaculum, which was partially incised to reach the anterior talofibular ligament. Then, arthrotomy was performed in the interval between the anterior talofibular and the anterior tibiofibular ligaments in order to expose the anterior aspect of the tibio-talo-fibular junction and the anterior superolateral margin of the talar dome.
Photograph showing the standardized incision pattern (dotted line). The vertical part of the incision is situated at the junction between the anterior third and the posterior two thirds of the interval between the posterior edge of the fibula and the lateral edge of the Achilles tendon. The distal part of the incision is on a straight line defined by the sinus tarsi and the tip of the lateral malleolus. Both parts of the incision cross behind the lateral malleolus at an angle of 110°. Continuous purple lines define the bony contours of the fibula and tibia anteriorly, and the lateral edge of the Achilles tendon posteriorly. The circle designates the sinus tarsi. Colored lines represent the course of the superficial peroneal (green) and sural (blue) nerves
We evaluated:
-
(1)
the structures at risk encountered while performing the dissection;
-
(2)
the best way to reach the posterior malleolus;
-
(3)
the quality of exposure of bony surfaces;
-
(4)
the quality of exposure of the articular margins;
-
(5)
the convenience to reduce and stabilize the simulated fractures.
Results
Vascular study
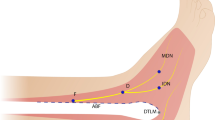
The external analysis of the four specimens revealed only little cutaneous coloration: toes were slightly green (injection into the anterior tibial artery) and the sole of the foot was slightly blue (injection into the posterior tibial artery). Dissection was performed to produce a thin skin flap in order to visualize the subcutaneous vascularization: a dense network of subcutaneous vessels was observed in all specimens, with some variations noted about the arterial territories (Fig. 2). The distribution of the anterior tibial artery extended overall to the anterior aspect of the ankle, in front of the lateral malleolus, and the peroneal artery territory was posterior to the lateral malleolus and extended to the lateral aspect of the hind foot. The contribution of the posterior tibial artery was variable. A dense network of anastomoses was present between these territories, demonstrating a rich vascularization of this zone.
Subcutaneous vascularization around the lateral malleolus. a Vascular network constituted of pink vessels from the peroneal artery (P) and green vessels from the anterior tibial artery (AT). The posterior tibial artery (blue vessels, PT) contributes to the network in front of the fibula in this specimen. Anastomoses between the anterior tibial and the posterior tibial arteries are seen (*). b The density of the vascularity in another specimen, in whom the anterior tibial artery predominates (green coloration)
Surgical approach
Structures at risk encountered while performing the more superficial part of the approach included: the superficial peroneal nerve; the sural nerve; the lesser saphenous vein. We made identical observations in all four specimens. The superficial peroneal nerve crossed the lateral malleolus 9 cm above its tip, then run 1 cm anteriorly of the apex of the lateral gutter (Fig. 3a) and 2 cm anteriorly of the distal part of the incision (sinus tarsi) (Fig. 3b). The sural nerve, together with the lesser saphenous vein, were found halfway between the posterior edge of the fibula and the lateral edge of the Achilles tendon, which also means that they were located 1 cm posteriorly to the posterior edge of peroneal tendons (Fig. 4a). Due to their subcutaneous location in the epifascial fat tissue, and to their position posteriorly to the portion of the crural fascia that had to be longitudinally sectioned to allow the deepening between the peroneal tendons and the flexor hallucis longus, the sural nerve and lesser saphenous vein could be efficiently protected by posterior retraction of the crural fascia (Fig. 4b). The peroneal artery was the only structure at risk when performing the deeper part of the approach. This occurred when creating the interval between the peroneal tendons and the flexor hallucis longus muscle belly. Protecting the artery requires to remain in close contact with the peroneal tendons and to retract the artery medially together with the flexor hallucis longus muscle.
Incising the crural fascia at the posterior margin of the peroneal tendons, and deepening the incision through the interval between the peroneal tendons and the flexor hallucis longus muscle belly appeared as the best way to access the posterior malleolus. It provided a large window on the posterior malleolus and required only gentle tissue retraction. Accessing the posterior malleolus by retracting the tendons medially was also possible but required a strong tension on the tendons, and allowed poor visualization of the posterior tibia.
A cartography of the bony surfaces that could be exposed is shown in Fig. 5 The exposure of the posterior malleolus using the interval between the peroneal tendons and the flexor hallucis longus corresponds to 80% of its width and extends proximally over more than 5 cm (Fig. 6a). The lateral malleolus could be fully exposed, including its posterior aspect, by mobilizing the peroneal tendons medially (Fig. 6b). The anterior extension of the approach further allowed visualization of the whole Chaput tubercle (Fig. 6c). The anterolateral articular margin, including the tibio-talo-fibular junction, could be exposed after arthrotomy between the anterior talofibular and the anterior tibiofibular ligaments (Fig. 6d). If a Basset ligament was present it had to be resected for optimal visualization. The anterolateral view also allowed to expose the superolateral talar surface over 1.5 cm2 (Fig. 6d). The lateral 80% of the posterior tibiotalar articular margin were visible while exposing the posterior malleolus (Fig. 6e). This, however, required the lower portion of the posterior tibiofibular ligament to be detached from its tibial insertion. Access to a small portion of the posterior talar dome was also possible.
The exposure of the anterolateral and posterior structures obtained with the PAMELA are shown. a Posterior malleolus. b Lateral and posterolateral aspects of the lateral malleolus. c Chaput tubercle—a fracture was simulated using an osteotome. d Anterolateral margin (tibio-talo-fibular junction), with exposition of the superolateral talar surface. e Posterior tibiotalar articular margin, after detachment of the lower portion of the posterior tibiofibular ligament, and visualization of a portion of the posterior talar dome
The procedure allowed to place plates on the posterior aspect of the lateral malleolus, on the posterior malleolus, and on the Chaput tubercle (Fig. 7). With the limb positioned in lateral decubitus, perpendicular position of the drill bit, or screw driver was possible for all three locations of the plates. Furthermore, as shown in Fig. 8, 90° of freedom was provided to access the posterior malleolus with the instruments.
Discussion
In this study we describe a surgical approach allowing to address complex ankle fractures involving the posterior, lateral, and anterolateral portions of the joint.
Our vascular analysis demonstrates that the anterior tibial artery is the most important contributor to the vascularization of the flap created by the described incision. Nevertheless, the anastomoses between the anterior tibial, peroneal and even posterior tibial arteries create a rich vascular network suggesting that the flap around the lateral malleolus is well vascularized. Our findings concur with previous reports. In their study of the angiosomes, Attinger et al. [15] found that the vascularity of the foot and ankle is redundant because of the multiple connections between the main supplying arteries. Borrelli and Lashgari [16] stated that the skin and subcutaneous tissues of the lateral aspect of the hindfoot appear to receive their blood supply from a complex of vessels and not from a single angiosome. Furthermore, Taylor and Pan [17] showed that connections between adjacent angiosomes occurred within tissues and not between them. Therefore, although our incision is not placed strictly between two angiosomes, our vascular assessment and the aforementioned studies allow to choose a compromise between the vascular supply and the quality of exposure, as suggested by Attinger [18].
Our incision is based on easy identifiable anatomical landmarks, including the lateral margin of the Achilles tendon, the posterior margin of the fibula, the tip of the lateral malleolus, and the sinus tarsi. Structures at risk while performing the superficial part of the approach include the superficial peroneal nerve, the sural nerve and the lesser saphenous vein. They do not cross the incision. Nevertheless, they can be easily identified if required and protected without tension. Solomon et al. [19] demonstrated that the sural nerve is located at an average of 7 mm posterior to lateral malleolus, which is consistent with our findings. Nevertheless, variations are frequent, as described by Kosinski [20], and the nerve is sometimes directly in contact with the posterior aspect or tip of the lateral malleolus [19]. The superficial peroneal nerve has been shown to be located at an average of 23 mm anterior to the tip of the lateral malleolus [19], which we also observed in our dissections.
Deepening the incision between the peroneal tendons and the flexor hallucis longus muscle, the only structure at risk is the peroneal artery. To avoid injuring this vessel, dissection is carried out very close to the peroneal tendons so that the artery and its surrounding tissues can be retracted laterally together with the flexor hallucis muscle belly. Furthermore, knowing that the peroneal artery usually bifurcates and perforates through the interosseous membrane 6–8 cm above the tibial plafond, and, in some cases, even 4 cm above it [21], careful proximal dissection and mobilization is required for safe placement of a buttress plate on the posterior malleolus.
The approach permits a large visualization of the posterior malleolus, excluding the very medial portion, an optimal exposure of the lateral malleolus, and a precise control of the anterior tibio-talo-fibular congruence. The anterior view further allows to address a fractured Chaput tubercle, a Wagstaffe-Le Fort avulsion fracture, a fracture of the anterolateral margin of the talar dome, and the extraction of small free bony fragments located within the lateral gutter of the ankle. Our approach finally creates optimal condition for placement of plates or screws to stabilize any of the above mentioned fractures.
To the best of our knowledge, the present study is the first to propose a comprehensive approach to address simultaneously the posterior, lateral and anterolateral portions of the ankle. Indications to select this approach are summarized in Table 1. We have learned from Haraguchi et al. [6] and Bartoníček et al. [8] that fractures of the posterior malleolus extending into the medial malleolus are best treated by a posteromedial approach or even by a modified posteromedial approach as described by Assal et al. [22]. In contrast, fractures of the posterior malleolus that can be addressed by our approach include Haraguchi type one, and Bartoníček type two and four fractures, which represent the majority of posterior malleolar fractures. The medial malleolus is then accessed through a second, medial, incision.
Studies on the posterolateral approach to the ankle, that can also be used in combination with a medial approach in case of trimalleolar fractures, have confirmed the good visualization of both the posterior and lateral malleoli [10, 11, 13, 23, 24]. However there is a lack of information regarding the landmarks to be used in case of severely comminuted lateral malleolar fractures as well as regarding the strategy to simultaneously address a displaced fracture of the anterolateral portion of the ankle, including the bony extremities of the anterior syndesmosis or the anterolateral margin of the talar dome. The present study contributes to fill this gap by providing the possibility to visualize additional landmarks while allowing the fixation of fractures of the anterolateral portion of the ankle. Mak et al. [3] emphasized the importance of stabilizing the mortise by anatomical reduction and stated that Chaput fractures are often overlooked and neglected, thus leading to poor reduction and poor outcome. Two studies focused on the importance of fixation of Wagstaffe or Chaput fragment in the setting of complex ankle fracture [25, 26]. However, poor description of the approach, and few consideration about the access to the posterior malleolus are provided. McGoldrick et al. [27] were the first to propose an incision that allows exposure of the posterior malleolus and access to the anterolateral portion of the ankle joint: they proposed an oblique incision running over the lateral malleolus from posterior proximal to anterior distal. They approached the posterior malleolus through an interval between the fibula and the peroneal tendons which we found, in our study, to be associated with poor visualization of the posterior malleolus and required strong retraction tension on the peroneal tendons. There is scant information regarding the methodology used in their study and no detailed recommendations are provided.
The main limitation of our study, as regards its applicability in clinical practice, is its design as a cadaveric study. However, there are no significant technical hurdles to overcome in order to use our approach in real conditions. Despite the reassuring results of our vascular study combined with previous reports about the rich vascularity of the soft tissues surrounding the lateral malleolus, clinical application alone would allow to assess the definitive risk of necrosis of the cutaneous flap.
In conclusion, the present study, is the first to propose a comprehensive approach allowing optimal exposure to address fractures of both the posterior and lateral malleoli and of the anterolateral portion of the ankle through a single incision and offers new perspectives in the optimal management of complex fractures of the ankle. Furthermore, anatomical guidelines are provided in case intraoperative decision to extend the standard posterolateral approach has to be taken. Our posterior to anterior malleolar extended lateral approach (PAMELA) can, of course, be combined with a medial incision for medial malleolus fixation. Application in clinical practice is the subject of a future prospective study in our institution.
References
Berkes MB, Little MTM, Lazaro LE et al (2013) Articular congruity is associated with short-term clinical outcomes of operatively treated SER IV ankle fractures. J Bone Joint Surg Am 95:1769–1775. https://doi.org/10.2106/JBJS.L.00949
Verhage SM, Krijnen P, Schipper IB, Hoogendoorn JM (2019) Persistent postoperative step-off of the posterior malleolus leads to higher incidence of post-traumatic osteoarthritis in trimalleolar fractures. Arch Orthop Trauma Surg 139:323–329. https://doi.org/10.1007/s00402-018-3056-0
Mak MF, Stern R, Assal M (2018) Repair of syndesmosis injury in ankle fractures: current state of the art. EFORT Open Rev 3:24–29. https://doi.org/10.1302/2058-5241.3.170017
Lübbeke A, Salvo D, Stern R et al (2012) Risk factors for post-traumatic osteoarthritis of the ankle: an eighteen year follow-up study. Int Orthop 36:1403–1410. https://doi.org/10.1007/s00264-011-1472-7
Solan MC, Sakellariou A (2017) Posterior malleolus fractures: worth fixing. Bone Joint J 99-B:1413–1419. https://doi.org/10.1302/0301-620X.99B11.BJJ-2017-1072
Haraguchi N, Haruyama H, Toga H, Kato F (2006) Pathoanatomy of posterior malleolar fractures of the ankle. J Bone Joint Surg Am 88:1085–1092. https://doi.org/10.2106/JBJS.E.00856
Yi Y, Chun D-I, Won SH et al (2018) Morphological characteristics of the posterior malleolar fragment according to ankle fracture patterns: a computed tomography-based study. BMC Musculoskelet Disord 19:51. https://doi.org/10.1186/s12891-018-1974-1
Bartoníček J, Rammelt S, Kostlivý K et al (2015) Anatomy and classification of the posterior tibial fragment in ankle fractures. Arch Orthop Trauma Surg 135:505–516. https://doi.org/10.1007/s00402-015-2171-4
Kumar A, Mishra P, Tandon A et al (2018) Effect of CT on management plan in malleolar ankle fractures. Foot Ankle Int 39:59–66. https://doi.org/10.1177/1071100717732746
Verhage SM, Boot F, Schipper IB, Hoogendoorn JM (2016) Open reduction and internal fixation of posterior malleolar fractures using the posterolateral approach. Bone Joint J 98-B:812–817. https://doi.org/10.1302/0301-620X.98B6.36497
Tornetta P, Ricci W, Nork S et al (2011) The posterolateral approach to the tibia for displaced posterior malleolar injuries. J Orthop Trauma 25:123–126. https://doi.org/10.1097/BOT.0b013e3181e47d29
Talbot M, Steenblock TR, Cole PA (2005) Posterolateral approach for open reduction and internal fixation of trimalleolar ankle fractures. Can J Surg 48:487–490
Dhillon M, Dureja K, Patel S (2017) How we do it. Trimalleolar fractures: fixing the posterior malleolus by posterolateral approach. J Foot Ankle Surg Asia-Pac 4:63–68
Abdelgawad AA, Kadous A, Kanlic E (2011) Posterolateral approach for treatment of posterior malleolus fracture of the ankle. J Foot Ankle Surg 50:607–611. https://doi.org/10.1053/j.jfas.2011.04.022
Attinger CE, Evans KK, Bulan E et al (2006) Angiosomes of the foot and ankle and clinical implications for limb salvage: reconstruction, incisions, and revascularization. Plast Reconstr Surg 117:261S–293S. https://doi.org/10.1097/01.prs.0000222582.84385.54
Borrelli J, Lashgari C (1999) Vascularity of the lateral calcaneal flap: a cadaveric injection study. J Orthop Trauma 13:73–77
Taylor GI, Pan WR (1998) Angiosomes of the leg: anatomic study and clinical implications. Plast Reconstr Surg 102:599–616 (discussion 617-618)
Attinger C, Cooper P, Blume P, Bulan E (2001) The safest surgical incisions and amputations applying the angiosome principles and using the Doppler to assess the arterial-arterial connections of the foot and ankle. Foot Ankle Clin 6:745–799
Solomon LB, Ferris L, Tedman R, Henneberg M (2001) Surgical anatomy of the sural and superficial fibular nerves with an emphasis on the approach to the lateral malleolus. J Anat 199:717–723
Kosinski C (1926) The course, mutual relations and distribution of the cutaneous nerves of the metazonal region of leg and foot. J Anat 60:274–297
Lidder S, Masterson S, Dreu M et al (2014) The risk of injury to the peroneal artery in the posterolateral approach to the distal tibia: a cadaver study. J Orthop Trauma 28:534–537. https://doi.org/10.1097/BOT.0000000000000089
Assal M, Dalmau-Pastor M, Ray A, Stern R (2017) How to get to the distal posterior tibial malleolus? A cadaveric anatomic study defining the access corridors through 3 different approaches. J Orthop Trauma 31:e127–e129. https://doi.org/10.1097/BOT.0000000000000774
OʼConnor TJ, Mueller B, Ly TV et al (2015) “A to p” screw versus posterolateral plate for posterior malleolus fixation in trimalleolar ankle fractures. J Orthop Trauma 29:e151–156. https://doi.org/10.1097/BOT.0000000000000230
Li M, Collier RC, Hill BW et al (2017) Comparing different surgical techniques for addressing the posterior malleolus in supination external rotation ankle fractures and the need for syndesmotic screw fixation. J Foot Ankle Surg 56:730–734. https://doi.org/10.1053/j.jfas.2017.01.053
Nelson OA (2006) Examination and repair of the AITFL in transmalleolar fractures. J Orthop Trauma 20:637–643. https://doi.org/10.1097/01.bot.0000211145.08543.4a
Zhang M, Chen Y-F, Wang L et al (2018) Clinical characteristics and surgical experience of Type III Wagstaffe fractures: pay attention to concomitant chondral injury of the talus. Foot Ankle Surg 24:394–399. https://doi.org/10.1016/j.fas.2017.04.013
McGoldrick NP, Murphy EP, Kearns SR (2016) Single oblique incision for simultaneous open reduction and internal fixation of the posterior malleolus and anterior syndesmosis. J Foot Ankle Surg 55:664–667. https://doi.org/10.1053/j.jfas.2016.01.031
Acknowledgements
The authors thank the UFAM (Université Facultaire d'Anatomie et de Morphologie) of the University of Lausanne directed by Prof. J.-P. Hornung for the dissection facilities.
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation was performed by HC. Data collection and analysis were performed by XC and AK. The first draft of the manuscript was written by AK and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kummer, A., Cadas, H. & Crevoisier, X. Posterior to anterior malleolar extended lateral approach to the ankle (PAMELA): a cadaveric anatomic study. Arch Orthop Trauma Surg 141, 427–435 (2021). https://doi.org/10.1007/s00402-020-03507-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03507-2