Abstract
Introduction
Despite the presence of various different surgical procedures, the preferable technique for repair of acute Achilles tendon ruptures is unknown and, therefore, object of discussions. The purpose of this meta-analysis was to compare clinical outcomes and complication-rates between the minimally invasive and the standard open repair of acute Achilles tendon ruptures.
Materials and methods
This meta-analysis was performed according to the PRISMA guidelines. In September 2019 the main databases were accessed. All clinical trials of evidence level I to III comparing minimally invasive vs. open surgery of Achilles tendon rupture were included in the present study. Only articles reporting quantitative data under the outcomes of interest were included. Missing data under the outcomes of interest warranted the exclusion from the present work. For the statistical analysis we referred to the Review Manager Software Version 5.3. (The Nordic Cochrane Centre, Copenhagen). Continuous data were analysed through the inverse variance method. For the effect estimate the mean difference was used. Dichotomous data were analysed through the Mante–Haenszel method via odd ratio effect measure. The confidence interval was set at 95% in all the comparisons. Values of P < 0.05 were considered statistically significant.
Results
A total of 25 articles were included for meta-analysis. The funnel plot revealed poor data dispersion, attesting to this study a low risk of publication bias. The quality of the methodological assessment was moderate. Data from 2223 (1055 open, 1168 minimally invasive) surgical procedures were extracted. The mean follow-up was of 24.29 ± 22.4 months. The open group reported a lower value of post-operative palpable knot at last follow-up and a lower rate of sural nerve palsy. In the minimally-invasive group a shorter surgery duration and a lower rate of post-operative wound necrosis and reduced risk of wound scarring and adhesions has been evidenced. The minimally-invasive cohort detected the lowest values of superficial and deep infections. In both groups no significant difference was shown in re-rupture rate.
Conclusions
Compared to the minimally-invasive Achilles tendon reconstruction, the open procedure evidenced a lower rate of sural nerve palsy and postoperative palpable knot, whereas in the minimally-invasive reconstruction group quicker surgery duration, a lower rate of post-operative wound necrosis, superficial and deep infections and less scar tissue adhesions could be observed. No relevant discrepancies were detected among the two techniques in terms of post-operative re-rupture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The adequate treatment of acute Achilles tendon rupture has been controversially discussed in the last decades and also in current literature. Both, non surgical and surgical treatment may be suitable, whereas surgical repair is regarded as achieving a better functional outcome, a decreased re-rupture rate and a shorter recovery time, therefore representing the favourable treatment especially for young patients [1, 2]. However, performing surgical repair might cause complications such as wound infections and necrosis resulting in devastating soft tissue complication which might require further surgical reconstruction. However, initially the percutaneous approach has been introduced 1977 by Ma and Griffth [3] to minimize the exposure of the Achilles tendon and thus to reduce complications in comparison to open procedures. The approach was supposed to be more challenging due to the missing exposure of the tendon and, furthermore, predisposed for re-ruptures based on insufficient suturing without direct visual control [4]. Therefore, in 1996 Assal et al. developed a device, called Achillon®, offering a minimally invasive (MIS) approach in combination with a percutaneous suture [5], which is partly based on the technique described by Kakiuchi in 1995 [6]. This combination of a percutaneous and mini-open technique offers direct visualisation of the rupture location, but a reduced risk for wound complications [4]. Nowadays, orthopaedic surgeons routinely use percutaneous-minimally invasive procedures and can make full use of surgical aid devices like Tenolig™, Achillon®, PARS® or the Dresden instrument in combination with ultrasound guided approaches [5, 7,8,9].
Previous meta-analysis concluded that minimally-invasive surgery for acute Achilles tendon repair promoted reduced infection rate and wound necrosis with a similar re-rupture risk in comparison to an open procedure [10, 11]. The most recent meta-analysis of randomized clinical trials (RCT) evaluating 358 procedures confirmed these findings and stated that patients treated with MIS surgery were more likely to report good or excellent subjective results without any difference according sural nerve injury, return to preinjury activity level or to work [12].
However, there is still discordance, since a systematic review of overlapping meta-analyses revealed that only superficial and not deep infections are reduced by MIS [10]. Moreover, previous meta-analysis pointed out, that their results are associated with a high heterogeneity and a considerable risk of bias due to limited high-quality studies [11, 12]. Recently, two additional RCT studies have been published evaluating a considerable higher number of procedures, which might improve the statistical value for recommendations [13, 14]. Additionally, previous meta-analysis are based on a limited amount of available RCT studies or on only a few included observational studies due to the evaluation of infrequent outcome parameters. Interestingly, numerous reports pointed out that there is only limited evidence for differences between effect estimations between RCTs and observational studies [15,16,17]. However, the addition of observational studies increases sample size, enabling evaluation of small treatment effects. Especially, analysis of a variety of populations, and long-term effects are not limited to the usually highly selected cohorts in RCTs [15, 18, 19].
Consequently, we conducted a comprehensive meta-analysis study comparing the complication-rates of open versus MIS for Achilles tendon repair including RCTs and observational studies without evaluating infrequent outcome parameters. The purpose of the present study was to update current evidences and to analyse the clinical trials presented in the current literature in order to clarify the role of these two techniques and to simplify the surgical decision making in selected patients.
Materials and methods
Literature research and data extraction
This meta-analysis was performed according to the Preferred Reporting Items for Systematic Review and Meta-Analysis: the PRISMA guidelines [20]. The PICO protocol was drafted to guide the search:
-
P (population): Achilles tendon rupture
-
I (intervention): open Achilles tendon reconstruction
-
C (comparison): percutaneous/minimally-invasive Achilles tendon reconstruction
-
O (outcomes): complications, functional outcome score
In September 2019 the main databases were accessed: Pubmed, Scopus, Google Scholar. The keywords were “Achilles tendon” combined through the Boolean operator AND with “rupture”, “percutaneous”, “minimally invasive”, “mini-invasive”, “open” as well as “Achillon”, “PARS”, “Tenolig” and “Dresden”. Additionally, manual scanning of the reference lists of the included articles and reviews were performed. Two independent reviewers (FM, MG) independently screened the literature for inclusion. If title matched the topic, the abstract was accessed and, if of interest, the full-text was read. The bibliographies of the articles were also screened. Disagreements between the authors were debated and mutually solved.
Eligibility criteria
All the clinical trials comparing the minimally-invasive repair vs. open surgery after acute Achilles tendon rupture were included in the present study. The percutaneous and minimally-invasive approach were put together as “minimally-invasive” and were opposed to the open procedure. According to Oxford Centre of Evidenced-Based Medicine [21], only clinical trials levels I to III of evidence were considered for inclusion. According to the author language capabilities, articles in English, French, Italian, Spanish, German and Portuguese were considered for inclusion. Only articles published after 2000 were included. Data from national register, case series, expert opinion, editorials were excluded as well as biomechanical, in-vitro and animal studies. Articles dealing with chronic Achilles tendon ruptures were excluded. Only articles reporting quantitative data under the outcomes of interest were included. Missing data under the outcomes of interest warranted the exclusion from the present work. Disagreements between the authors were mutually debated and solved.
Outcomes of interest
Two independent authors (FM, MG) independently grouped data from the articles of interest. The following demographic data were collected: author and year of publication, type of study, mean follow-up, number of samples, location of rupture, pain before rupture, body mass index (BMI), age and gender distribution. Additionally, data about surgical techniques, the suture material used and post-operative care were collected. Moreover, for each endpoint, the following clinical data and post-operative complications were collected: surgery duration, superficial and deep tissue infection, tendon re-rupture, scare tissue formation, tissue adhesions, sural nerve palsy, wound necrosis and palpable knot. Since patient-reported outcome measurements (PROMS) are infrequently and inconsistently used, their inclusion has been refused, in order to not downsize the sample size.
Methodological quality assessment
For the methodological quality assessment, we referred to the Review Manager Software Version 5.3. (The Nordic Cochrane Centre, Copenhagen). The risk of bias summary tool was performed according to the authors' judgements about each risk of bias item for each included study.
Statistical analysis
For the statistical analysis we referred to the Review Manager Software Version 5.3. (The Nordic Cochrane Centre, Copenhagen). Continuous data were analysed through the inverse variance method. For the effect estimate (EE) the mean difference was used. Dichotomous data were analysed through the Mantel–Haenszel method via odd ratio (OR) effect measure. Heterogeneity was evaluated trough the \(\chi\)2 and Higgins-I2 methods. If \(\chi\)2 > 0.5 the I2 test was evaluated. Ranges for interpretation of I2 according to the Cochrane Handbook for Systematic Reviews of Interventions were 0–40% (poor), 30–60% (fair), 50–90% (moderate) and 75–100% (considerable). A fixed model effect was used when heterogeneity was acceptable. In event of high heterogeneity, a random model was used. The confidence interval was set at 95% in all the comparisons. Values of p < 0.05 were considered statistically significant.
Results
Search result
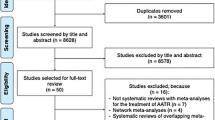
The literature search resulted in 4420 papers with 3229 articles screened for inclusion after removing duplicates (1191). A total of 2445 papers were excluded due to incompatibility with the eligibility criteria. Another 744 articles were excluded due to lack of quantitative data under the outcomes of interest. Further, 15 articles were excluded because of uncertain and/or ambiguous results. Finally, a total of 25 articles were included for the meta-analysis. The flow-chart of the literature search is shown in Fig. 1.
Risk of publication bias
To assess the risk of publication bias, the funnel plot of the most reported outcome was performed (infection). The plot detected good symmetrical distribution of the referral points. All the values are narrow to the no-effect line and none outside the range of acceptability. This revealed poor data dispersion, attesting to this study a low risk of publication bias. The funnel plot is shown in Fig. 2.
Methodological quality assessment
According to the risk of bias summary, high risk of detection bias was evidenced. This reflected the overall lack of samples blinding among the studies. The overall lack of randomization increased the selection bias. Incomplete outcome data detected a good risk of attrition bias, while the risk of other unknown bias was low. In conclusion, we attest to the present work a moderate quality of the methodological assessment. The authors' judgements about each risk of bias item for each included study are shown in Fig. 3.
Patient demographic
A total of 2223 procedures were examined. The mean follow-up was of 24.29 ± 22.4 months. In the open repair group, data from 1055 procedures were collected; the minority of these patients were females (19%) with a mean age of 42.17 ± 3.6 years and a mean BMI of 26.08 ± 1.8 kg/m2. In the MIS group, data from 1168 procedures were collected. Again, the minority of these patients were females (26%), the mean age was 41.16 ± 2.8 years and the mean BMI 26.15 ± 1.7 kg/m2. Among the two groups an optimal comparability with regard to patients’ age (P = 0.9) and BMI (P = 0.9) was present. Demographic data are reported in Table 1.
Outcomes of interest
The open group reported a lower value of post-operative palpable knot at last follow-up (OR: 0.10; 95% CI 0.01–0.81; P < 0.0001) and a lower rate of sural nerve palsy (OR: 0.45; 95% CI 0.28–0.74; P = 0.001). In the MIS group a shorter surgery duration (FE: 7.55; 95% CI 5.16–9.95; P < 0.0001) has been evidenced, a lower rate of post-operative wound necrosis (OR: 3.01; 95% CI 1.30–6.59; P = 0.006) and a reduced risk to develop scar tissue adhesions (OR: 4.10; 95% CI 2.13–7.88; P < 0.0001) were noted. Moreover, in the MIS group the lowest values of superficial (OR: 3.90; 95% CI 1.68–9.06; P = 0.002) and deep tissue infections (OR: 2.01; 95% CI 1.24–3.27; P = 005) were observed. Re-rupture rate has been equal among both groups without a significant difference (OR: 1.10; 95% CI 0.62–1.94; P = 0.75). An overview of the meta-analysis results is shown in Table 2.
Discussion
This meta-analysis conducted an updated comparison between open versus minimally-invasive surgery for acute Achilles tendon ruptures. According to the main findings, in the MIS technique a lower complication rate for Achilles tendon repair was observed. The re-rupture rate between both techniques showed no significant differences. The MIS cohort showed a noteworthy lower rate of post-operative wound necrosis and scar tissue adhesions, as well as a considerable reduction of superficial and deep tissue infection. In addition, the surgery duration was quicker in the MIS group. In favour of the open group, a slightly lower value of sural nerve palsy has been observed, along with a minimally reduced rate of post-operative palpable knot. Putting the results of this meta-analysis in a clinical context, MIS should be recommended as the surgical method of choice for acute Achilles tendon rupture. Furthermore, also conservative treatment is a considerable therapeutic option with only a slightly higher re-rupture rate in comparison to surgery, but less frequent complications compared to surgery [15]. Therefore, if surgical therapy is required it should aim to have a low rate of relevant complications.
Re-rupture
Although we were not evaluating PROMS we examined the re-rupture rate as one of the most important failures in Achilles tendon surgery, finding no significant differences between both groups, which is in line with previous meta-analyses [10,11,12, 45]. Keeping this in mind, discussions about the adequate surgical approach should therefore focus on reducing complications rather than differences in outcome. However, for clinical practice it should be considered that previous meta-analyses with small sample sizes reported a slightly better or equal subjective result in general outcome measures or the AOFAS score in favour of MIS [12, 45].
Sural nerve palsy, scar tissue adhesion and palpable knot
The present meta-analyses reveals, that sural nerve palsy might be still a considerable complication of MIS, whereas previous meta-analysis stated equal palsy rates for both approaches [10, 12, 45]. Initially, using the Ma and Griffith percutaneous technique a sural nerve palsy rate up to 60% has been reported, whereas the most recent RCT studying of Rozis et al. in 2018 reported a decreased rate of only 7% [12, 13]. However, it has to be emphasized that the present meta-analysis includes studies from the last two decades, while surgical techniques have been improved and several operation devices have been introduced during this time [12]. Therefore, in recent studies of Lacoste et al. using the Tenolig™ system and of Amlang et al. using the Dresden instrument none of the patients had a permanent sural nerve damage [9, 46]. For clinical practice it has to be considered that the risk of sural nerve palsy mainly depends on the surgeon’s skills. Traditionally, the open approach to the Achilles tendon is performed through a medial exposure to avoid affections to the sural nerve, allowing a good overview on the anatomical structures. However, tissue scarring and adhesions increase on the basis of exposure of the peritendineum leading to mild pain and discomfort. Contrary, the reduced exposure of the MIS makes the tendon repair more prone to nerve damage. Especially when the needles are pierced laterally into the proximal portion of the Achilles tendon, an increased risk of direct sural nerve injury or indirect irritation by sutures exists. However, in clinical practice there are surgical precautions to reduce the risk: usage of ultrasound guidance or tenoscopy as well as external rotation of the Achillon® suture device [1, 47].
Besides, lower sural nerve palsy rates, in the open group a decreased risk for palpable knots was observed. The clinical relevance of this outcome is fair, and it might show a reduced prevalence in the future thanks to modern knotless percutaneous techniques with suture anchoring in the calcaneus [48].
Wound necrosis, deep and superficial infections
The reduced risk of wound necrosis or tissue infections observed in the MIS group are clinically relevant, since being the most common reasons besides tendon re-rupture requiring revision surgery. Grassi et al. revealed that one wound infection could be avoided for every 10 minimally-invasive procedure performed instead of an open approach representing previous findings of higher infection rates and wound necrosis [12] Contrary to our findings, the meta-analyses of Li et al. and Yang et al. concluded that a reduced infection rate in favour of the minimally invasive approach only counts for superficial infections and not for deep infections [10, 11]. For clinical practice, Achilles tendon surgery should focus on a minimal wound area. Due to low skin perfusion over the Achilles tendon, there is a higher risk for wound necrosis followed by superficial tissue infections [49] even increased by means of individual risk factors such as smoking, vascular diseases or diabetes [50]. As a result perioperative prophylactic antibiotics do not reveal a significant reduction of infection prevalence [1, 51].
Operation time
Besides the lower rate of tissue infections and wound necrosis, MIS revealed a significant shorter operation time. However, analysing three studies offering suitable data, the average duration of both procedures was less than 60 min, assuming that adverse effects of general anaesthesia or tourniquet time most probably do not have that much impact on outcome. Additionally, the importance of short overall surgery duration reflects the need for higher cost-effectiveness, as the total estimated costs of open tendon repair comparison to a minimally-invasive repair excluding theatre time are nearly twice as high [36].
Strength, limitations and implications for future research
Point of strength of the present study is represented by the strict eligibility criteria and inclusion of only frequently reported findings along with the comprehensive nature of the literature search including observational studies and RCTs, so that the largest sample sizes compared to previous meta-analysis has been achieved [10, 12, 45]. Moreover, the adequate follow-up and the optimal baseline comparability represent a further important point of strength.
Nevertheless, caution should be taken with regard to the following limitations: According to inconsistent data of the underlying studies we were unable to evaluate outcomes according to subgroups like the location of tendon rupture. Only a few of the studies included classified the exact location of tendon rupture (insertion, mid-portion, musculotendinous transition) or the gap between the tendon stumps. Amlang et al. introduced an ultrasound based classification in 2011 making rupture classification also practicable in a MIS approach [52]. Consequently, we encourage future studies to classify the exact location of tendon rupture in order to achieve valuable information minimizing future failures and impaired functional outcome, potentially providing clear indications in favour of certain augmentation procedures. Moreover, most recently a knotless MIS procedure with calcaneal suture anchor fixation has been described, offering wider surgical use of MIS, not being limited to repair of mid-portion tendon ruptures [48].
With regard to subgroup analysis, pre-existing comorbidities like vascular diseases might have influenced the infection or necrosis rate, since in clinical practice they are already used as clear contraindication for open repair. To avoid bias, this data needs to be completely reported in future studies. According to the methodological quality assessment this study had a moderate level of quality, since there was a high risk of detection bias and a low rate of overall RCT studies (8/25). Moreover, this meta-analysis reported a considerable risk of bias in the given data due to various techniques and post-operative rehabilitation, suture materials and developing surgical procedures influencing outcome measures. In both approaches, there are numerous techniques using different suture types (Bunnell, Kessler, Krackow etc.), suture material (PDS®, Vicryl®, FiberWire® etc.), tendon augmentation and flap-down strategies (Lindholm, Bosworth, Lynn etc.). Based on this data recommending the superior technique is challenging and mainly based on the surgeon’s skill. According to biomechanical aspects, recent systematic reviews and meta-analyses showed improved outcomes for double or triple sutures and higher resistance for Krackow and Bunnell instead of Kessler suture techniques, without finding a difference between Achillon® versus Krackow techniques [53, 54]. Moreover, bioabsorbable sutures might cause less tissue irritation while maintaining sufficient strength capacity [1]. Additionally, early and prolonged functional rehabilitation and mobilisation is recommended with a lots of varieties as discussed by Yang et al. [1]. A further limitation is that, we did not include functional parameters such as the toe-rising test or calf circumference. However, it was not possible to examine persistent functional deficits like weakness or tendon elongation, due to missing data and/or consensus of a testing protocol of isokinetic muscle force evaluation.
Conclusion
Compared to the MIS technique, the open Achilles tendon reconstruction evidenced a slightly lower rate of sural nerve palsy and postoperative palpable knot, whereas in the MIS reconstruction group, a quicker surgery duration, a lower rate of post-operative wound necrosis, superficial and deep tissue infections as well as scar tissue adhesions was detected. No relevant discrepancies were detected among the two techniques in terms of post-operative re-rupture. Consequently, MIS should be used as the surgical technique of choice.
References
Yang X, Meng H, Quan Q, Peng J, Lu S, Wang A (2018) Management of acute Achilles tendon ruptures: a review. Bone Jt Res 7(10):561–569. https://doi.org/10.1302/2046-3758.710.BJR-2018-0004.R2
Wilkins R, Bisson LJ (2012) Operative versus nonoperative management of acute Achilles tendon ruptures: a quantitative systematic review of randomized controlled trials. Am J Sports Med 40(9):2154–2160. https://doi.org/10.1177/0363546512453293
Ma GW, Griffith TG (1977) Percutaneous repair of acute closed ruptured achilles tendon: a new technique. Clin Orthop Relat Res 128:247–255
Daghino W, Enrietti E, Sprio AE, di Prun NB, Berta GN, Masse A (2016) Subcutaneous Achilles tendon rupture: a comparison between open technique and mini-invasive tenorrhaphy with Achillon((R)) suture system. Injury 47(11):2591–2595. https://doi.org/10.1016/j.injury.2016.09.009
Assal M, Jung M, Stern R, Rippstein P, Delmi M, Hoffmeyer P (2002) Limited open repair of Achilles tendon ruptures: a technique with a new instrument and findings of a prospective multicenter study. J Bone Jt Surg Am 84(2):161–170
Kakiuchi M (1995) A combined open and percutaneous technique for repair of tendo Achillis. Comparison with open repair. J Bone Jt Surg Br 77(1):60–63
Gigante A, Moschini A, Verdenelli A, Del Torto M, Ulisse S, de Palma L (2008) Open versus percutaneous repair in the treatment of acute Achilles tendon rupture: a randomized prospective study. Knee Surg Sports Traumatol Arthrosc 16(2):204–209. https://doi.org/10.1007/s00167-007-0448-z
Hsu AR, Jones CP, Cohen BE, Davis WH, Ellington JK, Anderson RB (2015) Clinical outcomes and complications of percutaneous achilles repair system versus open technique for acute achilles tendon ruptures. Foot Ankl Int 36(11):1279–1286. https://doi.org/10.1177/1071100715589632
Amlang MH, Christiani P, Heinz P, Zwipp H (2006) The percutaneous suture of the Achilles tendon with the Dresden instrument. Oper Orthop Traumatol 18(4):287–299. https://doi.org/10.1007/s00064-006-1178-y
Li Q, Wang C, Huo Y, Jia Z, Wang X (2016) Minimally invasive versus open surgery for acute Achilles tendon rupture: a systematic review of overlapping meta-analyses. J Orthop Surg Res 11(1):65. https://doi.org/10.1186/s13018-016-0401-2
Yang B, Liu Y, Kan S, Zhang D, Xu H, Liu F, Ning G, Feng S (2017) Outcomes and complications of percutaneous versus open repair of acute Achilles tendon rupture: a meta-analysis. Int J Surg 40:178–186. https://doi.org/10.1016/j.ijsu.2017.03.021
Grassi A, Amendola A, Samuelsson K, Svantesson E, Romagnoli M, Bondi A, Mosca M, Zaffagnini S (2018) Minimally invasive versus open repair for acute Achilles tendon rupture: meta-analysis showing reduced complications, with similar outcomes, after minimally invasive surgery. J Bone Jt Surg Am 100(22):1969–1981. https://doi.org/10.2106/JBJS.17.01364
Rozis M, Benetos IS, Karampinas P, Polyzois V, Vlamis J, Pneumaticos SG (2018) Outcome of percutaneous fixation of acute achilles tendon ruptures. Foot Ankl Int 39(6):689–693. https://doi.org/10.1177/1071100718757971
Makulavicius A, Mazarevicius G, Klinga M, Urmanavicius M, Masionis P, Oliva XM, Uvarovas V, Porvaneckas N (2019) Outcomes of open "crown" type v. percutaneous Bunnell type repair of acute Achilles tendon ruptures. Randomized control study. Foot Ankl Surg. https://doi.org/10.1016/j.fas.2019.07.011
Ochen Y, Beks RB, van Heijl M, Hietbrink F, Leenen LPH, van der Velde D, Heng M, van der Meijden O, Groenwold RHH, Houwert RM (2019) Operative treatment versus nonoperative treatment of Achilles tendon ruptures: systematic review and meta-analysis. BMJ 364:k5120. https://doi.org/10.1136/bmj.k5120
Anglemyer A, Horvath HT, Bero L (2014) Healthcare outcomes assessed with observational study designs compared with those assessed in randomized trials. Cochrane Database Syst Rev 4:000034. https://doi.org/10.1002/14651858.MR000034.pub2
Concato J, Shah N, Horwitz RI (2000) Randomized, controlled trials, observational studies, and the hierarchy of research designs. N Engl J Med 342(25):1887–1892. https://doi.org/10.1056/NEJM200006223422507
Arditi C, Burnand B, Peytremann-Bridevaux I (2016) Adding non-randomised studies to a Cochrane review brings complementary information for healthcare stakeholders: an augmented systematic review and meta-analysis. BMC Health Serv Res 16(1):598. https://doi.org/10.1186/s12913-016-1816-5
Frieden TR (2017) Evidence for health decision making—beyond randomized. Controll Trials N Engl J Med 377(5):465–475. https://doi.org/10.1056/NEJMra1614394
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Howick JCI, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, Moschetti I, Phillips B, Thornton H, Goddard O, Hodgkinson M (2011) The 2011 oxford levels of evidence. Oxford centre for evidence-based medicine available at https://www.cebm.net/index.aspx?o=5653
Majewski M, Rickert M, Steinbruck K (2000) Achilles tendon rupture. A prospective study assessing various treatment possibilities. Orthopade 29(7):670–676
Lim J, Dalal R, Waseem M (2001) Percutaneous vs open repair of the ruptured Achilles tendon—prospective randomized controlled study. Foot Ankl Int 22(7):559–568. https://doi.org/10.1177/107110070102200705
Rebeccato A, Santini S, Salmaso G, Nogarin L (2001) Repair of the achilles tendon rupture: a functional comparison of three surgical techniques. J Foot Ankl Surg 40(4):188–194
Riedl S, Sandberger L, Nitschmann K, Meeder PJ (2002) Suture of fresh Achilles tendon rupture. Comparison of open with percutaneous suture technique. Chirurg 73(6):607–614
Haji A, Sahai A, Symes A, Vyas JK (2004) Percutaneous versus open tendo achillis repair. Foot Ankl Int 25(4):215–218. https://doi.org/10.1177/107110070402500404
Miller D, Waterston S, Reaper J, Barrass V, Maffulli N (2005) Conservative management, percutaneous or open repair of acute Achilles tendon rupture: a retrospective study. Scott Med J 50(4):160–165. https://doi.org/10.1177/003693300505000408
Cretnik A, Kosanovic M, Smrkolj V (2005) Percutaneous versus open repair of the ruptured Achilles tendon: a comparative study. Am J Sports Med 33(9):1369–1379. https://doi.org/10.1177/0363546504271501
Bhattacharyya M, Gerber B (2009) Mini-invasive surgical repair of the Achilles tendon–does it reduce post-operative morbidity? Int Orthop 33(1):151–156. https://doi.org/10.1007/s00264-008-0564-5
Ebinesan AD, Sarai BS, Walley GD, Maffulli N (2008) Conservative, open or percutaneous repair for acute rupture of the Achilles tendon. Disabil Rehabil 30(20–22):1721–1725. https://doi.org/10.1080/09638280701786815
Avina Valencia JA, Guillen Alcala MA (2009) Repair of acute Achilles tendon rupture. Comparative study of two surgical techniques. Acta Ortop Mex 23(3):125–129
Aktas S, Kocaoglu B (2009) Open versus minimal invasive repair with Achillon device. Foot Ankl Int 30(5):391–397. https://doi.org/10.3113/FAI.2009.0391
Chan AP, Chan YY, Fong DT, Wong PY, Lam HY, Lo CK, Yung PS, Fung KY, Chan KM (2011) Clinical and biomechanical outcome of minimal invasive and open repair of the Achilles tendon. Sports Med Arthrosc Rehabil Ther Technol 3(1):32. https://doi.org/10.1186/1758-2555-3-32
Henriquez H, Munoz R, Carcuro G, Bastias C (2012) Is percutaneous repair better than open repair in acute Achilles tendon rupture? Clin Orthop Relat Res 470(4):998–1003. https://doi.org/10.1007/s11999-011-1830-1
Grubor P, Grubor M (2012) Treatment of Achilles tendon rupture using different methods. Vojnosanit Pregl 69(8):663–668
Carmont MR, Heaver C, Pradhan A, Mei-Dan O, Gravare Silbernagel K (2013) Surgical repair of the ruptured Achilles tendon: the cost-effectiveness of open versus percutaneous repair. Knee Surg Sports Traumatol Arthrosc 21(6):1361–1368. https://doi.org/10.1007/s00167-013-2423-1
Karabinas PK, Benetos IS, Lampropoulou-Adamidou K, Romoudis P, Mavrogenis AF, Vlamis J (2014) Percutaneous versus open repair of acute Achilles tendon ruptures. Eur J Orthop Surg Traumatol 24(4):607–613. https://doi.org/10.1007/s00590-013-1350-7
Kolodziej L, Bohatyrewicz A, Kromuszczynska J, Jezierski J, Biedron M (2013) Efficacy and complications of open and minimally invasive surgery in acute Achilles tendon rupture: a prospective randomised clinical study–preliminary report. Int Orthop 37(4):625–629. https://doi.org/10.1007/s00264-012-1737-9
Jallageas R, Bordes J, Daviet JC, Mabit C, Coste C (2013) Evaluation of surgical treatment for ruptured Achilles tendon in 31 athletes. Orthop Traumatol Surg Res 99(5):577–584. https://doi.org/10.1016/j.otsr.2013.03.024
Rosso C, Buckland DM, Polzer C, Sadoghi P, Schuh R, Weisskopf L, Vavken P, Valderrabano V (2015) Long-term biomechanical outcomes after Achilles tendon ruptures. Knee Surg Sports Traumatol Arthrosc 23(3):890–898. https://doi.org/10.1007/s00167-013-2726-2
Obada B, Serban AO (2014) Achilles tendon ruptures: comparison between the clinical results of classical versus mini-invasive or percutaneous surgical treatment. ARS Med Tomitana 78(3):135–138
Lonzaric D, Kruscic A, Dinevski D, Povalej Brzan P, Jesensek Papez B (2017) Primary surgical repair of acute Achilles tendon rupture: comparative results of three surgical techniques. Wien Klin Wochenschr 129(5–6):176–185. https://doi.org/10.1007/s00508-016-1158-7
Araujo PJ, Moreno MV, de Souza GJ, Gomes MJ, Vieira TE, Jalil VS (2018) Comparison between the open and minimally invasive repair technique in acute Achilles tendon injuries. Sci J Foot Ankl 4(12):265–270. https://doi.org/10.30795/scijfootankle.2018.v12.789
Baumfeld D, Baumfeld T, Spiezia F, Nery C, Zambelli R, Maffulli N (2019) Isokinetic functional outcomes of open versus percutaneous repair following Achilles tendon tears. Foot Ankl Surg 25(4):503–506. https://doi.org/10.1016/j.fas.2018.03.003
Alcelik I, Diana G, Craig A, Loster N, Budgen A (2017) Minimally invasive versus open surgery for acute achilles tendon ruptures a systematic review and meta-analysis. Acta Orthop Belg 83(3):387–395
Lacoste S, Feron JM, Cherrier B (2014) Percutaneous Tenolig((R)) repair under intra-operative ultrasonography guidance in acute Achilles tendon rupture. Orthop Traumatol Surg Res 100(8):925–930. https://doi.org/10.1016/j.otsr.2014.09.018
Aibinder WR, Patel A, Arnouk J, El-Gendi H, Korshunov Y, Mitgang J, Uribe J (2013) The rate of sural nerve violation using the Achillon device: a cadaveric study. Foot Ankl Int 34(6):870–875. https://doi.org/10.1177/1071100712473097
Liechti DJ, Moatshe G, Backus JD, Marchetti DC, Clanton TO (2018) A percutaneous knotless technique for acute achilles tendon ruptures. Arthrosc Tech 7(2):e171–e178. https://doi.org/10.1016/j.eats.2017.08.065
Poynton AR, O'Rourke K (2001) An analysis of skin perfusion over the achilles tendon in varying degrees of plantarflexion. Foot Ankl Int 22(7):572–574. https://doi.org/10.1177/107110070102200707
Saxena A, Maffulli N, Nguyen A, Li A (2008) Wound complications from surgeries pertaining to the Achilles tendon: an analysis of 219 surgeries. J Am Podiatr Med Assoc 98(2):95–101
Marican MM, Fook-Chong SM, Rikhraj IS (2015) Incidence of postoperative wound infections after open tendo Achilles repairs. Singap Med J 56(10):549–554. https://doi.org/10.11622/smedj.2015150
Amlang MH, Zwipp H, Friedrich A, Peaden A, Bunk A, Rammelt S (2011) Ultrasonographic classification of Achilles tendon ruptures as a rationale for individual treatment selection. ISRN Orthop 2011:869703. https://doi.org/10.5402/2011/869703
Yammine K, Assi C (2017) Efficacy of repair techniques of the Achilles tendon: a meta-analysis of human cadaveric biomechanical studies. Foot (Edinb) 30:13–20. https://doi.org/10.1016/j.foot.2016.09.006
Sadoghi P, Rosso C, Valderrabano V, Leithner A, Vavken P (2012) Initial Achilles tendon repair strength–synthesized biomechanical data from 196 cadaver repairs. Int Orthop 36(9):1947–1951. https://doi.org/10.1007/s00264-012-1533-6
Funding
No external source of funding was used.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gatz, M., Driessen, A., Eschweiler, J. et al. Open versus minimally-invasive surgery for Achilles tendon rupture: a meta-analysis study. Arch Orthop Trauma Surg 141, 383–401 (2021). https://doi.org/10.1007/s00402-020-03437-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03437-z