Abstract
Purpose
Theoretically, proprioceptive acuity could decrease in patients with knee osteoarthritis. However, there have been conflicting results in terms of proprioceptive deficit in osteoarthritic knees. The purpose of this systematic review and meta-analysis was to compare knee proprioception between osteoarthritic and healthy control knees.
Methods
Studies comparing proprioception in osteoarthritic and healthy knees of age-matched control group using thresholds to detect passive motion (TTDPM) or joint position sense (JPS) tests were identified. JPS was assessed by measuring the reproduction of passive positioning (RPP) or active positioning (RAP) of the knees.
Results
Seventeen studies were finally included in this meta-analysis. The pooled results of the analyses of the TTDPM for both 30° and 45° knee flexion showed that the mean angle of error was 0.83° greater (95% confidence interval: 0.44 to 1.23°; p < 0.001) in the osteoarthritic knees than in control knees. The pooled data of the RAP and RPP also showed that the mean angle of error was 1.89° greater in the osteoarthritic knees than in the control group. The mean difference in the angle of error between the osteoarthritic knees and control group was 1.06° greater in the JPS test than in the TTDPM (p < 0.001).
Conclusion
The knee proprioceptive acuity of the patients with knee osteoarthritis was poorer than that of the patients with unaffected knees in the age-matched control group both in terms of the TTDPM and JPS; clinical relevance of these deficits needs to be clarified in further studies.
Level of evidence
Meta-analysis, Level II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Knee joint osteoarthritis could destroy the joint articular cartilage and change the soft tissue structures around the knee joint, including the joint capsule [45], muscles, and tendons, where the mechanoreceptors are located [2, 16, 46]. Mechanoreceptors are well known for their involvement in knee joint proprioception, which encompasses the sense of joint position and sense of joint motion [39], because these senses are particularly derived from afferent neural inputs arising from the mechanoreceptor in the joints, muscles, tendon, and associated tissues. Theoretically, proprioceptive acuity could decrease in patients with knee osteoarthritis [40, 44, 51]. However, previous studies [22, 31, 37] have yielded conflicting results regarding whether a proprioceptive deficit occurs in osteoarthritic knees, with some studies finding a significant deficit, but others reported similar proprioception in osteoarthritic knees compared with unaffected knees of an age-matched control group. In addition, the lack of a standardized method of measuring the proprioceptive acuity has made it difficult to conclude on the proprioceptive deficit of patients with osteoarthritic knees by pooling the data of previous studies. Further, it is difficult to compare the results obtained in various studies directly, although the threshold to detect passive motion (TTDPM) has been widely used as a measure of sense of joint movement, and reproduction of active joint repositioning (RAP) and reproduction of passive joint repositioning (RPP) have been frequently used to test joint position sense (JPS) [3, 11, 28, 30, 31, 37, 51].
Therefore, the purpose of this study was to determine whether the proprioceptive acuity is actually less in osteoarthritic knees compared with that in unaffected knees of the age-matched healthy control group. In addition, this study evaluated whether the proprioceptive deficit would vary on the basis of the method of proprioception measurement, such as the TTDPM measured between 30° and 45° knee flexion and the JPS test conducted between passive and active repositioning. It was hypothesized that the proprioception in patients with osteoarthritic knees would decrease compared with that in the patients with unaffected knees in the control group with a similar age, regardless of the method used to measure knee proprioception.
Materials and methods
Literature search
The study design was based on the Cochrane Review Methods. We conducted this study according to the guidelines of the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses, S1 PRISMA Checklist) statement. The study protocol was published online at the PROSPERO International Prospective Register of Systematic Reviews (https://www.crd.york.ac.uk/PROSPERO) under registration number CRD42018086249. Multiple comprehensive literature databases, including MEDLINE® (January 1, 1976–June 30, 2019), EMBASE® (January 1, 1976–June 30, 2019), and Cochrane Library (January 1, 1976–June 30, 2019), were searched for studies that compared the proprioception using the TTDPM and JPS test between patients with knee osteoarthritis and control groups without knee pain. There were no restrictions on the year of publication. The search terms used were the MeSH terms “knee”, “osteoarthritis”, and “proprioception”, and the individual corresponding free terms. Relevant articles and their bibliographies were searched manually following the initial electronic search.
Study selection
Two reviewers evaluated the titles and abstracts of the obtained articles and selected relevant articles for full review. If the abstract did not provide sufficient data to make a decision, the full text of the article was reviewed [20, 47]. Studies were included in the meta-analysis if (1) they dealt with patients with knee osteoarthritis; (2) they directly compared proprioception between osteoarthritic knees (diagnosed by American Rheumatism Association (ACR) criteria [1] for knee osteoarthritis) or knees with joint pain of Kellgren–Lawrence grade [26, 38] (K–L) grade 2 or higher and knees from a healthy age-matched control group (defined as healthy subjects with no history of pain in the knee joint and K–L grade 0 or 1); (3) they regarded comparisons of the TTDPM and/or JPS, and (4) the sample number, means and standard deviations were fully reported in their study.
JPS measurements are composed by two different methods—reproduction of passive positioning (RPP) and active repositioning (RAP). The RPP is measured using an electrogoniometer. The subject’s knee was placed at predetermined angle. The subject was ordered to remember that target position. The limb was passively moved to the predetermined angle. The subject was then instructed to stop the assessor when the limb returned to targeted position. On the other hand, in the RAP measurement, the knee joint was passively placed to predetermined angle by the examiner instead of by the electrogoniometer, and then the subject was ordered to reproduce predetermined angle actively. The JPS was quantified by angle difference between targeted and indicated by the subject. TTDPM is angle between starting position and halted position which the subject feels motion of their knee, measured digitally by electrogoniometer.
Data extraction
Two reviewers independently recorded data from each article using a predefined data extraction form. If there were discrepancies between the two reviewers, they were solved via a discussion. The variables extracted included the following: (1) mean and standard deviations of the TTDPM, reproduction angle error of the knee joint compared with that of the predetermined knee position in patients with osteoarthritic knees and control groups without radiographic knee osteoarthritis; (2) demographic data including age and sex and sample size of each osteoarthritis and control group; (3) knee joint angles and angular velocity when obtaining the TTDPM and predetermined target angle in the reproduction angle of the knee joint; (4) study type (e.g., prospective or retrospective comparison studies).
Assessment of methodological quality
Two reviewers independently assessed the methodological quality of each study using the Newcastle–Ottawa Assessment Scale [53], which is designed to appraise the quality of non-randomized studies. It consisted of three domains: selection, comparability, and outcome. For the selection (four numbered items) and outcome (three numbered items) domains, each assessed study could be given a maximum of one star for each numbered item. For the comparability (one numbered item) domain, a maximum of two stars could be given. A maximum of nine stars can be awarded. Studies with scores of ≥ 7, 5–7, 3–5, and 0–2 were considered to have good, fair, poor-fair, and poor qualities, respectively. Any unresolved disagreements between the reviewers were resolved via a consensus.
Statistical analysis
Statistical analysis of the TTDPM and JPS measurements between the osteoarthritic knees and control knees was performed. To pool primary outcomes of included studies, random-effects meta-analyses were used by estimating the weighted mean differences and 95% confidence intervals (CIs) in the JPS and TTDPM between two groups. The I2 statistic was calculated to present heterogeneity by estimating the proportion of between-study inconsistencies. All statistical analyses were performed using the RevMan version 5.2 and Stata/MP 13.0. The risks of bias (low, high, or unclear) were independently assessed by two investigators. Publication bias was also assessed using funnel plots and the Egger’s test. To test for the potential bias effect of demographic data, meta-regression analyses were performed for evaluating the affection of different demographic data (age and sex) of including studies on the differences of TTDPM and JPS.
Results
Identification of studies
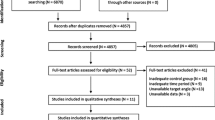
Figure 1 shows the details of the study identification, inclusion, and exclusion. The electronic search yielded 178 studies in the PubMed (MEDLINE), 327 in the EMBASE, and 61 in the Cochrane Library databases. Three additional publications were identified via manual searching. After removing 196 duplicates, 373 studies remained: of these, 340 were excluded upon reading the abstracts and full-text articles, and an additional 16 studies were excluded, since they did not have usable information which were only measured proprioception other than the TTDPM or JPS, or did not compare the proprioception of the age-matched control group. After applying these criteria, 17 studies were finally included in this meta-analysis.
Study characteristics and patient populations
The 17 included studies evaluated 327 patients with knee osteoarthritis and 333 control subjects with unaffected knees who underwent proprioception measurement using the TTDPM or JPS test. All 17 included studies were prospective comparative studies. Seven studies measured the TTDPM, and 10 measured the JPS. Of the seven studies that measured the TTDPM, two measured the TTDPM at a knee flexion of 30°, and five measured the TTDPM at a knee flexion of 45°. Of the ten studies that measured the JPS, eight measured the reproduction of active positioning (RAP), and two measured the reproduction of passive positioning (RPP) (Table 1).
Quality appraisal and publication bias
Of the 17 studies, eight were found to be of a good quality, with five having eight stars and three having seven stars. The remaining nine studies were of a fair quality, with seven having six stars and two having five stars (Table 1). Publication bias was analyzed by assessing the JPS because it was the only parameter that was evaluated in more than ten studies. Except for two studies that were skewed to the right, the funnel plots showed that the weighted mean differences in the angle of error in the JPS between the osteoarthritic and unaffected knees were relatively symmetric, indicating a lack of publication bias (Fig. 2). The Egger’s test also showed no significant publication biases in the angle of error in the JPS (p = 0.561).
Funnel plot showing the relatively symmetric mean differences in the mean angle of error in the joint position sense test between the osteoarthritic and unaffected knees. Eight of the ten included studies fell within or around the 95% confidence interval lines; the other two studies deviated to the right. WMD weighted mean difference
TTDPM
Of the 17 studies, seven compared the TTDPM between the patients with knee osteoarthritis and unaffected control groups with a similar age. The analysis of the subjects who underwent the TTDPM test at 30° knee flexion showed that the mean angle of error was 0.83° greater (95% CI 0.36°–1.30°; p < 0.001) in the osteoarthritic knees than in control knees. Similar results were observed in the subjects who underwent the TTDPM test at 45° knee flexion, with the mean angle of error being 0.89° greater (95% CI 0.33°–1.44°; p = 0.002) in the osteoarthritic knees than in the control group. However, the pooled mean difference in the angle of error between the knees at 30° and 45° knee flexion was 0.06°, which was not statistically significant (p = 0.878). The pooled results of both TTDPM test at 30° and 45° knee flexion analyses also showed that the mean angle of error was 0.83° greater (95% CI 0.44°–1.23°; p < 0.001) in the osteoarthritic knees than in control knees (Fig. 3).
Forest plot showing the mean differences of the threshold to detect passive motion (TTDPM) between the osteoarthritic and unaffected knees. The analysis of the TTDPM test at 30° and 45° knee flexion shows that the mean angles of error are significantly 0.83° and 0.89° greater in the osteoarthritic knees than in the unaffected knees. The pooled results of the TTDPM both in 30° and in 45° of knee flexion also show a 0.83° greater mean angle of error in the osteoarthritic knees than in the unaffected knees. (The values to the right of point “0” mean the measure is worse in people with knee osteoarthritis than in age-matched controls.). WMD weighted mean difference, CI confidence interval
JPS
Of the 17 studies, 10 compared the JPS between the osteoarthritic knees and unaffected knees of control group. The pooled data of the 306 osteoarthritic knees and 253 unaffected knees, which were examined by the reproduction of the targeted knee position tests showed that the pooled mean difference in the mean angle of error was 1.89° greater (95% CI 1.09°–2.70°; p < 0.001) in the osteoarthritic knees than in the unaffected knee of healthy control group. The analysis of the subjects who underwent RAP tests demonstrated that the pooled mean difference in the mean angle of error was 2.04° greater (95% CI 1.11°–2.97°; p < 0.001) in the osteoarthritic knees than in the unaffected knee of healthy control group, indicating that the osteoarthritic knees had a poor JPS than unaffected knee of healthy control group. Similarly, the analysis of the subjects who underwent RPP tests showed that the mean angle of error was 1.54° greater (95% CI 0.82°–2.26°; p < 0.001) in the osteoarthritic knees than in the unaffected knees of healthy control group (Fig. 4). However, the mean difference in the angle of error of 0.5° between the RAP and RPP tests did not reach a statistical significance (p = 0.408).
Forest plot showing the mean differences in the joint position sense between the osteoarthritic and unaffected knees. The analysis of the reproduction of active (RAP) and passive (RPP) positioning of the targeted angle demonstrates that the mean angles of error are significantly 2.04° and 1.54° greater in the osteoarthritic knees than in the unaffected knees. The pooled data of the RAP and RPP also show that the osteoarthritic knees had a 1.89° greater mean angle of error than the unaffected knees. (The values to the right of point “0” mean the measure is worse in people with knee osteoarthritis than in age-matched controls.). WMD weighted mean difference; CI confidence interval
TTDPM vs. JPS and meta-regression analyses
A comparison of the results of the TTDPM and JPS showed that the mean difference in the angle of error between the osteoarthritic knees and unaffected knees of healthy control group was 1.06° greater (95% CI 0.68°–0.74°; p < 0.001) in the JPS test than in the TTDPM test.
The results of the meta-regression analyses are reported in Table 2. The age and sex differences between the patients with knee osteoarthritis and control groups with unaffected knees were not significantly associated with the differences in the mean angle of error both in the TTDPM and JPS tests. This finding indicated that the results of the current study were not biased by the differences in the demographic characteristics of the patients and control groups.
Discussion
The most important findings of this study were that proprioception was lower in the osteoarthritic knees than in the unaffected knees of the age-matched control group both in the TTDPM and JPS tests and that the mean angle of error was greater in the JPS test than in the TTDPM test.
Proprioception is the sense of movement and position of the body and it is achieved by peripheral sensory input including changes in muscle length and tension, joint angle, and stretch of skin. These sensory inputs are derived from a number of sources including muscle spindles in skeletal muscle, stretch-sensitive receptors in tendons (Golgi tendon organ), and motion-sensitive receptors in ligaments and joint capsules (Ruffini receptor and Pacinian corpuscle) [9]. In clinical studies, knee joint proprioception is measured by two different methods—joint movement (kinesthesia) is tested by TTDPM and joint position is tested by JPS [27]. The results of the current study showed decreased proprioception not only in the joint movement sense but also in the joint position sense. It is possible that a reduction in proprioception in patients with knee osteoarthritis could be the result of a local effect of knee osteoarthritis or of the general development or progression of the osteoarthritis and muscle weakness [15, 28]. In terms of the local effect of knee osteoarthritis, the morphologic change in the knee joint resulting from knee osteoarthritis, including osteophyte, articular cartilage breakage, and increased joint effusion, could damage the mechanoreceptors in the articular cartilage and joint capsule. Beyond the intraarticular destruction, knee osteoarthritis could destroy or disturb the extraarticular soft tissues around the knee joint, therefore altering the function of the mechanoreceptors in the joint capsule, ligament, muscle, and tendinous portion surrounding the knee joint. Quadriceps muscle weakness or atrophy is well known for its correlation with progression of knee osteoarthritis. Previous studies showed a significant association between impaired motion sense and muscle weakness and insisted that muscle weakness or atrophy might decrease muscle spindle sensitivity [24, 25, 52]. These widespread damages in the mechanoreceptors of the intraarticular and extraarticular structures are large enough to be detected by proprioception measurement tools, such as the TTDPM and JPS tests [41]. Conversely, decreased proprioception by osteoarthritis could induce the progression of osteoarthritis [40]. Disruption of the afferent component of protective neuromuscular reflexes due to impaired proprioception may lead to poor spatial and temporal coordination of position sense, decreased muscle activity, and poor coordination of the quadriceps and hamstring [28]. This situation could subsequently increase loads on the knee joint owing to poor load distributions, which resulted from an increased joint laxity by poor muscular control and activity, thus resulting in a greater exposure of the knee joint to wear and tear [31]. In addition, a recent study [31] showing systemic proprioceptive deficits of elbow as well as knee joints suggest that proprioceptive deficit of the knee joint could be a cause of osteoarthritis. Although the results of the current study could not clearly demonstrate such a causal relationship, we believe that impaired proprioception could be both a cause and a result of knee osteoarthritis, because either of these possibilities alone is insufficient to explain the presence of impaired proprioception in patients with knee osteoarthritis. Therefore, it is also probable that these two pathways may create the “self-perpetuating vicious cycle” of knee osteoarthritis progression.
Many studies had made an effort to prove which factors are the prognostic factors for the progression of knee osteoarthritis. Obesity, sex (female), varus malalignment, age, former knee injury, high serum levels of hyaluronic acid, and TNF-α are proven potential factors for the progression of knee arthritis [5, 14]. Low quadriceps muscle strength is also well-known factor which is associated with the progression of knee osteoarthritis; however, the causal relationship had not been clarified [4, 29, 48]. We think the decrement of proprioceptive function might be one of causal relationship between knee osteoarthritis and quadriceps strength. When the patients had advanced osteoarthritis with uncontrolled pain, total knee arthroplasty is considered as the gold standard [38]. It is still controversial that arthroplasty yields better proprioception; however, optimal collaboration between surgery and subsequent rehabilitation might guarantee the good outcomes in terms of patients’ function [8, 12, 43].
In this study, the decrement of proprioception was greater in the JPS test (reproduction of angle) than in the joint motion sense (TTDPM) test. The difference in the decrement between the JPS and TTDPM tests could be explained in part by the fact that these two tests may measure different components of proprioception. Kinesthesia is the dynamic phase of proprioception and is, therefore, mainly regulated by rapid adapting mechanoreceptors (Pacinian corpuscles). Joint position is the static phase of proprioception and is chiefly controlled by slow adapting mechanoreceptors, such as Golgi tendon organs or Ruffini receptors [35]. In addition, the TTDPM test maximally stimulates the articular mechanoreceptors with minimal stimulation of the muscle spindles, whereas the JPS test stimulates both receptors. The insensitivity to rapid adapting mechanoreceptors and lack of reflection for mechanoreceptors in the muscle spindles in the TTDPM test could underestimate the actual decrement in the proprioception in osteoarthritic knee joints. Another possible cause of the greater decrement in the JPS test than in the TTDPM test may be the higher degree of measurement error in the JPS test. While both the JPS and TTDPM tests require the participants’ concentration abilities, only the JPS test is dependent on the participants’ memory during the test. Therefore, the reliability of the JPS test decreases not only because of one or two lapses in concentration but also because of a memory bias during the test. This might also explain the greater reduction in the JPS test than in the TTDPM test in the osteoarthritic knees [31].
Previous studies using patient-reported questionnaires demonstrated that proprioceptive deficit of the knee joint was associated with functional disability in terms of walking speed [32, 36, 42]. One report [10] suggested that a greater than 5° reduction in proprioception may have clinically significant impacts on osteoarthritic knees, but presented no evidence to support this assertion. To date, no consensus has been reached on how much reduction of proprioception in the TTDPM and JPS tests is required to give rise to clinically relevant changes in the functional ability of patients with knee osteoarthritis. The results of our study, showing a 0.83° deficit on the TTDPM test and a 1.89° deficit on the JPS test, may be insufficient to cause observable changes in functional ability. However, the deficits observed in our study were considerably greater than the range of measurement error of previous studies (0.03°–0.25°), suggesting that they have clinical relevance [7]. Also, given that the proprioception test was conducted on a non-weight bearing condition and a relatively lower angular velocity of 0.2–2°/s, which could not reflect the daily living activities of patients, it is possible that with the limb moving at great velocities and subjected to high forces in daily living, these low values take on a greater clinical significance than what was first thought [10]. In addition, a previous study showed that the mean side-to-side differences in healthy subjects were only 0.1° on both TTDPM and JPS measurements [18], thus also indicating that the less than 2° differences observed in our study may be underestimations of the proprioceptive deficits of the osteoarthritic knees. Further, considering that the proprioceptive deficit of patients with anterior cruciate ligament tear was not good in a recent meta-analysis [27], as determined by both TTDPM (0.23°) and JPS (0.94°), the proprioceptive deficit from 1° to 2° in the osteoarthritic knees in our study was relatively of a large magnitude, thus supporting the potential clinical relevance of these minimal proprioceptive deficits for the function of osteoarthritic knees. To prevent potential functional disability, early intervention, including muscle strengthening exercises, sensorimotor training or knee bandaging might be helpful to improve proprioceptive accuracy in patients with knee osteoarthritis [13, 25, 49, 50].
There were several limitations that should be considered in this meta-analysis. The heterogeneity of the demographic data among the included studies, such as age and sex distribution, could cause confounding effects on the results of this meta-analysis. However, the meta-regression analysis showed that age and sex were not significantly associated with the proprioceptive deficit in both the TTDPM and JPS tests in the osteoarthritic knees. In addition, we also could not exclude other potential confounders, such as habitual physical activity, concomitant medication, contralateral knee status [31], and prior medical or surgical conditions. These factors could have influenced the proprioception accuracy. Moreover, enrolled studies defined osteoarthritis using ACR criteria or K–L grade 2 or higher; therefore, it is hard to find the relationship between severity of osteoarthritis and decrement of proprioception. Another limitation was that the meta-analysis is based on a random effects analysis. In contrast to a fixed effects analysis, which can be used to estimate a common difference, a random effects analysis estimates an average difference, and the variability of this may have clinical implications. However, a random effects analysis was more adequate than a fixed effect model for pooling the data in this study because our results showed substantial heterogeneity (I2 > 50%). At last, the independent librarian who could supply more reliable data collection was not involved in the current study. It might be one of our limitations.
Conclusions
In conclusion, the knee proprioceptive acuity of patients with knee osteoarthritis was poorer than that of patients with unaffected knees in the age-matched control group both in terms of the TTDPM and JPS. Further evaluation is needed to determine the clinical relevance of these deficits.
References
Altman R, Asch E, Bloch D et al (1986) Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheumat 29(8):1039–1049
Araujo IL, Castro MC, Daltro C, Matos MA (2016) Quality of life and functional independence in patients with osteoarthritis of the knee. Knee Surg Relat Res 28(3):219–224
Baert IA, Mahmoudian A, Nieuwenhuys A et al (2013) Proprioceptive accuracy in women with early and established knee osteoarthritis and its relation to functional ability, postural control, and muscle strength. Clin Rheumatol 32(9):1365–1374
Baert IA, Staes F, Truijen S et al (2014) Weak associations between structural changes on MRI and symptoms, function and muscle strength in relation to knee osteoarthritis. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA 22(9):2013–2025
Bastick AN, Belo JN, Runhaar J, Bierma-Zeinstra SM (2015) What are the prognostic factors for radiographic progression of knee osteoarthritis? A meta-analysis. Clin Orthop Relat Res 473(9):2969–2989
Bayramoglu M, Toprak R, Sozay S (2007) Effects of osteoarthritis and fatigue on proprioception of the knee joint. Arch Phys Med Rehabil 88(3):346–350
Boerboom AL, Huizinga MR, Kaan WA et al (2008) Validation of a method to measure the proprioception of the knee. Gait Posture 28(4):610–614
Bragonzoni L, Rovini E, Barone G, Cavallo F, Zaffagnini S, Benedetti MG (2019) How proprioception changes before and after total knee arthroplasty: a systematic review. Gait Posture 72:1–11
Cabuk H, Kusku Cabuk F, Tekin AC, Dedeoglu SS, Cakar M, Buyukkurt CD (2017) Lower numbers of mechanoreceptors in the posterior cruciate ligament and anterior capsule of the osteoarthritic knees. Knee SURG SPORTS TRAUMATOL ARTHROSC 25(10):3146–3154
Callaghan MJ, Selfe J, Bagley PJ, Oldham JA (2002) The effects of patellar taping on knee joint proprioception. J Athletic Train 37(1):19–24
Cammarata ML, Dhaher YY (2012) Associations between frontal plane joint stiffness and proprioceptive acuity in knee osteoarthritis. Arthritis care & research 64(5):735–743
Chung JY, Min BH (2013) Is bicompartmental knee arthroplasty more favourable to knee muscle strength and physical performance compared to total knee arthroplasty? Knee Surg Sports Traumatol Arthros 21(11):2532–2541
Collins AT, Blackburn JT, Olcott CW et al (2011) Stochastic resonance electrical stimulation to improve proprioception in knee osteoarthritis. Knee 18(5):317–322
Correa-Valderrama A, Stangl-Herrera W, Echeverry-Velez A, Cantor E, Ron-Translateur T, Palacio-Villegas JC (2019) Relationship between Body Mass Index and Complications during the First 45 Days after Primary Total Hip and Knee Replacement: A Single-Center Study from South America. Clin Orthop Surg 11(2):159–163
Culvenor AG, Segal NA, Guermazi A et al (2018) The sex-specific influence of quadriceps weakness on worsening patellofemoral and tibiofemoral cartilage damage: the MOST Study. Arthritis Care Res 20:20
Felson DT, Gross KD, Nevitt MC et al (2009) The effects of impaired joint position sense on the development and progression of pain and structural damage in knee osteoarthritis. Arthritis Rheum 61(8):1070–1076
Garsden LR, Bullock-Saxton JE (1999) Joint reposition sense in subjects with unilateral osteoarthritis of the knee. Clin Rehabil 13(2):148–155
Gokeler A, Benjaminse A, Hewett TE et al (2012) Proprioceptive deficits after ACL injury: are they clinically relevant? Br J Sports Med 46(3):180–192
Hall MC, Mockett SP, Doherty M (2006) Relative impact of radiographic osteoarthritis and pain on quadriceps strength, proprioception, static postural sway and lower limb function. Ann Rheum Dis 65(7):865–870
Han JH, Bae JH, Nha KW et al (2019) Arthroscopic treatment of popliteal cysts with and without cystectomy: a systematic review and meta-analysis. Knee Surg Relat Rese 31(2):103–112
Hassan BS, Mockett S, Doherty M (2001) Static postural sway, proprioception, and maximal voluntary quadriceps contraction in patients with knee osteoarthritis and normal control subjects. Ann Rheum Dis 60(6):612–618
Hewitt BA, Refshauge KM, Kilbreath SL (2002) Kinesthesia at the knee: the effect of osteoarthritis and bandage application. Arthritis Rheum 47(5):479–483
Hortobagyi T, Garry J, Holbert D, Devita P (2004) Aberrations in the control of quadriceps muscle force in patients with knee osteoarthritis. Arthritis Rheum 51(4):562–569
Hurley MV, Scott DL, Rees J, Newham DJ (1997) Sensorimotor changes and functional performance in patients with knee osteoarthritis. Ann Rheum Dis 56(11):641–648
Jerosch J, Schmidt K, Prymka M (1997) Modification of proprioceptive ability of knee joints with primary gonarthrosis. Der Unfallchirurg 100(3):219–224
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Kim HJ, Lee JH, Lee DH (2017) Proprioception in patients with anterior cruciate ligament tears: a meta-analysis comparing injured and uninjured limbs. Am J Sports Med 45(12):2916–2922
Knoop J, Steultjens MP, van der Leeden M et al (2011) Proprioception in knee osteoarthritis: a narrative review. Osteoarthrit Cartil 19(4):381–388
Koca I, Boyaci A, Tutoglu A, Boyaci N, Ozkur A (2014) The relationship between quadriceps thickness, radiological staging, and clinical parameters in knee osteoarthritis. J Phys Ther Sci 26(6):931–936
Koralewicz LM, Engh GA (2000) Comparison of proprioception in arthritic and age-matched normal knees. J Bone Jt Surg 82-a(11):1582–1588
Lund H, Juul-Kristensen B, Hansen K et al (2008) Movement detection impaired in patients with knee osteoarthritis compared to healthy controls: a cross-sectional case–control study. J Musculoskelet Neuronal Interact 8(4):391–400
Marks R (1994) Correlations between measurements of the sense of knee position and the severity of joint lesions in knee osteoarthritis. Revue Rhumat (Ed. française: 1993) 61(6):423–430
Marks R, Quinney HA, Wessel J (1993) Proprioceptive sensibility in women with normal and osteoarthritic knee joints. Clin Rheumatol 12(2):170–175
Mohammadi F, Taghizadeh S, Ghaffarinejad F, Khorrami M, Sobhani S (2008) Proprioception, dynamic balance and maximal quadriceps strength in females with knee osteoarthritis and normal control subjects. Int J Rheum Dis 11(1):39–44
Ozenci AM, Inanmaz E, Ozcanli H et al (2007) Proprioceptive comparison of allograft and autograft anterior cruciate ligament reconstructions. Knee Surg Sports Traumatol Arthrosc 15(12):1432–1437
Pai YC, Rymer WZ, Chang RW, Sharma L (1997) Effect of age and osteoarthritis on knee proprioception. Arthritis Rheum 40(12):2260–2265
Pap G, Machner A, Awiszus F (1998) Measuring knee joint kinesthesis for determining proprioceptive deficits in varus gonarthrosis. Z Rheumatol 57(1):5–10
Qadir I, Shah B, Waqas M, Ahmad U, Javed S, Aziz A (2019) Component alignment in simultaneous bilateral versus unilateral total knee arthroplasty. Knee Surg Relat Res 31(1):31–36
Runhaar J, Luijsterburg P, Dekker J, Bierma-Zeinstra SM (2015) Identifying potential working mechanisms behind the positive effects of exercise therapy on pain and function in osteoarthritis; a systematic review. Osteoarthrit Cartil 23(7):1071–1082
Sharma L, Pai YC, Holtkamp K, Rymer WZ (1997) Is knee joint proprioception worse in the arthritic knee versus the unaffected knee in unilateral knee osteoarthritis? Arthritis Rheum 40(8):1518–1525
Shirazi ZR, Shafaee R, Abbasi L (2014) The effects of transcutaneous electrical nerve stimulation on joint position sense in patients with knee joint osteoarthritis. Physiother Theory Pract 30(7):495–499
Skinner HB, Barrack RL, Cook SD, Haddad RJ Jr (1984) Joint position sense in total knee arthroplasty. J Orthop Res 1(3):276–283
Slupik A, Kowalski M, Bialoszewski D (2013) Impact of knee arthroplasty on knee sensorimotor system performance. Ortoped Traumatol Rehabil 15(6):555–565
Smith TO, King JJ, Hing CB (2012) The effectiveness of proprioceptive-based exercise for osteoarthritis of the knee: a systematic review and meta-analysis. Rheumatol Int 32(11):3339–3351
Solomonow M, Krogsgaard M (2001) Sensorimotor control of knee stability. A review. Scand J Med Sci Sports 11(2):64–80
Song JS, Hong KT, Kim NM, Park HS, Choi NH (2020) Human umbilical cord blood-derived mesenchymal stem cell implantation for osteoarthritis of the knee. Arch Orthop Trauma Surg 20:20
Sun X, Wang J, Su Z (2020) A meta-analysis of total knee arthroplasty following high tibial osteotomy versus primary total knee arthroplasty. Arch Orthop Trauma Surg 20:20
Takagi S, Omori G, Koga H et al (2018) Quadriceps muscle weakness is related to increased risk of radiographic knee OA but not its progression in both women and men: the Matsudai Knee Osteoarthritis Survey. Knee Surg Sports Traumatol Arthrosc 26(9):2607–2614
Trans T, Aaboe J, Henriksen M, Christensen R, Bliddal H, Lund H (2009) Effect of whole body vibration exercise on muscle strength and proprioception in females with knee osteoarthritis. Knee 16(4):256–261
Tsauo JY, Cheng PF, Yang RS (2008) The effects of sensorimotor training on knee proprioception and function for patients with knee osteoarthritis: a preliminary report. Clin Rehabil 22(5):448–457
van der Esch M, Knoop J, Hunter DJ et al (2013) The association between reduced knee joint proprioception and medial meniscal abnormalities using MRI in knee osteoarthritis: results from the Amsterdam osteoarthritis cohort. Osteoarthrit Cartil 21(5):676–681
Van Der Esch M, Steultjens M, Harlaar J, Knol D, Lems W, Dekker J (2007) Joint proprioception, muscle strength, and functional ability in patients with osteoarthritis of the knee. Arthritis Care Rese 57(5):787–793
Wells GA, Shea B, O'Connell D, et al (2014) The Newcastle-Ottawa scale for assessing the quality of nonrandomized studies 2014. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 1 Mar 2018
Acknowledgements
We are very grateful for the helpful comments provided by the reviewers and journal editors. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article, nor have any funds been received in support of this study.
Funding
This study has no funding support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflicts of interest to disclose regarding this manuscript.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, SS., Kim, HJ., Ye, D. et al. Comparison of proprioception between osteoarthritic and age-matched unaffected knees: a systematic review and meta-analysis. Arch Orthop Trauma Surg 141, 355–365 (2021). https://doi.org/10.1007/s00402-020-03418-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03418-2