Abstract
Introduction
Postoperative pain management options are of great importance for patients undergoing total hip arthroplasty, as joint replacement surgery is reported to be one of the most painful surgical procedures. This study demonstrates pain outcome until 4 weeks postoperatively and evaluates factors influencing pain in the postoperative course after total hip arthroplasty.
Materials and methods
A total of 103 patients were included in this prospective cohort trial and underwent total hip arthroplasty. Postoperative pain was described using a numerical rating scale (NRS); demographic data and perioperative parameters were correlated with postoperative pain.
Results
Evaluation of pain scores in the postoperative course showed a constant decrease in the first postoperative week (mean NRS 3.1 on day 1 to mean NRS 2.3 on day 8) and, then, a perpetual increase for 3 days (mean NRS 2.6 on day 9 to mean NRS 2.3 on day 12). Afterwards, a continuous pain-level decrease was stated (continuous to a mean NRS 0.9 on day 29). No correlation was found between the potential influencing factors sex, age, body mass index, duration of surgery, ASA score, and postoperative pain levels, but a high significant correlation could be stated for preoperative pain levels and postoperative pain intensity (pain while moving p < 0.02 to p < 0.05 depending on the time period “week 1 postoperatively”, “week 2–4”, or “week 1–4”; pain while resting p < 0.001, in all the measured time intervals, respectively).
Conclusion
Increasing pain levels after the first week postoperatively, for 3 days, are most likely to be caused by the change to more extensive mobilization and physiotherapy in the rehabilitation unit. No significant influence or correlation on the intensity of postoperative pain could be found while evaluating potential predictors except preoperative pain levels. Pain management has to take these findings into account in the future to further increase patients’ satisfaction in the postoperative course after total hip arthroplasty and to adapt pain management programs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The procedure of total hip arthroplasty (THA) is a highly stressful surgical intervention for patients and pain is the key factor for patient’s satisfaction [1]. Hip arthroplasty is ranked 11th place on the list of most painful surgical procedures [2]. The development of chronic pain after THA is reported to be as high as 10% [3, 4], and therefore, high efforts were made to better understand this topic. How type of anesthesia in total hip arthroplasty affects postoperative pain intensity remains unclear [5].
Postoperative pain after total hip arthroplasty is a great strain for the patient and the ability for the early mobilization; besides, it may cause higher costs, lengthen hospital stays, and put additional burden on the health care system [5]. Pain furthermore is both influenced by psychological factors such as anxiety, helplessness, and depression, as well as it may increase those factors itself [6]. Multidisciplinary pain therapy, therefore, is of great importance. Furthermore, patients express concern about pain and dependence upon other persons during the postoperative and rehabilitation period after the surgical procedure [1]. Therefore, it is of importance to know and understand the timing of postoperative pain, and to provide for patients’ elucidation preoperatively.
The aim of this study was to evaluate the intensity and incidence of postoperative pain as well as possible influencing factors for its predisposition after total hip replacement surgery. Increased postoperative pain leads to increased analgesic use and a prolonged rehabilitation for the patient.
Materials and methods
In the present study, a total of 103 consecutive patients after total hip arthroplasty were prospectively evaluated in 2017. The patients were included a few days prior to the surgical intervention on the day of preoperative preparations in our admission department. Inclusion criteria were patients with primary arthroplasty of the hip, and consent for epidural anesthesia (spinal block) and sedation with propofol. Furthermore, only patients receiving stationary rehabilitation care in our own department for the time following the acute stationary care were included due to organizational reasons. Exclusion criteria were the existence of chronic pain syndrome preoperatively except the reported pain of the hip joint arthritis; furthermore, intraoperative change to general anesthesia was an exclusion criterion in order to prevent possible bias by anesthetic method used.
A standardized pain management concept was applied for all patients in this study:
Patients receive oral benzodiazepine premedication 1 h before the surgical procedure followed by spinal anesthesia with 4 ml of bupivacaine 0.5% and 0.1 mg of intrathecal morphine. During surgery, patients were sedated with propofol. A nurse in the intermediate care unit administers 3 mg of piritramide on patients demand in intervals during the first 12 h after the procedure. Ibuprofen 600 three times daily is used as standard analgesic medication on a regular daily basis. Oral-controlled analgesia is applied at the ward. Cool packs for the affected hip are also provided. Patients may receive additional analgetic medication depending on NRS values if required: tramadol 100 mg (40 gtt) with the possibility of a repeat dose after 30 min for NRS 3–6 and oxycodone 20 mg and a repeat dose after 1 h for NRS 7–10. In cases of persisting pain, the nurse will notify the physician for further device.
Patients received written and oral informed consent before the surgical procedure, general data (age, sex, BMI, and ASA score) were recorded as well as pain before surgery while resting and moving using the numerous rating scale (NRS 0 = no pain; NRS 10 = worst pain imaginable). All patients received a modified antero-lateral minimally invasive approach, DePuy (Warsaw, Poland) Pinnacle acetabular shells and Corail femoral stems were used and implanted cementless. Full weight bearing was already allowed in the immediate postoperative course. From the patients record, surgical duration was captured. Throughout postoperative course (4 weeks postoperatively), pain intensity was measured using the NRS scale, documented four times daily under supervision of the clinic staff—morning, lunchtime, evening, and night, as well as the maximum pain of the day (separately recorded and not calculated)—and entered in an anonymized databank. Patients received physiotherapy once daily including passive motion training gait practice. Specialized pain nurses supervised the documentation at the ward (7 full days during inpatient treatment in the hospital, standard in the observing orthopedic department). Patients documented their pain values as mentioned above on a standardized protocol in the following 3 weeks of inpatient rehabilitation three times daily plus the maximum pain of the day. Physiotherapy in the rehabilitation unit was applied to our colleague’s standardized and health insurance requested intense rehabilitation program.
Afterwards, a mean of the values recorded four times daily was calculated per day, the maximum pain of the day value was evaluated separately.
In addition, possible pain modulating factors and therefore correlation coefficients were calculated. The postoperative period was separated into values of the first postoperative week (acute hospital, T1), values of week 2–4 (rehabilitation unit, T2), and values of the overall time postoperatively to analyze these possible pain-influencing factors (T3).
The study was approved by the local Ethics Committee with the approval number 16-101-0204 (IRB approval). Furthermore, the project was registered in the German Registry of Clinical Studies (DRKS) with the approval number DRKS00011803 (WHO register). The study was applied in accordance with the ethical standards of the Declaration of Helsinki 1975.
Statistical analysis was performed using SPSS 22.0 (IBM SPSS Statistics, Armonk, NY, USA—IBM Corp.). For descriptive analysis, absolute and relative frequencies or mean and standard deviation were stated. Predictors of postoperative pain were analyzed using linear regression models. No imputation methods were used. A p value < 0.05 was considered statistically significant.
Results
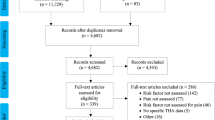
We were finally able to achieve a participation rate of 94% (n = 103). The reason for the missing data of 6% (n = 7) was that these patients refused to fill out pain sheets (n = 4), disclosed withdrawal of study participation (n = 2), or a second surgical intervention due to a complication (n = 1).
The cohort was composed of 50 men (48.5%) and 53 women (51.5%) with a total mean age of 64.7 ± 9.3 years (63.6 ± 9.1 for males, 65.7 ± 9.6 for females). The average value of the body mass index (BMI) was 27.9 kg/m2 ± 4.8 (28.2 ± 4.6 for males, 27.7 ± 4.9 for females). According to the definitions of the World Health Organization (WHO) 22.3% of patients showed normal weight, 46.6% overweight, and 31.1% obesity. The average duration of surgery was 56.5 ± 16.1 min with a minimum of 35 min and a maximum of 109 min. 35.9% of all patients had an ASA score (American Society of Anesthesiologists) of 1, 59.2% an ASA score of 2, and 4.9% an ASA score of 3; none of the patients had a higher ASA score.
Pain scores were evaluated preoperatively, separated into pain while resting (mean 3.9, SD 2.5) and while moving (mean 6.6, SD 2.0). In the following postoperative period, pain scores were measured four times daily (morning, lunchtime, evening and before going to bed) on days 1–day 29 (Table 1; Fig. 1). A mean was calculated per day for graphic representation and the later correlation analysis (Fig. 2). Furthermore, the maximum pain of the day was reported by the patients per day and was then evaluated (Table 1; Fig. 1).
For the possible influencing factors age, sex, BMI, duration of surgery, and ASA score, no correlation could be stated, whereas preoperative pain intensity showed a highly significant correlation to postoperative pain levels (Table 2).
Discussion
Clear postoperative pain-level decrease has been stated regarding the postoperative course after total hip arthroplasty. We were not able to find data evaluating the course of postoperative pain in the very early postoperative and especially the rehabilitation care period.
While the lowest pain levels in the first postoperative week were found on day 8 with an NRS of 2.3, these increased to 2.6 on day 9. This may be caused by the patient’s discharge into the rehabilitation unit coming along with the beginning of an intense rehabilitation program on day 9. This increased pain-level effect lasted for 3 days (day 9–11); pain levels of the eighth postoperative day were then undercut with a steady decrease until the end of the observation 4 weeks after the surgical procedure.
There are numerous studies evaluating pain scores at baseline and at one single postoperative assessment 6 or 12 months after arthroplasty by comparing NRS scores, demonstrating highly significant pain score decrease at this stage [7, 8]. However, hardly, any studies mention the immediate course of pain after the surgical procedure and in the rehabilitation period, although this period is particularly challenging for the patients to our experience and in the end accountable for socio-professional reintegration.
Findings on the extent and timing of pain made during the first 12 postoperative months show that most of the improvements evolve within the first 3 postoperative months [9,10,11,12,13,14,15,16,17,18,19]. While several studies have found no or minor improvements on pain levels after this period [9, 11, 13, 14, 18, 19], improvements beyond this 3-month course have also been stated [9, 10, 12, 15,16,17]. A few studies [12, 15,16,17] used statistical tests to ascertain the existence of any change in pain scores or developed continuous pain intensity evaluation postsurgery like we performed in the study at hand. Our results on improvements in pain after THA are consistent with the previous studies, although we showed that most of the recovery, measured by self-reported pain level, occurs in the first few weeks and not months after arthroplasty [9, 11,12,13,14, 20].
Davis et al. [21] described a preoperative pain level of NRS 9.4 and a decrease to NRS 3.9 6 months postoperatively, while function scores, which were not measured in this study, significantly improved. Both preoperative and 6-month postoperative values are higher compared to our results. Our results, however, show that the highest proportion of pain decline can already be stated within 4 weeks after the surgical procedure. Fitzgerald et al. [12] demonstrated an improvement of “bodily pain” 4 weeks postoperatively, while physical function did not improve in this time period. In this study, SF-36 pain values were compared pre- and postoperatively. The approach of using the SF-36 hinders the comparison to a couple of studies which have used the NRS score. In a study of Lenguerrand et al., a highly significant decrease of patient reported pain was stated for the time after 3 months postoperatively, with no significant change in the course between 3 and 12 months. In conclusion, the above-mentioned studies all show significant decrease of pain scores which is consistent with our results. Still, the close look onto very early postoperative pain scores in our study shows that the peak of pain decrease can be stated for the very first postoperative weeks. Therefore, most efficient pain therapy is needed in this period including adaptation of medication to patient reported pain levels, also considering a possible pain increase at the beginning of intense rehabilitation program.
The evaluation of potential influencing factors in three different time intervals (T1–T3) was decisively influenced by the fact that a considerable pain-level increase was shown on day 9 after total hip arthroplasty and will be discussed in the following section.
In general, the study shows that more women (51.5%) than men (48.5%) undergo implantation of hip endoprosthesis. This observation correlates with the results of Schrader et al. [22] who applied an arthroplasty gender distribution for 2006 in Germany, in which total hip arthroplasty was performed in 60.2% female and 39.8% male patients. When analyzing sex as a potential predictor for postoperative pain intensity, women did not show more pain than men after THA. This comes up to the results of Mannion et al. describing no difference in postoperative pain between women and men after 12 months [23]. This finding is contrary to the results of some studies. Evidence of a gender-related relationship with postoperative pain, as described by Wiesenfeld-Hallin [24], can be found in numerous studies [25, 26]. The cause is given by sociocultural, psychological, and biological factors. Wiesenfeld-Hallin also postulates that the female sex is more sensitive to pain than the male [27, 28]. Furthermore, Caicedo et al. [29] reported higher levels of pain after arthroplasty in women due to higher rate and severity of metal sensitization in women, which might be immunologically preset.
The average age of our patient population of 64.7 years is congruent with the results of the study by Schrader et al. [22]. They found that 67.3% of hip endoprosthesis were implanted at age 60–79. Age, in general, is considered a major risk factor for the occurrence of hip arthritis. The prevalence of this type of joint disease increases with age and reaches a plateau phase in the seventh decade of life [30]. Age was also examined in other studies as a possible predictor [26]. It is assumed that older patients, who may already suffer from osteoarthritis complaints for a long time, are more sensitive than younger patients in the sense of pain memory in the postoperative course. For example, Paladini et al. describe a decrease of pain tolerance in elderly patients and, furthermore, point out the change in neuronal sensation which might ask for different approaches to pain management [31]. However, analyzing predictors, no correlation between age and postoperative pain intensity could be stated in this study.
Another decisive influence on the development of hip osteoarthritis is a high BMI [32]. This risk factor is clearly evident when comparing our study participants with the German population. While, in the German population, 46.5% are of normal weight, only 22.3% of the patients collectively reach the corresponding BMI between 18.5 and 25 kg/m2. The most striking example is the difference in a BMI > 30 kg/m2 and, therefore, speaking of obesity. Among all participating patients, 31.1% were obese, whereas only 14.7% of Germans have BMI values above 30 kg/m2 [22]. Therefore, the BMI was also tested in the present work as a possible parameter influencing the postoperative course of pain, but no correlation could be found.
The duration of surgery as a possible cause of increased pain intensity was also analyzed, as the duration of surgery may reflect the difficulty of implantation. There may be repeated resection of bone or more frequent insertion of trial implants intraoperatively, which may affect postoperative pain development. Nonetheless, this hypothesis finds no support in the present evaluation.
When evaluating possible influence of the ASA score on postoperative pain levels, no correlation was found. Comorbidities, which might influence the ASA score, do not seem to effect pain in the postoperative course.
Finally, preoperative pain levels, both pain while resting and moving, showed a highly significant correlation with mean pain levels in the postoperative course. This may be caused by a large variety of factors. First of all, pain memory plays an important role in the further personal sensation of pain for the individual patient. If pain has been non-bearable before the operation for a long time, it may be more difficult to ‘erase’ the pain memory of the brain even after having removed the initial cause.
Then, pain may have negatively influenced the patient’s live before surgery, resulting in, i.e., unemployment or social isolation, therefore, inducing depression and anxiety. All of these cannot just be eliminated by the operation as the arthritis can be. The patient’s worries may even be worsened, because it remains unclear to the individual how the personal outcome is going to develop. In conclusion, this may also lead to higher postoperative pain intensities. Davis et al. [21] also reported, concordant to our results, preoperative pain levels, and comorbidity to be significant predictors for pain postoperatively, in this study, claimed for an interval after 2-year postprocedure.
Limitations to be mentioned are first of all the restriction on pain course for 4 weeks postoperatively. Possible external influence factors on pain sensation in the postoperative period, e.g., family, daily routine, and work, could not be considered. However, this circumstance is a strength of the study, as well, as all patients were treated in a standardized inpatient-rehabilitation setting and before mentioned possible factors were not causing bias on pain in the evaluated period. Furthermore, only patients treated in our own stationary rehabilitation unit were included due to organizational reasons—to be stated as a possible selection bias. As most of our acute hospital patients, who are allowed to take part in a stationary rehabilitation program by their assurance companies, choose to stay for the stationary rehabilitation program in our own department, this possible selection bias should be reduced to a minimum.
Besides, results in our study are limited to pain evaluation, functional scores or parameters were not assessed compared to other studies. However, the evaluation of functional outcome was not the target of this work.
In the specific pain management setting as described in this study, patients can expect the observed pain course. This information can be either used to improve patient education by explaining this information—“patient education”—or to improve the pain protocol to prevent an increase of NRS after discharge of the acute part of the medical treatment.
Conclusion
The present study demonstrates pain course after primary hip arthroplasty within 4 weeks postoperatively and analyses possible influence factors for pain intensity. Pain levels decreased steadily on the days in the acute hospital (first week), which showed an increase for 3 days with the beginning of intense mobilization at the rehabilitation unit and then a steady decrease until the end of the intensive rehabilitation phase (weeks 2–4).
Analgetic medication has to be administered according to the patients’ information and needs, which is often not the case, especially in rehabilitation units, where patients are not able to attain the same medical treatment compared to the acute hospital part.
High preoperative pain levels predict for higher postoperative pain intensity and vice versa. Other possible influencing factors such as age, sex, body mass index, duration of surgery, or ASA score did not show a significant correlation.
Orthopedic surgeons have to take these findings into account when preparing their pain management concept in the future to improve patients’ satisfaction in the postoperative course after primary total hip arthroplasty. Especially, the pain peak after the first postoperative week with a new pain increase might lead to confusion in many patients. The occurrence of postoperative pain and the relation to time should be clearly explained to patients before surgery.
In the future, studies should also take psychological factors into account, as pain sensation of each patient is individual.
References
Karlson EW, Daltroy LH, Liang MH, Eaton HE, Katz JN (1997) Gender differences in patient preferences may underlie differential utilization of elective surgery. Am J Med 102(6):524–530
Gerbershagen HJ, Pogatzki-Zahn E, Aduckathil S, Peelen LM, Kappen TH, van Wijck AJ, Kalkman CJ, Meissner W (2014) Procedure-specific risk factor analysis for the development of severe postoperative pain. Anesthesiology 120(5):1237–1245. https://doi.org/10.1097/ALN.0000000000000108
Wylde V, Sayers A, Lenguerrand E, Gooberman-Hill R, Pyke M, Beswick AD, Dieppe P, Blom AW (2015) Preoperative widespread pain sensitization and chronic pain after hip and knee replacement: a cohort analysis. Pain 156(1):47–54. https://doi.org/10.1016/j.pain.0000000000000002
Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P (2012) What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open 2(1):e000435. https://doi.org/10.1136/bmjopen-2011-000435
Greimel F, Maderbacher G, Zeman F, Grifka J, Meissner W, Benditz A (2017) No clinical difference comparing general, regional, and combination anesthesia in hip arthroplasty: a multicenter cohort-study regarding perioperative pain management and patient satisfaction. J Arthroplast 32(11):3429–3433. https://doi.org/10.1016/j.arth.2017.05.038
Fikentscher T, Grifka J, Benditz A (2015) Perioperative pain therapy in orthopedics. Orthopade 44(9):727–740. https://doi.org/10.1007/s00132-015-3152-6
Lenguerrand E, Wylde V, Gooberman-Hill R, Sayers A, Brunton L, Beswick AD, Dieppe P, Blom AW (2016) Trajectories of pain and function after primary hip and knee arthroplasty: the ADAPT cohort study. PLoS One 11(2):e0149306. https://doi.org/10.1371/journal.pone.0149306
Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY (2004) Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am 86-A(5):963–974
Bachmeier CJ, March LM, Cross MJ, Lapsley HM, Tribe KL, Courtenay BG, Brooks PM, Arthritis C, Outcome Project G (2001) A comparison of outcomes in osteoarthritis patients undergoing total hip and knee replacement surgery. Osteoarthr Cartil 9(2):137–146
Browne JP, Bastaki H, Dawson J (2013) What is the optimal time point to assess patient-reported recovery after hip and knee replacement? A systematic review and analysis of routinely reported outcome data from the English patient-reported outcome measures programme. Health Qual Life Outcomes 11:128. https://doi.org/10.1186/1477-7525-11-128
Halket A, Stratford PW, Kennedy DM, Woodhouse LJ (2010) Using hierarchical linear modeling to explore predictors of pain after total hip and knee arthroplasty as a consequence of osteoarthritis. J Arthroplast 25(2):254–262. https://doi.org/10.1016/j.arth.2009.01.007
Fitzgerald JD, Orav EJ, Lee TH, Marcantonio ER, Poss R, Goldman L, Mangione CM (2004) Patient quality of life during the 12 months following joint replacement surgery. Arthritis Rheum 51(1):100–109. https://doi.org/10.1002/art.20090
Kennedy DM, Stratford PW, Hanna SE, Wessel J, Gollish JD (2006) Modeling early recovery of physical function following hip and knee arthroplasty. BMC Musculoskelet Disord 7:100. https://doi.org/10.1186/1471-2474-7-100
Kennedy DM, Stratford PW, Riddle DL, Hanna SE, Gollish JD (2008) Assessing recovery and establishing prognosis following total knee arthroplasty. Phys Ther 88(1):22–32. https://doi.org/10.2522/ptj.20070051
Naylor JM, Harmer AR, Heard RC, Harris IA (2009) Patterns of recovery following knee and hip replacement in an Australian cohort. Aust Health Rev 33(1):124–135
Davis AM, Perruccio AV, Ibrahim S, Hogg-Johnson S, Wong R, Streiner DL, Beaton DE, Cote P, Gignac MA, Flannery J, Schemitsch E, Mahomed NN, Badley EM (2011) The trajectory of recovery and the inter-relationships of symptoms, activity and participation in the first year following total hip and knee replacement. Osteoarthr Cartil 19(12):1413–1421. https://doi.org/10.1016/j.joca.2011.08.007
Hamilton D, Henderson GR, Gaston P, MacDonald D, Howie C, Simpson AH (2012) Comparative outcomes of total hip and knee arthroplasty: a prospective cohort study. Postgrad Med J 88(1045):627–631. https://doi.org/10.1136/postgradmedj-2011-130715
Kennedy DM, Hanna SE, Stratford PW, Wessel J, Gollish JD (2006) Preoperative function and gender predict pattern of functional recovery after hip and knee arthroplasty. J Arthroplast 21(4):559–566. https://doi.org/10.1016/j.arth.2005.07.010
Kennedy DM, Stratford PW, Robarts S, Gollish JD (2011) Using outcome measure results to facilitate clinical decisions the first year after total hip arthroplasty. J Orthop Sports Phys Ther 41(4):232–239. https://doi.org/10.2519/jospt.2011.3516
Judge A, Cooper C, Williams S, Dreinhoefer K, Dieppe P (2010) Patient-reported outcomes one year after primary hip replacement in a European Collaborative Cohort. Arthritis Care Res (Hoboken) 62(4):480–488. https://doi.org/10.1002/acr.20038
Davis AM, Agnidis Z, Badley E, Kiss A, Waddell JP, Gross AE (2006) Predictors of functional outcome two years following revision hip arthroplasty. J Bone Joint Surg Am 88(4):685–691. https://doi.org/10.2106/JBJS.E.00150
Schrader P, Boy O, Schleiz W, Dienst R, Reinert C, Sanger V, Schauwecker HH, Siebert W, Scharf HP (2008) Determining the indication for primary total hip and knee replacement. Results of external quality assurance of over 270,000 primary total hip and knee replacements. Orthopade 37(10):1016–1026. https://doi.org/10.1007/s00132-008-1341-2
Mannion AF, Impellizzeri FM, Naal FD, Leunig M (2015) Women demonstrate more pain and worse function before THA but comparable results 12 months after surgery. Clin Orthop Relat Res 473(12):3849–3857. https://doi.org/10.1007/s11999-015-4479-3
Wiesenfeld-Hallin Z (2005) Sex differences in pain perception. Gend Med 2(3):137–145
Oak SR, Strnad GJ, O’Rourke C, Higuera CA, Spindler KP, Brooks PJ (2017) Mid-term results and predictors of patient-reported outcomes of Birmingham hip resurfacing. J Arthroplast 32(1):110–118. https://doi.org/10.1016/j.arth.2016.06.049
Lungu E, Vendittoli PA, Desmeules F (2015) Identification of patients with suboptimal results after hip arthroplasty: development of a preliminary prediction algorithm. BMC Musculoskelet Disord 16:279. https://doi.org/10.1186/s12891-015-0720-1
Henderson LA, Gandevia SC, Macefield VG (2008) Gender differences in brain activity evoked by muscle and cutaneous pain: a retrospective study of single-trial fMRI data. Neuroimage 39(4):1867–1876. https://doi.org/10.1016/j.neuroimage.2007.10.045
Hallin RG (2003) Pain more painful in women. Gender perspective neglected in research on the biological mechanisms of pain. Lakartidningen 100(46):3738–3741
Caicedo MS, Solver E, Coleman L, Jacobs JJ, Hallab NJ (2017) Females with unexplained joint pain following total joint arthroplasty exhibit a higher rate and severity of hypersensitivity to implant metals compared with males: implications of sex-based bioreactivity differences. J Bone Joint Surg Am 99(8):621–628. https://doi.org/10.2106/JBJS.16.00720
Creamer P, Hochberg MC (1997) Osteoarthr Lancet 350(9076):503–508. https://doi.org/10.1016/S0140-6736(97)07226-7
Paladini A, Fusco M, Coaccioli S, Skaper SD, Varrassi G (2015) Chronic pain in the elderly: the case for new therapeutic strategies. Pain Physician 18(5):E863–E876
Richmond SA, Fukuchi RK, Ezzat A, Schneider K, Schneider G, Emery CA (2013) Are joint injury, sport activity, physical activity, obesity, or occupational activities predictors for osteoarthritis? A systematic review. J Orthop Sports Phys Ther 43(8):515–519. https://doi.org/10.2519/jospt.2013.4796
Author information
Authors and Affiliations
Contributions
All authors made contributions to the interpretation of data and have been involved in drafting the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethical standards
The study was approved by the local Ethics Committee with the approval number 16-101-0204 (IRB approval). Furthermore, the project was registered in the German Registry of Clinical Studies (DRKS) with the approval number DRKS00011803 (WHO register). The study was applied in accordance with the ethical standards of the Declaration of Helsinki 1975.
Rights and permissions
About this article
Cite this article
Greimel, F., Dittrich, G., Schwarz, T. et al. Course of pain after total hip arthroplasty within a standardized pain management concept: a prospective study examining influence, correlation, and outcome of postoperative pain on 103 consecutive patients. Arch Orthop Trauma Surg 138, 1639–1645 (2018). https://doi.org/10.1007/s00402-018-3014-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-3014-x