Abstract
Purpose
The purpose of this study was to evaluate and classify causes for anterior cruciate ligament (ACL) reconstruction failure. It was hypothesized that specific technical and biological reconstruction aspects would differ when comparing traumatic and non-traumatic ACL reconstruction failures.
Materials and methods
One hundred and forty-seven consecutive patients who experienced ACL reconstruction failure and underwent revision between 2009 and 2014 were analyzed. Based on a systematic failure analysis, including evaluation of technical information on primary ACL reconstruction and radiological assessment of tunnel positions, causes were classified into traumatic and non-traumatic mechanisms of failure; non-traumatic mechanisms were further sub-divided into technical and biologic causes. Spearman’s rank correlation coefficient and chi-squared tests were performed to determine differences between groups based on various factors including graft choice, fixation technique, technique of femoral tunnel positioning, tunnel malpositioning, and time to revision.
Results
Non-traumatic, i.e., technical, and traumatic mechanisms of ACL reconstruction failure were found in 64.5 and 29.1% of patients, respectively. Biological failure was found only in 6.4% of patients. Non-anatomical femoral tunnel positioning was found the most common cause (83.1%) for technical reconstruction failure followed by non-anatomical tibial tunnel positioning (45.1%). There were strong correlations between non-traumatic technical failure and femoral tunnel malpositioning, transtibial femoral tunnel drilling techniques, femoral transfixation techniques as well as earlier graft failure (p < 0.05).
Conclusions
Technical causes, particularly tunnel malpositioning, were significantly correlated with increased incidence of non-traumatic ACL reconstruction failure. Transtibial femoral tunnel positioning techniques and femoral transfixation techniques, showed an increased incidence of non-traumatic, earlier graft failure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There has been a recent increase in the number of primary and revision anterior cruciate ligament (ACL) reconstructions being performed [1,2,3,4]. Reported rates of graft failure after ACL reconstruction vary from 0 to 14% [5,6,7,8]. Multiple studies have attempted to elucidate factors contributing to ACL reconstruction failure. Epidemiological factors such as age, gender, and body mass index (BMI) [9] have been identified as risk factors for ACL reconstruction failure. Bony morphology has also been demonstrated to be an important risk factor [10,11,12].
Risk factors for ACL reconstruction failure are typically categorized as either traumatic, technical, or biological in nature [1, 13, 14]. In a large prospective study of revision ACL reconstructions conducted by the Multicenter ACL Revision Study (MARS) Group, the reported mode of ACL reconstruction failure was traumatic in 32%, technical in 24%, biologic in 7%, and combined in 37% of cases [14]. Although traumatic rupture of the ACL graft has been cited as the most common cause of ACL reconstruction failure, other studies have identified technical factors, such as non-anatomic tunnel placement, as the most common etiology in 22–79% of cases [1].
It is important to note that, in most studies, the system for categorizing the mechanism of failure is solely determined by the revising surgeon. Given that there are no commonly accepted definitions or objective criteria for assessing causes of ACL reconstruction failure, it is unsurprising that there is wide variability among knee experts when assessing specific causes of ACL graft failure [15]. An expansion of the aforementioned classification system (traumatic, technical or biological causes) could increase comparability between studies and improve understanding of the various factors contributing to ACL reconstruction failure.
Thus, the purpose of this study was to systematically evaluate technical differences in primary ACL reconstruction comparing traumatic versus non-traumatic ACL reconstruction failure. It was hypothesized that specific technical aspects have a significant influence on non-traumatic ACL reconstruction failures when compared to traumatic re-injuries.
Materials and methods
Institutional review board approval was obtained.
Subjects
Between 2009 and 2014, 147 consecutive cases of failure after ACL reconstruction were evaluated and retrospectively reviewed. All patients had undergone primary ACL surgery at different institutions and underwent ACL revision surgery at the reporting department by a single experienced orthopedic surgeon.
ACL reconstructions were defined as failures when patients exhibited knee laxity, defined as a positive pivot shift or Lachman test (office exam as well as exam under anesthesia during revision surgery) with notable side-to-side difference on arthrometer testing (> 4 mm) [16]. Inclusion criteria for the study included either of the above-mentioned criteria in addition to arthroscopic and magnetic resonance imaging (MRI) confirmation of recurrent laxity. Criteria for exclusion included any history of prior ACL reconstruction failure, complex regional pain syndrome, incomplete medical records regarding the technique of the primary ACL reconstruction or mechanism of failure, incomplete or missing computed tomography (CT) scans, any prior ACL revision surgery, and the presence of concomitant ligamentous injuries.
Failure analysis
A systematic failure analysis was obtained in all cases before revision surgery. Data were collected on patient demographics and on information regarding the primary ACL reconstruction, including graft type, femoral tunnel drilling technique, graft fixation technique as well as postoperative complications, including additional revision surgery, and infection. Patients were administered a questionnaire that included questions regarding the mechanism of failure to identify whether a traumatic incidence was present or absent causing recurrent laxity. All patients underwent a comprehensive knee examination that was graded according to the 1999 International Knee Documentation Committee guidelines [17, 18].
Tibial and femoral tunnel positions were determined on CT scans using validated radiographic measurement methods [19, 20]. As previously described, [21, 22], tunnel positions were categorized as anatomic if the center of the femoral tunnel position was within a range of depth 19–29% and height 22–53% and if the tibial tunnel position was within a range of 30–44% in the CT scan measurements.
ACL reconstruction failures were categorized by the classification system previously described by Wright et al. [14]. A failure was classified as traumatic whenever a single adequate mechanism of trauma for ACL graft rupture was identified, regardless of other factors, such as tunnel positioning. A failure was classified as technical whenever there was no history of trauma and a technical cause for graft failure could be identified. All other cases were classified as biological when there was a history of a postoperative intraarticular knee infection with positive microbiology cultures and also in cases in which no mechanism of trauma or technical cause could be identified.
Data analysis
Descriptive statistics, including means, frequency counts, percentages, and ranges were determined as appropriate for continuous and categorical variables. Spearman’s rank correlation coefficient and chi-squared tests were performed to evaluate for predictors of non-traumatic ACL reconstruction failure, such as graft choice, fixation technique, technique of femoral tunnel positioning, or tunnel malpositioning. Data analyses were performed using IBM SPSS software version 22.0 (SPSS Inc, Chicago, Illinois). Significance was set at a p value of < 0.05.
Results
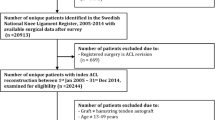
110 patients (74 males and 36 females) met the inclusion criteria and were included in the final analysis (Fig. 1).
Mean ages at the times of primary ACL reconstruction and revision were 25.05 (range 12–48 years) and 28.7 years (range 15–48 years), respectively.
Classification of ACL reconstruction failure (Fig. 2)
Classification of ACL reconstruction failure according to Wright et al. [14]
Using the system outline above, all cases of ACL reconstruction were assigned to either the traumatic, technical or biological failure group.
The traumatic group consisted of 32 patients (29.1%). In all cases, a mechanism of contact or non-contact trauma was reported, resulting in recurrent subjective laxity, objective knee laxity and arthroscopically verified graft rupture. In the remaining 78 non-traumatic cases (70.9%), no traumatic incident was reported, and all of these patients were reported to have experienced gradual-onset of recurrent laxity along with non-traumatic “giving away” episodes. In this non-traumatic group, technical causes for non-traumatic graft failure were identified in 71 patients (64.5%), while biological causes were only found in seven (6.4%) patients. Within the biological failure group, four cases (3.6%) were related to joint infections and three other cases (2.7%) were classified as biological since neither any episode of trauma nor any technical error could be detected.
Time between primary ACL reconstruction and revision (Fig. 3)
The mean time between primary and revision surgeries was 49.4 months (range 5–247 months). There was a significant difference (p ≤ 0.05) in the mean time between surgeries between traumatic (74.9 months; range 6–247 months) and non-traumatic cases (40.1 months; range 5–222 months), suggesting that patients with non-traumatic ACL reconstruction failure underwent revision surgery earlier. Furthermore, femoral transfixation was significantly associated with an earlier failure compared to other femoral fixation devices (p ≤ 0.05). No significant differences regarding the time to revision surgery were found comparing different tunnel positioning techniques (p ≥ 0.05).
Technical aspects of primary ACL reconstruction and technical failure analysis (Table 1; Fig. 4)
Comparison of the technical aspects of primary ACL reconstructions between traumatic and non-traumatic (including technical and biological) ACL reconstruction failure subgroups. Significant correlations were found between the presence of non-traumatic failure and femoral tunnel malpositioning, transtibial femoral tunnel drilling, and femoral transfixation (*p ≤ 0.05)
Data comparing various technical aspects of primary ACL reconstructions including graft choice, technique of femoral tunnel positioning, femorotibial fixation techniques and tunnel positioning between the traumatic, technical, and biological failure groups are represented in Table 1.
Non-anatomic femoral tunnel positioning was identified as the most common cause (83.1%) of non-traumatic technical ACL reconstruction failure followed by tibial malpositioning (45.1%). Of note, however, there were also large numbers of non-anatomic femoral (62.5%) and tibial (37.5%) tunnel positions in the traumatic group. There was a significant correlation between the incidence of non-traumatic technical failure and femoral tunnel malpositioning (p ≤ 0.05), but not tibial tunnel malpositioning (p ≥ 0.05).
There were also significant correlations between the incidence of non-traumatic technical failure and both transtibial femoral tunnel positioning techniques (p < 0.05) and femoral transfixation techniques (p ≤ 0.05). When different methods of femoral fixation techniques with non-anatomic tunnel positioning were compared, a significant correlation was found between the method of femoral transfixation and tibial tunnel malpositioning (p ≤ 0.05), although no correlation was found for femoral malpositioning (p ≥ 0.05).
Further comparison of the traumatic and non-traumatic group found no differences between graft types (p ≥ 0.05).
Other technical errors, such as femoral or tibial fixation failure or missed collateral ligament injuries associated with primary ACL reconstruction were not identified.
Discussion
The primary finding of this study was that, in agreement with the initial hypothesis, certain technical aspects, specifically the use of transtibial femoral tunnel positioning techniques and femoral transfixation techniques, were significantly correlated with increased incidence of non-traumatic ACL reconstruction failure. Furthermore, non-anatomic femoral tunnel positioning was identified as the most common cause for non-traumatic ACL reconstruction failure, though high rates of non-anatomic femoral and tibial tunnel positions were also found in patients with traumatic ACL reconstruction failure.
Based on the MARS’ system of classifying ACL reconstruction failures and the above-mentioned system of analyzing the causes of ACL reconstruction failure, non-traumatic (technical and biological) factors (70.9%) were identified as the most common cause of ACL reconstruction failure while traumatic causes for ACL reconstruction failure were found in 29.1% of the cases. This distribution is similar to a previously reported cohort of 90 revision ACL reconstructions [23] in which non-traumatic and traumatic ACL reconstructions failures accounted for 52 and 24% of cases, respectively, while other causes such as lack of graft incorporation (8%), loss of motion (3%), failure related to synthetic grafts (3%) and alignment or combined ligamentous instability patterns not addressed (9%) were found less frequently. In addition, the MARS Group [3] analyzed ACL reconstruction failure mechanisms in primary and multiple-revision patients. They found that the most common reasons for failure were non-traumatic, gradual-onset injury in 47% of multiple-revision patients and traumatic, non-contact ACL injuries (55%) in primary revision patients. Other studies have reported, however, that traumatic mechanisms are the predominant reason for ACL reconstruction failure [24]. The results of the present study highlight, therefore, that there is no consensus in literature concerning the predominant mechanism of ACL reconstruction failure.
While mechanisms of ACL reconstruction failure are commonly classified according to the MARS group’s mode of failure classification [14], there is still no clear agreement on definitions for failure [1]. Moreover, these systems do not fully allow for the fact that there may be combinations of different factors that may contribute to ACL reconstruction failure [3, 25, 26]. Wright et al. [26] emphasized that most studies examining potential causes of ACL reconstruction failure did not delineate the specific type of failure and only listed technical failure as a broad category. There is also a considerable amount of evidence that, in many studies, the classification of ACL reconstruction failures relies only on the individual surgeon’s assessment [14]. Matava et al. recently found that there is low inter- and intraobserver reliability regarding the evaluation of mechanisms of primary ACL reconstruction failure even among experienced knee surgeons [15].
To maximize reliability, the absence or presence of a detectable mechanism of trauma was chosen as the primary delineation for classifying mechanisms of failure in the present study. Furthermore, several technical aspects associated with ACL reconstruction failure were considered, including radiographic determination of tunnel positions based on validated measurement methods [19, 20].
Although there is ongoing debate regarding the most prevalent causes for ACL reconstruction failure, the results of the present study are in accordance with previous studies [1, 23, 27,28,29] which have identified technical failure as one of the more common causes of ACL reconstruction failure. Analyzing causes for revision after ACL reconstruction, Kamath et al. [1] recently reported that technical errors contribute to failure in 22–79% of cases, and Garofalo et al. [29] demonstrated malpositioning rates of 79 and 21% for femoral and tibial tunnels, respectively. The high rates of non-anatomic tunnel positions in patients with mechanisms of traumatic re-injury emphasizes that there may be combinations of different causes contributing to ACL reconstruction failure.
The present study found that transtibial drilling techniques were associated with non-traumatic technical failure, which supports the results of numerous cadaveric in vivo and clinical studies. In previous comparisons of transtibial with other femoral tunnel drilling techniques, it has been found that it may be technically more difficult to achieve anatomical tunnel positions with transtibial femoral drilling techniques [30,31,32,33,34,35]. Nevertheless, other studies do not confirm these results. Recent evidence from the Danish ACL Register detected an increased risk of revision after anteromedial compared with transtibial femoral tunnel drilling techniques [36]. However, tunnel positions were not analyzed in this study and, therefore, no conclusions on tunnel positions can be drawn.
The present study found similar frequencies of non-anatomic tunnel positioning with both anteromedial and the transtibial femoral tunnel drilling technique, which suggests that it is nevertheless a notable risk of non-anatomic tunnel positioning even with the anteromedial technique. This highlights the importance of placing tunnels anatomically during primary ACL reconstruction, regardless of the applied drilling technique. As tunnel malpositioning is a common cause of failure and occurs in considerable number of revision cases [37], it further has to be discussed whether tunnel positioning under fluoroscopic control or patient-specific drill template should be recommended [38].
The use of femoral transfixation techniques was found to be more commonly associated with non-traumatic and earlier ACL reconstruction failure. Although it cannot be definitely stated whether the transfixation method itself contributes to these findings, it is possible that non-anatomical tunnel positioning was more commonly associated with femoral transfixation techniques because this fixation technique was concurrent with the use of transtibial femoral tunnel drilling techniques in all cases. Discussing that only tibial tunnel positions could have been identified, being significantly more often associated with non-anatomic tunnel positions applying femoral transfixation techniques, it can be assumed that this may be related to modifications of tibial tunnel positions to achieve more anatomical femoral tunnel positions. However, identifying transtibial drilling techniques and femoral transfixation techniques, as independent factors contributing to non-traumatic technical ACL reconstruction failure, it has to be critically discussed, whether these techniques are suitable for ACL reconstruction especially when used in combination.
Graft choice is an important and frequently discussed factor in ACL reconstruction. The data here demonstrated no relevant differences in clinical outcomes and revision rates between graft types, which is in accordance with numerous previous studies [13, 14, 39]. However, results from a recent large prospective study found that patients receiving patellar tendon autografts had a significantly lower risk of revision compared with patients receiving hamstring autografts [40]. Given the relatively small sample size of patients with patellar tendon autografts in the present study, no significant conclusions could be drawn from the data presented here.
The present study found that non-traumatic ACL reconstruction failure, as compared to traumatic failure, was more commonly associated with earlier time to failure. Given that non-traumatic ACL graft failure is most commonly related to technical aspects of primary ACL reconstruction, it is possible that symptoms of failure may appear early after primary ACL reconstruction and thus lead to earlier time to failure. The relationship between non-traumatic mechanisms of ACL reconstruction failure and earlier time to failure may also be related to other previously described non-traumatic causes for early graft failure, such as failure of graft incorporation, loss of graft fixation and premature return to high-demand activities [1, 31, 41, 42]. The findings presented here are in line with previous studies which have reported that late failure is often secondary to a single or repetitive trauma to the graft [6, 43].
Limitations
There were several limitations to this study. Due to small sample sizes, statistically significant conclusions could not be drawn for some groups, such as allograft type subgroups. Furthermore, the present study was retrospective in nature. Of note, although the methodology used in the present study utilized clear definitions to delineate between failure mechanisms, technical (e.g., tunnel positions) and biological errors, no consensus on these definitions exists. Given the lack of a control group of patients with intact ACL reconstructions, the present study does not report on tunnel malpositioning rates in patients with intact ACL reconstructions. However, the data presented here does suggest that there are high rates of non-anatomic tunnel positioning in cases of both traumatic and non-traumatic ACL reconstruction failure.
Conclusion
In conclusion, this study showed significant correlations between non-anatomic tunnel positioning and the incidence of non-traumatic, technical ACL reconstruction failure. While this may suggest that non-anatomical tunnel positioning is an important cause for technical failure after primary ACL reconstruction, considerable numbers of non-anatomic tunnel positions were also found in patients with traumatic re-injuries. Furthermore, transtibial femoral tunnel drilling techniques and femoral transfixation techniques were also found to be significantly correlated with the incidence of non-traumatic graft failure. Consequently, the data highlight the importance of anatomically placed tunnel positions as well as tunnel positioning technique in primary ACL reconstruction.
References
Kamath GV, Redfern JC, Greis PE, Burks RT (2011) Revision anterior cruciate ligament reconstruction. Am J Sports Med 39(1):199–217. https://doi.org/10.1177/0363546510370929
Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD (2016) Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. https://doi.org/10.1177/0363546515621554
Chen JL, Allen CR, Stephens TE, Haas AK, Huston LJ, Wright RW, Feeley BT, Multicenter ACLRSG. (2013) Differences in mechanisms of failure, intraoperative findings, and surgical characteristics between single- and multiple-revision ACL reconstructions: a MARS cohort study. Am J Sports Med 41(7):1571–1578. https://doi.org/10.1177/0363546513487980
Spindler KP (2007) The Multicenter ACL Revision Study (MARS): a prospective longitudinal cohort to define outcomes and independent predictors of outcomes for revision anterior cruciate ligament reconstruction. J Knee Surg 20(4):303–307
Jarvela T (2007) Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective, randomize clinical study. Knee Surg Sports Traumatol Arthrosc 15(5):500–507. https://doi.org/10.1007/s00167-006-0254-z
Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K (2005) Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy 21(8):948–957. https://doi.org/10.1016/j.arthro.2005.04.110
Snow M, Campbell G, Adlington J, Stanish WD (2010) Two to five year results of primary ACL reconstruction using doubled tibialis anterior allograft. Knee Surg Sports Traumatol Arthrosc 18(10):1374–1378. https://doi.org/10.1007/s00167-009-0997-4
Shah AA, McCulloch PC, Lowe WR (2010) Failure rate of Achilles tendon allograft in primary anterior cruciate ligament reconstruction. Arthroscopy 26(5):667–674. https://doi.org/10.1016/j.arthro.2010.02.031
Brophy RH, Haas AK, Huston LJ, Nwosu SK, Group M, Wright RW (2015) Association of meniscal status, lower extremity alignment, and body mass index with chondrosis at revision anterior cruciate ligament reconstruction. Am J Sports Med 43(7):1616–1622. https://doi.org/10.1177/0363546515578838
Hashemi J, Chandrashekar N, Mansouri H, Gill B, Slauterbeck JR, Schutt RC Jr, Dabezies E, Beynnon BD (2010) Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med 38(1):54–62. https://doi.org/10.1177/0363546509349055
Hudek R, Fuchs B, Regenfelder F, Koch PP (2011) Is noncontact ACL injury associated with the posterior tibial and meniscal slope? Clin Orthop Relat Res 469(8):2377–2384. https://doi.org/10.1007/s11999-011-1802-5
Ireland ML, Ballantyne BT, Little K, McClay IS (2001) A radiographic analysis of the relationship between the size and shape of the intercondylar notch and anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc 9(4):200–205. https://doi.org/10.1007/s001670100197
MARS GROUP (2014) Effect of graft choice on the outcome of revision anterior cruciate ligament reconstruction in the Multicenter ACL Revision Study (MARS) Cohort. Am J Sports Med 42(10):2301–2310. https://doi.org/10.1177/0363546514549005
Group M, Wright RW, Huston LJ, Spindler KP, Dunn WR, Haas AK, Allen CR, Cooper DE, DeBerardino TM, Lantz BB, Mann BJ, Stuart MJ (2010) Descriptive epidemiology of the Multicenter ACL Revision Study (MARS) cohort. Am J Sports Med 38(10):1979–1986. https://doi.org/10.1177/0363546510378645
Matava MJ, Arciero RA, Baumgarten KM, Carey JL, DeBerardino TM, Hame SL, Hannafin JA, Miller BS, Nissen CW, Taft TN, Wolf BR, Wright RW, Group M (2015) Multirater agreement of the causes of anterior cruciate ligament reconstruction failure: a radiographic and video analysis of the MARS cohort. Am J Sports Med 43(2):310–319. https://doi.org/10.1177/0363546514560880
Dejour D, Ntagiopoulos PG, Saggin PR, Panisset JC (2013) The diagnostic value of clinical tests, magnetic resonance imaging, and instrumented laxity in the differentiation of complete versus partial anterior cruciate ligament tears. Arthroscopy 29(3):491–499. https://doi.org/10.1016/j.arthro.2012.10.013
Irrgang JJ, Ho H, Harner CD, Fu FH (1998) Use of the international knee documentation committee guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 6(2):107–114. https://doi.org/10.1007/s001670050082
Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, Richmond JC, Shelborne KD (2001) Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med 29(5):600–613
Bernard M, Hertel P, Hornung H, Cierpinski T (1997) Femoral insertion of the ACL. Radiographic quadrant method. Am J Knee Surg 10(1):14–21 (discussion 21–12)
Staubli HU, Rauschning W (1994) Tibial attachment area of the anterior cruciate ligament in the extended knee position. Anatomy and cryosections in vitro complemented by magnetic resonance arthrography in vivo. Knee Surg Sports Traumatol Arthrosc 2(3):138–146
Zantop T, Wellmann M, Fu FH, Petersen W (2008) Tunnel positioning of anteromedial and posterolateral bundles in anatomic anterior cruciate ligament reconstruction: anatomic and radiographic findings. Am J Sports Med 36(1):65–72. https://doi.org/10.1177/0363546507308361
Sullivan JP, Matava MJ, Flanigan DC, Gao Y, Britton CL, Amendola A, Group M, Wolf BR (2012) Reliability of tunnel measurements and the quadrant method using fluoroscopic radiographs after anterior cruciate ligament reconstruction. Am J Sports Med 40(10):2236–2241. https://doi.org/10.1177/0363546512458086
Carson EW, Anisko EM, Restrepo C, Panariello RA, O’Brien SJ, Warren RF (2004) Revision anterior cruciate ligament reconstruction: etiology of failures and clinical results. J Knee Surg 17(3):127–132
Salmon LJ, Pinczewski LA, Russell VJ, Refshauge K (2006) Revision anterior cruciate ligament reconstruction with hamstring tendon autograft: 5- to 9-year follow-up. Am J Sports Med 34(10):1604–1614. https://doi.org/10.1177/0363546506288015
Noyes FR, Barber-Westin SD (2006) Anterior cruciate ligament revision reconstruction: results using a quadriceps tendon-patellar bone autograft. Am J Sports Med 34(4):553–564. https://doi.org/10.1177/0363546505281812
Wright R, Spindler K, Huston L, Amendola A, Andrish J, Brophy R, Carey J, Cox C, Flanigan D, Jones M, Kaeding C, Marx R, Matava M, McCarty E, Parker R, Vidal A, Wolcott M, Wolf B, Dunn W (2011) Revision ACL reconstruction outcomes: MOON cohort. J Knee Surg 24(4):289–294
Diamantopoulos AP, Lorbach O, Paessler HH (2008) Anterior cruciate ligament revision reconstruction: results in 107 patients. Am J Sports Med 36(5):851–860. https://doi.org/10.1177/0363546507312381
Morgan JA, Dahm D, Levy B, Stuart MJ, Group MS (2012) Femoral tunnel malposition in ACL revision reconstruction. J Knee Surg 25(5):361–368. https://doi.org/10.1055/s-0031-1299662
Garofalo R, Djahangiri A, Siegrist O (2006) Revision anterior cruciate ligament reconstruction with quadriceps tendon-patellar bone autograft. Arthroscopy 22(2):205–214. https://doi.org/10.1016/j.arthro.2005.08.045
Duffee A, Magnussen RA, Pedroza AD, Flanigan DC, Group M, Kaeding CC (2013) Transtibial ACL femoral tunnel preparation increases odds of repeat ipsilateral knee surgery. J Bone Joint Surg Am Vol 95(22):2035–2042. https://doi.org/10.2106/JBJS.M.00187
Johnson DL, Swenson TM, Irrgang JJ, Fu FH, Harner CD (1996) Revision anterior cruciate ligament surgery: experience from Pittsburgh. Clin Orthop Relat Res 325(325):100–109
Arno S, Bell CP, Alaia MJ, Singh BC, Jazrawi LM, Walker PS, Bansal A, Garofolo G, Sherman OH (2016) Does anteromedial portal drilling improve footprint placement in anterior cruciate ligament reconstruction? Clin Orthop Relat Res. https://doi.org/10.1007/s11999-016-4847-7
Chen Y, Chua KH, Singh A, Tan JH, Chen X, Tan SH, Tai BC, Lingaraj K (2015) Outcome of single-bundle hamstring anterior cruciate ligament reconstruction using the anteromedial versus the transtibial technique: a systematic review and meta-analysis. Arthroscopy 31(9):1784–1794. https://doi.org/10.1016/j.arthro.2015.06.001
Thein R, Spitzer E, Doyle J, Khamaisy S, Nawabi DH, Chawla H, Lipman JD, Pearle AD (2016) The ACL graft has different cross-sectional dimensions compared with the native ACL: implications for graft impingement. Am J Sports Med. https://doi.org/10.1177/0363546516645531
Ahn JH, Lee YS, Jeong HJ, Park JH, Cho Y, Kim KJ, Ko TS (2017) Comparison of transtibial and retrograde outside-in techniques of anterior cruciate ligament reconstruction in terms of graft nature and clinical outcomes: a case control study using 3T MRI. Arch Orthop Trauma Surg 137(3):357–365. https://doi.org/10.1007/s00402-016-2606-6
Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind MC (2013) Increased risk of revision after anteromedial compared with transtibial drilling of the femoral tunnel during primary anterior cruciate ligament reconstruction: results from the Danish Knee Ligament Reconstruction Register. Arthroscopy 29(1):98–105. https://doi.org/10.1016/j.arthro.2012.09.009
Jaecker V, Zapf T, Naendrup JH, Pfeiffer T, Kanakamedala AC, Wafaisade A, Shafizadeh S (2017) High non-anatomic tunnel position rates in ACL reconstruction failure using both transtibial and anteromedial tunnel drilling techniques. Arch Orthop Trauma Surg 137(9):1293–1299. https://doi.org/10.1007/s00402-017-2738-3
Zhu M, Li S, Su Z, Zhou X, Peng P, Li J, Wang J, Lin L (2018) Tibial tunnel placement in anatomic anterior cruciate ligament reconstruction: a comparison study of outcomes between patient-specific drill template versus conventional arthroscopic techniques. Arch Orthop Trauma Surg 138(4):515–525. https://doi.org/10.1007/s00402-018-2880-6
Anderson MJ, Browning WM 3rd, Urband CE, Kluczynski MA, Bisson LJ (2016) A systematic summary of systematic reviews on the topic of the anterior cruciate ligament. Orthop J Sports Med 4(3):2325967116634074. https://doi.org/10.1177/2325967116634074
Gifstad T, Foss OA, Engebretsen L, Lind M, Forssblad M, Albrektsen G, Drogset JO (2014) Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med 42(10):2319–2328. https://doi.org/10.1177/0363546514548164
Jaureguito JW, Paulos LE (1996) Why grafts fail. Clin Orthop Relat Res (325):25–41
Eitzen I, Holm I, Risberg MA (2009) Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. Br J Sports Med 43(5):371–376. https://doi.org/10.1136/bjsm.2008.057059
Shelbourne KD, Gray T, Haro M (2009) Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med 37(2):246–251. https://doi.org/10.1177/0363546508325665
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Institutional review board approval was obtained by the ethics committee of Witten/Herdecke University (IRB Number: 09-2015).
Rights and permissions
About this article
Cite this article
Jaecker, V., Zapf, T., Naendrup, JH. et al. Differences between traumatic and non-traumatic causes of ACL revision surgery. Arch Orthop Trauma Surg 138, 1265–1272 (2018). https://doi.org/10.1007/s00402-018-2954-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-2954-5