Abstract
Background
Treatment recommendations for isolated radial neck delayed union/nonunion are sparse, but include mainly conservative treatment, electro-stimulation, bone grafting, open reduction and internal fixation (ORIF) and radial head resection. The purpose of this study was to perform a literature review on isolated delayed union/nonunion of radial neck fractures and to evaluate the reported outcomes of proposed treatment strategies. Furthermore, we aimed to generate data-based recommendations for this rare pathology. In the second part of this paper, we report two clinical cases of delayed union of isolated radial neck fractures recently treated at the senior authors institution.
Methods
A literature search on PubMed was performed. We selected all papers with a documented delayed union, pseudarthrosis or nonunion of the radial neck. All papers were reviewed for patient demographics, patient occupation, treatment type and timing relative to the initial trauma, X-ray documentation and outcome. The two patients with delayed union after isolated radial neck fractures recently treated at our institution were evaluated for age, mechanism of injury, occupation, treatment and outcome. Clinical and radiological follow-up examinations were performed 6, 12 weeks, and 1 year after initial trauma. Final clinical evaluations included the Mayo Elbow Performance Score (MEPS) [1] and the Disabilities of the Arm, Shoulder and Hand (DASH) Score [2].
Results
We found 17 cases reported in 11 articles matching our selection criteria of isolated radial neck delayed union or nonunion in adult patients. Average age was 55 years (range 29–73 years). The most frequent mechanism of injury was a fall on an outstretched arm from standing height. Initial treatment consisted of an arm sling for 1–4 weeks and physiotherapy. From the 17 included cases, six were operated on due to persistent pain. Three received bone grafts, one was supplemented with additional K-wire fixation, and three had radial head resections. Ten patients were treated conservatively: six were pain free and three were symptomatic at last follow-up; symptoms were not reported for one case. All surgically treated cases were pain free at the last follow-up, average 32 months (range 6–84). Of the conservatively treated group, eight of ten had documented nonunion. The two reported cases from our institution were initially treated conservatively for 4 and 6 months. Both had a radiologically documented delayed union. Both patients were operated on due to persistent pain precluding them from returning to work. At the last follow-up, MEPS and DASH scores were 100 points and 29 in one case and 100 points and 18 in the other, respectively.
Conclusion
Isolated delayed union or nonunion of the radial neck after conservative treatment in adult patients appears to be rare and often remains asymptomatic. Operative treatment is recommended for symptomatic delayed union/nonunion in patients with altered elbow function [3]. All surgically treated patients in our study with symptomatic delayed unions/nonunions had favorable clinical outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Isolated radial neck fractures in adult patients usually occur after a fall on an outstretched arm from standing height [4]. The initial treatment recommendation for nondisplaced radial neck fractures varies from no immobilization to immobilization for a short period of 1–6 weeks, followed by gentle mobilization. Delayed unions/nonunions after conservatively treated radial neck fractures are rarely reported and are probably only diagnosed due to persistent pain. This is reflected by the limited number of case reports found in the literature. The first reported symptomatic nonunion of a radial neck fracture was described in 1905 by Thomas et al. in a patient who presented with a painful nonunion 10 months after the initial trauma and conservative treatment [5].
Clinical experience supports that symptomatic radial neck nonunions are a rare condition, although a certain degree of neglect might underestimate this pathology. Therefore, it is not surprising that there is no standard clinical approach for the treatment of symptomatic isolated radial neck delayed union/nonunion in adult patients.
Approximately 25% of proximal forearm fractures involve the radial head and/or neck. This fracture type primarily occurs in males between 39 and 48 years of age or in elderly females with a peak incidence at > 80 years [4]. The most common reported mechanism of injury is a fall from standing height onto an outstretched hand. Lateral elbow pain, localized swelling and painful range of motion, particularly with pronation/supination, are the most common symptoms.
Various conservative treatment strategies have been proposed in the literature to address these fractures, including no immobilization to total immobilization with a cast for 1–6 weeks, followed by gentle mobilization by a physiotherapist. The operative approach to isolated delayed union/nonunion of radial neck fractures is restricted to symptomatic patients with functional restrictions in labor and includes bone grafting, K-wire fixation and radial head resection.
We recently treated two symptomatic delayed unions of isolated radial neck fractures with ORIF at our institution. We wanted to know whether this clinical decision is supported by the literature, and whether operative treatment should be delayed for more than 6 months, or if other factors could influence this decision.
Materials and methods
Literature review
A literature search was performed on PubMed that included the following keywords: “radial neck fracture”, “treatment”, “complications”, “outcome”, “delayed union”, “pseudarthrosis”, “nonunion”, “isolated” and “adult”. We included the terms “delayed union”, “nonunion” and “pseudarthrosis” in our search to include all reports independent of time definitions, which are inconsistent in the orthopedic trauma literature [6]. A few reports have suggested that delayed unions can generally be diagnosed between three and 6 months and still have the potential to heal; whereas, nonunions should be diagnosed between six and 9 months since they have little potential to heal, especially if they have evolved into a pseudarthrosis [6].
Demographic data such as age, gender, occupation, diagnosis, treatment and outcome were recorded. Authors were contacted when possible in the case of incomplete data (e.g., patient age or profession). We included all reports of X-ray documented delayed union or nonunion of isolated nondisplaced radial neck fractures in adult patients. We excluded children and adolescents under the age of 18 as well as combined fractures of the forearm and radial head.
Case reports
Both clinical cases were retrospectively evaluated using our institution’s clinical database. Informed consent was obtained from both patients. Patient follow-up took place on a regular basis at 6, 12 weeks and 4 months. Both patients remained symptomatic at the 4 month follow-up, and radiography showed delayed union in both. The decision to pursue operative treatment was made due to the fact that both patients were unable to return to work due to functional limitations. After operative treatment, clinical and radiological examinations were performed at 6, 12 weeks, and 1 year, and included Mayo Elbow Performance Score (MEPS) [1] and Disabilities of the Arm, Shoulder and Hand (DASH) Score assignments.
Results
Literature review
Our literature review revealed a total of 11 publications reporting a total of 16 patients (5 men, 11 women) with a mean age of 55 years (range 29–73 years) with 17 delayed unions/nonunions of isolated radial neck fractures. Two publications were retrospective case series, including four and three patients each. All other reports were case reports consisting of one or two cases each (Table 1). Data could be completed by personal communication with the author in three cases. In six cases, data on age, gender, pain, follow-up and persistent symptoms could not be completed.
Eight patients (2 men, 6 women) presented with a delayed union after a mean of 3.8 months (range 3–5 m), and 9 patients (3 men, 6 women) presented with a nonunion after a mean of 11.6 months (range 6–24 m).
Two cases with delayed union were healed on X-rays obtained at 7 and 20 months, respectively. Two of the eight patients with delayed union had physically demanding occupations (a farmer and a physician). Only the farmer underwent surgery with ORIF and bone grafting and had no residual pain shortly after surgery. The physician remained symptomatic at 1 year, whereas the other 6 patients from this group remained asymptomatic.
There were nine patients with nonunions, two of whom had physically demanding occupations (farmer and professional pianist). Out of the nine cases, five had surgery with ORIF and bone grafting or radial head excision. Four patients were treated conservatively, and three of those remained symptomatic at last follow-up. The five patients treated by surgery (including the farmer and the pianist) were pain free at the last follow-up.
With respect to treatment modality, the reported cases who had conservative treatment tended to be older compared with patients who had surgery. Out of the ten patients who were treated conservatively, four were still symptomatic and complained of pain at last follow-up. From this group, eight of the ten patients had radiologically proven persistent nonunions. Two patients showed a solid union after 7 and 20 months; one had received conservative treatment, whereas the other had electromagnetic field stimulation.
Patients with low-demand occupations remained asymptomatic after conservative treatment. As previously noted, one delayed union demonstrated a solid union on X-ray at 20 months. On the other hand, patients with high-demand occupations remained symptomatic in both groups. None of the patients in the operative group suffered complications or had residual symptoms.
Case reports
Case 1
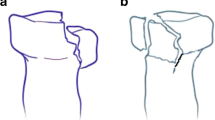
A 43-year-old man fell on his outstretched right arm during his work as an installation electrician and sustained an isolated radial neck fracture of his right elbow (Fig. 1). He was treated conservatively with a removable cast for 6 weeks. One week after the accident, X-ray revealed no displacement, and functional active-assisted physiotherapy out of the cast was begun. At the 3-month follow-up examination, the patient still complained of painful pronation/supination. He had limitation of his working capacity to 50%. Radiographs showed no evidence of radial neck union at 3 months (Fig. 2). The patient refused operative stabilization, so conservative treatment was continued as well as shock wave treatment. At the 3 month follow-up, the patient remained symptomatic and was only able to work part-time. CT scans proved nonunion after 6 months (Fig. 3). The patient consented to operative stabilization at that time. Due to minimal movements at the delayed union site during the operation, ORIF with two 2.0 mm lag screws crossing the nonunion was performed without formal debridement of the nonunion. No bone graft was added.
Postoperative immobilization with a cast was carried out for 4 days until secure wound healing was obtained. Functional aftercare guided by a physiotherapist was performed during the first 6 postoperative weeks. Twelve weeks postoperatively, the patient complained of some residual pain when lifting weights. The patient started working 3 months after the operation.
The clinical and radiological follow-up was then uneventful, and the patient regained full function with only slight residual pain after strenuous exercise. X-ray 12 months after the operation showed healing of the delayed union/nonunion (Fig. 4) and function MEPS 100 points, DASH-Index 29.2 (Fig. 5).
Case 2
A 36-year-old woman fell on her left side while hiking. She sustained a radial neck fracture as well as a traumatic dorsal hip dislocation with a posterior wall acetabular fracture on the same side. Radiography revealed a nondisplaced radial neck fracture without any intra-articular involvement (Fig. 6). Clinical examination showed tenderness over the radial neck and pain during pronation/supination. She was treated conservatively with a removable cast for a week. After confirmation of nondisplacement on X-ray 1 week after the accident, she started functional aftercare with supervised physiotherapy. Due to her surgically treated acetabular fracture, she was only allowed transfer mobilization using a wheelchair. Six weeks after the accident the X-ray showed a persistent fracture line. Clinical examination still elicited some pain during pronation/supination with local pressure. Three months after the fall, no evidence of consolidation was apparent (Fig. 7), and CT also revealed no signs of consolidation (Fig. 8). Flexion/extension as well as pronation/supination remained painful. Osteolysis at the fracture site was consistent with delayed union. Due to the high demands of the patient working at a sheltered workshop, we decided on ORIF using an anatomical plate for the proximal radius instrumented with locked screws in the radial head. This approach was chosen because scar tissue at the fracture site was removed and replaced by bone graft from the left iliac crest (Fig. 9).
Functional aftercare with physiotherapist-guided active-assisted movement was carried out during the first 6 postoperative weeks. After 6 weeks, radiological signs of consolidation were present. The fracture had healed after 12 weeks. Eleven months follow-up revealed some pain during strenuous exercises and with weather changes, and some crepitus on pronation/supination at the level of the annular ligament. Therefore, metal removal was decided upon and performed 12 months after the initial operation. On the last follow-up, the patient had full range of motion and was asymptomatic (MEPS 100 points, DASH-Index 18.3) (Fig. 10).
Discussion
Based on the data from our literature search made in PubMed with the Keywords radial neck fracture, nonunion, delayed union and pseudarthrosis after conservative treatment, isolated and adult, we recommend conservative treatment in asymptomatic patients. In patients with clinical symptoms, conservative treatment should be performed for a period of 6 months. If symptoms remain after this time, revision surgery with ORIF should be performed. In patients who have severe symptoms or physically demanding work that makes conservative treatment for 6 months unacceptable, ORIF may be performed earlier.
In symptomatic patients of any age with nonunion and physically demanding work, a revision surgery with ORIF may lead to better clinical results compared with conservative treatment. However, in patients older than 30 years who perform low-demand activities, conservative treatment may be of value.
The two patients reported here with isolated delayed union/nonunion of the radial neck both remained symptomatic after 4–6 months of conservative treatment. Delayed union/nonunion was proven by CT imaging in each. Therefore, operative stabilization was proposed to both patients, and both consented because their ability to work was severely hampered.
Both patients had uneventful postoperative courses and fracture healing was achieved. The clinical outcome of one case was excellent after 1 year except for some slight pain after strenuous exercise. The second case still had some pain with weather changes and with strenuous exercise, but after partial metal removal (leaving two broken screws in situ), the symptoms disappeared. Systemic etiological factors which might promote delayed union or nonunion, such as malnutrition, osteoporosis, nicotine abuse, diabetes and prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDS), were ruled out in both cases [7]. Furthermore, local factors, like poor bone contact, poor vascularity or infection, were identified in neither patient. Biomechanical instability due to the inability to comply with the non-weight-bearing regimen during conservative treatment seems to be the only common causative factor in both cases. Both patients were noncompliant with immobilization and non-weight bearing instructions due to their part-time occupations (installation electrician and carpenter).
From the literature search, analysis of the six symptomatic cases with complete information that were surgically treated revealed that all had professions with relatively strenuous activities. In only one case, the profession was not reported. Surgical intervention due to persistent pain was employed at a mean of 7.4 months (5–12) after the original accidents (Table 2). In the conservative group, six of ten remained asymptomatic: one office worker, one homemaker and two retired individuals (occupation not reported for two cases). In the symptomatic group, one was a physician; one, a homemaker; and one retired (occupation not reported for one case). Whether occupations with higher demands lead to more symptomatic nonunions compared with lower demand professions cannot be determined from these data due to the small patient population and incomplete information.
Conservative treatment protocols were very heterogeneous in the reported cases, and no conclusion for a preferred treatment modality could be derived.
It could be hypothesized that the natural history of radial neck delayed unions or nonunions is benign due to the rich, independent vascularization of the radial head and neck, which precludes necrosis and atrophy of the radial head. Recent injection studies by Yamaguchi et al. demonstrate high vascularization with a dual extraosseous blood supply: on one side from a branch of the radial recurrent artery with a direct supply to the radial head, and on the other side vessels from the radial artery and the interosseous recurrent artery that penetrate the capsular insertion at the radial neck [8]. The radial head remains as a biologic spacer and, even after a nonunion, it seems to be functionally sufficient in some patients, not causing relevant symptoms or functional impairment.
Three different operative treatment modalities were employed in the reported series. Radial head resection was performed in three cases. In the past, this was a standard procedure for the treatment of comminuted radial head fractures, but it was used in this population to treat symptomatic delayed union/nonunion. There are reports of good functional outcome after radial head resection [9]; however, residual pain, decreased strength, osteoarthrosis, joint instability, proximal radial translation and cubitus valgus have also been observed as late sequelae [9]. In the acute setting, radial head excision is contraindicated when there are associated osteo-ligamentous injuries, as in the case of a terrible triad or a medial collateral ligament rupture [10]. In the three cases treated by resection, it can be assumed that elbow joint stability was not a concern because the resections were performed 6–7 months after the accidents.
The insertion of a cancellous bone graft using a press fit technique seems appealing as long as there is an intact connection between the head and neck and it is confirmed intraoperatively that the head stays connected with the shaft during pronation and supination. This treatment modality was used in three cases. In one case, it was combined with K-wire fixation [11]. This flexible fixation resulted in bone healing. The healing even after flexible or no fixation was also demonstrated by Neumann et al., who treated 12 Mayson III fractures by fixing just the fragmented head with screws without combining the radial head to the shaft by an implant when the radial head rotated together with the shaft during intraoperative pronation and supination. After a mean follow-up of 7.8 years (4–114 m), they demonstrated that 11 out of 12 fractures had healed without problems [12]. Due to good vascularization, a radial neck fracture may heal if it is protected from relevant shearing forces even when not rigidly fixed. This patient population was treated by immobilization for 6 weeks with intermittent protected range of motion exercises during this time.
Surprisingly, only one patient in the reviewed cases underwent ORIF using K-wires. Nowadays, ORIF is the treatment of choice for displaced radial head and neck fractures if stable reconstruction is possible. The radial head remains in place as an osseous stabilizer and allows for healing of the associated medial collateral ligament if injured. Ikeda et al. showed that patients treated by ORIF had satisfactory joint motion with better function and greater strength compared with patients who underwent radial head resection [9]. Implant removal is often necessary when using ORIF with a plate for fracture stabilization [13] which is a drawback for this kind of fixation. Radial head necrosis is another rare sequelae after plate fixation of the radial neck [12].
Biomechanical studies reveal no significant difference regarding strengths and stiffness for transverse non-comminuted radial neck fracture fixation when using crossed oblique screws compared to plate fixation [14]. Clinical studies [13, 15] favor simple cross-screw fixation for transverse radial neck fractures due to the fact that they have a better functional outcome regarding forearm motion, less heterotopic ossification, less risk of compromise of the posterior interosseous nerve and less need for implant removal. Therefore, in nonunion with limited bone loss (Case 1) an in situ fixation with oblique screws is preferred. However, when a pseudarthrosis of the radial neck results in bone loss with the need of a bone graft to restore anatomy, plate fixation is mandatory (Case 2) to achieve a stable fixation.
Limitations of this study include its retrospective design, the limited number of patients (with incomplete information in 6/17 cases) and lack of a control group. However, radial neck delayed union/nonunion is a rare clinical entity which may also be underreported. Due to the sparse and inhomogeneous case reports in the literature, no predominant systemic or local etiologic factors could be identified. Strenuous manual labor demands and noncompliance with conservative management protocols are reasons to change to operative treatment even in the situation of a delayed union, without waiting for potential healing. However, conservative treatment seems the preferred treatment of choice in patients who remain non- or oligosymptomatic irrespective of the time since the accident.
The factor leading to nonunion in the two presented cases from our institution appears to be that both patients could not follow the suggested non-weight bearing protocol for their affected extremity. We hypothesize that this increased local instability resulted in a symptomatic delayed union. The clinical results in both surgically treated patients were good. However, data from different reviewed case reports do not allow for a valid conclusion with respect to the ideal time point to switch from conservative to operative treatment for a symptomatic delayed union/nonunion.
Conservative treatment remains the treatment of choice for isolated radial neck delayed union/nonunion in adults, since healing in two out of 10 cases was observed even after 7 and 20 months. Symptomatic nonunion, which limits functional capacity, however, is a good indication for operative treatment, showing favorable results with return to full function. The type of fixation—simple cross-screw fixation or plate fixation—depends on the amount of bone loss at the radial neck and the need of bone graft to restore anatomy.
Conclusion
Delayed union/nonunion of isolated radial neck fractures after conservative treatment are rare. Most patients are asymptomatic or have minimal symptoms, depending on their functional demands. Surgical treatment should be considered for patients with symptomatic delayed union/nonunion, especially for those with high-demand occupations. Clinical outcome seems favorable for this group of patients.
References
Morrey BF, An KN (2009) In: Morrey BF, Sanchez-Soleto (eds) The elbow and its disorders: functional evaluation of the elbow, 4th edn. WB Saunders, Philadelphia, pp 82–92
Hudak PL, Amadio PC, Bombardier C (1996) Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder, and head). Am J Ind Med 29:602–608
Ring D, Psychoyios VN, Chin KR, Jupiter JB (2002) Nonunion of nonoperatively treated fractures of the radial head. Clin Orthop Relat Res 398:235–238
Duckworth A, Clement N, Jenkins P (2012) ScienceDirect.com—The Journal of Hand Surgery—The Epidemiology of Radial Head and Neck Fractures. J Hand Surg 37A:112–119
Thomas TT (1907) Fractures of the head and neck of the radius. Ann Surg 46:280–291
Bhandari M, Fong K, Sprague S, Williams D, Petrisor B (2012) Variability in the definition and perceived causes of delayed unions and nonunions. A cross-sectional, multinational survey of orthopaedic surgeons. J Bone Jt Surg 94:e109(1-6)
Castillo RC, Bosse MJ, MacKenzie EJ, Patterson BM, LEAP Study Group (2005) Impact of smoking on fracture healing and risk of complications in limb-threatending open tibia fractures. J Orthop Trauma 19:151–157
Sweet FA, Bindra R, Morrey BF, Gelberman RH (1997) The extraosseous and intraosseous arterial anatomy of the adult elbow. J Bone Joint Surg Am 79:1653–1662
Ikeda M, Sugiyama K, Kang C, Takagaki T, Oka Y (2005) Comminuted fractures of the radial head. Comparison of resection and internal fixation. J Bone Jt Surg Am 87:76–84. doi:10.2106/JBJS.C.01323
Duckworth AD, McQueen MM, Ring D (2013) Fractures of the radial head. Bone Jt J 95-B:151–159. doi:10.1302/0301-620X.95B2.29877
Cha S-M, Shin H-D, Kim K-C, Song J-H (2013) Non-union of isolated radial neck fracture using a bone graft and temporary K-wire fixation: a case report. Hand Surg 18:389–392. doi:10.1142/S0218810413720210
Neumann MM, Nyffeler RR, Beck MM (2011) Comminuted fractures of the radial head and neck: is fixation to the Shaft necessary? J Bone Jt Surg Br 93:223–228. doi:10.1302/0301-620X.93B2.24760
Li SL, Lu Y, Wang MY (2015) Is cross-screw fixation superior to plate for radial neck fractures? Bone Jt J 97-B:830–835
Gutowski CJ, Darvish K, Ilyas AM, Jones CM (2015) Comparison of crossed screw versus plate fixation for radial neck fractures. Clin Biomech 30:966–970
Smith AM, Morrey BF, Steinmann SP (2007) Low profile fixation of radial head and neck fractures: surgical technique and clinical experience. J Orthop Trauma 10:718–724
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
There is no funding source.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Babst, C., Brunner, A. & Babst, R. Isolated radial neck delayed union/nonunion after conservative treatment in adults: two case reports and a literature review. Arch Orthop Trauma Surg 138, 179–188 (2018). https://doi.org/10.1007/s00402-017-2805-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-017-2805-9