Abstract
Purpose
Cemented unicompartmental knee replacement (UKR) has proven excellent long-term survival rates and functional scores in Price et al. (Clin Orthop Relat Res 435:171–180, 2005), Price and Svard (Clin Orthop Relat Res 469(1):174–179, 2011) and Murray et al. (Bone Joint Surg Br 80(6):983–989, 1998). The main causes for revision, aseptic loosening and pain of unknown origin might be addressed by cementless UKR in Liddle et al. (Bone Joint J 95-B(2):181–187, 2013), Pandit et al. (J Bone Joint Surg Am 95(15):1365–1372, 2013), National Joint Registry for England, Wales and Northern Ireland: 10th Annual Report 2013 (http://www.njrcentre.org.uk/njrcentre/Portals/0/Documents/England/Reports/10th_annual_report/NJR%2010th%20Annual%20Report%202013%20B.pdf, 2013), Swedish Knee Arthroplasty Register: Annual Report 2013 (http://www.myknee.se/pdf/SKAR2013_Eng.pdf, 2013).
Methods
This single-centre retrospective cohort study reports the 5-year follow-up results of our first 30 consecutively implanted cementless Oxford UKR (OUKR). Clinical outcome was measured using the OKS, AKSS, range of movement and level of pain (visual analogue scale). The results were compared to cemented OUKR in a matched-pair analysis.
Results
Implant survival was 89.7%. One revision each was performed due to tibial fracture, progression of osteoarthritis (OA) and inlay dislocation. The 5-year survival rate of the cementless group was 89.7% and of the cemented group 94.1%. Both groups showed excellent postoperative clinical scores.
Conclusions
Cementless fixation shows good survival rates and clinical outcome compared to cemented fixation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to recent registry data, the use of cemented UKR ranges between 5 and 10% of all knee arthroplasties performed [7,8,9]. The cemented OUKR proved to be reliable in terms of implant survival as well as functional outcome in trials by both designing centres as well as independent studies [1,2,3, 10].
Registry data show aseptic loosening of the tibial component and pain as the most common causes for revision in cemented OUKR. Component loosening is often caused by incorrect seating of the implant or micromotion causing a fibrous tissue layer between cement and bone that might inhibit secure fixation [11]. To foster bone ingrowth, the cementless prosthesis is coated with porous titanium and hydroxyapatite, with the aim for permanent biological fixation with excellent clinical results [12].
First studies about cementless OUKR have shown equally good clinical outcome and survival rates compared to the cemented version and higher survival than other cementless implants such as the Alpina prosthesis [4, 5, 13,14,15,16,17,18].
Nevertheless, there are reports raising concern about tibial plateau fractures and tibial valgus subsidence leading to revision in cementless fixation. Tibial plateau fractures seem to be more common in cementless UKR and they are associated with an extended sagittal saw cut, improper preparation of the tibia and low bone density [19]. Valgus subsidence in cementless OUKR may be caused by laterally implanted femoral components, causing mediolateral micromotion and impingement of the inlay against the medial tibial wall [11, 12].
The purpose of this study was to assess the mid-term clinical results, the survival rates and the complications of the first 30 knees treated consecutively with cementless OUKR at an independent centre. We also compared the clinical results to a cemented collective with a matched pair analysis.
Patients and methods
The institutional review board of the University of Heidelberg approved all procedures (S-546/2013), and the study was conducted in accordance with the Helsinki Declaration of 1964, as revised in 2013. Informed consent was obtained from all individual participants included in the study.
This single-centre cohort study includes the first 30 cementless OUKR implanted in 27 patients consecutively between 2007 and 2009 at our institution. All patients suffered from anteromedial osteoarthritis (AMOA). In all cases, the anterior cruciate ligament (ACL) and collateral ligaments were intact and the varus deformity was manually fully correctable. A previous osteotomy or a flexion deformity >15° was considered contraindications, whereas cartilage loss in the patello-femoral joint, obesity and age were not considered contraindications [20].
Implant design and implantation
The cementless implantation was performed by three orthopaedic consultants experienced in the Oxford Phase III unicompartimental knee prosthesis (Biomet UK Ltd, Swindon, United Kingdom) [21]. A few changes were made by the developing centres to allow cementless implantation: the weight bearing surfaces are coated with calcium hydroxyapatite (HA), and the cement pockets on both components are filled with porous titanium. The cut for the tibial keel is narrower than in the cemented model to ensure a tight press-fit and the cementless prosthesis is implanted in a more flexed knee position, so that the femoral part extends a further 17° anteriorly. The femoral component has two cylindrical HA-coated pegs to impede rotational stress on the implant [4, 5].
For clinical assessment, the range of motion (ROM), Oxford Knee Score (OKS, measured on a scale from 0 to 48 points) and the American Knee Society Score (AKSS) were tested pre- and postoperatively. The pain level was evaluated on a visual analogue scale (VAS). Revision was defined as any surgery with the exchange or removal of at least one part of the implant. Reoperation includes revisions as well as any other surgical procedures. Survival for the endpoints revision and reoperation was calculated using Kaplan–Meier Analysis.
In a matched-pair analysis, implant survival and clinical outcome of the cementless group were compared to a group of 30 patients with cemented OUKR who were implanted at our institution between 2001 and 2009. Patients were matched for sex, age and BMI as well as preoperative OKS score [5, 14].
Statistics
Data were described and analysed using IBM SPSS Statistics 21 (SPSS Inc., Somers, NY). We performed a power analysis to determine the number of patients needed to detect significant differences. As a far higher number of implants per group would be needed, we decided not to perform t test analysis. Values will be presented in total numbers or percent in combination with the range, standard deviation, and the 95% confidence interval.
Results
The results of this study are to be interpreted in the context of an early exploratory study. The cementless group consisted of 30 OUKR, implanted in 27 patients (15 male, 12 female). Mean age at surgery was 62.5 years (49–76) and mean follow-up time was 60.0 months (range 47–69; SD 8.3). No patient died or was lost to follow-up. One knee was excluded from the study, since it had not been implanted in accordance with the Oxford manual of surgical technique.
Survival rate
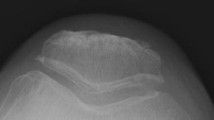
Two knees were excluded from clinical evaluation due to early revision (see Fig. 1). Overall, 5 years after implantation, three knees have undergone revision (see Table 1): There was one case of periprosthetic tibial plateau fracture within the first month after implantation. It was revised to a cemented tibial component and ORIF. The second patient was revised to a total knee replacement due to progressive OA of the lateral compartment and the patello-femoral joint (PFJ) 26 months after implantation. The third revision was due to a mobile-bearing dislocation that occurred 21 months after surgery. The bearing was exchanged to a thicker one. The remaining 27 knees were assessed clinically and radiologically 3 months, 1 and 5 years postoperatively. Additionally, one reoperation was performed due to OA of the PFJ. The patient was provided a femoro-patellar arthroplasty in addition to her OUKR without exchanging any of the previously implanted components. There was no tibial or femoral loosening in this study. Five-year survival rate with revision as endpoint was 89.7% (95% CI 0.79–1.0) (see Fig. 2), with reoperation it was 86.2% (95% CI 0.74–0.99). All reoperations occurred within the first 2 years after index surgery.
Clinical outcome
In the cementless group, all clinical and functional variables improved strongly from pre- to postoperative results (see Fig. 3). The mean OKS was 27.2 points (SD 6.4, 95% CI 24.6–29.7) pre-operatively and 42.1 points (SD 7.6, 95% CI 29.1–45.1) postoperatively, with a mean change of 15.0 points (SD 7.9, 95% CI 11.8–18.1). The mean AKSS-O improved from 50.7 before surgery (SD 13.3, 95% CI 45.4–56.0) to 92.7 after surgery (SD 10.7, 95% CI 88.5–96.9), with a mean increase of 42 points (SD 18.5, 95% CI 34.7–49.3).
Matched pair
The matched-pair collective was well matched for age, sex, BMI and preoperative OKS. AKSS-O improved in both groups after surgery, whereby the improvement did not differ more than one point between the groups. The cementless group improved in the pain score more distinct than the cemented group (ΔVAS 6.1 vs. 5.4), while the cemented group showed higher improvement in the ROM (ΔROM 15.1 vs. 8.0) (see Table 2). In the cemented collective, one revision was performed due to a posttraumatic tibial fracture. It was treated with ORIF and TKR. One reoperation had to be performed due to small cement bodies in the joint space. A therapeutic arthroscopy was performed and the cement was removed (see Table 2). The 5-year survival rate with revision as endpoint is 94.1% (95% CI 0.83–1.0); with reoperation as endpoint, it is 91.0% (95% CI 0.78–1.0).
Discussion
In this independent study, we enrolled the first 30 OUKR (27 patients) implanted consecutively in our hospital. With a mean follow-up of 5 years, we evaluated the clinical outcome using the OKS, AKSS, ROM and level of pain. Outcome and implant survival rate were compared to cemented medial OUKR in a matched-pair analysis.
The findings of our study show good clinical and functional outcome after cementless OUKR compared to cemented fixation. The cemented and the cementless group showed a strong improvement of AKSS-O and OKS-scores [ΔAKSS-O cemented: 41.1 (95% CI 34.6–48.3)]; ΔAKSS-O cementless: 42.0 (95% CI 34.7–49.3); ΔOKS cemented and cementless: 15.0, (95% CI cementless: 95% CI 11.8–18.1; 95% CI cemented: 11.6–18.5). Our findings are in line with prospective randomized studies comparing cemented and cementless OUKR by other authors as well as retrospective studies, e.g., by Akan et al. [5, 14, 16, 22, 23].
Kendrick et al. conducted one of the few prospective randomized studies comparing cemented and cementless OUKR. While their number of analysed cementless OUKR (n = 22) was relatively low and the mean age of the patients receiving cementless treatment was more than 5 years older than in our study (67.6 years), the 2-year follow-up examination shows a slightly higher improvement of OKS (17.7) than in our study and no significant difference from the cemented group [23].
Survival rates in our study were 89.7% in the cementless group and 94.1% in the cemented group. They seem rather low compared to literature findings of cemented OUKR, which range between 95 and 99% [1, 3, 24]. This might be ascribed to the fact that we included the 30 first patients consecutively operated with the cementless OUKR in our hospital. Considering the learning curve with the cementless system (Oxford Phase III), higher survival rates can be estimated with higher numbers of surgery performed [25,26,27,28,29].
None of the main reasons for revision of cemented OUKR (tibial or femoral loosening, pain of unknown origin) were encountered in our study [9]. However, neither did we see tibial component loosening nor pain of unknown origin in our cemented matched-pair collective, while Liddle et al. and Pandit et al. stated that the main causes of revision in cemented OUKR can be avoided by cementless fixation [4, 5]. Additionally, complications that are directly associated with cementation were avoided, whereas in the cemented collective one reoperation was performed due to small cement bodies. Main reasons for revision in this study were progress of OA of other knee compartments, tibial plateau fracture, and inlay dislocation (each one case = 3.4%). Complications found in our study correspond to the findings of Liddle et al., who stated the main causes for revision in cementless UKR to be progression of OA (0.6%), bearing dislocation (0.6%), fracture (0.4%) and infection (0.03%).
Cementless fixation so far renders survival rates between 95 and 100% in follow-up periods ranging between 1 and 6 years [4, 5, 13, 14, 16, 30,31,32]. In a systematic review by Campi et al., the overall survival rate for various cementless prosthetic designs was 90–99% at 5 years and 92–97% at 10 years [22]. It is difficult to compare these results with the present study, as the published studies are either conducted by developing centres [4, 5, 16], have shorter follow-up periods [13, 30, 31] or include other implant designs [22]. The lack of comparable studies puts emphasis on the conduction of randomised controlled trials from independent centres.
A prospective observational study conducted by Hooper et al. at an independent centre in New Zealand presents the radiological outcome of 150 OUKR and renders a 5-year revision rate of 2 out of 125 patients (1.6%). The authors of this study ascribe the low revision rate to the high number of annual arthroplasties performed by their surgeons rather than to a learning curve for cementless fixation, with an average of 82–106 arthroplasties performed by each surgeon per year. The weakness of this study is its high number of patients lost to follow-up (25 knees). While the overall arthroplasties performed per surgeon per year are comparable to our study, no patient was lost to follow-up, therefore minimizing the bias of this study [32].
In cementless implantation, tibial plateau fractures are a serious complication. Cadaveric studies have shown that the cementless OUKR is more susceptible to periprosthetic tibial plateau fractures than cemented prostheses, especially when accompanied by an extended sagittal saw cut and decreased bone mineral density [8, 19]. Due to the cementless fixation, more impaction is needed to insert the components with satisfactory primary fit which might increase the risk of consecutive tibial fracture. The careful preparation of the tibial plateau and the following press-fit are challenging procedures and have to be practised. As this study assessed the outcome of the first thirty patients in our hospital treated with a cementless implant, we expect the incidence of tibial plateau fractures to decrease with growing numbers of implants.
The main weakness of our study is the small number of knees analysed. The surgeons’ learning curve could have a big influence on the results. Furthermore, the study was designed with a retrospective design, so that selection bias could have influenced the results. Therefore, a prospective study design is currently being set up to avoid these disadvantages and obtain more valid information.
The main strength of this study is that no patient died or was lost to follow-up. All the patients were operated by the same experienced surgeons and got the same post-rehabilitation support. Furthermore, our department has a detailed arthroplasty registry so that the cemented collective could be matched very specifically. In addition, this study was completed in an independent centre showing that the cementless OUKR can be implanted successfully outside the designing centres. The study is among the first trials for cementless OUKR performed with a 5-year follow-up.
Conclusions
Cementless OUKR is a safe treatment of anteromedial OA, with excellent clinical outcome compared to cemented OUKR. There seems to be no difference in the implant survival. Aseptic loosening did not occur in the cementless group of our study, which shows that cementless fixation seems to be a safe and reliable alternative to cemented OUKR. Tibial plateau fractures are a serious complication. The surgical technique is crucial for the success of implantation. To minimize revisions and complications, surgeons should be encouraged to participate in training programmes for cementless OUKR.
References
Price AJ, Waite JC, Svard U (2005) Long-term clinical results of the medial Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res 435:171–180
Price AJ, Svard U (2011) A second decade lifetable survival analysis of the Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res 469(1):174–179. doi:10.1007/s11999-010-1506-2
Murray DW, Goodfellow JW, O’Connor JJ (1998) The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg Br 80(6):983–989
Liddle AD, Pandit H, O’Brien S, Doran E, Penny ID, Hooper GJ, Burn PJ, Dodd CA, Beverland DE, Maxwell AR, Murray DW (2013) Cementless fixation in Oxford unicompartmental knee replacement: a multicentre study of 1000 knees. Bone Joint J 95-B(2):181–187. doi:10.1302/0301-620X.95B2.30411
Pandit H, Liddle AD, Kendrick BJ, Jenkins C, Price AJ, Gill HS, Dodd CA, Murray DW (2013) Improved fixation in cementless unicompartmental knee replacement: five-year results of a randomized controlled trial. J Bone Joint Surg Am 95(15):1365–1372. doi:10.2106/JBJS.L.01005
Porter M (2013) National Joint Registry for England, Wales and Northern Ireland: 10th Annual Report 2013. http://www.njrcentre.org.uk/njrcentre/Portals/0/Documents/England/Reports/10th_annual_report/NJR%2010th%20Annual%20Report%202013%20B.pdf. Accessed 08 Aug 2016
Sundberg M (2012) Swedish Knee Arthroplasty Register: Annual Report 2013. http://www.myknee.se/pdf/SKAR2013_Eng.pdf. Accessed 08 Aug 2016
Clarius M, Haas D, Aldinger PR, Jaeger S, Jakubowitz E, Seeger JB (2010) Periprosthetic tibial fractures in unicompartmental knee arthroplasty as a function of extended sagittal saw cuts: an experimental study. Knee 17(1):57–60. doi:10.1016/j.knee.2009.05.004
Rothwell A, Hobbs T, Frampton C (2012) The New Zealand Joint Registry. Thirteen year report: January 1999 to December 2011. New Zeeland Orthopaedic Association. http://nzoa.org.nz/system/files/NJR%2013%20Year%20Report.pdf
Vorlat P, Putzeys G, Cottenie D, Van Isacker T, Pouliart N, Handelberg F, Casteleyn PP, Gheysen F, Verdonk R (2006) The Oxford unicompartmental knee prosthesis: an independent 10-year survival analysis. Knee Surg, Sports Traumatol, Arthrosc 14(1):40–45. doi:10.1007/s00167-005-0621-1
Yildirim G, Gopalakrishnan A, Davignon RA, Parker JW, Chawla H, Pearle AD (2016) comparative fixation and subsidence profiles of cementless unicompartmental knee arthroplasty implants. J Arthroplast 31(9):2019–2024. doi:10.1016/j.arth.2016.02.034
Liddle AD, Pandit HG, Jenkins C, Lobenhoffer P, Jackson WF, Dodd CA, Murray DW (2014) Valgus subsidence of the tibial component in cementless Oxford unicompartmental knee replacement. Bone Joint J 96-B (3):345–349. doi:10.1302/0301-620X.96B3.33182
Pandit H, Jenkins C, Beard DJ, Gallagher J, Price AJ, Dodd CA, Goodfellow JW, Murray DW (2009) Cementless Oxford unicompartmental knee replacement shows reduced radiolucency at one year. J Bone Joint Surg Br 91(2):185–189. doi:10.1302/0301-620X.91B2.21413
Akan B, Karaguven D, Guclu B, Yildirim T, Kaya A, Armangil M, Cetin I (2013) Cemented versus uncemented Oxford unicompartmental knee arthroplasty: is there a difference? Adv Orthop 2013:245915. doi:10.1155/2013/245915
Emerson RH Jr, Higgins LL (2008) Unicompartmental knee arthroplasty with the oxford prosthesis in patients with medial compartment arthritis. J Bone Joint Surg Am 90(1):118–122. doi:10.2106/JBJS.F.00739
Pandit HG, Campi S, Hamilton TW, Dada OD, Pollalis S, Jenkins C, Dodd CA, Murray DW (2015) Five-year experience of cementless Oxford unicompartmental knee replacement. Knee Surg, Sports Traumatol, Arthrosc. doi:10.1007/s00167-015-3879-y
W-Dahl A, Robertsson O, Lidgren L (2010) Surgery for knee osteoarthritis in younger patients. Acta Orthop 81(2):161–164
Lecuire F, Berard JB, Martres S (2014) Minimum 10-year follow-up results of ALPINA cementless hydroxyapatite-coated anatomic unicompartmental knee arthroplasty. Eur J Orthop Surg Traumatol 24(3):385–394. doi:10.1007/s00590-013-1192-3
Seeger JB, Haas D, Jager S, Rohner E, Tohtz S, Clarius M (2012) Extended sagittal saw cut significantly reduces fracture load in cementless unicompartmental knee arthroplasty compared to cemented tibia plateaus: an experimental cadaver study. Knee Surg, Sports Traumatol, Arthroscop 20(6):1087–1091. doi:10.1007/s00167-011-1698-3
Pandit H, Jenkins C, Gill HS, Smith G, Price AJ, Dodd CA, Murray DW (2011) Unnecessary contraindications for mobile-bearing unicompartmental knee replacement. J Bone Joint Surg Br 93(5):622–628. doi:10.1302/0301-620X.93B5.26214
Walker T, Streit MR, Gotterbarm T, Aldinger PR (2015) Tips and tricks for mobile bearing medial unicondylar knee replacement. Zeitschrift fur Orthopadie und Unfallchirurgie 153(3):331–333. doi:10.1055/s-0035-1546011
Campi S, Pandit HG, Dodd CA, Murray DW (2016) Cementless fixation in medial unicompartmental knee arthroplasty: a systematic review. Knee Surg, Sports Traumatol, Arthroscop. doi:10.1007/s00167-016-4244-5
Kendrick BJ, Kaptein BL, Valstar ER, Gill HS, Jackson WF, Dodd CA, Price AJ, Murray DW (2015) Cemented versus cementless Oxford unicompartmental knee arthroplasty using radiostereometric analysis: a randomised controlled trial. Bone Joint J 97-B(2):185–191. doi:10.1302/0301-620X.97B2.34331
Pandit H, Jenkins C, Barker K, Dodd CA, Murray DW (2006) The Oxford medial unicompartmental knee replacement using a minimally-invasive approach. J Bone Joint Surg Br 88(1):54–60. doi:10.1302/0301-620X.88B1.17114
Robertsson O, Knutson K, Lewold S, Lidgren L (2001) The routine of surgical management reduces failure after unicompartmental knee arthroplasty. J Bone Joint Surg Br 83(1):45–49
Rees JL, Price AJ, Beard DJ, Dodd CA, Murray DW (2004) Minimally invasive Oxford unicompartmental knee arthroplasty: functional results at 1 year and the effect of surgical inexperience. Knee 11(5):363–367. doi:10.1016/j.knee.2003.12.006
Robertsson O, Bizjajeva S, Fenstad AM, Furnes O, Lidgren L, Mehnert F, Odgaard A, Pedersen AB, Havelin LI (2010) Knee arthroplasty in Denmark, Norway and Sweden. A pilot study from the Nordic Arthroplasty Register Association. Acta Orthop 81(1):82–89. doi:10.3109/17453671003685442
Robertsson O, Lidgren L (2008) The short-term results of 3 common UKA implants during different periods in Sweden. J Arthroplast 23(6):801–807. doi:10.1016/j.arth.2007.07.011
Zhang Q, Zhang Q, Guo W, Liu Z, Cheng L, Yue D, Zhang N (2014) The learning curve for minimally invasive Oxford phase 3 unicompartmental knee arthroplasty: cumulative summation test for learning curve (LC-CUSUM). J Orthop Surg Res 9:81. doi:10.1186/s13018-014-0081-8
Hooper GJ, Maxwell AR, Wilkinson B, Mathew J, Woodfield TB, Penny ID, Burn PJ, Frampton C (2012) The early radiological results of the uncemented Oxford medial compartment knee replacement. J Bone Joint Surg Br 94(3):334–338. doi:10.1302/0301-620X.94B3.27407
Kerens B, Schotanus MG, Boonen B, Boog P, Emans PJ, Lacroix H, Kort NP (2016) Cementless versus cemented Oxford unicompartmental knee arthroplasty: early results of a non-designer user group. Knee Surg, Sports Traumatol, Arthrosc. doi:10.1007/s00167-016-4149-3
Hooper N, Snell D, Hooper G, Maxwell R, Frampton C (2015) The five-year radiological results of the uncemented Oxford medial compartment knee arthroplasty. Bone Joint J 97-B(10):1358–1363. doi:10.1302/0301-620X.97B10.35668
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
Tobias Gotterbarm has received payment from Zimmer Biomet and DePuy for a presentation and from Springer for a book section. He also received other financial support from Aesculap AG Germany. For another study, he and Tilman Walker were supported from Zimmer Biomet as a Principal Investigator.
Rights and permissions
About this article
Cite this article
Panzram, B., Bertlich, I., Reiner, T. et al. Cementless Oxford medial unicompartimental knee replacement: an independent series with a 5-year-follow-up. Arch Orthop Trauma Surg 137, 1011–1017 (2017). https://doi.org/10.1007/s00402-017-2696-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-017-2696-9