Abstract
Purpose
The purpose of the study was to evaluate the position of the subscapular nerves relative to surgical landmarks during exposure and to analyze the pattern of innervation of the subscapularis to avoid injury during anterior shoulder surgery.
Methods
20 embalmed human cadaveric shoulder specimens were used in the study. The muscular insertions of the subscapular nerves were marked and their closest branches to the musculotendinous junction and the coracoid process were measured in horizontal and vertical distances. In addition, the innervation pattern of each specimen was documented.
Results
14/20 specimens showed an innervation of the subscapularis with an upper, middle and lower subscapular nerve branch. Even though the nerve branches were in average more than 2 cm medial to the musculotendinous junction, minimal distances of 1.1–1.3 cm were found. The mean vertical distance as measured from the medial base of the coracoid to the nerve innervation point into the muscle was 0.7 cm for the upper nerve branch, 2.2 cm for the middle nerve branch and 4.4 cm for the lower nerve branch.
Conclusions
The subscapularis has a variable nerve supply, which increases the risk of muscle denervation during open shoulder surgery. Dissection or release should be avoided at the anterior aspect of the subscapularis muscle more than 1 cm medial to the musculotendinous junction. In approaches with a horizontal incision of the subscapularis, splitting should be performed at a vertical distance of 3.2–3.6 cm to the coracoid base to avoid iatrogenic subscapular nerve injuries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The anterior (deltopectoral) approach of the shoulder allows an access to the anterior, medial and lateral aspects of the glenohumeral joint, and is, therefore, often preferred for surgical exposure in open instability repair, rotator cuff repair, shoulder replacement and proximal humeral fracture treatment [1–3]. An insufficiency or dysfunction of the subscapularis is a commonly described postoperative complication after these types of open shoulder surgery [4–10], which can lead to severe functional limitations in patients, because the subscapularis plays a vital role in shoulder function as an important internal rotator and active anterior stabilizer of the glenohumeral joint, composing the anterior part of the transverse force couple [11–15]. Its insufficiency has been attributed to failure of tendon repair, postoperative muscular degeneration and the likelihood of denervation during release and mobilization of the musculotendinous unit [8, 9, 16]. To enter the joint, the subscapularis has to be identified, divided and reflected from the underlying joint capsule. Different incision and tenotomy techniques of the subscapularis have been described, which may not disturb the integrity of the musculotendinous unit and, thus, limit the postoperative risk of subscapularis insufficiency [5, 7, 17, 18]. The commonly described nerve supply of the subscapularis includes the lower and upper subscapular nerve, which have been the subject of previous cadaveric studies [19–24], with only a few describing the anatomy of the nerves and their location relative to surgical landmarks like the glenoid rim and the coracoid process [20, 24–26]. Other than previous studies, the present study aimed to describe the position of the subscapular nerve branches relative to the musculotendinous junction, which represents an important and well-visible landmark during surgical exposure and the entrance positions of the nerve branches in vertical relation to the coracoid base under the aspect of different incision and tenotomy techniques of the subscapularis. Moreover, the study aims to evaluate the prevalence and distribution patterns of the subscapularis nerve supply with the purpose to avoid injury during release.
Materials and methods
20 embalmed human cadaveric shoulder specimens were used in the study. These were composed of 12 right and 8 left shoulders out of a total of 20 body donors (12 female, 8 male) with an average age of 82 years (range 64–92 years).
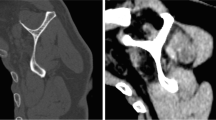
The same approach was taken in each specimen, which implied downward exposure and dissection of the deltoid groove and the detachment of the pectoralis major and the deltoid muscle from their origins at the clavicle and the acromion. Thereafter, the pectoralis minor and the conjoined tendon were retracted from the coracoid to expose the subscapularis and the brachial plexus, while preserving every neural structure entering the subscapularis muscle (Fig. 1).
Supplying branches of the subscapularis muscle were marked and retraced back to their origin. The branches’ pattern and their origin were documented in each shoulder. Muscular insertions of the nerve’s branches and also any additional branches were tagged at their closest entry points to the glenohumeral joint with a pin. Other pins were fixed at the medial base of the coracoid and in the transition zone of the musculotendinous junction of the subscapularis as presented in Fig. 2.
Marking of the entrance points of the upper (uE), middle (mE) and lower (lE) nerve branches with their closest distances to the musculotendinous junction (MJ) and the coracoid process (Co). Pc posterior cord of the plexus brachialis, suprascapular nerve black circle, axillary nerve black star, black line horizontal distance, black dotted line vertical distance)
Vertical and horizontal distances from the musculotendinous junction and the medial base of the coracoid process to the insertions of the nerve branches into the subscapularis, were taken in external rotation of the shoulder. The vertical distance was defined vertical to the horizontal measurement lines, along the course of the conjoint tendon (Fig. 2). In such cases where additional branches were present, the branches nearest to the medial coracoid base and the musculotendinous junction were chosen for measurement. The procedure was repeated and photographed for each specimen in a standardized fashion.
The mean, minimum, and maximum values as well as the standard deviation were calculated.
Analyses were performed in SPSS 23 (IBM Inc., Armonk, NY, USA). The institutional research board at the principal investigator’s hospital approved this study.
Results
14 specimens (70%) showed an innervation of the subscapularis limited to an upper subscapular nerve branch, a middle subscapular nerve branch and a lower subscapular nerve branch. An additional upper subscapular nerve branch was found in two specimens (10%) and an additional lower subscapular nerve branch was detected in four specimens (20%). The additional upper subscapular nerve branch originated in both specimens (10%) from the suprascapular nerve, the four additional lower subscapular nerve branches arose from the axillary nerve (20%). The posterior cord of the brachial plexus gave rise to the subscapular nerve branches in 14 specimens (70%); in four specimens, (20%) the lower nerve branch could be traced to the axillary nerve; and, in two specimens (10%), to the middle subscapular nerve.
The mean horizontal distance between the musculotendinous junction and the insertion point of the upper nerve branch into the subscapularis was 23.7 ± 6.1 mm (range 13.1–36.4 mm), to the insertion point of the middle nerve branch 25.3 ± 5.3 mm (range 11.4–34.3 mm) and to the lower nerve branch 24.3 ± SD 6.6 mm (range 13.4–38.2 mm). The horizontal distance from the medial coracoid base to the entry point of the upper nerve branch into the muscle was 31.8 ± 9.7 mm (range 16.4–46.0 mm) and the mean vertical distance was measured with 7.4 ± 4.5 mm (range 1.3–16.0 mm). The mean horizontal distance from the middle nerve branch entrance to the medial base of the coracoid process was 32.2 ± SD 8.2 mm (range 14.3–37.4 mm) and the mean vertical distance was measured with 22.1 ± SD 5.7 mm (range 11.0–31.3 mm). The mean distance between the entrance of the lower nerve branch and the medial coracoid base was 28.5 ± SD 10.5 mm (range 6.3–42.3 mm) and the mean vertical distance was measured with 44.4 ± SD 6.2 mm (range 37.0–57.0 mm). Table 1 presents an overview of the distances measured for the respective nerve branches.
Discussion
The present study confirms previous findings which suggest that the subscapularis muscle has a variable pattern of innervation [20, 25], even though in most cases, a single upper, middle and lower subscapular nerve branch were observed, which arose mostly from the posterior trunk of the brachial plexus. Despite the fact that the measured horizontal distances from the musculotendinous junction and the point of entry of the nerve branches into the subscapularis muscle in many cases appears to be sufficiently distant from the regular approaches—which in turn leads to the assumption that the risk of subscapular nerves injury is relatively low—our study shows that especially in cases of a subscapularis splitting or an inverted L-shaped tenotomy approach, the potential risk to denervate the subscapularis during release and mobilization of the musculotendinous unit is given.
While a former study found no signs of neurologic damage after total shoulder replacement using electromyographic assessment [8], many authors consider subscapularis nerve damage or denervation as a potential cause of joint instability and subscapularis dysfunction after anterior shoulder surgery [4, 7, 20, 27]. The subscapularis muscle is divided in an upper and lower portion based on previous biomechanical studies, which observed different functions of these units depending on shoulder position, whereas electromyographic and cadaveric investigations reported separate innervations [19, 28–31]. Based on these studies, different incision and tenotomy techniques of the subscapularis for entering the shoulder joint have been described. A complete tenotomy with a detachment of the musculotendinous insertion of the subscapularis 0.5–1 cm medial to the lesser tuberosity with a tendon-to-tendon repair is reported [32], as well as less-invasive approaches, like the inverted L-shaped tenotomy approach and the subscapularis splitting approach [7, 33]. While such types of approaches are designed to preserve the lower muscular attachment, our study shows that these exposures may also place the integrity and innervation of the lower and middle portion of the subscapularis muscle at risk. These results may be one reason for postoperative findings reporting of a loss of strength and degeneration of the subscapularis muscle belly after Latarjet procedure that used the inverted L-shaped tenotomy for exposure [18]. According to the vertical distances from the medial base of the coracoid process to the middle nerve branches, which were measured with 2.2 cm (range 1.1–3.1 cm) and to the lower subscapular nerve branch which were measured in mean with 4.4 cm (range 3.7–5.7 cm), a recommendation of a horizontal incision between 3.2 and 3.6 cm can be suggested as surgical guideline for safer surgery at the subscapularis muscle. From this point of view, a complete subscapularis tenotomy approach, which is often used in shoulder arthroplasty, seems to minimize the risk of denervation of the nerve branches. Different modifications like creating a musculotendinoperiosteal flap or osteotomy technique are reported [8, 34, 35].
In cases which necessitate a circumferential release of the subscapularis—for example in patients with internal rotation contractures—attention should be given to the nerve supply—especially while releasing at the anterior aspect of the subscapularis [7]. Therefore, the musculotendinous junction is a good intraoperative marker, which can be identified with ease when a deltopectoral approach is performed. Previous studies have described the position of the subscapular nerve in relation to other anatomical landmarks, like the glenoid rim or the coracoid process [24–26, 36]. However, in most cases, the glenoid rim cannot be traced through direct intraoperative visualization and the coracoid process alters its reference values depending on the relative arm position and the torn/retracted or released tendon of the subscapularis, which make these studies more useful when applying arthroscopic surgery or reconstruction of the acromioclavicular joint [37–39].
In the present study, the entry points of the subscapular nerve branches were measured to be in average more than 2 cm medial from the musculotendinous junction, with the minimum distance being 1.3 cm at the upper nerve branch, 1.1 cm at the middle nerve branch and 1.3 cm at the lower nerve branch. Based on these findings, dissection or release should be avoided at the anterior aspect of the subscapularis muscle more than 1 cm medial to the musculotendinous junction (Fig. 3).
Areas when dissecting or releasing the subscapularis muscle in distance to the musculotendinous junction (mj), with a safe zone (green), less then 1 cm, a risk zone (orange) 1–2 cm and a high-risk zone (red) more than 2 cm medial to the mj. If the interval between the junction of the superior two-thirds and the inferior one-third is exploited in line with its fibers [subscapularis split (red dotted line)], L-inverted approach (black)] a horizontal incision should be placed in a vertical distance (along the course of the conjoint tendon) of 3.2–3.6 cm to the coracoid base (cb)
Furthermore, we were able to show a variable nerve supply of the lower unit of the subscapularis, which was found with its origin from the posterior trunk of the brachial plexus in 14 specimens (70%), from the axillary nerve in four specimens (20%) and from the middle subscapular nerve in two specimens (10%). Moreover, in 4 specimens (20%), an additional lower nerve branch was found. This confirms previous studies which reported that the lower subscapular nerve originated from the axillary nerve in 55% [27], in 23% [25] and in 25% of cases [20]. The variability of additional lower nerve branches arising from the axillary nerve may account for the small distances in the group of the lower nerve branches. These more distal origins of the lower nerve may place the nerve supply closer to the surgical field, thereby placing it at greater risk during open shoulder surgery.
A possible drawback of the study is the fact that the specimens were embalmed, because during fixation, the tissue is dehydrated and shrinks, which may have a negative influence on the taken measurements of this study. A second limitation is the high average age (82 years) and the limited sample size of the specimens, which may lead to incorrect measurements when compared to the application of landmarks in patients of a significantly younger age. However, especially in anterior shoulder surgery for shoulder replacement and the treatment of a humeral fracture, it is true that the average age of patients does not significantly differ from the average age of our study group.
Nevertheless, the present results help to define a potential risk area for denervation of the subscapularis during surgical exposure. The risk of a subscapular nerve injury during anterior open shoulder surgery is a valid concern. Further research like electromyographic assessment after anterior shoulder surgery is necessary to evaluate whether nerve damage or denervation is a potential underdiagnosed cause of postoperative joint instability and subscapularis dysfunction.
Conclusion
The subscapularis shows variable patterns of innervation and entrance points of the nerve branches in relation to the musculotendinous junction, which enhances the risk to denervate the muscle during open anterior surgery of the shoulder. Dissection or release should be avoided at the anterior aspect of the subscapularis more than 1 cm medial to the musculotendinous junction. If the muscular interval between the junction of the superior two-thirds and inferior one-third is exploited in line with its fibers (subscapularis split, L-inverted approach), a horizontal incision should be performed in vertical distance of 3.2–3.6 cm to the coracoid base.
References
Harryman DT 2nd (1992) Common surgical approaches to the shoulder. Instruct Course Lect 41:3–11
Oppermann J, Celik E, Bredow J, Beyer F, Hackl M, Spies CK, Muller LP, Burkhart KJ (2016) Shoulder arthroplasty in Germany: 2005–2012. Archiv Orthop Trauma Surg 136(5):723–729
von Engelhardt LV, Manzke M, Filler TJ, Jerosch J (2015) Short-term results of the reverse Total Evolutive Shoulder System (TESS) in cuff tear arthropathy and revision arthroplasty cases. Arch Orthop Trauma Surg 135(7):897–904
Miller SL, Hazrati Y, Klepps S, Chiang A, Flatow EL (2003) Loss of subscapularis function after total shoulder replacement: A seldom recognized problem. J Shoulder Elbow Surg Am Shoulder Elbow Surg 12(1):29–34
Scheibel M, Tsynman A, Magosch P, Schroeder RJ, Habermeyer P (2006) Postoperative subscapularis muscle insufficiency after primary and revision open shoulder stabilization. Am J Sports Med 34(10):1586–1593
Sachs RA, Williams B, Stone ML, Paxton L, Kuney M (2005) Open Bankart repair: correlation of results with postoperative subscapularis function. Am J Sports Med 33(10):1458–1462
Scheibel M, Habermeyer P (2008) Subscapularis dysfunction following anterior surgical approaches to the shoulder. J Shoulder Elbow Surg Am Shoulder Elbow Surg 17(4):671–683
Gerber C, Yian EH, Pfirrmann CA, Zumstein MA, Werner CM (2005) Subscapularis muscle function and structure after total shoulder replacement with lesser tuberosity osteotomy and repair. J Bone Joint Surg Am 87(8):1739–1745
Greis PE, Dean M, Hawkins RJ (1996) Subscapularis tendon disruption after Bankart reconstruction for anterior instability. J Shoulder Elbow Surg Am Shoulder Elbow Surg 5(3):219–222
Maier D, Izadpanah K, Ogon P, Mutzel M, Bayer J, Sudkamp NP, Jaeger M (2015) Open fixation of acute anterior glenoid rim fractures with bioresorbable pins: analysis of clinical and radiological outcome. Arch Orthop Trauma Surg 135(7):953–961
Kuechle DK, Newman SR, Itoi E, Niebur GL, Morrey BF, An KN (2000) The relevance of the moment arm of shoulder muscles with respect to axial rotation of the glenohumeral joint in four positions. Clin Biomech 15(5):322–329
Symeonides PP (1972) The significance of the subscapularis muscle in the pathogenesis of recurrent anterior dislocation of the shoulder. J Bone Joint Surg Br 54(3):476–483
Ahmad CS, Wing D, Gardner TR, Levine WN, Bigliani LU (2007) Biomechanical evaluation of subscapularis repair used during shoulder arthroplasty. J Shoulder Elbow Surg Am Shoulder Elbow Surg 16(3 Suppl):S59–S64
Hedtmann A, Kircher J (2014) Instabilität des Glenohumeralgelenks Pathomechanismen. Klassifikation und Therapieprinzipien. Obere Extremität 9(2):66–77
Heuberer P, Kranzl A, Laky B, Anderl W, Wurnig C (2015) Electromyographic analysis: shoulder muscle activity revisited. Arch Orthop Trauma Surg 135(4):549–563
Armstrong A, Lashgari C, Teefey S, Menendez J, Yamaguchi K, Galatz LM (2006) Ultrasound evaluation and clinical correlation of subscapularis repair after total shoulder arthroplasty. J Shoulder Elbow Surg Am Shoulder Elbow Surg 15(5):541–548
Picard F, Saragaglia D, Montbarbon E, Tourne Y, Thony F, Charbel A (1998) Anatomo-clinical consequences of the vertical sectioning of the subscapular muscle in Latarjet intervention. Rev Chir Orthop Reparatrice Appar Mot 84(3):217–223
Maynou C, Cassagnaud X, Mestdagh H (2005) Function of subscapularis after surgical treatment for recurrent instability of the shoulder using a bone-block procedure. J Bone Joint Surg Br 87(8):1096–1101
McCann PD, Cordasco FA, Ticker JB, Kadaba MP, Wootten ME, April EW, Bigliani LU (1994) An anatomic study of the subscapular nerves: a guide for electromyographic analysis of the subscapularis muscle. J Shoulder Elbow Surg Am Shoulder Elbow Surg 3(2):94–99
Kasper JC, Itamura JM, Tibone JE, Levin SL, Stevanovic MV (2008) Human cadaveric study of subscapularis muscle innervation and guidelines to prevent denervation. J Shoulder Elbow Surg Am Shoulder Elbow Surg 17(4):659–662
Yoshinaga K, Kawai K, Tanii I, Imaizumi K, Kodama K (2008) Nerve fiber analysis on the so-called accessory subscapularis muscle and its morphological significance. Anatom Sci Int 83(1):55–59
Breisch EA (1986) A rare human variation: the relationship of the axillary and inferior subscapular nerves to an accessory subscapularis muscle. Anatom Record 216(3):440–442
Chen LZ, Chen L, Zhu Y, Gu YD (2013) Semiquantifying of fascicles of the C7 spinal nerve in the upper and lower subscapular nerves innervating the subscapularis and its clinical inference in Erb’s palsy. Clin Anat 26(4):470–475
Checchia SL, Doneaux P, Martins MG, Meireles FS (1996) Subscapularis muscle enervation: the effect of arm position. J Shoulder Elbow Surg Am Shoulder Elbow Surg 5(3):214–218
Yung SW, Lazarus MD, Harryman DT 2nd (1996) Practical guidelines to safe surgery about the subscapularis. J Shoulder Elbow Surg Am Shoulder Elbow Surg 5(6):467–470
Greiner S, Gerber Popp A (2005) The subscapularis nerves are anatomical constraints to circumferential release of the subscapularis muscle. In: 18th Congress of the European Society for Surgery of the Shoulder and Elbow. Rome, Italy
Kato K (1989) Innervation of the scapular muscles and its morphological significance in man. Anatomischer Anzeiger 168(2):155–168
Kadaba MP, Cole A, Wootten ME, McCann P, Reid M, Mulford G, April E, Bigliani L (1992) Intramuscular wire electromyography of the subscapularis. J Orthop Res Off Publ Orthop Res Soc 10(3):394–397
Liu J, Hughes RE, Smutz WP, Niebur G, Nan-An K (1997) Roles of deltoid and rotator cuff muscles in shoulder elevation. Clin Biomech 12(1):32–38
Stefko JM, Jobe FW, VanderWilde RS, Carden E, Pink M (1997) Electromyographic and nerve block analysis of the subscapularis liftoff test. J Shoulder Elbow Surg Am Shoulder Elbow Surg 6(4):347–355
Tokish JM, Decker MJ, Ellis HB, Torry MR, Hawkins RJ (2003) The belly-press test for the physical examination of the subscapularis muscle: electromyographic validation and comparison to the lift-off test. J Shoulder Elbow Surg Am Shoulder Elbow Surg 12(5):427–430
Rowe CR, Patel D, Southmayd WW (1978) The Bankart procedure: a long-term end-result study. J Bone Joint Surg Am 60(1):1–16
Jobe FW, Giangarra CE, Kvitne RS, Glousman RE (1991) Anterior capsulolabral reconstruction of the shoulder in athletes in overhand sports. Am J Sports Med 19(5):428–434
Ponce BA, Ahluwalia RS, Mazzocca AD, Gobezie RG, Warner JJ, Millett PJ (2005) Biomechanical and clinical evaluation of a novel lesser tuberosity repair technique in total shoulder arthroplasty. J Bone Joint Surg Am 87(Suppl 2):1–8
Habermeyer P, Magosch P, Lichtenberg S (2007) Recentering the humeral head for glenoid deficiency in total shoulder arthroplasty. Clin Orthop Relat Res 457:124–132
Denard PJ, Duey RE, Dai X, Hanypsiak B, Burkhart SS (2013) Relationship of the subscapular nerves to the base of the coracoid. Arthrosc J Arthrosc Related Surg Off Publ Arthrosc Assoc NA Int Arthrosc Assoc 29(6):986–989
Agneskirchner JD, Lafosse L (2014) Transfer of the coracoid process in recurrent anterior instability of the shoulder joint. Arthrosc Latarjet Proced Operat Orthop Traumatol 26(3):296–306
Agneskirchner JD, Haag M, Lafosse L (2014) Arthroscopic nerve release and decompression of ganglion cysts around the shoulder joint. Operat Orthop Traumatol 26(3):277–287
Beitzel K, Mazzocca AD (2014) Open anatomic reconstruction of chronic acromioclavicular instability. Operat Orthop Traumatol 26(3):237–244
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Institutional review board
The Ethics Commission of the Faculty of Medicine of Cologne University has approved the study (16-034).
Conflict of interest
Tim Leschinger, Michael Hackl, Martin Scaal, Felix Zeifang, Lars Peter Müller, and Kilian Wegmann: None. These authors, their immediate families, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
Rights and permissions
About this article
Cite this article
Leschinger, T., Hackl, M., Zeifang, F. et al. Nerve supply of the subscapularis during anterior shoulder surgery: definition of a potential risk area. Arch Orthop Trauma Surg 137, 135–140 (2017). https://doi.org/10.1007/s00402-016-2585-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-016-2585-7