Abstract
Introduction
Only few procedures for Lisfranc ligaments reconstruction to treat subtle injury of the Lisfranc joint have been reported. We have developed a novel technique for Lisfranc ligaments reconstruction, which was applied to treat chronic symptomatic subtle injuries that had failed to respond to initial treatment or were misdiagnosed. This article describes the technique and its operative outcome in a small case series.
Methods
Between April 2011 and October 2013, 5 (4 male and 1 female) athletes with a mean age of 19.4 (range 17–21) years were diagnosed with chronic subtle injury of the Lisfranc joint and underwent our novel reconstructive operation. In this technique, only a bone tunnel between the medial cuneiform and the second metatarsal bone is needed for near-anatomical reconstruction of the dorsal and interosseous ligaments. All patients were evaluated before and at 1 year after surgery using the American Orthopaedic Foot and Ankle Society (AOFAS) scale for the ankle–midfoot. In addition, the interval between surgery and return to athletic activity, defined as return to near pre-injury performance level, was investigated.
Results
Mean duration of postoperative follow-up was 18.8 (range 12–26) months. Mean AOFAS score improved significantly from 74.6 ± 2.5 (range 71–77) preoperatively to 96.0 ± 5.5 (range 90–100) at 1 year after the operation (p < 0.01). All patients were able to return to their previous athletic activities and the interval between surgery and return to athletic activity was 16.8 ± 1.1 (range 15–18) weeks. There was no complication related to the operation.
Conclusion
The results of this study suggest that our technique of Lisfranc ligaments reconstruction using autologous graft is effective for athletes with chronic subtle injury.
Level of evidence
Level IV, retrospective case series.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The types of Lisfranc joint injury have been divided according to whether the injury is high or low energy, and the typical injury in athletes is caused by low-energy trauma [1, 2]. The characteristic of Lisfranc joint injury due to low-energy trauma is subtle radiographic findings such as subtle diastasis with or without an avulsion fragment arising from either the lateral edge of the medial cuneiform bone or the medial aspect of the second metatarsal base, so appropriate diagnosis of such an injury requires a high index of suspicion [1, 2]. Subtle diastasis caused by low-energy trauma means disruption of ligament structures between the medial cuneiform and second metatarsal base, comprising the dorsal, interosseous, and plantar ligaments. The interosseous ligament, also referred as Lisfranc ligament, is known to be the strongest structure between the three ligaments supporting the tarsometatarsal joint complex [1, 2].
Faciszewski et al. [3] described “subtle injury of the Lisfranc joint” in 1990 and this name for the condition has been widely used since. Some reports have defined the key diagnostic feature as diastasis or instability between the first and second metatarsals on radiological investigation [4–6]. Most surgeons recommend screw or plate fixation for a fresh unstable subtle injury [1, 2, 7–9], and novel techniques using Endobutton [10] or Tightrope [11] have been recently reported. Although good clinical outcomes have been reported after operations [1, 2, 7–11], a standard operative technique does not exist for chronic symptomatic cases that failed to respond to conservative treatment or did not undergo appropriate initial treatment because of misdiagnosis as a simple midfoot sprain. We therefore developed a novel technique for Lisfranc ligaments reconstruction using autologous gracilis tendon to treat chronic subtle injury. The purpose of this study was to introduce the reconstruction technique and examine its outcome in athletes with chronic subtle injury.
Methods
Between April 2011 and October 2013, 5 (4 male and 1 female) athletes with a mean age of 19.4 (range 17–21) years were diagnosed with chronic subtle injury of the Lisfranc joint and underwent a reconstructive operation in our institution. All patients were engaged in competitive athletic activities: three were university rugby players, one was an American football player, and one was a high school judo player. Three were initially diagnosed with injury of the Lisfranc joint and had conservative treatment supervised by their practitioners, including cast immobilization with no weight-bearing for several weeks followed by partial weight-bearing, but midfoot pain during activities hindered their performance after they had resumed their sports. One patient consulted her practitioner immediately after injury but did not receive adequate treatment as she was diagnosed with a midfoot sprain. One patient neither visited a medical institution after the injury nor returned to athletic activity (Table 1).
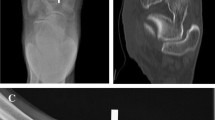
The diagnosis of chronic subtle injury was easily reached in all patients through typical physical examination findings such as point tenderness over the midfoot and radiographic finding of diastasis between the first and second metatarsals with or without diastasis between the medial and middle cuneiform bones which were evaluated in the weight-bearing radiograph of both feet by comparing the injured and uninjured sides (Fig. 1). The mean interval from the initial injury to reconstructive operation was 10.4 (range 5–24) months (Table 1).
All patients were evaluated using the American Orthopaedic Foot and Ankle Society (AOFAS) scale for the ankle–midfoot [12] preoperatively and at 1 year postoperatively. In addition, the interval between surgery and return to athletic activity, defined as return to close to pre-injury performance level, was investigated.
Operative technique
The operation was conducted under general anesthesia in the supine position with application of a pneumatic tourniquet (260 mmHg) to the thigh. At first, the gracilis tendon of the ipsilateral knee was harvested using a tendon harvester inserted through a medial knee skin incision of approximately 3 cm in length. An approximate 12-cm segment of harvested gracilis tendon was made into an autograft and shaped into a usable form for reconstruction of the Lisfranc ligaments. Next, a longitudinal skin incision was made over the part between the first and second metatarsal base, and scar tissue between the first metatarsal, medial cuneiform, and second metatarsal bone was resected. A medial skin incision over the medial cuneiform was made and reduction was performed with a large bone-reduction clamp that was applied between the base of the second metatarsal and the medial cuneiform through two incisions. By squeezing the clamp, the base of the second metatarsal was reduced into the anatomical position and the maintenance of reduced position was confirmed by an image intensifier. Then, a guide wire that was passed along the course of Lisfranc ligament was inserted from the medial side of the medial cuneiform to the base of the second metatarsal bone under the guidance of the image intensifier. Overdrilling was performed along this guide wire to create a bone tunnel using a cancellous bone-harvesting drill with a bit diameter of 4.2 mm (Meira Co., Ltd., Nagoya, Japan) (Fig. 2). Then, a 2-0 nylon loop was inserted into the bone tunnel using a passing pin, and the autograft was introduced into the bone tunnel through the 2-0 nylon loop. The distal end of the autograft was pulled out from the bone tunnel and the autograft was fixed at the proximal part of the bone tunnel by a solid interference screw with a diameter of 4.0 mm (Meira Co., Ltd.) under additional manual tension at the two ends of the autograft (Fig. 3). The proximal end of the autograft was pulled out into the skin incision that was made between the first and second metatarsal base through the released subcutaneous tissue. At that time, cannulated cancellous screw fixation was performed for instability between the medial and middle cuneiform bones. The two ends of the autograft were manually tensioned and a suture anchor was inserted into the base of the second metatarsal bone perpendicularly to its long axis. Then, the tensioned distal end of the autograft was fixed by a suture anchor and finally, the tensioned ends of the autograft were sutured using 3-0 absorbable sutures (Figs. 4, 5).
a Intraoperative photograph showing reduction of the diastasis between the base of the second metatarsal and the medial cuneiform using a large bone-reduction clamp through two incisions and insertion of the guide wire. b Image intensifier view showing the reduced position and insertion of the guide wire. c Image intensifier view showing the creation of a bone tunnel using a cancellous bone-harvesting drill with a bit diameter of 4.2 mm (patient 1)
a Intraoperative photograph showing introduction of the autograft into the bone tunnel through the 2-0 nylon loop. b Schematic diagram of the intraoperative photograph of a. c Intraoperative photograph showing the introduced autograft. d Image intensifier view showing fixation of the autograft at the proximal part of the bone tunnel by a solid interference screw with a diameter of 4.0 mm (patient 1)
Intraoperative photograph (a) and schematic diagram (b) showing insertion of a suture anchor into the base of the second metatarsal bone perpendicularly to its long axis. Intraoperative photograph (c) and schematic diagram (d) showing fixation of the tensioned distal end of the autograft by the suture anchor, and suturing of the tensioned ends using 3-0 absorbable sutures (patient 1)
Postoperatively, short leg cast immobilization was applied for 4 weeks and active and passive range of motion exercises were allowed after removal of the cast. Partial and full weight-bearings were permitted 6 and 8 weeks postoperatively, respectively. Return to running was allowed 12 weeks after the operation, except for the case with screw fixation between the medial and middle cuneiform bones, which required screw removal before commencement of running to avoid breakage of the screw. Full return to their pre-injury sports activities was allowed if they felt confident and had experienced no difficulties in their sport-specific drills.
Statistical analysis
AOFAS scores before and at 1 year after operation were compared using the paired t test. A difference in the pre- and postoperative scores was considered significant when the p value was ≤0.05.
Results
The mean postoperative follow-up period was 18.8 (range 12–26) months. All five patients experienced improvement of their symptoms postoperatively. The mean AOFAS score improved significantly from 74.6 ± 2.5 (range 71–77) preoperatively to 96.0 ± 5.5 (range 90–100) 1 year postoperatively (p < 0.01). All patients were able to return to their previous athletic activities, and the mean interval between the operation and return to athletic activity was 16.8 ± 1.1 (range 15–18) weeks (Table 2). There was no complication related to the operation such as superficial or deep infection, delayed wound healing, deep vein thrombosis or nerve injury.
Discussion
The consensus among orthopedic surgeons is that an operation is indicated for fresh unstable subtle injury of the Lisfranc joint, especially for injuries in athletes [1, 2, 7–11]. The goal of the operation is to achieve an anatomical reduced position of the injured tarsometatarsal (TMT) joint complex, and the quality of the reduction has been shown to correlate with prognosis. Good outcomes after open anatomical reduction with internal fixation by screw fixation or plating have been reported [7–9], and recently, novel techniques using suture Endobutton [10] or Tightrope [11] have also been reported. These procedures can be applied to fresh subtle injury where healing of injured ligaments is possible [7–11]; however, healing in chronic cases cannot be expected despite internal fixation.
Although arthrodesis may be selected to treat chronic subtle injury, it results in a loss of motion in the medial and middle column of the TMT joint—the maintenance of which seems to be necessary for restoration of complete function in athletes [1, 2].
A few surgeons have performed ligament reconstruction for acute subtle injury [13, 14]. Nery et al. [13] recommended creation of three bone tunnels before harvesting the third extensor digitorum longus tendon as a reconstructive substitute: first, a transverse tunnel that runs from the deep point of the medial cuneiform to the midpoint of the lateral cuneiform; second, an oblique tunnel that runs from the medial surface of the medial cuneiform to the proximal metaphysis of the second metatarsal bone; and third, a plantar tunnel that runs obliquely from the medial cuneiform to the base of the third metatarsal. They selected which tunnels will be needed according to the injury pattern revealed by preoperative radiological evaluation [13]. In their procedure, the Lisfranc ligament was replaced by the autograft introduced into the second oblique tunnel [13]; however, the presence of only one bundle seems to be inadequate for stabilizing the area between the medial cuneiform and the second metatarsal bone because the ligamentous structure in this part consists of the dorsal, interosseous (Lisfranc), and plantar ligaments according to an anatomical investigation [15]. Furthermore, their technical report did not describe the fixation of the autograft in detail. Hirano et al. [14] introduced a new procedure of anatomical and functional ligament reconstruction for Lisfranc joint fracture dislocation. In their procedure, the reconstruction route was via burr hole that was created on base of the second metatarsal bone perpendicular to its long axis and another two burr holes were then created from the medial cuneiform to the second metatarsal bone, which were connected to the bur hole created on base of the second metatarsal bone [14]. They used autologous gracilis tendon as a tendon graft for ligament reconstruction, and interference screws were used to fix the graft at the base of the second metatarsal and at the entry of each burr hole in the medial cuneiform bone [14]. This procedure enables anatomical reconstruction of the dorsal and interosseous ligaments but is technically troublesome because three burr holes have to be created. Furthermore, the three burr holes are concentrated at the base of the second metatarsal bone, which is susceptible to an iatrogenic fracture. In addition, these techniques have not been used to treat chronic subtle injury.
In our technique, only a bone tunnel between the medial cuneiform and the second metatarsal bone is needed for near-anatomical reconstruction of the dorsal and interosseous ligaments, which is easy to perform with a low risk of iatrogenic fracture of the second metatarsal bone. Furthermore, sufficient fixation of the autograft is achieved by a solid interference screw at the proximal part of the bone tunnel and by a suture anchor at the distal end of the autograft. However, the technique does not achieve true anatomical reconstruction because the dorsal ligament and interosseous (Lisfranc) ligament—which has been reported as the strongest of these ligaments—were reconstructed but the plantar ligament between the medial cuneiform and the second metatarsal bone could not be reconstructed because of technical limitation. One of the abovementioned reports is a technical note without details of the surgical outcome and the other was a case report with the surgical outcome of only one case, so a comparison of efficacy and safety of these cases with the present case series could not be made. Although the present case series had only five patients, it revealed that the surgical outcome was good as assessed by a clinical scoring system without the development of any surgical complication.
This study has several limitations. This was a retrospective case series with a limited number of patients, a short follow-up period, and no control cases, so the results of other surgical methods such as arthrodesis could not be directly compared. To resolve this limitation, a multicenter matched paired study could be an option because cases with chronic subtle injury of the Lisfranc joint are relatively rare. Furthermore, follow-up of a longer duration is necessary to confirm the safety and efficacy of the presented surgical technique. Although further study is necessary for the current technique to become standard operative treatment for chronic subtle injury, the results of this study suggest that it is effective for athletes with chronic subtle injury.
Conclusion
Our novel procedure for Lisfranc ligaments reconstruction using autologous gracilis tendon resulted in return to athletic activities for five athletes who had chronic symptomatic subtle injury that failed to respond to initial treatment or were misdiagnosed as midfoot sprain. There was no surgical complication. Although further study is necessary before the procedure can become a standard treatment for chronic subtle injury, the results of this study suggest that it is effective for athletes with chronic subtle injury.
References
Myerson MS, Cerrato RA (2008) Current management of tarsometatarsal injuries in the athlete. J Bone Joint Surg Am 90:2522–2533
Watson TS, Shurnas PS, Denker J (2010) Treatment of Lisfranc joint injury: current concepts. J Am Acad Orthop Surg 18:718–728
Faciszewski T, Burks RT, Manaster BJ (1990) Subtle injuries of the Lisfranc joint. J Bone Joint Surg Am 72:1519–1522
Curtis MJ, Myerson M, Szura B (1993) Tarsometatarsal joint injuries in the athlete. Am J Sports Med 21:497–502
Coss HS, Manos RE, Buoncristiani A, Mills WJ (1998) Abduction stress and AP weightbearing radiography of purely ligamentous injury in the tarsometatarsal joint. Foot Ankle Int 19:537–541
Nunley JA, Vertullo CJ (2002) Classification, investigation, and management of midfoot sprains: lisfranc injuries in the athlete. Am J Sports Med 30:871–878
Thordarson DB, Hurvitz G (2002) PLA screw fixation of Lisfranc injuries. Foot Ankle Int 23:1003–1007
Lee CA, Birkedal JP, Dickerson EA, Vieta PA Jr, Webb LX, Teasdall RD (2004) Stabilization of Lisfranc joint injuries: a biomechanical study. Foot Ankle Int 25:365–370
Alberta FG, Aronow MS, Barrero M, Diaz-Doran V, Sullivan RJ, Adams DJ (2005) Ligamentous Lisfranc joint injuries: a biomechanical comparison of dorsal plate and transarticular screw fixation. Foot Ankle Int 26:462–473
Lundeen G, Sara S (2009) Technique tip: the use of a washer and suture endobutton in revision lisfranc fixation. Foot Ankle Int 30:713–715
Brin YS, Nyska M, Kish B (2010) Lisfranc injury repair with the TightRope device: a short-term case series. Foot Ankle Int 31:624–627
Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M (1994) Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 15:349–353
Nery C, Réssio C, Alloza JF (2012) Subtle Lisfranc joint ligament lesions: surgical neoligamentplasty technique. Foot Ankle Clin 17:407–416
Hirano T, Niki H, Beppu M (2014) Newly developed anatomical and functional ligament reconstruction for the Lisfranc joint fracture dislocations: a case report. Foot Ankle Surg 20:221–223
de Palma L, Santucci A, Sabetta SP, Rapali S (1997) Anatomy of the Lisfranc joint complex. Foot Ankle Int 18:356–364
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miyamoto, W., Takao, M., Innami, K. et al. Ligament reconstruction with single bone tunnel technique for chronic symptomatic subtle injury of the Lisfranc joint in athletes. Arch Orthop Trauma Surg 135, 1063–1070 (2015). https://doi.org/10.1007/s00402-015-2250-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-015-2250-6