Abstract
Introduction
The aim of this study was to evaluate functional outcome after surgically treated acetabular fracture using radiography and patient-reported outcome measures, and to determine predictors of hip joint failure 5 years post-surgery.
Patients and methods
All patients with acetabular fractures treated with open reduction and internal fixation (ORIF) at our unit are prospectively entered into a local register. 101 acetabular fractures in 112 patients treated from 2004 to 2007 were eligible for analysis 5 years after surgery. Radiographs and questionnaires regarding physical function (Short Form[SF]-36) and pelvic discomfort index (PDI, 100 % = worst outcome) were obtained. The primary outcome measure was “joint failure” defined as either secondary total hip arthroplasty (THA) or a Girdlestone situation. Univariable analysis was used to compare patients with joint failure to those without, and binary logistic regression analysis was performed to identify risk factors of joint failure.
Results
77 % of 101 followed patients had a preserved hip joint 5 years after surgery, and failure of the hip joint most often occurred within the first 2 years after injury. Patients with preserved hip joints had higher scores in the SF-36 physical function domain (median 75 vs. 48; p = 0.004) and better PDI (28 vs. 43 %, p = 0.03). Femoral head impaction was associated with an increased risk of joint failure [relative risk (RR) = 15.2, 95 % CI 3–95; p = 0.002], as was an age of ≥60 years at the time of injury (RR = 4.2, CI 1.3–15; p = 0.02).
Conclusions
Patients with failed hip joints after surgery for acetabular fracture have inferior global and disease-specific functional outcomes, even after secondary arthroplasty surgery. We suggest that patients with predictors of joint failure could benefit from other treatment strategies than ORIF, and primary insertion of THA may be an alternative treatment strategy for this subgroup.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The goal of surgical reconstruction of displaced acetabular fractures is to restore hip function, but post-traumatic arthritis or avascular necrosis (AVN) of the femoral head can necessitate secondary procedures such as insertion of a total hip arthroplasty (THA) or conversion to a Girdlestone situation in the case of infection. In a review by Giannoudis et al. [1] the rate of THA reported in 16 studies on surgically treated acetabular fractures was described to range between 6 and 25 %. The largest reported series of surgically treated acetabular fractures with 2–20 years follow-up indicated that 21 % of the patients later received a THA [2]. Risk factors of joint failure were also identified but no functional outcome was assessed in that study. Most published studies on this subject are retrospective and a substantial proportion of patients are often lost to follow-up, rendering many conclusions on this group of patients uncertain.
Little is therefore known about hip function and quality of life at specific time points following acetabular fracture surgery. Functional outcome 2 years after surgery has been reported [3], but information is scarce after longer time periods in a prospective setting.
The primary aim of this study was to evaluate the preservation of the hip joint within the framework of a prospective follow-up of all patients operated at our institution 5 years after surgery for acetabular fracture. We also aimed to identify risk factors of joint failure as well as general physical function and condition-specific hip function after 5 years.
Methods
Study population
112 patients of age 16 years or older that were surgically treated for acetabular fractures at our institution during the period September 2004–December 2007 were prospectively included. 30 hospitals referred patients after providing primary care. The study was approved by the local ethics committee and patients gave informed consent to be included in the study.
11 patients were lost to follow-up after 5 years, leaving 101 patients in the study population (76 men, 25 women, mean age 49, range 17–83). Patients were localized using the updated national registry, which also established whether a patient had died. Questionnaires were sent to living patients including one reminder in the case of no response after 2 weeks, and requests for the above-described set of radiographs were sent to the closest hospital, with persistent correspondence as required.
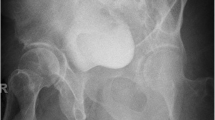
Low-molecular weight heparin was administered subcutaneously as prophylaxis against venous thrombosis for a minimum of 10 days after surgery, and prolonged for patients not mobilized by that time. Systemic antibiotics were given perioperatively for 24 h as infection prophylaxis. NSAID was given orally for 3 weeks to all patients operated through the Kocher-Langenbeck approach as prophylaxis for heterotopic ossification. Preoperative radiological examination included conventional radiographs and CT scans. The presence of acetabular impaction and femoral head damage was assessed on the CT scans and chondral lesions intraoperatively when the Kocher-Langenbeck approach was used allowing visualisation of the femoral head. Postoperative conventional radiographs included the three standardized views anteroposterior pelvis, obturator oblique, and iliac oblique. All patients were allowed active hip motion but weight bearing was restricted to partial weight bearing for 8–10 weeks after surgery.
Evaluation of function
Patients were assessed using the SF-36, described by Ware and Sherbourne [4]. The SF-36 is a health-related quality of life instrument and one of its 8 domains addresses general physical function. We also used a condition-specific instrument for self-assessment following acetabular fractures that evaluated patient discomfort related to the pelvic injury using a 6-graded scale from 0 (no discomfort) to 5 (very severe discomfort) for each of six items: pain, walking, hip motion, leg sensation, sexual activity and operation scar) [5]. The patients’ ratings are then converted as an aggregate index, the pelvic discomfort index (PDI), which ranges from 0 % pelvic discomfort (best) to 100 % discomfort (worst).
Statistics
Frequencies, means, medians and ranges were used to describe data. Frequency distributions of numerical variables were assessed by visual inspection of histograms, Q-Q plots, and using the Shapiro–Wilk test. The primary outcome measure was “failed hip joint”, defined as hips where a THA had been inserted or that had been converted to a Girdlestone situation. Secondary outcome measures were incidence of complications (neurological, infectious or thromboembolic), occurrence of avascular necrosis (AVN), and degree of radiographic changes after 5 years. Age, sex, type of injury, fracture type (according to Letournel [6]), time to surgery, and the quality of reduction (according to Matta [7]) were considered independent covariates. Age was treated either as a continuous variable or dichotomised into age below 60 or 60 and above. The rationale for choosing an age of 60 years at surgery as the cut-off was based upon the finding that 60 years was the crossing point of the density functions describing age distributions in “failures” vs. “non-failures” (supplementary figure 1). Categorical variables were investigated using the χ 2 test or Fisher’s exact test (with Yates’ continuity correction) where appropriate, while the numerical variables age, time to surgery, and time to failure were investigated with Welch’s 2 sample t test, Mann–Whitney U test or Kruskal–Wallis’ rank sum test, depending on data distributions and numbers of groups. Data with normal distribution were analysed using parametric methods, non-normally distributed data were analysed using non-parametric methods.
Binary logistic regression analysis was performed after dichotomising the patient population into cases that were defined as “failed hips” and those that were not. Regression coefficients expressed as risk ratios (RR) with 95 % confidence intervals (CI), z-scores and p values were calculated. Exploratory models included the independent covariates mentioned above but excluded those combinations that were strongly correlated with each other. Exploratory models also included age treated as a continuous variable. The final model fitted for the endpoint joint failure included the covariates sex, age as a dichotomous variable (below 60 or 60 and above), presence of acetabular impaction, femoral head impaction, posterior hip dislocation, and quality of reduction according to Matta, based on the proposed clinical relevance of these covariates. The pseudo R 2 for the final model was 0.41 (calculated according to Nagelkerke’s modification). Apart from standardized and studentized residuals model diagnostics included Cook’s distances DfBetas, and there were no influential cases in the final model according to these criteria.
Two-tailed p values ≤0.05 were considered significant in all tests. SPSS (version 19) and the R software package (version 2.14.1) were used for statistical analyses [8].
Results
Injury mechanisms and fracture types
High-energy trauma was present in 64 patients (63 %) where motor vehicle accidents dominated with 43 patients, fall from height <3 m was present in 21 (21 %) and ground level fall in 16 (16 %) of all 101 cases. 59 patients (58 %) had no associated injury, whereas 42 (42 %) had one or more associated injuries out of which 21 (21 %) had an ISS of 16 or higher. Fracture types were associated in 61 (60 %) and elementary in 40 (40 %). Fracture classifications according to Letournel are given in Table 1. Posterior femoral head dislocation was present in 22 patients (22 %). Acetabular impaction was present in 10 patients (10 %), and femoral head impaction or a chondral lesion was found in 12 (12 %) patients.
Surgery, quality of reduction, and incidence of complications
Median time to definitive ORIF was 6 days (2–17). 59 (59 %) patients were operated through an ilioinguinal approach and 40 (40 %) through a Kocher-Langenbeck incision, 1 patient was operated through an iliofemoral and 1 through a Smith-Peterson approach. The quality of reduction measured according to Matta was 0–1 mm residual fracture diastasis (anatomic) in 77 (76 %) cases, and ≥2 mm (inferior) in 24 (24 %). The proportion of patients with anatomical reduction according to Matta (0–1 mm) was higher among elementary fracture types than among associated fracture types (36 of 40, vs. 41 of 61; p = 0.02).
Postoperative complications included deep infections in 4 patients, and thromboembolic complications in 6.
Outcome after 5 years
5 years post-surgery, 101 of the 112 patients included in this prospective study could be followed, 11 patients were lost to radiographic examination and did also not return a questionnaire: 3 patients had died, 4 patients chose not to comply, 2 patients lived in a region not able to perform the radiographic examinations, 1 patient had emigrated, and 1 patient with a history of drug abuse had no traceable address. The outcome for the 11 patients lost to the radiographic 5-year follow-up was investigated by consulting the Swedish Hip Arthroplasty Register, and none had been operated with a THA at any Swedish institution. Another 2 patients died during the follow-up time period, 1 had received a THA and 1 a Girdlestone.
The hip joint was preserved in 78 (77 %) patients whereas the joint had failed in 23 (23 %) of the 101 patients with radiographic information. 21 patients with a failed joint had received a THA and the remaining 2 had a Girdlestone situation, these two patients were excluded from the analyses of functional outcome. Secondary surgery was most often necessary during the first 2 years after ORIF (Fig. 1). Six patients (5.4 % of all patients) with joint failure had developed AVN of the femoral head, 2 joints failed due to infection and the other 15 joint failures were due to secondary posttraumatic osteoarthritis. The radiographic appearance 5 years after ORIF in the patients with a preserved hip joint is described in Table 2, indicating that 68 (87 %) patients had no or only mild radiographic changes. Heterotopic ossifications were undetectable or only present as small islands (Brooker grades 0–I) in 73 (94 %) patients, 4 patients had Brooker grade II and 1 patient Brooker grade IV ossifications.
Patients with a preserved hip joint had higher scores in the physical function domain of the SF-36 (Fig. 2, median 75.0 vs. 47.5, p = 0.004) than those with failed hip joints. Patients with preserved hip joints also had better PDI scores (Fig. 3, mean 28 vs. 43 %, p = 0.03) and were more often represented in the best PDI category (0–20 % discomfort), whereas patients with joint failure were evenly distributed over the remaining categories, indicating higher degrees of pelvic discomfort.
Physical function domain of the SF-36 at follow-up after 5 years for the groups with a preserved hip joint (no failure) and failed hip joint (failure). Best scores are in the upper range of the scale. Most patients with joint failure had received their THA several years before the time of follow-up. *p = 0.004 (derived from Wilcoxon rank sum test)
Injury-specific hip score at follow-up after 5 years for the groups with a preserved hip joint (no failure) and failed hip joint (failure). Best scores are in the lower range of the scale. Most patients with joint failure had received their THA several years before the time of follow-up. *p = 0.04 (derived from Wilcoxon rank sum test)
Risk factors of joint failure
Patients that had joint failure were older than those with a preserved hip joint (57 vs. 47 years, p = 0.02). 9 of 25 women and 14 of 76 men had joint failures (p = 0.1). The distribution of elementary and associated fracture types as classified according to Letournel was similar for patients with a preserved hip joint and those with failed hips (7 failures among 40 elementary, 16 failures among 61 associated; p = 0.4). There were more failures among the hips with the fracture pattern “anterior combined with posterior hemitransverse” when classified according to Letournel (8 failures among 22 fractures of this type), but this observation failed to reach the threshold of statistical significance (standardized residual = 1.3, p = 0.3). Posterior femoral head dislocation had been present in 8 of 23 failures and in 15 of 78 preserved hip joints (p = 0.2). The presence of acetabular impaction was more frequent among patients with failed joints (5 acetabular impactions among 23 failures vs. 5 impactions among 78 preserved joints; p = 0.05), as was femoral head impaction (8 femoral head impactions among 23 failures vs. 3 impactions among 78 preserved joints; p < 0.001). Patients with ground level fall were older (65 years) than those with fall <3 m (59 years) or high-energy trauma (42 years; p < 0.001). The quality of reduction was unevenly distributed between patients with preserved and those with failed joints, with a residual diastasis classified according to Matta as 2 mm or above in 10 among 23 with failed joints compared with 14 among 78 preserved joints (p = 0.03). Time to surgery differed between groups, with a surgical delay of 5.4 days for those with failed joints compared to 7.0 days among those with a preserved hip joint (p = 0.04).
The relative risks associated with selected covariates in a multivariable logistic regression analysis are given in Table 3. Briefly, femoral head impaction was associated with an increased risk of joint failure with an RR of 15.2, and an age of 60 years and above increased the risk of failure by a factor of 4.2. The quality of reduction did not reach the threshold of statistical significance (p = 0.08). In contrast, posterior dislocation, acetabular impaction, or gender did not affect risk for failed joints when weighted together with the other covariates. When age was entered into the model as a continuous variable, the risk of failure increased by 4 % for each year of life (95 % CI 0–8, p = 0.05).
Discussion
This prospective 5-year follow-up study of patients with displaced acetabular fractures identified age >60 years and femoral head impaction as important predictors of joint failure. This finding is in agreement with previous reports on the outcome after surgically treated acetabular fractures [2, 9, 10]. An age over 40 years is an unfavourable prognostic indicator in a case series describing 53 surgically treated acetabular fractures [9], a finding that is confirmed in a large cohort of 810 patients with acetabular fractures followed for 2–20 years [2]. Advanced age is also described to strongly correlate with inferior quality of reduction that negatively influenced outcome [10]. In the series described by Tannast et al. [2] patients were generally younger, 47 % were below the age of 40 as opposed to 31 % in our study.
Other predictors than age of an unfavourable outcome found in the present study were uncontrollable variables determined by the fracture pattern, namely femoral head impaction and acetabular impaction. Femoral head impaction was associated with a more than 15-fold increased risk of failure. This finding is in agreement with previous studies where femoral head impaction has been described as being associated with a subsequent need for conversion to THA [2, 9, 10].
Quality of reduction is a controllable variable. The majority of our patients (76 %) were placed in the category with minimal residual displacement, 0–1 mm, also termed “anatomical” reduction. In multivariable regression analysis the quality of reduction did not quite reach the threshold of statistical significance, but taking the difference in univariate analysis into account we consider this parameter to be of clinical importance. This interpretation is in line with previous analyses of the influence of reduction quality on outcome [2, 9].
Tannast et al. [2] proposed a nomogram-based approach to estimate the risk for a future THA. Our findings support that advanced age, a femoral head lesion and poor surgical reduction predispose towards an unfavourable outcome. However, our study goes beyond mere confirmation of these previous findings: functional outcome after 5 years was inferior in the group with failed hips compared to the group of patients with a preserved hip joint. Although the vast majority of patients with a THA underwent this secondary procedure during the first two postoperative years, they obviously did not recover to the average functional level of patients with a preserved hip joint. This finding contradicts a generally held belief that failed hip joints after acetabular fractures can be successfully converted into well-functioning joints by THA surgery.
Limitations of the study include the fact that there was no clinical examination at final follow-up. Another limitation was that the quality of reduction was assessed using conventional X-rays only. Furthermore, a limitation is as always patients lost to follow-up. Using patient-reported outcome instruments such as SF-36 propose a limitation in itself.
The present study’s strengths include the prospective collection of data on all cases with acetabular fractures surgically treated at our institution, the radiographic follow-up of all patients at defined time points, and the inclusion of functional parameters such as physical function from the SF-36 and the injury-specific pelvic discomfort index. In previous studies there is a substantial amount of non-responders, with little information presented regarding this group. We had few non-responders and an attempt to analyse them through a review performed by the Swedish Hip Arthroplasty Register showed that no THA had been registered among those lost to radiographic follow-up.
The prospective design distinguishes the present study from other literature on the subject of acetabular fractures that mostly are retrospective in nature [9–11]. A large cohort of 810 cases with acetabular fractures was followed prospectively, but in that study 32 % of the original study population had been lost to follow-up, introducing selection bias and necessitating the calculation of best- and worst-case scenarios [2].
We believe that continuing radiographic follow-up is important since it enables us to identify cases of secondary posttraumatic arthritis of the hip joint even if this condition has not led to insertion of a THA. Furthermore, the development of periarticular ossifications can be assessed. The uncertainty with respect to impending failure that is inherent to other studies that lack long-term radiographic follow-up can thus be minimized.
The assessment of functional outcome after surgical intervention of any kind is of growing interest. In an attempt at assessing such information several large arthroplasty registers now include patient-reported outcome measures [12]. Our finding of impaired physical function and quality of life among patients with failed hips—even after insertion of a THA—indicates that there is a need for novel treatment strategies for certain subgroups of patients with increased risk of failure.
The indications for acute THA in acetabular fracture are still unclear [13, 14]. A simultaneous osteosynthesis is required in most cases to ensure bony union of the columns and primary stability of the cup, and the use of reinforcement rings might be necessary. The outcome after THA surgery performed due to posttraumatic arthritis have yielded inferior results in retrospective studies [15], and it is widely considered a challenging procedure. Our study confirms this finding, pointing in the direction which acetabular fractures are at higher risk of subsequent joint replacement.
Conclusions
An age of 60 years or above and femoral head impaction were important predictors of failure. Treatment strategies such as primary insertion of THA combined with ORIF should be investigated in future comparative studies of acetabular fracture patients with risk factors of joint failure.
References
Giannoudis PV, Grotz MR, Papakostidis C, Dinopoulos H (2005) Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Joint Surg Br 87:2–9
Tannast M, Najibi S, Matta JM (2012) Two to 20-year survivorship of the hip in 810 patients with operatively treated acetabular fractures. J Bone Joint Surg Am 94:1559–1567
Borg T, Berg P, Larsson S (2012) Quality of life after operative fixation of displaced acetabular fractures. J Orthop Trauma 26:445–450
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Borg T, Carlsson M, Larsson S (2012) Questionnaire to assess treatment outcomes of acetabular fractures. J Orthop Surg (Hong Kong) 20:55–60
Letournel E (1980) Acetabulum fractures: classification and management. Clin Orthop Relat Res 151:81–106
Matta JM (1996) Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within 3 weeks after the injury. J Bone Joint Surg Am 78:1632–1645
Development Core Team R (2012) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Liebergall M, Mosheiff R, Low J, Goldvirt M, Matan Y, Segal D (1999) Acetabular fractures. Clinical outcome of surgical treatment. Clin Orthop Relat Res 366:205–216
Mears DC, Velyvis JH, Chang CP (2003) Displaced acetabular fractures managed operatively: indicators of outcome. Clin Orthop Relat Res 407:173–186
Kreder HJ, Rozen N, Borkhoff CM, Laflamme YG, McKee MD, Schemitsch EH, Stephen DJ (2006) Determinants of functional outcome after simple and complex acetabular fractures involving the posterior wall. J Bone Joint Surg Br 88:776–782
Rolfson O, Karrholm J, Dahlberg LE, Garellick G (2011) Patient-reported outcomes in the Swedish Hip Arthroplasty Register: results of a nationwide prospective observational study. J Bone Joint Surg Br 93:867–875
Mears DC, Velyvis JH (2002) Acute total hip arthroplasty for selected displaced acetabular fractures: two to 12-year results. J Bone Joint Surg Am 84-A:1–9
Herscovici D Jr, Lindvall E, Bolhofner B, Scaduto JM (2010) The combined hip procedure: open reduction internal fixation combined with total hip arthroplasty for the management of acetabular fractures in the elderly. J Orthop Trauma 24:291–296
Ranawat A, Zelken J, Helfet D, Buly R (2009) Total hip arthroplasty for posttraumatic arthritis after acetabular fracture. J Arthroplasty 24:759–767
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Borg, T., Hailer, N.P. Outcome 5 years after surgical treatment of acetabular fractures: a prospective clinical and radiographic follow-up of 101 patients. Arch Orthop Trauma Surg 135, 227–233 (2015). https://doi.org/10.1007/s00402-014-2137-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-014-2137-y