Abstract
Purpose
Vitamin D has a crucial role in our metabolic health. We aimed to examine associations of vitamin D status and its related dietary pattern (DP) with prevalent risk of metabolic syndrome (MetS) in 9,237 Korean adults aged 19–64 years based on the National Health and Nutrition Examination Survey.
Methods
Vitamin D status was examined by serum 25-hydroxyvitamin D (25(OH)D). A vitamin D-related DP associated with 25(OH)D levels was derived using reduced rank regression (RRR). Associations of vitamin D status and its related DP with MetS prevalence were examined using multivariable logistic regression models adjusted for potential confounders.
Results
Men with sufficient vitamin D status had a 44% lower risk of MetS prevalence (OR: 0.56; 95%CI: 0.36–0.87) compared to those with deficiency. A vitamin D-related DP derived using RRR was characterized by high intakes of vegetables, fish, fruits, and nuts and low intakes of eggs, oils, and mushrooms in this study population. Among men, the DP was significantly associated with a lower risk of MetS prevalence, showing a 12% (95%CI: 4–20%) reduction in risk for a one-unit increase in the DP score. However, there was no significant association among women.
Conclusion
The study’s findings suggest that a sufficient vitamin D status and a related DP with high intakes of vegetables, fish, fruit, and nuts were associated with the risk of MetS, particularly in Korean male adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metabolic syndrome (MetS), a cluster of abdominal obesity, hypertension, dyslipidemia, and hyperglycemia, increases risks of type 2 diabetes (T2D) and cardiovascular diseases (CVDs) [1,2,3]. The global prevalence of MetS among adults was estimated at 20–25% in 2018 and has continuously increased [4]. The MetS prevalence in Korean adults was 25.6% and 12.4% in men and women, respectively, in 2016–2018 [5].
The complex pathophysiology and interrelations among the components of MetS remain incompletely understood. Key mechanisms like insulin resistance, chronic inflammation, and hormonal activation are pivotal in its development and progression [6]. Despite extensive research, the precise underlying cause remains elusive, with various contributing factors proposed, including genetic factors, adipose tissue dysfunction derived from overweight/obesity, physical inactivity, and microbiota dysbiosis [7, 8]. Unbalanced diets, including deficiencies of micronutrients such as vitamin D, also play crucial roles in the MetS development by linking to other contributing factors [8].
Numerous studies have addressed the preventive role of vitamin D in MetS [8, 9]. Vitamin D plays an essential role as a prohormone in our body, not only being involved in bone metabolism but also having preventive effects against metabolic diseases such as anti-inflammatory and anti-fibrotic effects. The main source of vitamin D is cholecalciferol (vitamin D3) synthesized by sunlight or from animal food and ergocalciferol (vitamin D2) from vegetable food. These sources could be biologically active forms through two hydroxylations in our body, the first in the liver (25-hydroxyvitamin D, 25(OH)D) and then in the kidney (1,25-dihydroxyvitamin D, 1,25(OH)2D). A blood level of 25(OH)D indicates vitamin D status in our body.
Several observational studies among Western populations reported that serum 25(OH)D level had a significant inverse association with the risk of MetS [3, 10, 11]. In the Korean population, the prevalence rate of vitamin D deficiency (25(OH)D level < 20 ng/ml) was 71% in 2010 ∼ 2014, which was higher compared to other Western countries – about 40% in the US and European population [11,12,13]. A few studies within the Korean population also showed preventive effects of vitamin D on MetS [14, 15], but it is still controversial due to inconsistent results in studies [15, 16].
In addition, examining the association between dietary vitamin D intake and disease outcomes is challenging due to the limitations of traditional nutritional assessment tools, which cannot accurately reflect the bioavailability of vitamin D from various food sources and cannot account for its interaction with other micronutrients and biomolecules in our body during digestion and absorption [17]. Some attempts to tackle these limitations include using statistical approaches such as reduced rank regression (RRR) in nutrition epidemiology [18, 19]. Several studies have reported the advantage of using RRR models in deriving dietary patterns (DPs) related to biomarkers of interest and examining their association with chronic diseases [20,21,22]. However, only a few studies have applied RRR to investigate the association of DPs with MetS, especially vitamin D-related DPs, in an Asian population [23, 24].
Therefore, our study hypothesized that vitamin D status and vitamin D-related DP are associated with the prevalence of MetS in the Asian population. Thus, this study aimed to examine the associations of vitamin D status and vitamin D-related DP based on serum 25(OH)D level with risk of MetS prevalence in Korean adults using population-based data from the Korean National Health and Nutrition Examination Surveys (KNHANES) 2010–2014.
Materials and methods
Study population
This study was conducted based on data from the 5th-6th (2010–2012 & 2013–2014) KNHANES, where serum 25(OH)D levels of participants were measured. The KNHANES is a population-based cross-sectional survey conducted by the Korea Disease Control and Prevention Agency (KDCA) to monitor and assess the health and nutritional status of Koreans [25]. The sampling involved a stratified multistage probability method based on household and regional units, considering administrative divisions, housing type, age, sex, and residential property characteristics. All eligible household members aged one year and older who met the criteria of Korean representatives were included as survey participants [25]. The KNHANES survey protocol was approved by the KDCA Institutional Review Board (IRB) (Reference No: 2010-02CON-21-C; 2011-02CON-06-C; 2012-01EXP-01–2 C; 2013-07CON-03–4 C; 2013-12EXP-03–5 C). All participants provided informed consent for the use of their examination data. All survey procedures and examinations complied with the Declaration of Helsinki.
Definition of MetS
Based on the modified Third National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (NCEP-ATP III)] [26], we defined MetS as the presence of three or more of the following: (1) abdominal obesity: waist circumference > 90 cm in men and > 85 cm in women (according to the Korean Society for the Study of Obesity, KSSO) [27], (2) elevated fasting glucose: FG ≥ 100 mg/dL, (3) elevated triglycerides: TGs ≥ 150 mg/dL, (4) reduced HDL-cholesterol: HDL-C level < 40 mg/dL in men and < 50 mg/dL in women, (5) elevated blood pressure: SBP ≥ 130 mm Hg and/or DBP ≥ 85 mm Hg.
Definition of vitamin D status
Vitamin D status was evaluated based on serum 25(OH)D levels, which were measured by radioimmunoassay using the 25(OH)D 125I RIA Kit (DiaSorin, U.S.A) and a 1470 WIZARD gamma-Counter (PerkinElmer, Finland) [25]. Vitamin D status was defined as deficient (25(OH)D < 10 ng/mL), insufficient (25(OH)D ≥ 10 and < 20 ng/mL), or sufficient (25(OH)D ≥ 20 ng/mL) according to the WHO criteria for vitamin D deficiency [28,29,30].
Vitamin D-related dietary pattern
Dietary intake of study participants was assessed by using a 24-hour recall method [25]. All reported food items were categorized into 17 food groups (Supplementary Table S1). The daily intake (g/day) of each food group was calculated based on an established KNHANES database. The vitamin D-related DP was derived by using RRR [18], with 17 food group intakes as predictor variables and serum 25(OH)D level as a response variable in the model. RRR is similar to factor analysis but has the advantage of deriving linear combinations of predictor variables (herein, a DP consisting of 17 food groups) that maximally explain the variance of response variables (herein, serum 25(OH)D), based on a priori hypothesis related to the outcome of interest (herein, MetS) [18]. More details on statistical analysis for deriving the DP are described in the Statistical Analysis section below.
Potential confounders
Data of potential confounders, including sex, age, education level, regular exercise, smoking status, and alcohol intake, were collected by the KNAHNES self-reported questionnaire [25]. Body mass index (BMI) was calculated as the body weight (kg) divided by the square of body height (m2). Educational level was classified into four categories: ≤ Elementary school, Middle school, High school, or ≥ College. Regular physical activity was categorized into three levels based on walking days per week: < 2 days/week, 2–4 days/week, or > 4 days/week. Smoking status was categorized into three groups: current, former, or non-smoker. Alcohol intake was categorized into three levels: non-consumer, ≤ 1 time/ week, or ≥ 2 times/week.
Statistical analysis
All analyses were performed using the SAS program (Statistical Analysis System, version 9.4, SAS Institute Inc., Cary, NC, USA). Clusters, strata, and sample weights were used in all analyses to adjust for the survey design of KNHANES, which enabled the results to be representative of the entire Korean population. Differences in general characteristics, socioeconomic factors, and clinical data between non-MetS and MetS groups were examined using Student’s t-test for continuous variables and chi-square test for categorical variables.
To derive the vitamin D-related DP, RRR analysis was conducted with 17 food groups as predictor variables and serum 25(OH)D as the response variable. Prior to the RRR analysis, the daily intake of the 17 food groups was adjusted for energy intake by taking residuals from general linear models (GLMs) after log transformation to make the distributions symmetrical and normal. The RRR analysis identified a linear combination of the food groups explaining serum 25(OH)D, referred to as vitamin D-related DP, with factor loadings indicating associations between the food groups and the DP. Factor loadings with absolute values of 0.20 or more are considered statistically meaningful. Additionally, the DP score of each subject was calculated based on eigenvectors from the covariance matrix of predictors and responses [31].
Associations of vitamin D status, based on the 25(OH)D levels, and the vitamin D-related DP score with risk of MetS prevalence and each component of MetS were examined by multiple logistic regression analysis with adjustment for age, BMI, and other confounders (education level, smoking, alcohol drinking, regular exercise, and energy intakes). The DP score was analyzed both as a continuous variable (using a one-unit increase in the DP score) and as a categorical variable (using quartiles). Tests for linear trends across quartiles were performed using the same multiple logistic regression models with a continuous variable ranging from 1 to 4 for quartiles. All statistical significance levels were defined as P < 0.05.
Results
Among a total of 23,985 participants aged 19 ∼ 64 years, we excluded 5,102 subjects who were pregnant, breastfeeding, or menopausal, in a physiological condition that could affect both vitamin D metabolism and MetS. We also excluded subjects with extremely high or low daily energy intake (< 500 kcal/day or ≥ 5000 kcal/day) (n = 184) and those with missing data for serum 25(OH)D, MetS components, dietary intake, or anthropometric measurements (n = 7,637). Additionally, subjects who had not fasted for at least 8 h prior to blood sampling or had TG serum levels exceeding 400 mg/dL (n = 365), were treated for hypertension, diabetes, and dyslipidemia (n = 1,189), and did not completely answer the questions regarding potential confounders, including education level, smoking, alcohol intake and physical activity (n = 271) were excluded. Finally, a total of 9,237 participants were included in the analysis (Fig. 1).
General characteristics of study subjects
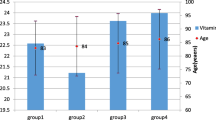
The characteristics of subjects according to the presence of MetS are presented in Table 1. Out of 9,237 subjects, 1,312 (14.2%) were diagnosed with MetS. The proportion of men (64.5%) with MetS was higher than those without MetS (44.7%). MetS subjects were older (42.3 ± 0.3 years vs. 36.2 ± 0.2 years) and had higher BMI (27.0 ± 0.1 kg/m2 vs. 22.7 ± 0.1 kg/m2) and serum 25(OH)D level (17.0 ± 0.2 ng/ml vs. 16.5 ± 0.1 ng/ml) significantly, compared to non-MetS subjects. MetS subjects had higher proportions of drinkers and smokers and energy intake, whereas lower levels of education and regular physical activity compared to non-MetS subjects (P < 0.05).
Associations between vitamin D status and risk of MetS prevalence
The proportion of subjects with vitamin D deficiency (< 10 ng/ml), insufficiency (10–20 ng/ml), and sufficiency (≥ 20 ng/ml) according to serum 25(OH)D level were 9.8%, 67.0%, and 23.3%, respectively. Table 2 shows associations between vitamin D status and the prevalence of MetS. In men, vitamin D status was significantly associated with risk of MetS prevalence, but no significant association in women. Men with vitamin D sufficiency had a 44% lower risk of MetS prevalence (OR = 0.56; 95% CI 0.36, 0.87) compared to those with vitamin D deficiency. Regarding each MetS diagnostic component, men with vitamin D sufficiency had lower risks of elevated TGs (OR = 0.48; 95% CI 0.34, 0.67; P for trend < 0.001) and reduced HDL-C (OR = 0.69; 95% CI 0.47, 1.00; P for trend < 0.05 in the model adjusted for age and BMI only) compared to those with vitamin D deficiency. Women with vitamin D sufficiency had lower risks of elevated TGs (OR = 0.50; 95% CI 0.32, 0.77; P for trend < 0.01), reduced HDL-C (OR = 0.69; 95% CI 0.53, 0.91; P for trend < 0.01), and elevated BP (OR = 0.59; 95% CI 0.37, 0.94; P for trend < 0.05), while had a higher risk of elevated FG (OR = 1.74; 95% CI 1.07, 2.83; P for trend < 0.05) than those with vitamin D deficiency.
Associations between a dietary pattern related to vitamin D status and risk of MetS prevalence
The vitamin D-related DP was characterized by high intakes of vegetables, fish, fruit, and nuts, and low intakes of eggs, oils, and mushrooms, according to factor loadings with absolute values ≥ 0.20 (Fig. 2 & Supplementary Table S2). Associations between the vitamin D-related DP and MetS prevalence are shown in Table 3. The DP was associated with a lower risk of MetS prevalence, particularly in men, with a 12% (95% CI: 4–20%; P-value = 0.006) reduction in risk for a one-unit increase in the DP score. In particular, men with higher DP scores had a 25% lower risk (ORQ4vs.Q1 = 0.75; 95% CI 0.59, 0.97; p for trend < 0.01) compared to those with lower DP scores. However, no significant association was observed among women. For individual MetS components, the DP showed non-significant linear associations but indicated that the lowest risks of elevated FG in men (ORQ3vs.Q1 = 0.80; 95% CI 0.64, 1.00) and elevated TG in women (ORQ3vs.Q1 = 0.76, 95% CI = 0.57, 1.00) in the 3rd quartile groups of DP score.
Discussion
We examined the vitamin D status using serum 25(OH)D levels and a vitamin D-related DP associated with the serum 25(OH)D levels using RRR in Korean adults aged 19–64 years based on the KNHANES 2010–2014. In addition, we investigated cross-sectional associations of vitamin D status and its related DP with MetS risk in this study population. We found that men with a sufficient vitamin D level had a 44% lower risk of MetS and a 52% lower risk of elevated TG than those with a deficient vitamin D level. Women with a sufficient status of vitamin D had lower risks of elevated TG, reduced HDL-C, and elevated BP, even though there was no statistically significant association with MetS risk. The vitamin D-related DP identified in this study population was characterized by high intakes of vegetables, fish, fruit, and nuts and low intakes of eggs, oils, and mushrooms. This DP was associated with a 12% lower risk of MetS prevalence for a one-unit increase in the DP score in men, while no significant association was observed in women.
Vitamin D, mainly acquired through sun exposure and dietary intake, acts as a prohormone involved not only in classical functions related to bone metabolism but also in non-classical pleiotropic pathways affecting immune function, inflammation, antioxidant, and anti-fibrosis, which link to pathophysiological mechanisms of MetS and its component [8]. Vitamin D deficiency is, therefore, a potential risk factor for MetS affecting the cardiovascular system, increasing insulin resistance and obesity, and stimulating the renin-angiotensin-aldosterone system leading to hypertension [32]. Several studies have assessed the association of vitamin D with MetS, suggesting that higher 25(OH)D levels are inversely associated with MetS [33, 34]. A meta-analysis of 28 observational studies including ∼ 100 K participants [35] found that high levels of 25(OH)D in the adult population were associated with significant reductions in CVDs, T2D, and MetS. Another meta-analysis of 18 observational studies including a total of 41 K participants [36] also showed a significant inverse association between blood levels of 25(OH)D and the risk of MetS. In line with these previous studies, we found a significant inverse association between serum 25(OH)D levels and the prevalence of MetS, mainly in men, not women.
Regarding individual components of MetS, serum 25(OH)D was inversely associated with TG levels in both men and women in this study. Many previous studies showed this relationship, including a recent meta-analysis of 59 observational studies [37], suggesting that high levels of serum 25(OH)D reduce hypertriglyceridemia and dyslipidemia. Vitamin D might have both direct and indirect effects on serum lipid levels [38]. In vitro studies demonstrated that 1,25(OH)2D can directly control adipogenesis by blocking adipocyte differentiation [39, 40]. Indirectly, vitamin D can reduce serum lipids by increasing intestinal absorption of calcium, which leads to less intestinal absorption and more fecal excretion of fat [41], and/or by suppressing serum parathyroid hormone (PTH), which reduces lipolysis in vitro studies [42]. We also found that serum 25(OH)D was associated negatively with BP, but only in women, which could also be explained by the effect on the PTH-BP link [43]. Additionally, we found a positive association between HDL-C and serum 25(OH)D, also only in women. An underlying mechanism could be the role of vitamin D in the formation of HDL particles. Vitamin D can promote the formation of large HDL particles, affecting reverse cholesterol transport and preventing cardiovascular risk [44].
Our findings suggest sex differences in the effect of vitamin D related to MetS and its components as addressed in previous studies. Compelling evidence [45,46,47] shows a higher prevalence of metabolic disorders like obesity, T2D, and CVD in men compared to women (especially pre-menopausal) due to sex-specific genetic and hormonal differences. For instance, genetic studies revealed sex-specific effects of the X chromosome in CVD [47, 48], observational studies found higher insulin sensitivity in women [49], and large clinical and experimental evidence indicated sex hormones contribute to metabolic disease susceptibility [45], suggesting the protective effect of estrogens. In the current study, the Mets prevalence was twice as high in men (19.3%) compared to women (9.6%). In addition, a recent review suggests sex differences in vitamin D metabolism [50], such as the effect of sex hormones on the expression levels of vitamin D-related genes [51], which could also contribute to differential susceptibility to MetS. In line with that, the current study showed a higher MetS prevalence rate in men (18.4%) than in women (10.0%) in the vitamin D deficiency group (25(OH)D < 10 ng/mL), suggesting a stronger link between vitamin D and MetS in men.
In particular, this sex difference was more pronounced in associations with FG levels. Although previous evidence suggests that vitamin D deficiency links to the onset of diabetes [52, 53], our study found that serum 25(OH)D level was positively associated with FG level in women. Several studies indicated that insufficient levels of vitamin D induced the onset of insulin resistance, potentially leading to non-insulin-dependent diabetes by the disruption of insulin sensitivity, β-cell function, or a combination of both [54,55,56]. Despite the evidence, results from several observational studies remain an open issue for intense debate on the relationship between 25(OH)D levels and diabetes risk [57, 58]. In addition, some studies showed sex differences in the vitamin D and FG relationship. For instance, a cross-sectional study among 542 Arab Americans found a significant inverse correlation between 25(OH)D concentration and FG in men but not women [59], consistent with our findings. As mentioned, women have higher insulin sensitivity, especially during the reproductive period, due to the protective effect of estrogens. The interaction between vitamin D and estrogen levels might influence FG levels in women. Therefore, future studies examining the associations between vitamin D status and diabetes-related outcomes should consider variations in sex hormones.
This study also aimed to identify vitamin D-related DPs, and then examine their association with MetS prevalence in Korean adults. Traditional nutritional assessment methods, relying on self-reported dietary intake data and food composition databases, have limitations in estimating vitamin D intake due to their inability to capture its bioavailability and interactions with other micronutrients and biomolecules [17]. Consequently, previous studies have shown inconsistent results. Moreover, conventional DP analysis techniques, such as principal component, factor, or cluster analysis, share these limitations. Therefore, this study applied the RRR technique to address these issues. We identified a vitamin D-related DP of 17 food groups by RRR, using 25(OH)D as a proxy of vitamin D and also a potential mediator of MetS demonstrated in previous and current studies. Many studies have reported the association between DPs and MetS [23, 34, 60,61,62,63,64,65]. Yet, vitamin D-specific DPs using RRR were rarely studied.
In this study, the vitamin D-related DP was characterized by high intakes of vegetables, fish, fruits, and nuts and low intakes of eggs, oil, and mushrooms. This result is similar to ‘healthy’ and ‘prudent’ DPs in other studies on DPs and MetS. Vitamin D-rich diets include both animal and plant foods. The main form of vitamin D in animal-based food is cholecalciferol (vitamin D3), rich in fatty fish, meat, eggs, milk, and dairy products, while the main form in plant-based food is ergocalciferol (vitamin D2), rich in cereal grains, vegetables, fruits, mushrooms [8]. Cholecalciferol (vitamin D3) is known to be more effective in increasing and maintaining circulating 25(OH)D levels and the bioavailability is higher in animal-based and fortified foods, though data are still insufficient to draw definitive conclusions [66]. Fish intake is a key component of the vitamin D-related DP in the study, as a previous study based on KNHANES reported that the main food source of vitamin D among Korean adults was fish (71.3%) and then eggs (14.9%) [67]. In the current study, the DP was negatively associated with egg intake, reflecting a DP where a higher intake of fish corresponds with lower intakes of eggs and other animal-based food in this study population. Interestingly, vegetable intake was more strongly associated with this vitamin D-related DP than fish intake, which is likely aligned with dietary habits where people with healthier dietary patterns tend to consume more vegetables and fish. Additionally, in the Korean diet, Kimchi – a traditional dish of fermented cabbage with various types of sources – constitutes a significant portion of vegetable consumption and often includes fish-based sauces like anchovy or oyster, which might contribute to serum vitamin D levels in this study population.
The vitamin D-related DP high in vegetables, fish, fruits, and nuts was associated with lower risks of MetS and its components including FG and TG in our study. According to a meta-analysis of 28 cross-sectional studies and 3 cohort studies including ∼ 70 K participants [64], prudent and healthy patterns, high in fruit, vegetables, whole grains, fish and seafood, legumes, poultry, olive oil, nuts, seeds, and fat-free or low-fat dairy similar to the DP in our study, were associated with a lower risk of MetS. Also, in previous cohort studies in western populations [65, 68], DPs rich in fruits, vegetables, nuts, and fish were inversely associated with MetS risk. To date, one study among 1,092 Japanese adults showed that the DP extracted by using RRR with intakes of 6 MetS-related nutrients including vitamin D as response variables was high intakes of vegetables, fruits, fish, and natto, and was associated with reduced risk of MetS [23].
Our study, to the best of our knowledge, is the first to examine a vitamin D-specific DP derived by RRR with 25(OH)D and its association with MetS prevalence risk in Korean adults aged 19–64 years using large, representative, population-based data. However, there are some limitations. First, the cross-sectional design of the study limits our ability to explain causal relationships. Second, we used dietary data from a single 24-hour recall, which may not fully represent usual intake. However, serum 25(OH)D levels respond to vitamin D intake in a relatively short time. A dose-response study demonstrated that peak serum level (Cmax) was reached 7 days after vitamin D intake, with a half-life of approximately one month [69]. Therefore, it would be more appropriate to derive the DP related to serum 25(OH)D levels using short-term intake data, such as 24-hour recall data. In addition, we could not account for other unmeasured factors that could affect both serum 25(OH)D levels and MetS, such as sex-specific genetic and hormonal variation (e.g., estrogen) and sun exposure. The limitation regarding sun exposure arises because the dates of blood collection/examination, which could reflect seasonal variation, were not available due to the data privacy constraints of KNHANES. Given these limitations, therefore, the interpretation of the results should be cautious.
In conclusion, findings from this study suggest that maintaining sufficient vitamin D status and adhering to a DP with high intakes of vegetables, fish, fruits, and nuts could prevent MetS and dyslipidemia, especially in Korean men. Our results also indicate sex differences in MetS susceptibility related to vitamin D and its related DP. Future studies in prospective or interventional settings are required with considering sex-specific genetic and hormonal variation, which could aid in developing sex-specific nutrition guidelines or educational programs to prevent MetS.
References
Grundy SM (2008) Metabolic syndrome pandemic. Arterioscler Thromb Vasc Biol 28:629–636. https://doi.org/10.1161/ATVBAHA.107.151092
O’Neill S, O’Driscoll L (2015) Metabolic syndrome: a closer look at the growing epidemic and its associated pathologies. Obes Rev 16:1–12. https://doi.org/10.1111/obr.12229
Pannu PK, Zhao Y, Soares MJ et al (2017) The associations of vitamin D status and dietary calcium with the metabolic syndrome: an analysis of the victorian Health Monitor survey. Public Health Nutr 20:1785–1796. https://doi.org/10.1017/S1368980016001609
Lear SA, Gasevic D (2019) Ethnicity and metabolic syndrome: implications for assessment, management and prevention. Nutrients 12:15. https://doi.org/10.3390/nu12010015
Park YS, Kang SH, Jang S-I et al (2022) Association between lifestyle factors and the risk of metabolic syndrome in the South Korea. Sci Rep 12:13356. https://doi.org/10.1038/s41598-022-17361-2
Fahed G, Aoun L, Bou Zerdan M et al (2022) Metabolic syndrome: updates on pathophysiology and management in 2021. Int J Mol Sci 23(2):786. https://doi.org/10.3390/ijms23020786
Xu H, Li X, Adams H et al (2019) Etiology of metabolic syndrome and dietary intervention. Int J Mol Sci 20(1):128. https://doi.org/10.3390/ijms20010128
Melguizo-Rodríguez L, Costela-Ruiz VJ, García-Recio E et al (2021) Role of vitamin D in the metabolic syndrome. Nutrients 13:830. https://doi.org/10.3390/nu13030830
Wang H, Chen W, Li D et al (2017) Vitamin D and chronic diseases. Aging Dis 8:346. https://doi.org/10.14336/AD.2016.1021
Bea JW, Jurutka PW, Hibler EA et al (2015) Concentrations of the vitamin D metabolite 1,25(OH)2D and odds of metabolic syndrome and its components. Metab Clin Exp 64:447–459. https://doi.org/10.1016/j.metabol.2014.11.010
Parva NR, Tadepalli S, Singh P al (2018) Prevalence of vitamin D deficiency and associated risk factors in the US population (2011–2012). Cureus 10:e2741. https://doi.org/10.7759/cureus.2741
Cashman KD, Dowling KG, Škrabáková Z et al (2016) Vitamin D deficiency in Europe: pandemic? Am J Clin Nutr 103:1033–1044. https://doi.org/10.3945/ajcn.115.120873
Park HY, Lim YH, Park JB et al (2020) Environmental and occupation factors associated with vitamin D deficiency in Korean adults: the Korea National Health and Nutrition Examination Survey (KNHANES) 2010–2014. Int J Environ Res Public Health 17:9166. https://doi.org/10.3390/ijerph17249166
Yoon H, Kim GS, Kim SG et al (2015) The relationship between metabolic syndrome and increase of metabolic syndrome score and serum vitamin D levels in Korean adults: 2012 Korean National Health and Nutrition Examination Survey. J Clin Biochem Nutr 57:82–87. https://doi.org/10.3164/jcbn.15-31
Yoon H, Jeong DK, Park CE et al (2017) The association between gender difference with metabolic syndrome, metabolic syndrome score and serum vitamin D levels in Korean adults. Int J Food Sci Nutr 68:121–129. https://doi.org/10.1080/09637486.2016.1221899
Bonakdaran S, Fakhraee F, Karimian MS et al (2016) Association between serum 25-hydroxyvitamin D concentrations and prevalence of metabolic syndrome. Adv Med Sci 61:219–223. https://doi.org/10.1016/j.advms.2016.01.002
Cashman KD, Kiely M (2014) Recommended dietary intakes for vitamin D: where do they come from, what do they achieve and how can we meet them? J Hum Nutr Diet 27:434–442. https://pubmed.ncbi.nlm.nih.gov/24580775/
Hoffmann K, Schulze MB, Schienkiewitz A et al (2004) Application of a New Statistical Method to derive dietary patterns in Nutritional Epidemiology. Am J Epidemiol 159:935–944. https://doi.org/10.1093/aje/kwh134
Merz B, Frommherz L, Rist MJ et al (2018) Dietary pattern and plasma BCAA-variations in healthy men and women—results from the KarMeN study. Nutrients 10(5):623. https://doi.org/10.3390/nu10050623
Biesbroek S, Van Der ADL, Brosens MC et al (2015) Identifying cardiovascular risk factor–related dietary patterns with reduced rank regression and random forest in the EPIC-NL cohort. Am J Clin Nutr 102:146–154. https://doi.org/10.3945/ajcn.114.092288
Lamichhane AP, Liese AD, Urbina EM et al (2014) Associations of dietary intake patterns identified using reduced rank regression with markers of arterial stiffness among youth with type 1 diabetes. Eur J Clin Nutr 68:1327–1333. https://doi.org/10.1038/ejcn.2014.96
Livingstone KM, McNaughton SA (2017) Dietary patterns by reduced rank regression are associated with obesity and hypertension in Australian adults. Br J Nutr 117:248–259. https://doi.org/10.1017/S0007114516004505
Bahari T, Uemura H, Katsuura-Kamano S et al (2018) Nutrient-derived dietary patterns and their association with metabolic syndrome in a Japanese population. J Epidemiol 28:194–201. https://doi.org/10.2188/jea.JE20170010
Yeh C-J, Chang H-Y, Pan W-H et al (2011) Time trend of obesity, the metabolic syndrome and related dietary pattern in Taiwan: from NAHSIT 1993–1996 to NAHSIT 2005–2008. Asia Pac J Clin Nutr 20:292–300
The Korea National Health and Nutrition Examination Survey (KNHANES), 2010–2014. Korea Disease Control and Prevention Agency
Grundy SM, Cleeman JI, Daniels SR et al (2005) Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Curr Opin Cardiol 112:2735–2752. https://doi.org/10.1161/CIRCULATIONAHA.105.169404
Choi SH, KIm DJ, Lee KE et al (2004) Cut-off value of waist circumference for metabolic syndrome patients in Korean adult population. J Korean Soc Study Obes 13: 53–60. https://www.jomes.org/journal/view.html?spage=53&volume=13&number=1
Choi HS (2013) Vitamin D status in Korea. Endocrinol Metab 28:12–16. https://doi.org/10.3803/EnM.2013.28.1.12
Lim S, Kim MJ, Lim S et al (2013) Association of vitamin D deficiency with incidence of type 2 diabetes in high-risk Asian subjects. Am J Clin Nutr 97:524–530. https://doi.org/10.3945/ajcn.112.048496
Van Schoor N, Lips P (2018) In: Feldman D (ed) Chap. 59 - Worldwide vitamin D status. In vitamin D (Fourth Edition). Academic, pp 15–40
Hoffmann K, Boeing H, Boffetta P et al (2005) Comparison of two statistical approaches to predict all-cause mortality by dietary patterns in German elderly subjects. Br J Nutr 93:709–716. https://doi.org/10.1079/bjn20051399
Prasad P, Kochhar A (2016) Interplay of vitamin D and metabolic syndrome: a review. Diabetes Metab Syndr 10:105–112. https://doi.org/10.1016/j.dsx.2015.02.014
Brenner DR, Arora P, Garcia-Bailo B et al (2011) Plasma vitamin D levels and risk of metabolic syndrome in canadians. Clin Invest Med 34:377–384. https://doi.org/10.25011/cim.v34i6.15899
Ahluwalia N, Raghavan R, Zhang G et al (2022) Vitamin D status and prevalence of metabolic syndrome by race and hispanic origin in US adults: findings from the 2007–2014 NHANES. Am J Clin Nutr 116:1400–1408. https://doi.org/10.1093/ajcn/nqac234
Parker J, Hashmi O, Dutton D et al (2010) Levels of vitamin D and cardiometabolic disorders: systematic review and meta-analysis. Maturitas 65:225–236. https://doi.org/10.1016/j.maturitas.2009.12.013
Ju SY, Jeong HS, Kim DH (2014) Blood vitamin D status and metabolic syndrome in the general adult population: a dose-response meta-analysis. J Clin Endocrinol Metab 99:1053–1063. https://doi.org/10.1210/jc.2013-3577
Bahadorpour S, Hajhashemy Z, Saneei P (2023) Serum 25-hydroxyvitamin D levels and dyslipidemia: a systematic review and dose-response meta-analysis of epidemiologic studies. Nutr Rev 81:1–25. https://doi.org/10.1093/nutrit/nuac038
Jorde R, Grimnes G (2011) Vitamin D and metabolic health with special reference to the effect of vitamin D on serum lipids. Prog Lipid Res 50:303–312. https://doi.org/10.1016/j.plipres.2011.05.001
Blumberg JM, Tzameli I, Astapova I et al (2006) Complex role of the vitamin D receptor and its ligand in adipogenesis in 3T3-L1 cells. J Boil Chem 281:11205–11213. https://doi.org/10.1074/jbc.M510343200
Kong, Li YC (2006) Molecular mechanism of 1,25-dihydroxyvitamin D3 inhibition of adipogenesis in 3T3-L1 cells. Am J Physiol Endocrinol Metab 290:916–924. https://doi.org/10.1152/ajpendo.00410.2005
Boon N, Hul GBJ, Stegen JHCH et al (2007) An intervention study of the effects of calcium intake on faecal fat excretion, energy metabolism and adipose tissue mRNA expression of lipid-metabolism related proteins. Int J Obes 31:1704–1712. https://doi.org/10.1038/sj.ijo.0803660
Zemel MB, Shi H, Greer B et al (2000) Regulation of adiposity by dietary calcium. FASEB J 14:1132–1138. https://doi.org/10.1096/fasebj.14.9.1132
Jorde R, Svartberg J, Sundsfjord J (2005) Serum parathyroid hormone as a predictor of increase in systolic blood pressure in men. J Hypertens 23:1639–1644. https://doi.org/10.1097/01.hjh.0000179764.40701.36
Alkerwi A, Sauvageot N, Gilson G et al (2015) Prevalence and correlates of vitamin D deficiency and insufficiency in Luxembourg adults: evidence from the observation of cardiovascular risk factors (ORISCAV-LUX) study. Nutrients 7:6780–6796. https://doi.org/10.3390/nu7085308
Tramunt B, Smati S, Grandgeorge N et al (2020) Sex differences in metabolic regulation and diabetes susceptibility. Diabetologia 63:453–461. https://doi.org/10.1007/s00125-019-05040-3
Kautzky-Willer A, Leutner M, Harreiter J (2023) Sex differences in type 2 diabetes. Diabetologia 66:986–1002. https://doi.org/10.1007/s00125-023-05891-x
Regitz-Zagrosek V, Gebhard C (2023) Gender medicine: effects of sex and gender on cardiovascular disease manifestation and outcomes. Nat Rev Cardiol 20:236–247. https://doi.org/10.1038/s41569-022-00797-4
Ventura-Clapier R, Dworatzek E, Seeland U et al (2017) Sex in basic research: concepts in the cardiovascular field. Cardiovasc Res 2017 113:711–724. https://doi.org/10.1093/cvr/cvx066
Kautzky-Willer A, Brazzale AR, Moro E, Vrbíková J et al (2012) Influence of increasing BMI on insulin sensitivity and secretion in normotolerant men and women of a wide age span. Obes (Silver Spring) 20:1966–1973. https://doi.org/10.1038/oby.2011.384
Wierzbicka A, Oczkowicz M (2022) Sex differences in vitamin D metabolism, serum levels and action. Br J Nutr 128:2115–2130. https://doi.org/10.1017/S0007114522000149
Liel Y, Shany S, Smirnoff P et al (1999) Estrogen increases 1,25-dihydroxyvitamin D receptors expression and bioresponse in the rat duodenal mucosa. Endocrinology 140:280–285. https://doi.org/10.1210/endo.140.1.6408
Berridge MJ (2017) Vitamin D deficiency and diabetes. Biochem J 474:1321–1332. https://doi.org/10.1042/BCJ20170042
Zhang Y, Tan H, Tang J et al (2020) Effects of vitamin D supplementation on prevention of type 2 diabetes in patients with prediabetes: a systematic review and meta-analysis. Diabetes Care 43:1650–1658. https://doi.org/10.2337/dc19-1708
Gagnon C, Daly RM, Carpentier A et al (2014) Effects of combined calcium and vitamin D supplementation on insulin secretion, insulin sensitivity and β-Cell function in multi-ethnic vitamin D-deficient adults at risk for type 2 diabetes: a pilot randomized, placebo-controlled trial. PLoS ONE 9:e109607. https://doi.org/10.1371/journal.pone.0109607
Gao Y, Wu X, Fu Q et al (2015) The Relationship between Serum 25-Hydroxy Vitamin D and isulin sensitivity and β-Cell fFunction in newly diagnosed type 2 diabetes. J Diabetes Res 2015: e636891, https://doi.org/10.1155/2015/636891
Park JE, Pichiah PBT, Cha YS (2018) Vitamin D and metabolic diseases: growing roles of vitamin D. J Obes Metab Syndr 27:223–232. https://doi.org/10.7570/jomes.2018.27.4.223
Scragg R, Sowers M, Bell C (2004) Serum 25-hydroxyvitamin D, diabetes, and ethnicity in the Third National Health and Nutrition Examination Survey. Diabetes Care 27:2813–2818. https://doi.org/10.2337/diacare.27.12.2813
Das G (2017) Vitamin D and type 2 diabetes. Practical Diabetes 34:19–24b. https://doi.org/10.1002/pdi.2072
Pinelli NR, Jaber LA, Brown MB et al (2010) Serum 25-Hydroxy vitamin D and insulin resistance, metabolic syndrome, and glucose intolerance among arab americans. Diabetes Care 33:1373–1375. https://doi.org/10.2337/dc09-2199
Esmaillzadeh A, Kimiagar M, Mehrabi Y et al (2007) Dietary patterns, insulin resistance, and prevalence of the metabolic syndrome in women. Am J Clin Nutr 85:910–918. https://doi.org/10.1093/ajcn/85.3.910
Fabiani R, Naldini G, Chiavarini M (2019) Dietary patterns and metabolic syndrome in adult subjects: a systematic review and meta-analysis. Nutrients 11:2056. https://doi.org/10.3390/nu11092056
Lutsey PL, Steffen LM, Stevens J (2008) Dietary intake and the development of the metabolic syndrome: the atherosclerosis risk in communities study. Circulation 117:754–761. https://doi.org/10.1161/circulationaha.107.716159
Panagiotakos DB, Pitsavos C, Skoumas Y et al (2007) The Association between food patterns and the metabolic syndrome using principal components analysis: the ATTICA Study. J Am Diet Assoc 107:979–987. https://doi.org/10.1016/j.jada.2007.03.006
Rodríguez-Monforte M, Sánchez E, Barrio F et al (2017) Metabolic syndrome and dietary patterns: a systematic review and meta-analysis of observational studies. Eur J Nutr 56:925–947. https://doi.org/10.1007/s00394-016-1305-y
Steffen LM, Horn LV, Daviglus ML et al (2014) A modified Mediterranean diet score is associated with a lower risk of incident metabolic syndrome over 25 years among young adults: the CARDIA (coronary artery risk development in young adults) study. Br J Nutr 112:1654–1661. https://doi.org/10.1017/s0007114514002633
Chungchunlam SMS, Moughan PJ (2023) Comparative bioavailability of vitamins in human foods sourced from animals and plants. Crit Rev Food Sci Nutr 31:1–36. https://doi.org/10.1080/10408398.2023.2241541
Yoo K, Cho J, Ly S (2016) Vitamin D intake and serum 25-Hydroxyvitamin D levels in Korean adults: analysis of the 2009 Korea National Health and Nutrition Examination Survey (KNHANES IV-3) using a newly established vitamin D database. Nutrients 8:610. https://doi.org/10.3390/nu8100610
Rumawas ME, Meigs JB, Dwyer JT et al (2009) Mediterranean-style dietary pattern, reduced risk of metabolic syndrome traits, and incidence in the Framingham offspring cohort. Am J Clin Nutr 90:1608–1614. https://doi.org/10.3945/ajcn.2009.27908
Oliveri B, Mastaglia SR, Brito et al (2015) Vitamin D3 seems more appropriate than D2 to sustain adequate levels of 25OHD: a pharmacokinetic approach. Eur J Clin Nutr 69:697–702. https://doi.org/10.1038/ejcn.2015.16
Acknowledgements
The authors appreciate all participants in the Korean NHANES.
Author information
Authors and Affiliations
Contributions
The study concept, design, and method were developed by all authors together. All statistical analysis was performed by YL and supervised by HN. The first draft of the manuscript was written by YL, and then all authors reviewed and edited previous versions of the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, Y., Noh, H. & Lee, S. Association of a dietary pattern related to serum vitamin D levels with metabolic syndrome risk among Korean adults: based on the Korean national health and nutrition examination survey. Eur J Nutr (2024). https://doi.org/10.1007/s00394-024-03463-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00394-024-03463-2