Abstract
Purpose
To evaluate the association between intuitive eating and health outcomes in patients with type 2 diabetes in a cross-sectional study.
Methods
Consecutively, outpatients attending at university hospital underwent clinical, laboratory, lifestyle, and eating behavior evaluations. Intuitive eating was assessed using the Intuitive Eating Scale-2 (IES-2), and the Three Factor Eating Questionnaire-21 was adopted as a confirmatory tool for disordered eating behavior. Optimized health outcomes were considered according to the American Diabetes Association criteria for BMI, HbA1c, lipid profile, and blood pressure values, and the International Diabetes Federation criteria for waist circumference. Considering the answers of the IES-2 items, patients were grouped by latent class analysis, and their characteristics were compared by appropriate tests.
Results
In total, 267 patients were evaluated: 62.2% women, with 60 (53–65) years, BMI 31.9 ± 5.4 kg/m², diabetes duration of 16 ± 9 years, HbA1c 8.5 ± 1.5%, and an IES-2 total score of 58 (50–67)%. Three intuitive eating groups were identified: higher intuitive eating, nonemotional-oriented coping, and lower intuitive eating. Patients with higher intuitive eating have higher chances of having optimized BMI and serum triglycerides values compared to patients with lower intuitive eating. Also, the 10-point increase on IES-2 was associated with a 0.62 kg/m² reduction on BMI values (95%CI -1.18;-0.06), 1.90 cm on waist circumference (95%CI -3.26;-0.54), and 23 mg/dL in serum triglycerides values (95%CI -38.27;-7.40) after adjustment for age, sex, psychotropic drug use, medication effect score, smoking, and BMI.
Conclusion
Intuitive eating seems to be associated with optimized health outcomes and may contribute to better personalized interventions in nutritional treatment that promote adaptive behaviors in diabetes management, but should be tested.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus is a complex, chronic disease characterized by the presence of hyperglycemia, which occurs when the body cannot produce or effectively use insulin [1]. Type 2 diabetes (T2D) accounts for the majority (over 90%) of diabetes cases worldwide [2]. Diabetes Self-Management Education and Support, medical nutrition therapy, routine physical activity, smoking cessation counseling when needed, health behavior counseling, and psychosocial care are essential aspects to achieve diabetes treatment goals. In this context, nutrition therapy for adults with diabetes aims to promote and support healthy eating behaviors to improve overall health, achieve and maintain body weight goals, attain individualized glycemic, blood pressure, and lipid goals, and delay or prevent diabetes complications [3].
However, adherence to dietary prescriptions is still a challenge, and achieving long-term and sustainable changes is clearly difficult [4]. This most likely results from a gradual return to old lifestyle habits that occurs due to the complex interaction among biological, environmental, behavioral, and cognitive factors [5]. Also, distress is a very common condition in T2D [3] (36% prevalence rate) and has negative effects on self-care behaviors [6]. In this sense, new strategies, so-called “non-diet approaches”, have been proposed to encourage sustainable dietary changes and improvements in disordered eating patterns, self-esteem, and depression [7]. Intuitive eating approach has gained increasing attention as an alternative or complementary form of dietary treatment in diabetes management [8].
Intuitive eating is described as an adaptive form of eating characterized by an intentional focus on physiological hunger and satiety cues rather than external cues to guide food intake [9]. The Intuitive Eating Scale-2 (IES-2) is a scale developed to assess the presence of intuitive eating attitudes and behaviors [10]. In a sample of Brazilian Portuguese-speaking adults, a study evaluated the psychometric properties of IES-2 and suggested that the instrument may be useful for assessing eating behavior in both males and females [11]. Associations between intuitive eating and lower BMI [12,13,14,15,16,17], weight stability [18], psychological health and well-being [14, 19], and higher fruit and vegetable intake [13, 20] have been observed in the overall population of different countries worldwide. However, studies associating intuitive eating with health outcomes in the diabetes population are still scarce [21,22,23], especially in T2D [24,25,26]. To date, intuitive eating has been inversely associated with poor glycemic control in a single cross-sectional study with 179 patients with T2D living in Vitória, Brazil [24]. The same authors observed that eating more intuitively, by considering the signs of hunger and satiety, was associated with greater body satisfaction in the same sample [25].
Therefore, this study hypothesized that patients with T2D and greater intuitive eating have optimized health outcomes compared to those with lower levels of intuitive eating. Thus, this study aimed to evaluate the association between intuitive eating and optimized health outcomes in patients with T2D. Establishing this association would benefit the development of more personalized interventions to improve adherence to nutritional prescriptions and promote sustainable changes in eating behavior within this population.
Methods
Study design and sample
This cross-sectional study was conducted on outpatients with T2D who attended primary or secondary care at the Hospital de Clínicas de Porto Alegre, Brazil, from July 2021 to October 2022. The study adhered to the principles outlined in the Declaration of Helsinki, and all procedures involving patients were approved by the Research Ethics Committee of the Hospital de Clínicas de Porto Alegre, Brazil (2020 − 0654). All patients provided written, informed consent.
For sample size estimation, a difference of 0.13 points was considered in the mean total score obtained from IES-2 between individuals with HbA1c within (SD = 0.26) and outside the target recommended by the American Diabetes Association (SD = 0.46) [24], with a 5% margin of error and an 80% confidence level. In total, 260 patients were required for this study. The OpenEpi program version 3.01 was used [27].
Patients
T2D diagnosis was based on the following criteria: glycated hemoglobin (HbA1c) ≥ 6.5%, or fasting plasma glucose value ≥ 126 mg/dL, or the two-hour plasma glucose value during a 75-gram oral glucose tolerance test ≥ 200 mg/dL [3], with no previous episode of ketoacidosis or documented ketonuria, and no use of insulin in the five years since diagnosis [28]. Patients were included if they presented with an age < 70 years and ≤ 12% HbA1c.
Exclusion criteria were maturity-onset diabetes of the young (MODY), severe neuropathy, cancer, chemical dependence/alcoholism, chronic steroid use, gastroparesis, pregnancy and/or lactation, acute coronary syndrome episode in the previous 60 days, wheelchair users, stage V chronic kidney disease, chronic obstructive pulmonary disease, diagnosis of eating disorders, ≥ 50 kg/m² body mass index (BMI), and those who have undergone bariatric surgery or were on use of enteral or parenteral nutrition. Patients who were unable to answer questions were also excluded.
Data collection
For the consecutive selection of participants, electronic medical records were assessed following the regulations of the General Data Protection Law. Eligible patients were invited to participate in the study and answered the informed consent document, scales, and questionnaires over the phone. Subsequently, patients went to the hospital for blood sample collection, anthropometric assessment, and to provide their informed consent signature. After data collection, all patients received nutritional counseling according to the Diabetes Plate Method [3].
Clinical and laboratory evaluations
Patients were subjected to clinical, laboratory, and lifestyle evaluations. Information about clinical data such as duration of diabetes, associated comorbidities, diabetes complications, and medication use was collected from the patient’s electronic medical records in the medical visit of the closest date to the nutritional assessment.
Diabetic kidney disease was defined by the presence of an estimated < 60 mL/min/1.73m2 glomerular filtration rate and/or persistently elevated urinary albumin excretion, defined as ≥ 14 mg/dL albuminuria [3, 29]. Diabetic retinopathy was considered as the presence of mild, moderate, and severe nonproliferative or proliferative diabetic retinopathy by fundoscopic examination via a specialist diagnosis [30]. Diabetic neuropathy diagnosis described in the medical history by a 10-g monofilament exam was considered [3]. Cardiovascular disease was defined by a current or previous history of cardiovascular disease, such as coronary heart disease, peripheral arterial disease, heart failure, myocardial infarction, and/or stroke.
The Medication Effect Score (MES) was estimated to assess the intensity of glucose-lowering agents in reducing HbA1c based on the doses and potency of medications. First, the maximum daily dose of each medication was determined. Then, the actual drug dose was divided by the maximum drug dose and multiplied by a drug-specific adjustment factor corresponding to the median absolute decrease in HbA1c for each agent. These products were then summed for the final MES [31].
Information about the use of psychotropic drugs that interact with appetite and weight loss/gain was also taken from the electronic medical records and checked with patients, considering the use of antidepressants (tricyclics, selective serotonin reuptake inhibitors, monoamine oxidase inhibitors, and antidepressants with other mechanisms of action); mood stabilizers; antipsychotics (typical and atypical); and benzodiazepines.
Sitting blood pressure was measured three times, after a 5-minute rest, using a digital sphygmomanometer (Omron® HEM-705CP). Hypertension was defined as ≥ 140 mmHg systolic blood pressure or ≥ 90 mmHg diastolic blood pressure measured on two occasions or the use of antihypertensive drugs [32].
Blood samples were obtained after a 12-hour fast, and all tests were performed at the Laboratory Diagnostic Service of the Hospital de Clínicas de Porto Alegre, Brazil. Plasma glucose was measured by the enzymatic colorimetric method; HbA1c was measured by the high-performance liquid chromatography in a variant II Turbo System (4.0–6.0% reference range); serum values of total cholesterol, high density lipoprotein (HDL) cholesterol, and triglycerides were measured by enzymatic colorimetric methods. Low-density lipoprotein (LDL) cholesterol was estimated using the Friedewald equation (LDL cholesterol = total cholesterol − HDL cholesterol − triglycerides/5) [33] for patients with triglycerides values < 400 mg/dL.
Anthropometric evaluation
Anthropometric data (weight, height, and waist circumference) were evaluated. Weight and height were measured with patients barefoot and wearing light clothing (Welmy® mechanical scale, 150 kg capacity, and stadiometer with 210 cm capacity). Waist circumference was measured at the midpoint between the upper edge of the iliac crest and the last floating rib, close to the navel, with a flexible, non-elastic fiberglass tape. BMI was estimated using the equation: weight (kg)/height (m)².
Health outcomes
Health outcomes evaluated were BMI, glycemic control, lipid profile, blood pressure values, and diabetes complications. Patients were considered with optimized health outcomes according to the following criteria: BMI < 25 kg/m² for adults [34] or < 27 kg/m² for older adults [35]; waist circumference < 80 cm for women or < 94 cm for men [36]; serum triglycerides < 150 mg/dL; serum HDL-cholesterol > 40 mg/dL for men and > 50 mg/dL for women; LDL-cholesterol < 100 mg/dL [3]; systolic blood pressure < 140 mmHg; and diastolic blood pressure < 90 mmHg [30]. For HbA1c classification, patients were considered within adequate glycemic control when presenting < 7% HbA1c values when adults and older adults presented up to one associated comorbidity; <7.5% HbA1c values when older adults presented two associated comorbidities, and < 8% HbA1c values when older adults presented three or more associated comorbidities. The common comorbidities considered were diabetes complications, previous history of cardiovascular disease or stroke, hypertension, obstructive sleep apnea-hypopnea syndrome, urinary incontinence, and depression [3].
Sociodemographic and lifestyle covariates
Patients were classified as current, former, and nonsmokers and self-identified as White or non-White. Socioeconomic class was evaluated by a standardized Brazilian questionnaire [37], and patients were classified as low-income if their socioeconomic stratum was C1, C2, or D/E. The short version of the International Physical Activity Questionnaire was used to evaluate physical activity during a typical week, in minutes [38]. Patients whose reported activities corresponded to < 600 metabolic equivalent tasks per week were considered to have sedentary lifestyles [39].
Intuitive eating assessment
Intuitive eating was assessed using the Brazilian Portuguese version of the IES-2 [11], applied face-to-face or remotely by trained nutritionists. The 23-item scale evaluates an individual’s tendency to follow physiological signs of hunger and satiety using four factors (subscales): Unconditional Permission to Eat (six items), Eating for Physical Rather than Emotional Reasons (eight items), Reliance on Hunger and Satiety Cues (six items), and Body-Food Choice Congruence (three items). All items are measured via a 5-point Likert scale, from strongly disagree (one point) to strongly agree (five points), except questions 1, 2, 4, 5, 9, 10, and 11, which are counted with a reverse score. The average obtained from the sum of the questions for the total score and each subscale was converted to a scale ranging from 0 to 100% with the following equation: [(result of the questions multiplied by the factor − the lowest possible score) / scale of possible points * 100]. For instance, the intuitive eating total score was estimated accordingly: [(result of the questions multiplied by the factor − 23) / 92 * 100], Unconditional Permission to Eat and Reliance on Hunger and Satiety Cues subscales: [(result of the questions multiplied by the factor − 6) / 24 * 100], Eating for Physical Rather than Emotional Reasons subscale [(result of the questions multiplied by the factor − 8) / 32 * 100], and Body-Food Choice Congruence subscale: [(result of the questions multiplied by the factor − 3) / 12 * 100]. Each intuitive eating score was considered as continuous variables. Higher scores indicate higher levels of intuitive eating attitudes. In this sample, fit indices of IES-2 were adequate [X² = 312.606, df = 224, p < 0.001; X²/df = 1.39; RMSEA = 0.039 (90%CI 0.028;0.048); SRMR = 0.070; CFI = 0.975; TLI = 0.972] according to confirmatory factorial analysis [40]. Additionally, the internal consistency of the IES-2 was found to be acceptable, with a Cronbach’s α of 0.81 for the overall sample. Moreover, the reliability for its subscales was deemed adequate (α = 0.73–0.87), except for the Unconditional Permission to Eat subscale (α = 0.44).
Eating behavior assessment
To enhance comprehension of eating behaviors within our population, we used another instrument assessing eating behaviors. The 21-item Three Factor Eating Questionnaire (TFEQ-R21), adapted to Brazilian Portuguese [41], was applied face-to-face or remotely by trained nutritionists and was used to assess three factors (subscales) of eating behavior: cognitive restraint (six items); emotional eating (six items); and uncontrolled eating (nine items). Participants responded to items on a 4-point Likert scale, and item 21 was answered with an 8-point Likert scale, which was subsequently turned into a 4-point scale. Questions 1–16 are counted with a reverse score. The average obtained from the sum of the questions for the total score and each subscale was converted to a scale ranging from 0 to 100. Each eating behavior score was considered as continuous variables. Higher scores indicate greater cognitive restraint, uncontrolled eating, or emotional eating. In the current sample, fit indices of TFEQ-R21 were adequate [X² = 255.291, df = 186, p < 0.001; X²/df = 1.37; RMSEA = 0.040 (90%CI 0.027;0.051); SRMR = 0.070; CFI = 0.988; TLI = 0.987] according to confirmatory factorial analysis [40]. The TFEQ-R21 exhibited strong internal consistency (α = 0.87) across the entire sample, with α values of 0.58 for the cognitive restraint, 0.95 for emotional eating, and 0.89 for uncontrolled eating subscales.
Statistical analysis
A latent class analysis (LCA) was performed to identify distinct homogenous groups (latent class) based on responses to IES-2 items. All LCA analyses were conducted with the poLCA package (Polytomous Variable Latent Class Analysis) available in the library of the R statistical software version 4.3.2 for Microsoft. To identify the groups, we first estimated a one class model and then added classes until we identified the model with the best fit (data shown in Table 1in supplementary material): The most adjusted model presented three latent classes (AIC = 8818.086, BIC = 9320.301, df = 127, and entropy = 0.9610). In order to guarantee a better adjustment of data, the 5-point Likert scale was recoded into a 3-point Likert scale (whereas strongly disagree and disagree = 1, neutral = 2, agree and strongly agree = 3 points).
The normality of the variables was assessed by the Kolmogorov-Smirnov test. Descriptive analysis of the variables was performed, with the continuous variables being presented as mean (standard deviations) or median (interquartile range) according to their distribution. Categorical variables were presented as absolute and relative frequencies. The chi-square test, one-way analysis of variance (ANOVA; Bonferroni post hoc test), and the Kruskal Wallis test (Bonferroni post hoc correction) were used to compare differences between intuitive eating classes (denominated groups).
Models of logistic regression were used to assess a possible association between intuitive eating groups and optimized health outcomes (BMI, HbA1c, lipid profile, blood pressure values, and diabetes complications). The first analysis (Model 1) was adjusted for age, sex, psychotropic drug use, MES, and smoking. The second analysis (Model 2) was additionally adjusted for BMI. Furthermore, linear regression was used to assess the association between the 10-point increase on IES-2 and optimized health outcomes, adjusting for the same confounders.
Values of p < 0.05 (two-tailed) were considered statistically significant. The IBM SPSS version 20.0 (PASW Inc., Chicago, IL) was used to perform the analyses.
Results
In total, 1,896 electronic records of outpatients were screened for eligibility criteria, and 540 patients were considered eligible for the study. Of these, 292 patients consented to participate, and 267 attended clinical and/or anthropometric evaluations (Fig. 1). Most of the sample consisted of women (n = 166; 62.2%), attended to in specialized care (n = 223; 83.5%), with a median age of 60 (53–65) years, 31.9 ± 5.4 kg/m² BMI, diabetes duration of 16 ± 9 years, and 8.5 ± 1.5% HbA1c. The median of the total score in IES-2 was 58% (50–67%). In this sample, 27 (11.7%) patients had a normal BMI, 63 (24%) patients had optimized HbA1c values, 28 (12.5%) patients had optimized lipid values, and 152 (72.7%) patients had optimized blood pressure values. We did not observe differences in the total score of IES-2 between patients with or without the optimized HbA1c values: 61% (53–70%) vs. 58% (49–66%), P = 0.07.
Three intuitive eating groups were identified by LCA, and Table 1 shows the medians and interquartile ranges of eating behavior patterns according to IES-2. Patients in Group 3 presented higher scores on the IES-2 total score [64% (58–72%)] and respective subscales (especially “Eating for Physical Rather than Emotional Reasons” and “Reliance on Hunger and Satiety Cues”), when compared with Group 2 [55% (51–61%)] and Group 1 [41% (37–48%); p < 0.001]. Group 2 patients had higher scores on the IES-2 subscale “Eating for Physical Rather than Emotional Reasons” and lower scores on emotional and uncontrolled eating than Group 1 patients (p < 0.001 for all comparisons). No difference in the “Unconditional Permission to Eat” and cognitive restraint subscales was observed among the three groups. Also, Group 3 presented lower scores of emotional and uncontrolled eating according to TFEQ-R21 when compared to the other groups (p < 0,001 for all comparisons). In this sense, Group 3 was named Patients with higher intuitive eating (n = 168), Group 2 had lower scores on the IES-2, but no eating for emotional reasons and was named nonemotional-oriented coping (n = 32), and Group 1 presented lower scores on the IES-2 and was named patients with lower intuitive eating (n = 67). The box plot illustrates the distribution of each subscale values of IES-2 among different groups (see Fig. 1 in supplementary material).
Table 2 shows the sociodemographic, clinical, and nutritional characteristics of patients according to Groups. Patients with lower intuitive eating included a higher proportion of women, presence of obesity, presented a higher proportion of psychotropic drug use, and higher triglycerides values than those with higher intuitive eating (p < 0.05 for all analyses), but not in comparison with the nonemotional-oriented coping patients. Higher intuitive eating and nonemotional-oriented coping patients presented significantly lower MES and HbA1c values when compared to patients with lower intuitive eating (p < 0.05 for both analyses). We did not observe differences in the use of diabetes medication between the three intuitive eating groups. The non-insulin glucose-lowering agents used by our sample were metformin, glyburide, gliclazide, saxagliptin, sitagliptin, dapagliflozin, and empagliflozin. Other differences in clinical, laboratory, and anthropometric values were not observed among the three groups.
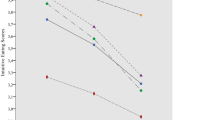
Figure 2 shows the proportion of patients with optimized health outcomes according to intuitive eating groups. Patients with higher intuitive eating presented a higher proportion of normal BMI and optimized triglycerides values than other groups (p < 0.01 for both comparisons). Patients of the nonemotional-oriented coping group presented a higher proportion of patients with optimized HbA1c values (41.9%) compared to patients with higher intuitive eating (25.6%) or patients with lower intuitive eating (11.9%), P < 0.01.
Proportion of patients with optimized health outcomes according to intuitive eating groups. *P < 0.01 (Chi-square test). BMI, body mass index; WC, waist circumference; HbA1c, glycated hemoglobin; HDL-c, HDL-cholesterol; LDL-c, LDL-cholesterol; SBP, systolic blood pressure; DBP, diastolic blood pressure; Diabetes complications considered: diabetic kidney disease, diabetic retinopathy, diabetic neuropathy, and/or cardiovascular disease
Models of logistic regression were performed to assess the possible association between higher intuitive eating (Group 3) or nonemotional-oriented coping (Group 2) and optimized health outcomes (as dependent variables). Table 3 shows these analyses. Patients with higher intuitive eating (Group 3) have a higher chance to have optimized BMI (OR = 8.94; 95%CI 1.14–70.13) and triglycerides values (OR = 3.45; 95%CI 1.64–7.26) compared to patients with lower intuitive eating (Group 1) after adjusting for age, sex, psychotropic drug use, MES, smoking, and BMI (except for anthropometric outcomes). Patients with nonemotional-oriented coping (Group 2) have a higher chance to have optimized HbA1c values (OR = 4.11; 95%CI 1.16–14.52) compared to patients with lower intuitive eating (Group 1), after adjusting for the same confounder variables. We did not observe associations between other optimized health outcomes and higher intuitive eating (Group 1) or nonemotional-oriented coping (Group 2). Only 12 patients had optimized waist circumference according to IDF criteria; thus, it was not possible to perform multivariate analyses.
Likewise, models of linear regression were estimated to test the possible relationship between the 10-point increase on IES-2 and the variability of health outcomes (as a dependent variable). The 10-point increase on IES-2 was associated with a decrease of 0.62 kg/m² (95% CI − 1.18; −0.06 kg/m², p < 0.05) on BMI values and 1.90 cm (95% CI − 3.26; −0.54, p < 0.01) on waist circumference after adjusting for age, sex, psychotropic drug use, MES, and smoking (Model 1). Regarding the lipid profile, the 10-point increase on IES-2 was associated with a 23 mg/dL (95% CI − 38.27; -7.40 mg/dL, p < 0.01) reduction on serum triglycerides values after adjustment for age, sex, psychotropic drug use, MES, smoking, and BMI (Table 2in supplementary material).
Discussion
This cross-sectional study examined the possible association between intuitive eating and optimized health outcomes in patients with T2D. We identified three intuitive eating groups according to IES-2 by latent class analysis in this sample: patients with higher intuitive eating (Group 3), patients with nonemotional-oriented coping (Group 2), and those with lower intuitive eating (Group 1). Our findings indicate that patients with higher intuitive eating have higher chances of having optimized BMI and serum triglycerides values compared to patients with lower intuitive eating. Also, the 10-point increase on IES-2 was associated with a decrease of 0.62 kg/m² on BMI values, 1.90 cm on waist circumference, and 23 mg/dL on serum triglycerides values, after adjustment for confounders.
In our T2D sample, a higher intuitive eating group was associated with optimized BMI, and the 10-point increase on IES-2 was associated with a decrease of 0.62 kg/m² on BMI values. These findings corroborate the results of other cross-sectional studies with the overall population [12,13,14,15,16,17]. Moreover, participants with higher intuitive eating practices were less likely to report engaging in emotional and uncontrolled eating behavior. Possibly, emotional eating is correlated to BMI [41] and may occur concomitantly with uncontrolled eating, i.e., the tendency to lose control over eating when feeling hungry or when exposed to external cues, as a very palatable food [42], although they refer to independent constructs. These eating behaviors are somewhat opposed to intuitive eating, which is characterized by recognizing the physiological signs of hunger and fullness (satiety) to control eating. Due to cross-sectional design issues, it should raise the possibility of reverse causality. However, we cannot fail to consider that individuals with a health condition that alters the “natural” cues of hunger and fullness, such as overweight or obesity, may present altered hunger and satiety signals [43]. On the other hand, individuals with overweight or obesity are attempting to control their intake more than normal-weight individuals do. It is important to address the fact that the “Unconditional Permission to Eat” subscale had the lowest scores. Likewise, a recent prospective, non-controlled clinical trial with outpatient overweight women with chronic kidney disease (54.5% of patients had diabetes) observed no difference in this subscale when comparing less and more intuitive eaters [44]. The permission dimension reflects individuals’ willingness to eat when hungry (i.e., not try to stave off hunger) and refuse to label certain foods as forbidden [10] according to items such as “I try to avoid certain foods high in fat, carbohydrates, or calories” and “I have forbidden foods that I don’t allow myself to eat”. Moreover, the cognitive restraint subscale of the TFEQ-R21, which evaluates a similar inversely construct as the “Unconditional Permission to Eat” subscale and is characterized by the self-imposed limitation of food intake to control body weight [45], also showed no differences among the three intuitive eating groups. One possible explanation for this is the absence of a “one-size-fits-all” eating pattern for individuals with diabetes [3]. Health professionals may provide varied and sometimes extreme dietary advice, leading to fears associated with consuming certain foods. Unfortunately, T2D may be surrounded by confusion, controversy, and misinformation about food.
Higher intuitive eating levels were significantly associated with optimized triglycerides values, and the 10-point increase on IES-2 was associated with a decrease of 23 mg/dL in serum triglycerides values. To our knowledge, this is the first study to evaluate the association between intuitive eating and optimized health outcomes in T2D, hindering the comparison between our findings and other studies. However, this is consistent with the results observed by Bacon et al. (2002) in middle-aged women with obesity and Teas et al. (2022) in older adults [46, 47]. It is known that individuals with lower intuitive eating eat for reasons other than hunger, especially due to emotional situations, and may increase their intake of palatable foods with a high content of refined carbohydrates, free sugar, and unhealthy fats [48]. An increase in dietary energy from carbohydrates, especially from added sugar, is usually associated with an increase in fasting plasma triglycerides [49].
Regarding glycemic control, patients with higher intuitive eating and non-emotional oriented coping had lower HbA1c values than patients with lower intuitive eating, although in linear regression models, after adjusting for age, sex, psychotropic drug use, and smoking, the association could not be confirmed. Soares et al. (2020) observed that patients with HbA1c values within American Diabetes Association targets presented higher scores on IES-2, and this result was unlike ours, possibly due to differences between the proportion of patients with insulin use and with optimized HbA1c values, like the HbA1c criteria adopted [24].
Our study has strengths, as the inclusion of men in the sample and the information on eating behavior (IES-2 and TFEQ-R21) were collected by trained nutritionists using instruments with good psychometric properties for the sample. Although we should consider that it may have interfered with the assurance of responses due to social rules imposed by the profession. Furthermore, as no cut-off point was defined for IES-2 to classify individuals as less or more intuitive eaters, we used another strategy, namely latent class analysis. This is a statistical procedure used to identify qualitatively different subgroups within populations that often share certain outward characteristics. Nonetheless, some limitations in the study design should be mentioned. Firstly, the cross-sectional nature of the study does not allow for the demonstration of causality among variables. Also, the sample consisted of patients followed at primary or secondary care at a single hospital in Southern Brazil; therefore, these results should be replicated in different populations. Moreover, the majority of scales and questionnaire applications were conducted remotely (85.8%), which made it impossible to control environmental distractions during data collection. Also, a possible limitation of this study was the absence of food and alcohol consumption data, as individuals may cope with their emotions not only by increasing food (emotional eating) but also by consuming alcohol.
Regarding clinical practice, our study is interesting for better personalized interventions. From this perspective, emotional support and the development of skills to cope with emotional distress can be a great differential to promote sustainable changes in eating behavior and achieve a healthy body weight. However, the results regarding intuitive eating interventions and the improvement of health outcomes in obesity are scarce and controversial [46, 50]. However, a randomized clinical trial with a mindful eating approach based mainly on hunger and satiety cues showed that this treatment promoted a greater decrease in HbA1c values when compared with conventional treatments in T2D [51]. The effectiveness of this strategy needs to be tested in different populations in well-designed randomized clinical trials with an expressive sample size. Moreover, the associations between intuitive eating and optimized health outcomes considering dietary intake should be evaluated in different samples of patients with diabetes in longitudinal studies.
In conclusion, eating more intuitively was associated with optimized BMI prevalence and triglycerides values compared to eating less intuitively in this sample of outpatients with T2D. These findings have important theoretical and practical implications and highlight the relevance of developing strategies to promote intuitive eating in this population.
References
World Health Organization (2019) Classification of diabetes mellitus. https://apps.who.int/iris/handle/10665/325182. Accessed 03 January 2023
International Diabetes Federation (2021) IDF Diabetes Atlas: 10th edition. https://diabetesatlas.org/en/. Accessed 03 January 2023
American Diabetes Association (2023) Standards of Medical Care in Diabetes. Diab Care 46(1)
Nordmo M, Danielsen YS, Nordmo M (2020) The challenge of keeping it off, a descriptive systematic review of high-quality, follow-up studies of obesity treatments. Obes Rev 21(1):e12949. https://doi.org/10.1111/obr.12949
MacLean PS, Wing RR, Davidson T, Epstein L, Goodpaster B, Hall KD et al (2015) NIH working group report: innovative research to improve maintenance of weight loss. Obes 23(1):7–15. https://doi.org/10.1002/oby.20967
Perrin NE, Davies MJ, Robertson N, Snoek FJ, Khunti K (2017) The prevalence of diabetes-specific emotional distress in people with type 2 diabetes: a systematic review and meta-analysis. Diabet Med 34(11):1508–1520. https://doi.org/10.1111/dme.13448
Clifford D, Ozier A, Bundros J, Moore J, Kreiser A, Morris MN (2015) Impact of non-diet approaches on attitudes, behaviors, and health outcomes: A systematic review. J Nutr Educ Behav 47(2):143 – 55.e1. https://doi.org/10.1016/j.jneb.2014.12.002. PMID: 25754299
Fuentes Artiles R, Staub K, Aldakak L, Eppenberger P, Rühli F, Bender N (2019) Mindful eating and common diet programs lower body weight similarly: systematic review and meta-analysis. Obes Rev 20(11):1619–1627. https://doi.org/10.1111/obr.12918
Tribole T, Resch E (2012) Intuitive eating - A revolutionary program that works. St. Martin’s Griffin, New York
Tylka TL, Van Kroon AM (2013) The intuitive eating Scale-2: item refinement and psychometric evaluation with college women and men. J Couns Psychol 60(1):137–153. https://doi.org/10.1037/a0030893
da Silva WR, Neves AN, Ferreira L, Campos JA, Swami V (2020) A psychometric investigation of Brazilian Portuguese versions of the caregiver eating messages Scale and intuitive eating Scale-2. Eat Weight Disord 25(1):221–230. https://doi.org/10.1007/s40519-018-0557-3
Augustus-Horvath CL, Tylka TL (2011) The acceptance model of intuitive eating: a comparison of women in emerging adulthood, early adulthood, and middle adulthood. J Couns Psychol 58(1):110–125. https://doi.org/10.1037/a0022129
Madden CE, Leong SL, Gray A, Horwath CC (2012) Eating in response to hunger and satiety signals is related to BMI in a nationwide sample of 1601 mid-age New Zealand women. Public Health Nutr 15(12):2272–2279. https://doi.org/10.1017/S1368980012000882
Tylka TL, Calogero RM, Daníelsdóttir S (2015) Is intuitive eating the same as flexible dietary control? Their links to each other and well-being could provide an answer. Appetite 95:166–175. https://doi.org/10.1016/j.appet.2015.07.004
Camilleri GM, Méjean C, Bellisle F, Andreeva VA, Kesse-Guyot E, Hercberg S, Péneau S (2016) Intuitive eating is inversely associated with body weight status in the general population-based NutriNet-Santé study. Obes 24(5):1154–1161. https://doi.org/10.1002/oby.21440
Carrard I, Rothen S, Rodgers RF (2021) Body image concerns and intuitive eating in older women. Appetite 164:105275. https://doi.org/10.1016/j.appet.2021.105275
Braun TD, Unick JL, Abrantes AM, Dalrymple K, Conboy LA, Schifano E, Park CL, Lazar SW (2022) Intuitive eating buffers the link between internalized weight stigma and body mass index in stressed adults. Appetite 169:105810. https://doi.org/10.1016/j.appet.2021.105810
Tylka TL, Calogero RM, Daníelsdóttir S (2020) Intuitive eating is connected to self-reported weight stability in community women and men. Eat Disord 28(3):256–264. https://doi.org/10.1080/10640266.2019.1580126
Markey CH, Strodl E, Aimé A et al (2023) A survey of eating styles in eight countries: examining restrained, emotional, intuitive eating and their correlates. Br J Health Psychol 28(1):136–155. https://doi.org/10.1111/bjhp.12616
Christoph MJ, Hazzard VM, Järvelä-Reijonen E, Hooper L, Larson N, Neumark-Sztainer D (2021) Intuitive eating is associated with higher fruit and vegetable intake among adults. J Nutr Educ Behav 53(3):240–245. https://doi.org/10.1016/j.jneb.2020.11.015
Quansah DY, Gross J, Gilbert L, Helbling C, Horsch A, Puder JJ (2019) Intuitive eating is associated with weight and glucose control during pregnancy and in the early postpartum period in women with gestational diabetes mellitus (GDM): a clinical cohort study. Eat Behav 34:101304. https://doi.org/10.1016/j.eatbeh.2019.101304
Quansah DY, Gilbert L, Gross J, Horsch A, Puder JJ (2021) Intuitive eating is associated with improved health indicators at 1-year postpartum in women with gestational diabetes mellitus. J Health Psychol 26(8):1168–1184. https://doi.org/10.1177/1359105319869814
Quansah DY, Schenk S, Gilbert L, Arhab A, Gross J, Marques-Vidal PM et al (2022) Intuitive eating behavior, diet quality and metabolic health in the postpartum in women with gestational diabetes. Nutrients 14(20):4272. https://doi.org/10.3390/nu14204272
Soares FL, Ramos MH, Gramelisch M, Silva RP, Batista JS, Cattafesta M, Salaroli LB (2021) Intuitive eating is associated with glycemic control in type 2 diabetes. Eat Weight Disord 26(2):599–608. https://doi.org/10.1007/s40519-020-00894-8
Ramos MH, Silva JM, de Oliveira TA, Batista JS, Cattafesta M, Salaroli LB, Soares FL (2022) Intuitive eating and body appreciation in type 2 diabetes. J Health Psychol 27(2):255–267. https://doi.org/10.1177/1359105320950791
Basinger ED, Cameron SJ, Allen G (2023) Stigma, self-care, and intuitive eating in black americans with type 2 diabetes. J Racial Ethn Health Disparities doi. https://doi.org/10.1007/s40615-023-01772-6
Dean AG, Sullivan KM, Soe MM, OpenEpi Open Source Epidemiologic Statistics for Public Health. Version 3.01. www.OpenEpi.com. Accessed 19 December 2022
World Health Organization (2003) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus. World Health Organization, Geneva, Switzerland. Accessed 19 December 2022
Viana LC, Gross JL, Camargo JL, Zelmanovitz T, Rocha EP, Azevedo MJ (2012) Prediction of cardiovascular events, diabetic nephropathy, and mortality by albumin concentration in a spot urine sample in patients with type 2 diabetes. J Diabetes Complications 26(5):407–412. https://doi.org/10.1016/j.jdiacomp.2012.04.014
Das T, Takkar B, Sivaprasad S, Thanksphon T, Taylor H, Wiedemann P et al (2021) Recently updated global diabetic retinopathy screening guidelines: commonalities, differences, and future possibilities. Eye 35(10):2685–2698. https://doi.org/10.1038/s41433-021-01572-4
Alexopoulos AS, Yancy WS, Edelman D, Coffman CJ, Jeffreys AS, Maciejewski ML et al (2021) Clinical associations of an updated medication effect score for measuring diabetes treatment intensity. Chronic Illn 17(4):451–462. https://doi.org/10.1177/1742395319884096
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, AAPA/ABC/ACPM/AGS/APhA/ASH et al (2018) /ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension 71(6):1269–1324. https://doi.org/10.1161/HYP.0000000000000066
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18(6):499–502
World Health Organization (2006) Global database on body mass index. BMI classification. http://www.assessmentpsychology.com/icbmi.htm. Accessed January 03, 2023
Lipschitz DA (1994) Screening for nutritional status in the elderly. Prim Care 21(1):55–67
International Diabetes Federation (2020) Belgium: IDF. https://www.idf.org/about-diabetes. Accessed 19 December 2022
Associação Brasileira de Empresas de Pesquisa. Critério de Classificação Econômica Brasil. https://www.abep.org/criterio-brasil. Accessed 19 December 2022
Matsudo S, Araújo T, Matsudo V, Andrade D, Andrade E, Oliveira LC, Braggion G (2012) Questionário Internacional De Atividade física (IPAQ): estudo de validade e reprodutibilidade no brasil. Rev Bras Ativ Fís Saúde [Internet]. Available in: https://rbafs.org.br/RBAFS/article/view/931
International Physical Activity Questionnaire. https://sites.google.com/site/theipaq/scoring-protocol. Accessed 19 December 2022
Brown TA (2006) Confirmatory factor analysis for applied research. The Guilford, New York
de Medeiros AC, Yamamoto ME, Pedrosa LF, Hutz CS (2017) The Brazilian version of the three-factor eating questionnaire-R21: psychometric evaluation and scoring pattern. Eat Weight Disord 22(1):169–175. https://doi.org/10.1007/s40519-016-0256-x
Cappelleri JC, Bushmakin AG, Gerber RA, Leidy NK, Sexton CC, Lowe MR, Karlsson J (2009) Psychometric analysis of the three-factor eating Questionnaire-R21: results from a large diverse sample of obese and non-obese participants. Int J Obes 33(6):611–620. https://doi.org/10.1038/ijo.2009.74
Lean ME, Malkova D (2016) Altered gut and adipose tissue hormones in overweight and obese individuals: cause or consequence? Int J Obes 40(4):622–632. https://doi.org/10.1038/ijo.2015.220
Pereira RA, Alvarenga MD, de Andrade LS, Teixeira RR, Teixeira PC, da Silva WR, Cuppari L (2022) Effect of a nutritional behavioral intervention on intuitive eating in overweight women with chronic kidney disease. J Ren Nutr 33(2):289–297. https://doi.org/10.1053/j.jrn.2022.01.012
Herman CP, Mack D (1975) Restrained and unrestrained eating. J Pers 43(4):647–660. https://doi.org/10.1111/j.1467-6494.1975.tb00727.x
Bacon L, Keim NL, Van Loan MD, Derricote M, Gale B, Kazaks A, Stern JS (2002) Evaluating a ‘non-diet’ wellness intervention for improvement of metabolic fitness, psychological well-being and eating and activity behaviors. Int J Obes Relat Metab Disord 26(6):854–865. https://doi.org/10.1038/sj.ijo.0802012
Teas E, Kimiecik J, Ward RM, Timmerman K (2022) Intuitive eating and biomarkers related to cardiovascular disease in older adults. J Nutr Educ Behav 54(5):412–421. https://doi.org/10.1016/j.jneb.2022.01.010
Massicotte E, Deschênes SM, Jackson PL (2019) Food craving predicts the consumption of highly palatable food but not bland food. Eat Weight Disord 24(4):693–704. https://doi.org/10.1007/s40519-019-00706-8
Sacks FM, Lichtenstein AH, Wu JH, Appel LJ, Creager MA, Kris-Etherton PM et al (2017) Dietary fats and cardiovascular disease: a presidential advisory from the American Heart Association. Circulation 136(3):e1–e23. https://doi.org/10.1161/CIR.0000000000000510
Campos MB, Menezes IH, Peixoto MD, Schincaglia RM (2022) Intuitive eating in general aspects of eating behaviors in individuals with obesity: randomized clinical trial. Clin Nutr ESPEN 50:24–32. https://doi.org/10.1016/j.clnesp.2022.06.002
Miller CK, Kristeller JL, Headings A, Nagaraja H, Miser WF (2012) Comparative effectiveness of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: a pilot study. J Acad Nutr Diet 112(11):1835–1842. https://doi.org/10.1016/j.jand.2012.07.036
Acknowledgements
The authors would like to thank the patients who agreed to participate in the study.
Funding
This study was partly funded by the Research Incentive Fund (FIPE) of the Hospital de Clínicas de Porto Alegre; and by the Coordination for the Improvement of Higher Education Personnel - Brazil (CAPES) - Finance Code 001. OGK received a federal scholarship from CAPES.
Author information
Authors and Affiliations
Contributions
The authors’ contributions were as follows: OGK assisted in the design of the study and collected, analyzed, and interpreted the data and wrote the manuscript; VMM and AB collected data; and JCA designed and supervised the study, analyzed, and interpreted the data, and critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Research Ethics Committee of the Hospital de Clínicas de Porto Alegre, Brazil (2020 − 0654). All procedures were performed in accordance with the relevant guidelines and regulations.
Consent to participate
Written informed consent was provided by all participants prior to their inclusion in the study.
Consent for publication
The authors affirm that human research participants provided informed consent for the publication of the current study.
Conflict of interest
The authors declare no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Koller, O., Menezes, V., Busanello, A. et al. Association between intuitive eating and health outcomes in outpatients with type 2 diabetes: a cross-sectional study. Eur J Nutr 63, 1623–1634 (2024). https://doi.org/10.1007/s00394-024-03361-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-024-03361-7