Abstract
Purpose
This study aimed at quantifying and ranking the effects of different foods or food groups on weight loss.
Methods
We searched PubMed, Scopus, Cochrane Central Register of Controlled Trials, and Embase to April 2021. We included randomized trials evaluating the comparative effects of two or more food groups, or compared a food group against a control group (usual diet, no intervention) for weight loss in adults. We conducted random-effects network meta-analysis with Bayesian framework to estimate mean difference [MD] and 95% credible interval [CrI] of the effect of food groups on weight loss.
Results
152 RCTs with 9669 participants were eligible. Increased consumption of fish (MD − 0.85 kg, 95% CrI − 1.66, − 0.02; GRADE = low), whole grains (MD − 0.44 kg, 95% CrI − 0.88, 0.0; GRADE = very low), and nuts (MD − 0.37 kg, 95% CI − 0.72, − 0.01; GRADE = low) demonstrated trivial weight loss, well below minimal clinically important threshold (3.9 kg), when compared with the control group. Interventions with other food groups led to no weight loss when compared with either the control group or other food groups. The certainty of the evidence was rated low to very low with the point estimates for all comparisons less than 1 kg. None of the food groups showed an important reduction in body weight when restricted to studies conducted in participants with overweight or obesity.
Conclusions
Interventions with a single food or food group resulted in no or trivial weight loss, especially in individuals with overweight or obesity. Further trials on single foods or food groups for weight loss should be highly discouraged.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Worldwide, the obesity epidemic has continued to increase for three decades [1]. Adiposity has become a global public health concern and is accompanied by a large financial burden on the health care system [2]. People with obesity are at greater risk of cardiovascular disease [3], site-specific cancers [4], and premature death [3]. Individuals living with obesity may experience blame and shame, [5] and weight-related discrimination that can lead to loneliness and psychological distress [6, 7].
Obesity results from a complex interaction between a series of metabolic, genetic, behavioral and environmental factors [8, 9], leading to positive energy balance related to higher energy intake and lower levels of physical activity. Interventional strategies targeting dietary intake or physical activity are a core part of weight management programs [10]. There exist meta-analyses and network meta-analyses of randomized controlled trials (RCT) demonstrating the short-term comparative effectiveness of different structured dietary programs such as low carbohydrate versus low fat diets for weight loss [11,12,13].
In addition to dietary programs, there are 100 s of RCTs on single nutrients, natural health products, food and food categories. For instance, some foods or food groups such as walnuts and whole grains including rye and wheat kernels have satiating [14] and thermogenic [15] properties and thus, may have weight-reducing effects. Weight loss effects of other foods or food groups including dairy products (rich in calcium) [16], legumes (rich in dietary fibers) [17], and fruits and vegetables (rich in dietary fibers and phytochemicals) [18] have also been evaluated in previously published meta-analyses.
However, there are limited high-quality meta-analyses assessing the effectiveness of food or food categories for weight loss [16, 19,20,21,22,23], and there are no comparative network meta-analyses addressing these interventions for weight-loss. In addition, the quality of body of evidence, considering minimal clinically important difference (MCID) threshold, has rarely been used in the published systematic reviews addressing nutrition questions.
To elucidate whether increasing the consumption of a specific food or food group is an effective interventional strategy for weight loss, we performed a systematic review and network meta-analysis of RCTs to quantify and rank the effects of specific food groups on weight loss in adults.
Materials and methods
We followed instructions outlined in Cochrane Handbook for Systematic Reviews of Interventions [24] and the Grading of Recommendations Assessment, Development and Evaluation (GRADE) Handbook to conduct our systematic review [25]. We registered the protocol for our systematic review at Open Science Framework (registered form: osf.io/aex7c; registration https://doi.org/10.17605/OSF.IO/Q8VN4) [26].
Systematic search
We systematically searched PubMed, Scopus, Cochrane Central Register of Controlled Trials (CENTRAL), and Embase on January 31, 2021 from inception until January 31, 2021, and an updated search on April 31, 2021 to April 31, 2021. The systematic search was conducted at the same time in all databases. In consultation with a librarian, we developed and performed the literature search (SSB and AJ) and teams of two reviewers (MA and HS; MS and SM) independently and in duplicate screened titles and abstracts and full-text articles. Differences were resolved by discussion with a third reviewer (AJ) when necessary. We also screened the reference lists of all published meta-analyses of RCTs on the effect of foods or food groups on body weight. The complete search strategy used to find articles of original research for inclusion in the present systematic review is provided in Supplementary Table 1.
Eligibility criteria
Original controlled trials with the following criteria (Table 1) were considered eligible for inclusion: (1) randomized trials with either parallel or cross-over design conducted in adults (≥ 18 years); (2) trials with an intervention period of four weeks or longer; and (3) trials evaluating two or more foods or food groups including whole grains, refined grains, fruits, vegetables, fruits and vegetables combined, legumes, nuts, fish, red meat, white meat, processed meat, eggs, dairy, and sugar sweetened beverages; or compared one of these foods or food groups against placebo, no intervention or usual diet (control group). A recent meta-analysis of cohort studies indicated that higher intake of some food groups such as whole grains, nuts, and legumes was associated with a decreased risk of overweight/obesity [27]. In addition, evidence is lacking about weight reducing effects of some food groups such as eggs, red and processed meat, white meat, and fish. Therefore, we classified foods into 14 major food groups to provide a comprehensive picture of the effects of almost all foods consumed in a typical diet on body weight.
Exclusion criteria
We excluded (1) cross-over trials with a wash-out period shorter than 2 weeks, (2) trials conducted in patients with a history of cancer, pregnant women, children and adolescents, and (3) trials that implemented a structured dietary program (e.g., low fat [28] or low carbohydrate [29]) or dietary supplements (e.g. L carnitine, cayenne pepper).
Outcomes
Our main outcome was weight loss in kilograms (kg), while our secondary outcomes included health-related quality of life (HRQoL) and adverse events. Adverse events included any undesirable event reported in primary trials such as constipation, headache, muscle cramps, and diarrhea. We defined HRQoL as an individual’s assessment of well-being, including physical, mental, emotional and/or social health status [30, 31]. Measures for assessing different aspects of an individual’s HRQoL included generic measures and disease-specific measures.
Screening and data extraction
After the study selection process, two reviewers (AJ and SS-B) independently and in duplicate extracted the following characteristics from each trial: the last name of the first author, year of publication, study design (parallel or cross-over), sample size, mean age, baseline weight (mean and SD), % female, intervention duration, follow-up duration, description of intervention/control arms, the dosage of foods or food groups, energy restriction (yes, no; if yes, kcal restriction details), exercise and/or physical activity (yes, no; if yes, details of exercise modality and duration), behavioral support (yes, no; if yes, details of support provided) [32], potential adverse events following a dietary intervention, and mean and corresponding SD of change from baseline weight for each arm. Disagreements were resolved by consensus between the two authors.
Risk of bias (quality) assessment
Two authors (AJ and SS-B) independently assessed the risk of bias of the trials using guidance outlined in the Cochrane tool for risk of bias assessment [24].
Data synthesis and analysis
We carried out Bayesian random-effects pairwise meta-analyses for each comparison to inform direct estimates [33, 34]. We calculated mean differences (MDs) with corresponding 95% credible intervals (CrI) for weight loss. We calculated changes from baseline weight following intervention with each food or food group relative to the control group. If the mean values and SDs of changes were not available in text or in graphs, we calculated these values using data from measures before and after the intervention, based on the Cochrane Handbook guidance [24]. For trials that reported standard error instead of SD, the former was converted to SD [24]. If either SD or standard error were not reported in the trials, we used the average SDs obtained from other trials included in the corresponding analyses [35]. For trials that reported median data instead of mean data, we converted the former to mean data using standard methods [36, 37].
We conducted a random-effects network meta-analysis also using a Bayesian framework [33, 34]. We used three Markov-chains with 100 000 iterations after an initial burn-in of 10 000 and a thinning of 10. The convergence was assessed using trace plots and the Brooks-Gelman-Rubin statistic. We used node-splitting models to evaluate incoherence and generate the indirect estimates. We calculated ranking probabilities and calculated surface under the cumulative ranking curves (SUCRA). Both pairwise meta-analysis and network meta-analyses were performed under the gemtc package of R version 3.4.3 (RStudio, Boston, MA).
We considered the following three effect modifiers if they were implemented in parallel with food group’s intervention in primary trials: calorie restriction, physical activity, and behavioral support. Physical activity was defined as having explicit instructions for weekly physical activities performed under the supervision of investigators, or instructions to monitor physical activities using established tools (e.g. pedometer, time recorded exercising). Studies with behavioral support asked participants to attend at least two group or individual sessions per month for the first 3 months alongside increased consumption of food groups [32]. Using the U.S. Preventive Services Task Force (USPSTF) recommendations, we defined a high-intensity intervention as more than 1 person-to-person (individual or group) session per month for at least the first 3 months of the intervention, a moderate intensity intervention as a monthly intervention, and anything less frequent is a low-intensity intervention [32]. We also considered calorie restriction as one of our effect modifiers. Any instructions to calorie restrict or documented or anticipated decrement in usual calorie intake in participants included in primary RCTs was considered as calorie restriction.
To test the potential effect modification by calorie restriction, physical activity ***and behavioral support, we did a network meta-regression assuming a common coefficient across comparisons. Two pre-specified sensitivity analyses were also carried out by restricting the analyses to trials that were conducted exclusively in people with overweight or obesity (body mass index [BMI] ≥ 25), as well as trials rated to have a low risk of bias. We also conducted two post-hoc sensitivity analyses with trials wherein control group was usual diet/no intervention, as well as trials wherein weight loss was the primary outcome.
Publication bias
The potential for publication bias was assessed by evaluating the magnitude of asymmetry in the funnel plot by creating a comparison-adjusted funnel plot (Supplementary Fig. 1) [38].
Grading of the evidence
We rated the certainty of the evidence using the GRADE approach with two independent reviewers (AJ and SS-B). Any disagreements were resolved by consensus with a third reviewer (LG). We rated the certainty of the evidence as high, moderate, low, or very low for our direct, indirect, and network evidence for each outcome, respectively.
To start, we rated the certainty of the evidence for each direct comparison according to standard GRADE guidance [39]. We then rated the evidence for indirect estimates based on the dominant first-order loop and evidence of intransitivity [40]. Subsequently, we rated the certainty of network evidence based on the direct or indirect evidence that was the predominate comparison and then considered rating down the certainty in the network estimate imprecision and for incoherence between the indirect and direct estimates [40]. We used the GRADE guidelines to interpret the size of the effect and accordingly, point estimates less than minimal clinically important difference (MCID) threshold was considered as trivial [41, 42]. The MCID for weight loss was considered as 5% weight loss [43], equal to 3.9 kg in the present meta-analysis.
Summary of most to least effective treatments
To present our overall results for our foods and food groups network meta-analysis, we used a new GRADE approach to summarize the findings, ranking food groups from the most to the least effective, considering the effect estimates obtained from the meta-analysis and the certainty of evidence [11, 44]. According to this approach, dietary interventions were classified into the following three groups. First, the control group and food groups that did not differ from the reference (that is, credible interval crossed mean difference = 0), which we referred to as “among the least effective”. Second, food groups that were superior to the reference, but not superior to any other group superior to the reference (which we called category 1 and described as “inferior to the most effective, but superior to the least effective”). Third, food groups that proved superior to at least one category 1 group (which we called “among the most effective”). Finally, the aforementioned three categories were classified into two groups as follows: food groups with moderate or high certainty evidence relative to the placebo, and those with low or very low certainty evidence relative to the placebo [11].
Results
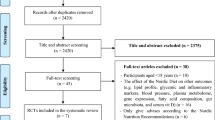
Literature search and study selection process
As described in Fig. 1, the initial database and reference lists search identified 45,363 records. We excluded 9121 duplicates and 35,778 irrelevant articles based on screening of the title and abstract. These records were irrelevant to our aims and did not meet our inclusion criteria. Finally, we reviewed 464 full-texts in detail for eligibility. Overall, 152 articles met our inclusion criteria and were considered eligible for our network meta-analysis. The list of studies excluded via full-text assessing with reasons for exclusions is provided in Supplementary Table 2.
Characteristics of primary trials included in the network meta-analysis
Supplementary Table 3 summarizes the general characteristics of 152 primary trials included in this network meta-analysis. Included trials were published from 1983 to 2020. Overall, 109 trials (72%) had parallel design and 43 trials (28%) had a cross-over design. Follow-up duration ranged between 4 and 72 weeks. The intervention period of 114 trials (75%) lasted between 4 to ≤ 12 weeks, 27 trials (18%) between 12 and ≤ 24 weeks, and 11 trials (7%) > 24 weeks. Of 152 trials, 62 trials (41%) were conducted exclusively in adults with overweight and obesity (body mass index ≥ 25 kg/m2) and considered weight loss as a primary outcome or one of the primary outcomes, while the other trials were conducted in a mixed population (normal weight, overweight, obese often with multiple cardiovascular risk factors). Forty-three trials (28%) were conducted in women, four in men, and the others in either sex. Fifty-one trials (34%) implemented a calorie-restricted diet alongside dietary intervention, 26 trials (17%) implemented behavioral support, and 17 trials (11%) a physical activity program. Sixty-one trials (40%) considered weight loss as a primary outcome or one of their primary outcomes, and 47 trials (31%) used usual diet/no intervention as control group. Of the trials, 63 (41%) were rated to have a low risk of bias (Supplementary Table 4).
Effects of food groups on body weight
The network diagram presenting direct comparisons between food groups is indicated in Fig. 2. Included trials performed a broad range of comparisons between food groups. The most common comparisons between food groups were between whole grains and refined grains (n = 28) and nuts and refined grains (n = 12).
Network plot of all included trials for major food groups. The size of the nodes is proportional to the total number of participants allocated to each food group, and the thickness of the lines is proportional to the number of trials evaluating each direct comparison. Numbers are the number of trials evaluating each direct comparison. SSB, sugar-sweetened beverages
Comparative effects of different food groups on body weight are presented in Table 2. According to the results, increased fish intake may lead to trivial weight loss when compared with the control group (MD − 0.84, 95% CrI − 1.66, -0.02; GRADE = low certainty). Whole grains (MD − 0.44 kg, 95% CrI − 0.88, 0.0; GRADE = very low certainty) and nuts (MD − 0.37, 95% CrI − 0.72, − 0.01; GRADE = low certainty) may lead to trivial weight loss when compared with the control group. Increasing the consumption of other food groups also led no difference in weight loss either when compared with the control group or when compared with other food groups (Table 2). Fish was ranked to have the highest SUCRA value (86%), followed by whole grains (67%), vegetables (64%), and nuts (60%) (Table 3). Detailed direct, indirect, and network estimates for the effects of food groups on body weight are presented in Supplementary Table 5, and the percentage contribution of direct and indirect estimates to the network estimates are depicted in Supplementary Table 6.
Sensitivity and subgroup analyses
We did two sensitivity analyses by restricting the analyses to studies with a low risk of bias (Supplementary Table 7) and studies conducted in participants who were overweight and/or obese (Supplementary Table 8). The trivial impact of fish, whole grains, and nuts was no longer apparent for weight loss in studies with low risk of bias, as well as in participants with overweight and obesity. There was trivial weight loss following increased consumption of other food groups in sensitivity analyses. We also performed two post-hoc sensitivity analyses by restricting the analysis to trials wherein weight loss was a primary outcome (n = 61) and to trials with usual diet or no intervention as the control arm (n = 47). No significant weight loss was seen in the analysis of trials with weight loss as a primary outcome (Supplementary Table 9), whilst the same findings with the main analysis were seen in the analysis of trials with usual diet or no intervention as control group (Supplementary Table 10).
To determine potential effect modification by calorie restriction, physical activity, and behavioral support, we did network meta-regression analyses. The analyses illustrated that none of the regression factors including calorie restriction (β-coefficient = 0.08, 95% CI − 0.43, 0.58), behavioral support (β-coefficient = − 0.28, 95% CI − 0.97, 0.41) and physical activity (β-coefficient = 0.37, 95% CI − 0.34, 1.09) had statistically significant effects. The effects of three effect modifiers including calorie restriction, physical activity, and behavioral support on the results are reported in Supplementary Tables 11–13, respectively. The results were the same with the main analyses, wherein fish, whole grains and nuts showed trivial or no impact for weight loss when compared with the control group, with the point estimates smaller than 1 kg. Other food groups showed no promise for weight loss.
Grading the evidence and summary of more and less preferred treatments
The certainty of the evidence for direct and indirect estimates is presented in Supplementary Table 14 and Supplementary Table 15, respectively. The certainty of the evidence for the network estimates was rated moderate for the comparison between whole grains vs legumes and fruits vs control group. The certainty of the evidence was rated low to very low for all other food groups (Supplementary Table 16). The magnitude of weight loss for all comparisons was trivial (< 1 kg), not meeting our MCID for weight loss (5% of baseline weight, equal to 3.9 kg) [45, 46].
Based on GRADE methods for ranking foods and food groups from the most to the least effective, considering the effect estimates obtained from the meta-analysis and the certainty of evidence, we found fish was the most effective food group for weight loss followed by nuts, vegetables, and whole grains, but again these interventions had little to no effect overall when considering the magnitude of effect and the certainty of the effect estimate. Again, all point estimates were smaller than 1 kg and based on low to very low certainty evidence (Table 4).
Health-related quality of life
Five trials assessed and reported the effects of fat-free milk, eggs, pistachios, walnuts, and strawberries on aspects of health-related quality of life. No significant or clinically important effects on quality of life were reported (Supplementary Table 17).
Adverse events
Of the trials, 35 trials evaluated and recorded adverse events following dietary interventions. Only one serious adverse event requiring hospitalization (atrial fibrillation) following increased consumption of mixed nuts was reported [47]. The event was determined to be unrelated to dietary intervention. Otherwise, adverse events were mild to somewhat moderate, consisting of gastrointestinal discomfort, abdominal pain, constipation and diarrhea, and were related to increasing the consumption of whole grains, fruits, legumes, and dairy (Supplementary Table 18).
Discussion
The present systematic review and network meta-analysis of RCTs is the first to assess and rank the comparative effects of different foods or food groups on body weight in adults with and without overweight and/or obesity. According to our findings, obtained from 152 trials, increasing the consumption of fish, nuts, and whole grains resulted in trivial weight loss in adults, with the point estimates smaller than 1 kg and with the certainty of evidence being rated low to very low. Interventions with other foods or food groups showed even less promise for weight loss when compared with either the control group or other food groups. Surprising, perhaps subject to the limitations of a small combined sample size (n = 288 participants) and short follow-up duration, among 6 RCTs we found little or no effect on body weight following dietary interventions comparing sugar-sweetened beverages with dairy (MD 1.10, kg, 95% CrI − 0.65, 2.82), fruits (0.03 kg, 95% CrI − 1.83, 1.90), or usual diet (MD 0.15 kg, 95% CrI − 1.67, 1.37).
We did two sensitivity analyses by restricting the analyses to studies with a low risk of bias, as well as trials including only individuals with overweight or obesity. Fish, whole grains and nuts or other foods or food groups were not effective for weight loss in trials with a low risk of bias, or in trials (n = 62) restricted to participants with overweight or obesity. We also performed network meta-regression to test for potential effect modification by calorie restriction, physical activity, and behavioral support. None of the regression factors had significant effects, and the estimates of effect remained largely unchanged.
To our knowledge, there has been no systematic review on the effects of other foods or food groups such as refined grains, red meat, egg, fruits, vegetables, fish, and sugary sweetened beverages on weight loss. In addition, potential weigh loss effects of food groups relative to every other food group have not been evaluated using network meta-analysis methods. Overall, our results show a trivial impact for 3 of 14 foods or food groups. Future studies of foods and food groups for weight-loss should be discouraged so as to avoid misleading participants and to mitigate the use of resources on wasteful research questions.
With respect to other reviews, two published meta-analyses of RCTs suggested that increasing the consumption of whole grain products can slightly reduce body weight in adults [21, 48]. However, another recent meta-analysis indicated that increasing the consumption of whole grains did not affect body weight in adults [22]. Our findings consistently indicated that whole grain intake led to a trivial reduction in body weight. Increased consumption of nuts has also been shown to have no or trivial effects on anthropometric measures in adults [20, 48,49,50,51,52]. Similarly, five published meta-analyses of randomised trials suggested that dairy consumption in the absence of calorie restriction had no significant effects on body weight in adults [16, 19, 53,54,55].
Our paper has a number of strengths. First, we included a large number of randomised trials on foods and food groups and we analysed the trials according to a predefined approach established based on our publicly available study protocol [26]. Second, we applied a novel statistical approach to determine and rank the effects of different foods and food groups on weight loss in adults. This method allowed for the first time, the quantification of the comparative effects of foods and food groups. Third, we rated the certainty of evidence using the emerging GRADE approach [56, 57] to rank foods and food groups from the most to the least effective, a method that combines SUCRA rankings with GRADE certainty of evidence as well as the magnitude of the effects to optimally classify the comparative effectiveness of interventions. Fourth, of 152 trials, 62 trials (41%) were conducted exclusively in overweight and obese participants and considered weight loss as a primary outcome or one of the primary outcomes. A sensitivity analysis restricting to participants with overweight and obesity indicated no significant effect of foods or food groups on weight loss which confirmed the main findings. Finally, we evaluated the effects of food or food groups on HRQoL and recorded adverse events following dietary interventions, indicating that dietary interventions with food groups had no significant effects on HRQoL. There is only one serious adverse event unrelated to study interventions. Otherwise, adverse events were mild to somewhat moderate.
Our network meta-analysis is also accompanied by some limitations. First, the certainty of the evidence for almost all network estimates was rated as low to very low because of the serious risk of bias, imprecision, and inconsistency. Second, the majority of trials are short-term with 114 trials (75%) lasting between 4 and ≤ 12 weeks, while 11 trials (7%) lasted longer than 24 weeks and we are, therefore. unable to determine the long-term effects of food groups on weight loss. Third, although we searched the literature, we did not find any RCTs that evaluated the effects of processed and white meats on weight loss. Finally, while the use of an MCID estimate to interpret our weight-loss results was an overall strength, the population among our 152 RCTs was mixed (normal weight, overweight and obese, most with multiple cardiovascular risk factors). Of 152 trials, 62 trials were conducted in strictly overweight and/or obese participants (for our MCID based on 5% of the average baseline weight = 4.36 kg), while the other 90 trials were conducted in mixed populations (5% of the average baseline weight = 3.6 kg). We used 5% of the average baseline weight among all eligible trials (3.9 kg) as MCID to rate for imprecision. The effect size did not surpass 1 kg in either the overweight/obese participants or in our main analysis, with the overall results showing trivial effects when considering our lowest MCID estimate of 3.6 kg.
Clinical and public health implications
Currently, important weight loss is defined as 5% baseline weight [58, 59], with some evidence suggesting that 3 to 5% loss can exert significant improvement in obesity-related cardiometabolic abnormalities such as blood pressure, particularly in those that are obese [60]. However, the greatest degree of weight loss observed in our network meta-analysis was − 0.85 kg (~ 1% of baseline weight) following increased consumption of with fish, which was far less than the MCID for weight loss in those with and without overweight issues. Still further, weight loss associated with increased consumption of whole grains and nuts was even smaller at 0.5 kg (~ 0.65% of baseline weight). Our findings indicated that increasing the consumption of a specific food or food group, when compared with either usual diet or other food groups, had trivial effects on body weight.
Conclusions and future research
The present network meta-analysis of 152 randomised trials indicated that increased consumption of a single food or food group exerted no or trivial effects on weight loss in adults, with the certainty of evidence being rated moderate to very low. Further trials on single foods or food groups for weight loss should be discouraged, particularly if there are no important effects on other cardiometabolic risk factors. Overall, our results show a trivial impact for 3 of 14 foods or food groups. Future studies of foods and food groups for weight-loss should be discouraged so as to avoid misleading participants and to mitigate the use of resources on wasteful research questions.
Availability of data and material
All data indicated and analyzed for this study are available by request to the corresponding author.
Abbreviations
- BMI:
-
Body mass index
- GRADE:
-
Grading of recommendations assessment, development and evaluation
- HRQoL:
-
Health-related quality of life
- RCT:
-
Randomized controlled trials
References:
Abarca-Gómez L, Abdeen ZA, Hamid ZA, Abu-Rmeileh NM, Acosta-Cazares B, Acuin C, Adams RJ, Aekplakorn W, Afsana K, Aguilar-Salinas CA (2017) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128· 9 million children, adolescents, and adults. The lancet 390:2627–2642
Tremmel M, Gerdtham U-G, Nilsson PM, Saha S (2017) Economic burden of obesity: a systematic literature review. Int J Environ Res Public Health 14:435
Jayedi A, Soltani S, Zargar MS, Khan TA, Shab-Bidar S (2020) Central fatness and risk of all cause mortality: systematic review and dose-response meta-analysis of 72 prospective cohort studies. BMJ 370
Kyrgiou M, Kalliala I, Markozannes G, Gunter MJ, Paraskevaidis E, Gabra H, Martin-Hirsch P, Tsilidis KK (2017) Adiposity and cancer at major anatomical sites: umbrella review of the literature. BMJ 356
Kirk SF, Price SL, Penney TL, Rehman L, Lyons RF, Piccinini-Vallis H, Vallis TM, Curran J, Aston M (2014) Blame, shame, and lack of support: a multilevel study on obesity management. Qual Health Res 24:790–800
Hatzenbuehler ML, Keyes KM, Hasin DS (2009) Associations between perceived weight discrimination and the prevalence of psychiatric disorders in the general population. Obesity 17:2033–2039
Lewis S, Thomas SL, Blood RW, Castle DJ, Hyde J, Komesaroff PA (2011) How do obese individuals perceive and respond to the different types of obesity stigma that they encounter in their daily lives? A qualitative study. Soc Sci Med 73:1349–1356
Garvey WT, Mechanick JI (2020) Proposal for a scientifically correct and medically actionable disease classification system (ICD) for obesity. Obesity 28:484–492
Mechanick JI, Hurley DL, Garvey WT (2017) Adiposity-based chronic disease as a new diagnostic term: the American Association of Clinical Endocrinologists and American College of Endocrinology position statement. Endocr Pract 23:372–378
Wharton S, Lau DC, Vallis M, Sharma AM, Biertho L, Campbell-Scherer D, Adamo K, Alberga A, Bell R, Boulé N (2020) Obesity in adults: a clinical practice guideline. CMAJ 192:E875–E891
Ge L, Sadeghirad B, Ball GD, da Costa BR, Hitchcock CL, Svendrovski A, Kiflen R, Quadri K, Kwon HY, Karamouzian M (2020) Comparison of dietary macronutrient patterns of 14 popular named dietary programmes for weight and cardiovascular risk factor reduction in adults: systematic review and network meta-analysis of randomised trials. BMJ 369
Johnston BC, Kanters S, Bandayrel K, Wu P, Naji F, Siemieniuk RA, Ball GD, Busse JW, Thorlund K, Guyatt G (2014) Comparison of weight loss among named diet programs in overweight and obese adults: a meta-analysis. JAMA 312:923–933
Tobias DK, Chen M, Manson JE, Ludwig DS, Willett W, Hu FB (2015) Effect of low-fat diet interventions versus other diet interventions on long-term weight change in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 3:968–979
Sanders LM, Zhu Y, Wilcox ML, Koecher K, Maki KC (2021) Effects of whole grain intake, compared with refined grain, on appetite and energy intake: a systematic review and meta-analysis. Adv Nutr
Casas-Agustench P, López-Uriarte P, Bulló M, Ros E, Gómez-Flores A, Salas-Salvadó J (2009) Acute effects of three high-fat meals with different fat saturations on energy expenditure, substrate oxidation and satiety. Clin Nutr 28:39–45
Abargouei AS, Janghorbani M, Salehi-Marzijarani M, Esmaillzadeh A (2012) Effect of dairy consumption on weight and body composition in adults: a systematic review and meta-analysis of randomized controlled clinical trials. Int J Obes 36:1485–1493
Kim SJ, De Souza RJ, Choo VL, Ha V, Cozma AI, Chiavaroli L, Mirrahimi A, Blanco Mejia S, Di Buono M, Bernstein AM (2016) Effects of dietary pulse consumption on body weight: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr 103:1213–1223
Mytton OT, Nnoaham K, Eyles H, Scarborough P, Ni Mhurchu C (2014) Systematic review and meta-analysis of the effect of increased vegetable and fruit consumption on body weight and energy intake. BMC Public Health 14:1–11
Chen M, Pan A, Malik VS, Hu FB (2012) Effects of dairy intake on body weight and fat: a meta-analysis of randomized controlled trials. Am J Clin Nutr 96:735–747
Flores-Mateo G, Rojas-Rueda D, Basora J, Ros E, Salas-Salvadó J (2013) Nut intake and adiposity: meta-analysis of clinical trials. Am J Clin Nutr 97:1346–1355
Pol K, Christensen R, Bartels EM, Raben A, Tetens I, Kristensen M (2013) Whole grain and body weight changes in apparently healthy adults: a systematic review and meta-analysis of randomized controlled studies. Am J Clin Nutr 98:872–884
Sadeghi O, Sadeghian M, Rahmani S, Maleki V, Larijani B, Esmaillzadeh A (2020) Whole-grain consumption does not affect obesity measures: an updated systematic review and meta-analysis of randomized clinical trials. Adv Nutr 11:280–292
Akhlaghi M, Zare M, Nouripour F (2017) Effect of soy and soy isoflavones on obesity-related anthropometric measures: a systematic review and meta-analysis of randomized controlled clinical trials. Adv Nutr 8:705–717
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (2019) Cochrane handbook for systematic reviews of interventions. John Wiley & Sons
Schunemann H (2008) GRADE handbook for grading quality of evidence and strength of recommendation. Version 3.2. https://gdt.gradepro.org/app/handbook/handbook.html
Ahmad Jayedi LG, Bradly J, Morteza A, Maryam S, Saba M, Hossein S, Parivash G, Sakineh S-B (2020) Food groups and body weight: a protocol for a systematic review and network meta-analysis of randomized trials. OSF June 4. https://doi.org/10.17605/OSF.IO/Q8VN4
Schlesinger S, Neuenschwander M, Schwedhelm C, Hoffmann G, Bechthold A, Boeing H, Schwingshackl L (2019) Food groups and risk of overweight, obesity, and weight gain: a systematic review and dose-response meta-analysis of prospective studies. Adv Nutr 10:205–218
Identification EPot, Overweight To, Adults Oi, Heart N, Lung, Institute B, Diabetes NIo, Diseases K (1998) Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. vol 98. National Institutes of Health, National Heart, Lung, and Blood Institute
Feinman RD, Pogozelski WK, Astrup A, Bernstein RK, Fine EJ, Westman EC, Accurso A, Frassetto L, Gower BA, McFarlane SI (2015) Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base. Nutrition 31:1–13
Group W (1998) Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med 28:551–558
Sullivan M, Sullivan L, Kral J (1987) Quality of life assessment in obesity: physical, psychological, and social function. Gastroenterol Clin North Am 16:433–442
Force UPST (2003) Screening for obesity in adults: recommendations and rationale. Ann Intern Med 139:930
Ades A, Sculpher M, Sutton A, Abrams K, Cooper N, Welton N, Lu G (2006) Bayesian methods for evidence synthesis in cost-effectiveness analysis. Pharmacoeconomics 24:1–19
Lumley T (2002) Network meta-analysis for indirect treatment comparisons. Stat Med 21:2313–2324
Furukawa TA, Barbui C, Cipriani A, Brambilla P, Watanabe N (2006) Imputing missing standard deviations in meta-analyses can provide accurate results. J Clin Epidemiol 59:7–10
Luo D, Wan X, Liu J, Tong T (2018) Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res 27:1785–1805
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:1–13
Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G (2013) Graphical tools for network meta-analysis in STATA. PLoS One 8:e76654
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336:924–926
Brignardello-Petersen R, Bonner A, Alexander PE, Siemieniuk RA, Furukawa TA, Rochwerg B, Hazlewood GS, Alhazzani W, Mustafa RA, Murad MH (2018) Advances in the GRADE approach to rate the certainty in estimates from a network meta-analysis. J Clin Epidemiol 93:36–44
Santesso N, Glenton C, Dahm P, Garner P, Akl EA, Alper B, Brignardello-Petersen R, Carrasco-Labra A, De Beer H, Hultcrantz M (2020) GRADE guidelines 26: informative statements to communicate the findings of systematic reviews of interventions. J Clin Epidemiol 119:126–135
Schünemann H, Brożek J, Guyatt G, Oxman A (2013) GRADE handbook for grading quality of evidence and strength of recommendations [Internet]. The grade Working group
Shi Q, Wang Y, Hao Q, Vandvik PO, Guyatt G, Li J, Chen Z, Xu S, Shen Y, Ge L (2021) Pharmacotherapy for adults with overweight and obesity: a systematic review and network meta-analysis of randomised controlled trials. The Lancet
Florez ID, Veroniki A-A, Al Khalifah R, Yepes-Nunez JJ, Sierra JM, Vernooij RW, Acosta-Reyes J, Granados CM, Perez-Gaxiola G, Cuello-Garcia C (2018) Comparative effectiveness and safety of interventions for acute diarrhea and gastroenteritis in children: a systematic review and network meta-analysis. PloS One 13
Food U, Administration D (2009) Centre for drug evaluation and research: guidance for industry. Bioanal Method Valid. 2001.
Heymsfield SB, Wadden TA (2017) Mechanisms, pathophysiology, and management of obesity. N Engl J Med 376:254–266
Jenkins DJ, Kendall CW, Lamarche B, Banach MS, Srichaikul K, Vidgen E, Mitchell S, Parker T, Nishi S, Bashyam B (2018) Nuts as a replacement for carbohydrates in the diabetic diet: a reanalysis of a randomised controlled trial. Diabetologia 61:1734–1747
Wang W, Li J, Chen X, Yu M, Pan Q, Guo L (2020) Whole grain food diet slightly reduces cardiovascular risks in obese/overweight adults: a systematic review and meta-analysis. BMC Cardiovasc Disord 20:1–11
Asbaghi O, Hadi A, Campbell MS, Venkatakrishnan K, Ghaedi E (2020) Effects of pistachios on anthropometric indices, inflammatory markers, endothelial function, and blood pressure in adults: a systematic review and meta-analysis of randomized controlled trials. Br J Nutr:1–27
Del Gobbo LC, Falk MC, Feldman R, Lewis K, Mozaffarian D (2015) Effects of tree nuts on blood lipids, apolipoproteins, and blood pressure: systematic review, meta-analysis, and dose-response of 61 controlled intervention trials. Am J Clin Nutr 102:1347–1356
Eslampour E, Moodi V, Asbaghi O, Ghaedi E, Shirinbakhshmasoleh M, Hadi A, Miraghajani M (2020) The effect of almond intake on anthropometric indices: a systematic review and meta-analysis. Food Funct 11:7340–7355
Fang Z, Dang M, Zhang W, Kord-Varkaneh H, Nazary-Vannani A, Santos HO, Tan SC, Clark CC, Zanghelini F, do Nascimento IJB (2020) Effects of walnut intake on anthropometric characteristics: a systematic review and dose-response meta-analysis of randomized controlled trials. Complement Ther Med:102395
Geng T, Qi L, Huang T (2018) Effects of dairy products consumption on body weight and body composition among adults: an updated meta-analysis of 37 randomized control trials. Mol Nutr Food Res 62:1700410
Schwingshackl L, Hoffmann G, Schwedhelm C, Kalle-Uhlmann T, Missbach B, Knüppel S, Boeing H (2016) Consumption of dairy products in relation to changes in anthropometric variables in adult populations: a systematic review and meta-analysis of cohort studies. PLoS One 11:e0157461
Stonehouse W, Wycherley T, Luscombe-Marsh N, Taylor P, Brinkworth G, Riley M (2016) Dairy intake enhances body weight and composition changes during energy restriction in 18–50-year-old adults—a meta-analysis of randomized controlled trials. Nutrients 8:394
Brignardello-Petersen R, Florez ID, Izcovich A, Santesso N, Hazlewood G, Alhazanni W, Yepes-Nuñez JJ, Tomlinson G, Schünemann HJ, Guyatt GH (2020) GRADE approach to drawing conclusions from a network meta-analysis using a minimally contextualised framework. BMJ 371
Brignardello-Petersen R, Izcovich A, Rochwerg B, Florez ID, Hazlewood G, Alhazanni W, Yepes-Nuñez J, Santesso N, Guyatt GH, Schünemann HJ (2020) GRADE approach to drawing conclusions from a network meta-analysis using a partially contextualised framework. BMJ 371
Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, Hu FB, Hubbard VS, Jakicic JM, Kushner RF (2014) 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol 63:2985–3023
Lau DC, Douketis JD, Morrison KM, Hramiak IM, Sharma AM, Ur E (2007) 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary]. CMAJ 176:S1–S13
Group LAR (2014) Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity 22:5–13
Funding
The authors reported no funding received for this study. BCJ reports receiving a grant from Texas A&M AgriLife Research to fund investigator-initiated research related to saturated and polyunsaturated fats. The grant was from Texas A&M AgriLife institutional funds from interest and investment earnings, not a sponsoring organization, industry, or company. In 2015 (outside ICJME 36 month disclosure period), Dr. Johnston received funding from the International Life Sciences Institute (North America) to assess the methodological quality of nutrition guidelines using internationally accepted GRADE and AGREE guideline standards for a study titled “The Scientific Basis of Guideline Recommendations on Sugar Intake: A Systematic Review.”
Author information
Authors and Affiliations
Contributions
AJ, BCJ, LG, and SS-B conceived and designed the study; AJ and SS-B conducted systematic search; “MA and HS” and “MS and SM” screened articles and selected eligible articles; AJ and SS-B extracted information from eligible studies; LG performed analysis; AJ and SS-B performed quality assessment; LG, BCJ and SS-B critically revised the manuscript and contributed to the interpretation of the results. All authors contributed to write, review or revise the paper. SS-B and BCJ are the guarantors. All authors have read and approved the final manuscript. All authors had full access to all the data and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding authors
Ethics declarations
Conflict of interest
The authors conducted this study independently without involvement of the funder. Other authors: No competing interest.
Registration
Open Science Framework (registered form: osf.io/aex7c; registration https://doi.org/10.17605/OSF.IO/Q8VN4).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jayedi, A., Ge, L., Johnston, B.C. et al. Comparative effectiveness of single foods and food groups on body weight: a systematic review and network meta-analysis of 152 randomized controlled trials. Eur J Nutr 62, 1153–1164 (2023). https://doi.org/10.1007/s00394-022-03046-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-022-03046-z