Abstract
Purpose
Gastroesophageal reflux disease (GERD) is a widely prevalent condition. High consumption of dairy foods and dietary fat are associated with worse GERD symptoms. However, existing data are inconsistent and mostly based on observational studies. The purpose of this exploratory analysis of a randomized controlled trial was to investigate the impact of low-fat and full-fat dairy food consumption on GERD symptoms.
Methods
Seventy-two participants with metabolic syndrome completed a 4-week wash-in diet during which dairy intake was limited to three servings of nonfat milk per week. Participants were then randomized to either continue the limited dairy diet or switch to a diet containing 3.3 servings per day of either low-fat or full-fat milk, yogurt and cheese for 12 weeks. Here, we report intervention effects on the frequency of acid reflux, and the frequency and severity of heartburn, exploratory endpoints assessed by a questionnaire administered before and after the 12-week intervention.
Results
In the per-protocol analysis (n = 63), there was no differential intervention effect on a cumulative heartburn score (p = 0.443 for the time by diet interaction in the overall repeated measures analysis of variance). Similarly, the intervention groups did not differentially affect the odds of experiencing acid regurgitation (p = 0.651). The intent-to-treat analyses (n = 72) yielded similar results.
Conclusion
Our exploratory analyses suggest that, in men and women with the metabolic syndrome, increasing the consumption of either low-fat or full-fat dairy foods to at least three servings per day does not affect common symptoms of GERD, heartburn and acid regurgitation compared to a diet limited in dairy.
Clinical trial registration
ClinicalTrials.gov Identifier: NCT02663544, registered on January 26, 2016.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastroesophageal reflux disease (GERD) is common, with a prevalence of 8.6% in Western Europe, 12.6% in Eastern Europe, and 12.3% in North America [1]. Per the Montreal definition, GERD is the mild presentation of heartburn (HB) and acid regurgitation (AR) at least twice weekly, or moderate-to-severe presentation at least once weekly [2]. The pathogenesis of GERD is multifactorial: contributing factors include decreased lower esophageal sphincter (LES) pressure, higher frequency of transient LES relaxations (TLESRs), and structural changes at the gastroesophageal junction [3, 4]. Patients with GERD suffer from impaired quality of life due to reduced functioning and sleep, and are at increased risk for developing functional bowel diseases [5]. It has been estimated that the average medical cost for a patient with GERD is double that of a healthy individual, leading to annual economic costs in the United States alone of ~ $24 billion [5].
Medical treatment includes the use of antacids, proton pump inhibitors, and histamine 2-receptor antagonists [6]. Discontinuation of treatment often results in relapse of symptoms, because these drugs do not reverse the pathogenesis of GERD [7]. Therefore, lifestyle and dietary modifications are currently regarded as the first line of therapy. Lifestyle factors including obesity, smoking, and strenuous physical activity; dietary factors like large meals and high fat intake; and specific foods such as chocolate, coffee, and spicy foods have all been identified as potential risk factors for the development and progression of GERD [5, 7, 8]. Medical advice recommends patients with GERD target these lifestyle and dietary factors. However, most of these recommendations are based on limited evidence from observational studies [7], highlighting the need for stronger evidence on how specific dietary factors influence GERD symptoms.
Dairy is another dietary factor that a limited number of mostly observational studies has linked to GERD. Ndebia et al. [9] found that milk and milk products are risk factors for acid regurgitation. Caselli et al. [10] proposed food intolerance as a potential pathogenic pathway to explain milk as a risk factor for GERD, based on their pilot study wherein individuals with a positive leukocytotoxic test reaction to dairy foods improved their GERD symptoms by avoiding dairy. On the other hand, some findings suggest that dairy has a protective effect against GERD as frequent milk consumption has also been associated with reduced risk of experiencing GERD symptoms [11, 12]. While most of these studies did not differentiate between low-fat and full-fat dairy foods, the fat content of dairy foods may be an important factor, as some studies have reported a positive correlation between fat content of milk and heartburn symptoms [13, 14]. Consumption of higher fat foods delays gastric emptying and leads to gastric distention, a suggested trigger of TLESRs, which is another factor linked to the pathogenesis of GERD [7]. Although both total fat and saturated fatty acid intake have been associated with risk for GERD symptoms [15], the literature has not distinguished between the different sources of saturated fatty acids, so it is unclear what role, if any, dairy fat may play. Other studies again observed no associations between risk for GERD and the consumption of milk [16] or dairy foods [15].
Collectively, modest evidence suggests an association between the consumption of dairy foods, particularly full-fat dairy, and symptoms of GERD. However, this evidence is almost entirely based on data from observational studies, and is inconsistent. To our knowledge, no study has investigated the effect of both low-fat and full-fat dairy consumption on symptoms of GERD using a randomized controlled design. Therefore, this study aimed to explore the impact of dairy consumption, and the fat content of dairy consumed, on the frequency of acid reflux and frequency and severity of HB, using data from a randomized controlled dietary intervention trial.
Methods
Study participants
The clinical portion of this study was completed between January 2016 and October 2018. We recruited men and women with metabolic syndrome living in the greater Seattle area (Supplemental Material 1). A full description of recruiting and screening procedures has been previously published [17]. In short, we identified 4277 potentially eligible individuals from an automated screen of the University of Washington (UW) Medical Center electronic medical record system; screened 354 by telephone and 130 in person at Fred Hutchinson Cancer Research Center (FHCRC); enrolled 76; and randomized 72 to one of three dietary intervention arms. Screening procedures included anthropometric measurements and complete medical, nutritional, physical activity, and medication history questionnaires.
Study design and diets
Following the study initiation visit, all eligible participants completed a 4-week wash-in diet period. During this period, participants were asked to consume a maximum of three servings of nonfat milk per week, not to consume any other dairy products, and otherwise to consume their habitual diet ad libitum. Dietary compliance was assessed at a check-in visit during the wash-in diet period when participants came to FHCRC to pick up dairy products. Each participant also completed two unannounced 24 h dietary recall interviews during the wash-in phase, which were administered by staff from the FHCRC Nutrition Assessment Shared Resource not otherwise associated with the study team. Participants were excluded from the trial for noncompliance if they consumed more than three servings of non-study dairy products over the first 2 weeks of the study, failed to complete one or more daily dairy logs, or did not complete at least one of the two 24 h dietary recall interviews during this period. Individuals excluded for noncompliance or who dropped out during the wash-in period were not randomized, did not complete any clinic visits, did not count toward the recruitment goal, and were not included in any statistical analyses.
In the last week of the wash-in phase, participants completed clinic visit 1 at the UW Translational Research Unit, where they completed a GERD questionnaire to assess the frequency of acid regurgitation and the frequency and severity of HB, both during the day and at night (Supplemental Material 2). We also collected anthropometric measurements and participants completed a modified Blair PAQ and a health questionnaire to assess changes in physical activity, illness and medication/supplements.
Following completion of the wash-in diet phase and baseline assessments at clinic visit 1, participants were randomized to one of three intervention arms. We utilized a block randomization procedure stratified by gender and the homeostasis model assessment index of insulin resistance (HOMA, < 5.0 vs. ≥ 5.0 or diagnosis of diabetes). Subjects either continued to consume a diet with little dairy (“limited dairy diet”, control), or switched to a diet including 3.3 servings/day of either nonfat/low-fat dairy products (“low-fat dairy diet”) or full-fat dairy products (“full fat dairy diet”). The rationale for providing 3.3 servings per day was to ensure that all participants included in the per protocol analysis (consumption of > 90% of administered dairy foods, among other criteria; see below) would consume at least the 3 servings per day that are recommended as part of the Dietary Guidelines in the United States [18]. The FHCRC Human Nutrition Laboratory provided all dairy products to participants.
The limited dairy diet included three servings/week of nonfat milk (i.e., skim milk). The low-fat dairy diet included 23.1 servings/week of nonfat or low-fat dairy products, for an average of 3.3 servings per day. These 23.1 weekly servings consisted of eight servings of nonfat milk, 7.1 servings of nonfat yogurt, and eight servings of low-fat cheese (11–21% fat). In the full-fat dairy diet arm, participants were also provided with 23.1 servings/week, consisting in this case of eight servings of whole milk (3.25% milkfat), 7.1 servings of plain full-fat yogurt (3.1% milk fat), and eight servings of full-fat cheese (21–33% fat). Low-fat and full-fat versions of al study milk, yogurt, and cheese products were procured from the same manufacturer, with the only difference being the fat content of the specific dairy food (for more detail, see Schmidt et al. [17]). One serving of milk was 240 mL, one serving of yogurt 170 g, and one serving of cheese 42.5 g. The total content of dairy fat averaged 0.3 g/day, 8.7 g/day, and 28.5 g/day in the limited, low-fat dairy, and full-fat dairy groups. Participants randomized to the low-fat and full-fat dairy diets were asked to consume all of the dairy products that were provided to them for a given week. Consumption of the nonfat milk was optional for participants randomized to the limited dairy arm. All participants were asked to not consume any other dairy products. Participants kept a daily dairy log of any dairy foods eaten, including study and non-study dairy foods, to track compliance. Participants also recorded any changes in medication or supplement intake as well as any illness. Participants visited the FHCRC Human Nutrition Laboratory every 1–2 weeks to meet with a kitchen staff member, return any leftover dairy foods, and receive a 7–14-day supply of dairy products. Staff weighed all returned dairy products to assess the amount of dairy foods consumed. Additionally, the returned dairy logs were compared against the returned dairy foods and checked for compliance. We contacted participants by phone if compliance was below the desired level (i.e., < 90% of the study dairy foods were consumed, and/or non-study dairy foods were consumed regularly). During the intervention period, participants also completed two additional modified Blair PAQs at approximately 4-week intervals. Participants also completed three additional unannounced 24-h recalls during the intervention phase.
During clinic visit 2, completed 12 weeks ± 1 week after starting the intervention diet, participants completed the same GERD questionnaire administered at clinic visit 1. All the other data collected at clinic visit 1 were also collected at clinic visit 2.
Statistical analysis
This was an exploratory analysis of data collected from a randomized controlled dietary intervention trial designed and powered to test the impact of low-fat and full-fat dairy foods on glucose homeostasis. Statistical analyses were performed using SPSS for Windows (Version 26; IBM). All data are reported as means ± standard deviations for normally distributed variables, or medians (25th; 75th percentile) for non-normally distributed variables, or percentages for categorical variables. Key baseline characteristics were compared by study arm to ensure successful randomization, defined as a p value > 0.1 in statistical tests across the three dietary intervention groups. We conducted both an intent-to-treat (ITT) and a per-protocol analysis. For the ITT analysis, which included all randomized participants, we used multiple imputations to generate five complete datasets, and all analyses were run on all five. For the per-protocol analysis, participants were included if they (a) completed the dietary intervention and all clinic visits, (b) were compliant with the dietary regimen (defined as consuming at least 90% of the study dairy foods provided, and consuming 10 or fewer servings of non-study dairy foods during the 12-week intervention period), and (c) had complete data from the GERD questionnaire.
We also compared changes in other dietary variables that may have resulted from the dietary intervention by conducting repeated measures analyses of variance (RM-ANOVA), with time (clinic visit 1 vs. clinic visit 2) as the within-subjects variable and diet group (limited dairy vs. low-fat dairy vs. full-fat dairy) as the between-subjects variable, to determine whether there was a significant differential change during the intervention period (i.e., a time × diet group interaction). Logarithmic transformations were performed on all outcome variables that were not normally distributed, which included energy intake (kcal/d), the added sugars/fiber-ratio, protein intake (% of energy intake), calcium intake (mg/1,000 kcal), and the changes in carbohydrate intake (% of energy intake), the added sugars/fiber ratio, fat intake (% of energy intake), and saturated fat intake (% of energy intake). Any significant overall time × diet group interaction was followed up with three post hoc repeated RM-ANOVAs with two intervention groups included at a time.
Primary outcome 1: Heartburn Score: A HB score was calculated by adding the products of frequency score (0–4) and severity score (0–3) for HB during the day and at night, resulting in a score ranging from 0 to 24 for each participant (Supplemental Material 2). The HB score was analyzed using RM-ANOVA, with time (clinic visit 1 vs. clinic visit 2) as the within-subjects variable and diet group (limited dairy vs. low-fat dairy vs. full-fat dairy) as the between-subjects variable, to determine whether there was a significant time × diet group interaction. Logarithmic transformations were performed on all outcome variables that were not normally distributed, which included age, BMI, energy intake, physical activity, heart burn score, change in weight, change in waist circumference, and change in physical activity.
Primary outcome 2: Acid Regurgitation: AR was dichotomized as “never”, for participants who indicated they did not experience AR, and “ever”, for participants who indicated they experienced any frequency of AR. We created a binomial logistic regression model to analyze the effect of the dietary interventions on AR at the conclusion of the intervention period (clinic visit 2), adjusted for baseline AR (clinic visit 1).
We also conducted sensitivity analyses for both primary outcomes 1 and 2, excluding participants who had ever been diagnosed with GERD or who used medication for GERD (antacids, PPIs or H2RAs) at any time point. Similarly, we conducted sensitivity analyses adjusting for changes in GERD medication use during the intervention period of the study (decreased use, stable use, increased use). We also conducted sensitivity analyses adjusting for changes in body weight, waist circumference, total energy intake, physical activity, and dietary fiber intake. And lastly, we conducted sensitivity analyses adjusting for any dietary variable that changed differentially during the intervention, which included energy intake, carbohydrate intake, total sugar intake, fiber intake, total fat intake, saturated fatty acid intake, monounsaturated fatty acid intake, protein intake, calcium intake, and the 2015 Healthy Eating Index. This was done by re-running the overall RM-ANOVA model (for HB score) and binomial logistic regression model (for AR), including each of these baseline or change variables as co-variates. The alpha-error level was set to 5%.
Results
Description of participants
All 72 participants randomized to one of the three intervention groups (n = 24 in all three groups) were included in the ITT analysis. Nine subjects were excluded from the per-protocol analysis for a total of 63 participants. Three of the nine excluded participants dropped out of the study prior to the final clinic visit, two were excluded for noncompliance with the dietary intervention, and four participants did not have complete data from the GERD questionnaire collected at one or both clinic visits. At the screening visit, fourteen of the 63 participants indicated a past medical diagnosis of GERD, and 36 participants reported regularly experiencing either AR, HB, or both. Ten took GERD-related medications at baseline (clinic visit #1). During the intervention period, one participant in the full-fat dairy group reported a reduction in GERD medication use, and three participants (two in the full-fat, and one in the limited dairy group) began using GERD medications. There were no significant differences in key baseline characteristics between the intervention groups in both ITT and per-protocol (Table 1) analyses.
Adherence of intervention
Based on data from the Human Nutrition Laboratory on administered and returned study dairy foods and participants’ dairy log entries of consumed non-study dairy foods, per protocol participants (n = 63) consumed 98.3 ± 1.7% and 98.0 ± 2.8% (mean ± SD) of the study dairy foods provided to them during the low-fat and full-fat dairy intervention diet periods, respectively (Table 2). During the limited dairy intervention period, participants consumed an average of 76.5 ± 33.6% of the provided (non-mandatory) nonfat milk. Consumption of non-study dairy foods was 0.6 ± 1.0, 0.6 ± 0.9, and 1.3 ± 2.3 total servings during the 12 weeks of the limited, low-fat, and full-fat dairy diet periods, respectively. Consistent data on total consumption of dairy foods were obtained from the average of three unannounced 24 h dietary recall interviews conducted during the intervention period.
Effects of the intervention on habitual dietary intakes
Avoiding or including dairy foods affected the diets of participants in the three intervention groups differently, in a number of ways (Supplemental Material 3). Specifically, energy intake increased in the full-fat dairy group compared to both the limited and the low-fat dairy group. As a percentage of total energy intake, total fat and saturated fatty acid intake increased while carbohydrate intake decreased in the full-fat dairy group compared to the low-fat dairy group. The 2015 Healthy Eating Index increased in the low-fat dairy group compared to the full-fat dairy group, and calcium intake increased in both dairy groups compared to the limited dairy group.
Effects of the intervention on heartburn and acid regurgitation
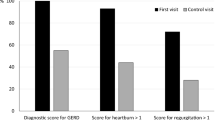
In the per-protocol analysis, there was no effect of the dairy interventions on HB symptoms, as assessed by the HB score (p = 0.443, Fig. 1). The intervention groups also were not significantly associated with AR after adjusting for baseline (clinic visit #1) AR (p = 0.651) (Table 3).
Change in the Heartburn Score in the three dietary intervention groups (per protocol analysis, n = 63). Boxes represent 25th-75th percentiles, and whiskers 5th and 95th percentiles, with outliers represented by a solid dot. Medians are represented by horizontal bars across the boxes and means are represented by crosses. The p value for the time by diet interaction from the overall repeated measures analysis of variance is displayed at the top
Sensitivity analyses adjusting for changes in GERD medications during the intervention, or excluding participants with a past medical history of GERD or GERD-related medication use did not impact the overall intervention effect on frequency of AR or HB score. Similarly, sensitivity analyses adjusting for changes in body weight, waist circumference, total energy intake, fiber intake (in g/1,000 kcal), carbohydrate intake, fat intake, protein intake, saturated fatty acid intake, monounsaturated fatty acid intake, total sugar intake, the 2015 Healthy Eating Index, calcium intake, or physical activity also did not impact the overall intervention effect on either of the two primary outcomes. These findings were identical in the ITT analyses including all 72 randomized participants.
Discussion
In this exploratory analysis of data from a randomized controlled dietary intervention trial, we found that neither the consumption of low-fat nor full-fat dairy products, including milk, yogurt, and cheese, had an effect on HB or AR symptoms in men and women with metabolic syndrome. These findings were consistent in both ITT and per-protocol analyses, and remained robust in sensitivity analyses that adjusted for past medical history of GERD, use of GERD medications, changes in GERD medications during the intervention period, and anthropometric, dietary, and lifestyle changes that may affect GERD symptoms.
To our knowledge, this is the first study to investigate the effects of both low-fat and full-fat dairy consumption on GERD symptoms using data from a randomized controlled trial. Our results are consistent with findings from two observational studies also conducted with participants from the USA that observed no associations between risk for GERD and milk [16] or dairy foods [15]. Both of these studies used food frequency questionnaires to assess dietary intakes and did not distinguish between the different fat contents of dairy products, and what products constituted the dairy food group was not defined in the latter study. GERD symptoms were assessed by a simple questionnaire to determine frequency of either HB or AR [16], or a 32-question validated Gastroesophageal Reflux Questionnaire [15]. In comparison, we used a questionnaire with five questions to assess frequency of AR and both frequency and severity of HB during the day and at night.
On the other hand, our results contradict findings from several other observational studies. Ndebia et al. [9] reported that the consumption of milk and milk products was strongly associated with AR among healthy South African adults in unadjusted analyses. They found that milk product consumption, as assessed by food frequency questionnaire, was associated with the greatest number of reflux parameters, as objectively measured by 24 h esophageal pH-impedance monitoring. Unfortunately, potential confounding by other dietary or non-dietary factors was not addressed in this study. This contrasts with Nam et al. [11] and Chowdhury et al. [12], both of which reported milk as a protective factor for symptoms of GERD. The former, a case–control study from South Korea, analyzed data collected from 3-day food records and GERD questionnaires to find that the third and fourth quartiles of milk consumption were associated with a reduced risk of GERD symptoms. The latter was a cross-sectional study from South India, where a survey was employed to assess GERD symptoms, lifestyle factors, and specific dietary intakes. These authors found that consuming milk less than three times per week was associated with GERD symptoms compared with higher milk consumption. Considering the design of these observational studies, it is not possible to exclude reverse causation underlying these associations, making this literature largely inconclusive.
In our trial, we found no difference in the effect of low-fat vs. full-fat dairy on GERD symptoms. This finding is not consistent with findings from two other studies suggesting that there may be a relationship between the fat content of dairy and GERD. Feldman and Barnett [13] observed a significant positive correlation between fat content of milk and self-reported frequency of HB in a cross-sectional study among middle-aged men and women with a history of HB. Babka and Castell [14] observed a decrease in LES pressure following ingestion of whole milk and an increase in LES pressure with nonfat milk in six young, healthy adults (19–24 years). Given that decreased LES pressure is hypothesized to contribute to the pathogenesis of GERD [6], these data suggest that dietary fat intake could affect GERD symptoms. However, these findings are only generalizable to young adults, which is an important limitation given that GERD is more prevalent among adults older than 50 years [19]. It is also worth considering that the effect of a diet rich in dairy fat may differ dependent on which foods are consumed, such that the full-fat diet in our study may not have affected GERD symptoms, because participants consumed dairy foods with a complex matrix, such as cheese and yogurt along with milk.
Overall, the literature on the impact of dairy on symptoms of GERD is very inconsistent. Some of these inconsistencies could be attributed to the large heterogeneity of studies in terms of study population, outcomes measured, and data collection tools. There are several discrepancies about the criteria used to define GERD symptoms[19], and studies used different GERD questionnaires to assess outcomes. These questionnaires rely on self-reported data from participants and, therefore, are subject to recall bias, and the rating scales employed could be open to interpretation. Some studies opted for more objective measurement tools like esophageal pH-impedance monitoring and intraluminal pressure measurements, but did not always report how these measures compared to clinical symptoms experienced by participants. Another hypothesis that may explain these inconsistencies is the potential role of food intolerances in the development of GERD. The use of leukocytotoxic test-based exclusion diets with GERD patients in the double-blind, randomized, controlled pilot trial of Caselli et al. [10] provides compelling evidence for this theory. Interestingly, this study found that milk was the most frequent food type to induce leukocytotoxic test positivity, affecting 84% (32/38) of participants in this trial. While this may indicate that individuals with GERD symptoms may be more likely to have milk intolerance, it also suggests that the relationship between diet and GERD may be more individualized than previously thought.
Strengths of our study include the randomized, controlled study design, making it the first trial to test effects of low-fat and full-fat dairy food intake on GERD symptoms; strong adherence rates; the standardized wash-in diet limited in dairy; and the inclusion of a wide variety of dairy foods, including fermented versus non-fermented and full-fat versus low-fat versions. However, our study also had several limitations. Data were collected from a study that was not designed to specifically test the impact of dairy foods on GERD symptoms. While more than 50% of participants in each group reported symptoms of GERD (HB, AR, or both), while on the limited dairy wash-in diet period, 27 of the 63 participants included in the per protocol analysis did not suffer from even mild symptoms of AR or HB at baseline. Unquestionably, this may have reduced our ability to detect effects of dairy foods on GERD symptoms. Due to the lack of a power calculation for this exploratory analysis, it is also unclear whether we were adequately powered to detect differences in GERD symptoms between the three study arms, especially in the sensitivity analyses. It may also be suboptimal that we used a questionnaire to assess GERD symptoms, as opposed to objective pH testing, and that the questionnaire we used had not previously been validated. It also remains possible that some selection bias may be present, as individuals who are aware of GERD symptoms in response to dairy may have chosen not to participate. Additionally, the generalizability of our findings to populations other than those with metabolic syndrome is uncertain, as is the effect of dairy foods other than milk, yogurt, and cheese, such as butter, cream, or ice cream. It is, therefore, unclear whether our findings can be extrapolated to the population of GERD patients for whom this research is most relevant. Lastly, the duration of the intervention may have been insufficient to fully capture dairy effects on GERD symptoms.
In conclusion, our study indicates that consuming three servings of dairy per day, regardless of fat content, does not have an effect on AR or HB in men and women with metabolic syndrome. This suggests that consuming dairy may not necessarily trigger, worsen, or alleviate the common GERD symptoms. Given the widespread prevalence of GERD, and that clinicians often offer dietary advice as a first line of therapy, it is important to better understand the role of specific dietary factors in the pathogenesis and management of GERD. Future intervention studies should investigate the effects of different types of dairy foods on AR and HB among participants that have been clinically diagnosed with GERD. Such studies may also benefit from considering the role of individual food intolerances and other lifestyle or dietary factors that may mediate symptoms of GERD, like meal size, macronutrient meal composition, and the time lapse between eating meals and lying down.
Data availability
An anonymized dataset and anonymized biological specimen from this study, including fasting blood and stool, can be made available to qualified investigators by request to Dr. Mario Kratz.
Code availability
The statistical analytical code (an SPSS syntax script) as well as the SPSS dataset can be made available by request to Dr. Mario Kratz.
References
GBD 2017 Gastro-Oesophageal Reflux Disease Collaborators (2020) The global, regional, and national burden of gastro-oesophageal reflux disease in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol 5:561–581. https://doi.org/10.1016/S2468-1253(20)30007-8
Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R, Group GC (2006) The montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol 101:1900–1920. https://doi.org/10.1111/j.1572-0241.2006.00630.x
De Giorgio F, Palmiero M, Esposito I, Mosca F, Cuomo R (2006) Pathophysiology of gastro-oesophageal reflux disease. Acta Otorhinolaryngol Ital 26:241–246
Fox M, Forgacs I (2006) Gastro-oesophageal reflux disease. BMJ 332:88–93. https://doi.org/10.1136/bmj.332.7533.88
Sethi S, Richter JE (2017) Diet and gastroesophageal reflux disease: role in pathogenesis and management. Curr Opin Gastroenterol 33:107–111. https://doi.org/10.1097/MOG.0000000000000337
Badillo R, Francis D (2014) Diagnosis and treatment of gastroesophageal reflux disease. World J of Gastrointestinal Pharm Therapeutics 5:105–112
Surdea-Blaga T, Negrutiu DE, Palage M, Dumitrascu DL (2017) Food and gastroesophageal reflux disease. Curr Med Chem 24:1–14
Festi D, Scaioli E, Baldi F, Vestito A, Pasqui F, Di Biase AR, Colecchia A (2009) Body weight, lifestyle, dietary habits and gastroesophageal reflux disease. World J Gastroenterol 15:1690–1701. https://doi.org/10.3748/wjg.15.1690
Ndebia EJ, Sammon AM, Umapathy E, Iputo JE (2017) Diet affects reflux in a rural African community. Acta Gastro-Enterologica Belgi L 80:357–360
Caselli M, Zuliani G, Cassol F, Fusetti N, Zeni E, Lo Cascio N, Soavi C, Gullini S (2014) Test-based exclusion diets in gastro-esophageal reflux disease patients: a randomized controlled pilot trial. World J Gastroenterol 20:17190–17195. https://doi.org/10.3748/wjg.v20.i45.17190
Nam SY, Park BJ, Cho Y-A, Ryu KH, Choi IJ, Park S, Kim Y-W (2017) Different effects of dietary factors on reflux esophagitis and non-erosive reflux disease in 11,690 Korean subjects. J Gastroenterol 52:818–829. https://doi.org/10.1007/s00535-016-1282-1
Chowdhury SD, George G, Ramakrishna K, Ramadass B, Pugazhendhi S, Mechenro J, Jeyaseelan L, Ramakrishna BS (2019) Prevalence and factors associated with gastroesophageal reflux disease in southern India: a community-based study. Indian J Gastroenterol 38:77–82. https://doi.org/10.1007/s12664-018-00931-6
Feldman M, Barnett C (1995) Relationships between the acidity and osmolality of popular beverages and reported postprandial heartburn. Gastroenterology 108:125–131. https://doi.org/10.1016/0016-5085(95)90016-0
Babka JC, Castell DO (1973) On the genesis of heartburn: the effects of specific foods on the lower esophageal sphincter. Am J Dig Dis 18:391–397. https://doi.org/10.1007/BF01071988
El-Serag HB, Satia JA, Rabeneck L (2005) Dietary intake and the risk of gastro-oesophageal reflux disease: a cross sectional study in volunteers. Gut 54:11–17. https://doi.org/10.1136/gut.2004.040337
Mehta RS, Song M, Staller K, Chan AT (2019) Association between beverage intake and incidence of gastroesophageal reflux symptoms. Clin Gastroenterol Hepatol. https://doi.org/10.1016/j.cgh.2019.11.040
Schmidt KA, Cromer G, Burhans MS, Kuzma JN, Hagman DK, Fernando I, Murray M, Utzschneider KM, Holte S, Kraft J, Kratz M (2020) The impact of diets rich in low-fat or full-fat dairy on glucose tolerance and its determinants: a randomized controlled trial. Am J Clin Nutr 113:534–547. https://doi.org/10.1093/ajcn/nqaa301
United States. Department of Health and Human Services, United States. Department of Agriculture., United States. Dietary Guidelines Advisory Committee. 2015. Dietary guidelines for Americans, 2015–2020. Washington, DC: US Department of Health and Human Services and US Department of Agriculture. 122 pages pp
Eusebi LH, Ratnakumaran R, Yuan Y, Solaymani-Dodaran M, Bazzoli F, Ford AC (2018) Global prevalence of, and risk factors for, gastro-oesophagal reflux symptoms: a meta-analysis. Gut 67:430–440
Acknowledgements
We are deeply indebted to the individuals who volunteered to participate in this trial. We also owe many thanks to the staff of the Human Nutrition Lab, the Prevention Center, and the Nutrition Assessment Shared Resource at Fred Hutch as well as the Translational Research Unit and the Biomolecular Imaging Center at the University of Washington.
Funding
This project was funded to MK by an international consortium of dairy organization, including the United States National Dairy Council, Dairy Farmers of Canada, the Dutch Dairy Organisation (Nederlandse Zuivel Organisatie), Dairy Australia, and the French Dairy Interbranch Organization (CNIEL). This project also received support from the University of Washington Diabetes Research Center (National Institutes of Health grant P30 DK017047) and the Fred Hutch Cancer Center Support Grant (National Institutes of Health grant P30 CA015704). KAS was supported in part by grant T32 CA094880 from the National Institutes of Health. MSB was supported in part by grants R25CA094880, T32DK007247, and T32HL007028 from the National Institutes of Health. KMU is supported by the Department of Veteran Affairs. MK has received honoraria and reimbursements for travel. JK has received honoraria and reimbursements for travel as well as research grants from the Vermont Dairy Promotion Council and the National Dairy Council. IF, GC, MSB, JNK, DKH, KMU, SH, TLV have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Contributions
Conceptualization: IF, KAS, KMU, TLV, MK. Methodology: IF, KAS, KMU, SH, JK, TLV, MK. Formal analysis and investigation: IF, KAS, GC, MSB, JNK, DKH. Writing–original draft preparation: IF, KAS, MK. Writing–review and editing: all authors. Funding acquisition: MK. Supervision: MK.
Corresponding author
Ethics declarations
Conflict of interest
This project was funded to MK by an international consortium of dairy organization, including the United States National Dairy Council, Dairy Farmers of Canada, the Dutch Dairy Organisation (Nederlandse Zuivel Organisatie), Dairy Australia, and the French Dairy Interbranch Organization (CNIEL). MK has also received honoraria and reimbursements for travel from several dairy-related organizations. JK has received honoraria and reimbursements for travel as well as research grants from the Vermont Dairy Promotion Council and the National Dairy Council/Dairy Management Inc. IF, GC, MSB, JNK, DKH, KMU, SH, TLV have no conflicts of interest to disclose.
Ethical approval
Approval for this study was obtained from the Fred Hutch Institutional Review Board, protocol number #8399.
Consent to participate
All participants gave informed written consent prior to being enrolled, and prior to any study procedures.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fernando, I., Schmidt, K.A., Cromer, G. et al. The impact of low-fat and full-fat dairy foods on symptoms of gastroesophageal reflux disease: an exploratory analysis based on a randomized controlled trial. Eur J Nutr 61, 2815–2823 (2022). https://doi.org/10.1007/s00394-022-02855-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-022-02855-6