Abstract
Purpose
Oxidative stress might play an important role in the development of osteoarthritis, but not much is known about the effect of antioxidants on osteoarthritis risk. We, therefore, aimed to investigate the effect of dietary vitamin C, E, beta-carotene, and non-enzymatic antioxidant capacity (NEAC), which measures overall antioxidant activity from the diet, on the risk of osteoarthritis.
Methods
For this study 43,865 men and women from the Swedish National March Cohort (SNMC) were followed for up to 19 years. We computed dietary intake of vitamin C, E and beta-carotene using information from a Food Frequency Questionnaire (FFQ). To estimate dietary NEAC we combined the information from the FFQ with food item-specific antioxidant capacity values from an antioxidant food database. Cases of osteoarthritis were identified through the Swedish National Patient Registers. We categorized all exposure variables into sex-specific quartiles and used multivariable-adjusted Cox proportional hazards regression models to estimate hazard ratios (HRs) with 95% confidence intervals (95% CIs).
Results
In total, we observed 5976 cases of OA during 469,148 person-years of follow-up. After adjusting for potential confounders, we did not find any association between vitamin C, beta-carotene and NEAC (p-values for trend > 0.5), but a positive association was found with higher dietary vitamin E intake (HR Q4 vs Q1: 1.11; 95% CI 1.02–1.21; p for trend = 0.01) and the risk of OA.
Conclusion
Our findings do not provide evidence for dietary antioxidants to protect from the development of OA, and a higher dietary vitamin E intake might even increase the risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is the most common form of arthritis and given the rising obesity rates and the ageing population its prevalence is expected to increase [1]. Exact numbers are difficult to obtain since they vary depending on the definition of OA used, characteristics of the study population, and which specific joints the study included. However, studies have estimated that OA affects around 15% of the total world population and up to 50% of older adults [2,3,4].
OA and its development have been widely investigated and well-known risk factors include age, sex, obesity, and joint injury [2]. In addition, oxidative stress, a condition characterized by an imbalance between free radicals and the body’s antioxidants [5], might play an important role in the pathogenesis of OA [6]. It has been suggested that oxidative stress might lead to chondrocyte and cartilage ageing by inducing telomere genomic instability, replicative senescence, and chondrocyte dysfunction [7]. Further, increased levels of oxidative stress and reduced levels of plasma antioxidants have been reported in patients with knee OA compared to healthy controls [8].
Based on current evidence, treatment options for OA are limited and rather restricted to symptom treatment. Therefore, there is a growing interest in understanding the role of diet for both primary and secondary prevention of OA [9]. Since antioxidants are able to reduce oxidative stress [10], a wide range of dietary antioxidants, such as vitamin C, E and beta-carotene and their association with incidence of OA and OA related symptoms, have been investigated, with inconsistent findings. Some studies reported dietary or plasma vitamin C and E to be positively associated with knee OA [11, 12], whereas other studies have found an inverse association with dietary beta-carotene and vitamin C or supplemental vitamin C with either progression of OA [13] or incidence of knee OA [14].
Antioxidants are known to interact with each other, which could lead to a greater protective effect compared to that achieved by single antioxidant compounds alone [10]. Non-enzymatic antioxidant capacity (NEAC), also known as Total Antioxidant Capacity (TAC), measures overall antioxidant activity from the diet by considering complex synergistic and cumulative interactions between known and unknown antioxidants [10]. To our knowledge, the relation between dietary NEAC and the incidence of OA has not been studied before. To further clarify the effect of antioxidants on the risk of incidence OA we aimed to investigate the effect of dietary vitamin C, E, beta-carotene and NEAC on the risk of OA in men and women over the age of 40 years in a large prospective cohort study.
Subjects and methods
Study design
The Swedish National March Cohort (SNMC) was established in 1997, in conjunction with a 4-day national fundraising event organized by the Swedish Cancer Society in almost 3600 cities and villages around the country [15]. In total, 43,865 men and women filled out a 36-page questionnaire concerning socio-demography, lifestyle and medical history. Informed consent was provided by all participants and the study was approved by the Research Ethics Review Committee at the Karolinska Institutet.
Outcome assessment
To identify OA cases we used the Swedish National Inpatient and Outpatient Register. We defined cases as subjects receiving their first OA diagnosis during follow-up, identified using the International Coding of Disease (ICD-10) codes M15-M19 [polyosteoarthritis (M15), hip (M16), knee (M17), OA of first carpometacarpal joint (M18), other OA (M19)].
Follow-up
The availability of individually unique national registration numbers assigned to all Swedish residents permitted accurate follow-up of health status through continuously updated nationwide registers. To further obtain information about emigration and death, the cohort was linked to the Register of the Total Population and Population Changes. Subjects were followed up from October 1, 1997, until they were first diagnosed with OA, emigrated, died, or until the end of follow-up on December 31, 2016, whichever occurred first.
Study participants
Our final sample was based on 29,406 subjects, after we excluded subjects under the age of 40 years (n = 11,780), and subjects who had been diagnosed with OA (ICD-8 713–715; ICD-9 715, ICD-10 M15–M19) (n = 855), malignant neoplasms of bone and articular cartilage or secondary malignant neoplasm of bone or bone marrow (n = 17), joint injury (n = 1276), or any arthropathy disease other than OA (n = 418) (additional information on ICD-codes 8, 9 and 10 are given in Online Resource 1) before the beginning of follow-up. We further excluded subjects with extreme energy intake (± 3 standard deviations from the ln-transformed mean energy intake, n = 446). None of the participants had a completely missing food frequency questionnaire (a flow-chart with the exclusion criteria is provided in Online Resource 2).
Assessment of exposure and other variables
We used a validated 85-item semi-quantitative food frequency questionnaire (FFQ) [16] to estimate individual intake of common Swedish food items, which further allowed estimation of and adjustment for total energy intake. Subjects were asked how often, on average, they had consumed these items during the previous year, with response categories varying from seldom/never to three or more times per day. Missing values were interpreted as null intakes [17]. To estimate subject-specific energy and nutrient intake, we linked all dietary information to the Swedish National Food Composition database [18].
Daily intakes of dietary vitamin C, E and beta-carotene were computed by multiplying the reported daily consumption frequencies for each food item by the standard portion sizes and the food-specific nutrient values. NEAC values for each food item were obtained from an Italian antioxidant food database, which provided in vitro measurements using the Ferric Reducing Antioxidant Power (FRAP) assay, measured in mmol Fe2+ equivalents per 1 kg fresh weight (FW) of single foods [19, 20]. NEAC values were available for 66 out of the 85 items from the FFQ. Food groups without information on NEAC contained mainly animal products (meat, dairy products), sweets and pastries, which, however, are foods with a low antioxidant content. We then computed total daily dietary NEAC by multiplying reported consumption frequencies by food-specific antioxidant capacity values, taking standard portion sizes into account. In the assessment of dietary NEAC we did not include coffee consumption, since it is unclear if the Maillard products, which are the main contributors to the in vitro antioxidant capacity of coffee, exert the same antioxidant activity in vivo [21]. Further, we did not include vitamin and mineral supplements in the NEAC assessment due to limited information on consumption frequency and duration. The assessment of dietary NEAC through an FFQ has previously been validated in other study populations and has been suggested to be a suitable tool for nutritional epidemiology studies [22,23,24].
The questionnaire additionally provided information on the following potential confounders: Body mass index [BMI, computed as weight divided by height squared (kg/m2)], educational level, alcohol consumption, smoking status, use of vitamin supplements, as well as self-reported history of diabetes, lipid disturbance, and hypertension. Physical activity during a typical day was estimated using a validated Energy Expenditure Questionnaire [25, 26]. This allowed us to compute an estimate of MET-hours per day (METh/day), where MET stands for metabolic energy turnover with one MET corresponding to an energy expenditure of 1 kcal/kg body weight per hour [27].
Statistical methods
We adjusted all exposure variables for energy intake using the nutrient residual model [28] and categorized the distribution into sex-specific quartiles (Q1–Q4), as women in our cohort tended to have a higher dietary antioxidant intake compared to men. Descriptive statistics of the cohort were presented by groups defined by quartiles of each exposure variable. We computed age-standardized incidence rates for OA for each exposure quartile. We used a direct standardization approach using the distribution of follow-up person-years across 5-year age categories in the whole sample.
We used the Cox proportional hazard regression model with age as underlying time scale to estimate hazard ratios (HRs) with 95% confidence intervals (CIs) for each quartile of the exposure, using the lowest quartile as the reference category [29]. We tested the proportional hazards assumption using scaled Schoenfeld residuals. The multivariable models were adjusted for the following potential confounders, which were chosen based on literature knowledge: sex, body mass index (BMI, kg/m2), total physical activity (METh/d), smoking (never, former, current), education (≤ 13 years, > 13 years), total energy intake (kcal/day), alcohol (g/month), use of vitamin supplements (yes, no), self-reported diabetes (yes, no), hypertension (yes, no) and lipid disturbance (yes, no). We additionally adjusted the model for dietary NEAC for coffee intake (0, 1–2, 3–4, ≥ 5 cups/day) because coffee was not included in the NEAC assessment.
We investigated linear trends by estimating the median value of each quartile of dietary vitamin C, E, beta-carotene and NEAC. To investigate possible nonlinear associations, we fitted restricted cubic splines with knots at the 5th, 35th, 65th, and 95th percentiles of the distribution of each exposure variable [30].
We further investigated the role of sex, BMI, total physical activity, smoking, vitamin supplement use, alcohol consumption, and age at baseline as potential effect modifiers of the relationship between NEAC and OA, both, on the multiplicative and the additive scale. To test effect modification on the multiplicative scale we included the cross-product interaction term with the variables of interest and used the likelihood ratio test to compare nested models. Effect modification on the additive scale was tested using the Relative Excess Risk due to Interaction (RERI) [31]. Stratified analyses were conducted if the interaction term was significant.
We categorized potential effect modifiers as follows: sex (female, male), BMI (≤ 25 kg/m2, > 25 kg/m2), smoking (never, ever), vitamin supplement use (no, yes), alcohol consumption [women (≤ 10 g/day, > 10 g/day), men (≤ 20 g/day, > 20 g/day) [32]], and age at baseline (≤ 60 years, > 60 years). This specific age cut-off was set at the age of 60 since previous studies have shown that around that age the risk of OA increases significantly [2]. Total physical activity was categorized into three groups (low, medium, high; categorized according to tertiles of METh/day) and in two groups (low vs. high; categorized according to median METh/day) when testing multiplicative and additive interaction, respectively.
To investigate the robustness of our results we performed several sensitivity analyses. We used the Total Radical Antioxidant Parameter (TRAP) assay, expressed as mmol of Trolox per 1 kg fresh weight, instead of FRAP, to assess dietary NEAC. In addition, we included coffee in the assessment of NEAC, assuming an absorption rate of 6% for antioxidants in coffee [33]. Moreover, we repeated the analyses after excluding subjects diagnosed with secondary OA [ICD-10 M15.3 (multiple arthritis), M16.4–M16.7 (hip), M17.2–M17.5 (knee), M18.2–M18.5 (carpometacarpal joints), M19.1, M19.2, M19.93 (other joints)], since these diagnoses more likely are due to mechanical, rather than dietary factors. In addition, we repeated the analyses separately for hip- and knee OA. We further excluded cases occurring during the first two years of follow-up to investigate possible effects of reversed causality.
For smoking, total physical activity, lipid disturbance, and BMI, 6.5%, 6.5%, 5.8%, and 2.4% of the data were missing, respectively. For the other covariates, the number of missing values was below 2%. To analyse whether or not the missing data affected our results, we performed a multiple imputation analysis by rerunning the model after imputing the missing data based on chained equations, assuming data missing at random [34]. We generated five imputed datasets and the final HRs were obtained by pooling HRs estimated for each of the five datasets. Standard errors were obtained according to Rubin’s rules [35].
All statistical analyses were performed using Stata version 15.1 (Stata Corporation, College Station, TX, USA). All reported p-values were two-sided and p-values < 0.05 were considered statistically significant.
Results
Baseline characteristics of the study population are presented for each exposure variable in Table 1. Women represented 64% of the subjects. The mean age of the study population at baseline was 58 (standard deviation = 11) years. Subjects with a higher intake of vitamins and dietary NEAC tended to have a lower BMI, higher education, and a higher intake of tea, alcohol, fruits, and vegetables. They were also more likely to use vitamin supplements and, if females, more likely to receive hormone replacement therapy. Further, they had a higher intake of each other vitamin or NEAC, respectively. In addition, they reported to a higher extent to have diabetes, hypertension or lipid disturbance more often than the rest of the population. Subjects with a lower intake of vitamins and dietary NEAC were more likely to be smokers and to drink more coffee. Foods contributing most to total dietary NEAC were tea (26%), fruits and vegetables (21%), grains (20%), chocolate (9%) and alcohol (5%).
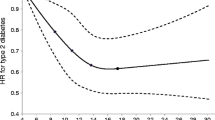
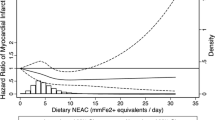
The association between dietary antioxidants, NEAC and OA incidence is presented in Table 2. Overall, we observed 5976 cases of OA during 469,148 person-years of follow up. No significant association was found between dietary vitamin C, beta-carotene, NEAC and the risk of OA in the age- or the multivariable-adjusted models (p-values for trend > 0.5). The regression spline further showed that there was no deviation from linearity (p-values for nonlinearity > 0.05) (Online resource Figs. 2–4). For vitamin E we found a 11% higher risk of OA in subjects in the fourth quartile compared to the first, both in the age-adjusted (HR: 1.11; 95% CI 1.03–1.19; p for trend = 0.003) and the multivariable-adjusted model (HR: 1.11; 95% 1.02–1.21, p for trend = 0.01), both with a significant trend. As before, the regression spline did not show any evidence for a non-linear association (p-value for non-linearity > 0.05) (Fig. 1).
When investigating whether the effect of each exposure variable on the risk of OA was modified by sex, BMI, total physical activity, smoking, vitamin supplement use, alcohol intake, and age, we did not detect any evidence for effect modification for dietary vitamin C, beta-carotene and NEAC on the multiplicative (all p-values for the LR-test > 0.05) or additive scale (all p-values for RERI > 0.05). The effect of vitamin E on the risk of OA was modified by sex (p-value for RERI = 0.02) and vitamin supplement use (p-value for RERI = 0.03) on the additive scale (stratified results are presented in Online resource Table 3a-b).
When running our main model after performing sensitivity analyses by using TRAP instead of FRAP, estimates remained essentially the same (data not shown). When including coffee in the assessment of NEAC, we found a positive association between higher dietary NEAC and the risk of OA in the age- and sex-adjusted model (HR Q4 vs. Q1: 1.11; 95% CI 1.03–1.19; p for trend = 0.39), however, the trend was not significant. Further, this association was attenuated and not significant after adjusting the model for potential confounders (HR Q4 vs. Q1: 1.05; 95% CI 0.97–1.15; p for trend = 0.58). Moreover, excluding subjects with secondary OA (n = 132) and excluding cases occurring during the first two years of follow-up did not affect our estimates (data not shown). When repeating the analyses for hip and knee OA separately, we similarly detected a positive association between vitamin E and the risk of knee OA but not hip OA. No association was found between vitamin C, beta-carotene or NEAC, with any subtype of OA (results are presented in Online resource Table 4a-4d). Finally, when running our main model after using imputed missing data we obtained similar results (data not shown).
Discussion
In this large cohort study of Swedish men and women above the age of 40 years, baseline dietary vitamin C, beta-carotene, and non-enzymatic antioxidant capacity were not associated with the risk of osteoarthritis, whereas a positive association was observed between high intake of dietary vitamin E and the risk of osteoarthritis.
To the best of our knowledge, this is the first study investigating the association between dietary NEAC and the risk of OA.
As oxidative stress might be involved in the development of OA, the hypothesis of antioxidants to protect from OA by reducing levels of oxidative stress is plausible. Several possible mechanisms have been described earlier and various antioxidants might affect OA by reinforcing the cellular antioxidant status. Amongst others, vitamin C is essential for the biosynthesis of the extracellular matrix and protects chondrocytes from differentiation, senescence, and apoptosis. In addition, selenium might help to restore the antioxidative capacity of chondrocytes. Vitamin E might be a potent antioxidant by protecting cell membranes from oxidation by reactive oxygen species. Further, the oral administration of vitamin E was found to protect articular chondrocytes from destruction through lipid peroxidation [6].
Against our expectations, we did not find any association between dietary vitamin C, beta-carotene, NEAC and the risk of incidence OA. We did find a higher dietary vitamin E intake to be associated with an increased risk of overall OA and knee OA. In a previous cross-sectional study among 4685 participants, dietary vitamin C intake was positively correlated with the prevalence of knee OA, whereas no significant association was observed with dietary carotenoids, vitamin E and selenium [11]. Similarly, in a nested case–control study including 3026 male and female participants higher plasma vitamin C and E were associated with an increased risk of radiographic knee OA [12]. In contrast, in a prospective study including 640 participants from the Framingham Heart Study high dietary intake of vitamin C was associated with a reduced risk of developing knee pain. They also reported inverse associations for vitamin C and beta-carotene with the risk of OA progression. No association was found for any dietary antioxidant and incidence of knee OA [13]. Among 1,023 participants from the Clearwater Osteoarthritis longitudinal study, vitamin C supplementation was inversely associated with the incidence of knee OA, but not OA progression [14]. Although vitamin E is also known to become a pro-oxidant if present at high concentrations [36], reaching such high levels through diet only, is unlikely and might therefore not explain our findings of higher dietary vitamin E intake to increase the risk of OA. Vitamin E levels measured through an FFQ in subjects in the highest quartile of dietary vitamin E in our population ranged from 6.1–15.2 mg/day, which is just close to the Recommended Dietary Allowance (RDA) for vitamin E (15 mg/day for adult men and women) [37].
In an intervention study among 38 patients with knee OA, the consumption of pomegranate juice improved OA symptoms and increased plasma antioxidant status. Further, physical function and stiffness were significantly improved in the intervention group at the end of follow-up [38]. Grover et al. [39] published a review article reporting that evidence exists for some antioxidant supplements having beneficial effects on pain relief and function in subjects with knee OA. These supplements were based on curcumin, avocado-soya bean unsaponifiables, Boswellia, and certain herbs used in Chinese and Ayurvedic medicine. Although these findings support our hypothesis, that the beneficial effect of antioxidants on OA risk might be achieved through interactions between antioxidants, we did not detect any association between dietary NEAC and the risk of OA.
In general, studies focusing on the incidence of OA have been inconsistent, whereas the role of diet and antioxidants might be more evident in relation to disease progression and severity of symptoms. One explanation could be the role of the inflammation status, which is directly related to oxidative stress. Thus, if subjects have a higher inflammation status, higher intake of dietary antioxidants might be more effective than in subjects without inflammation.
Our study has several limitations. Food intake was assessed only once at the beginning of follow-up and dietary patterns might change over time, which could lead to misclassification of the exposure. Thus, given the study design, the misclassification is most likely non-differential and would have biased the estimates towards the null, leading to an underestimation of the true association. Although we used a validated FFQ, the validation study does not reveal any information on the performance of single food items, such as tea, fruits, vegetables and grain products, which were the biggest contributors to total dietary NEAC in our study. Nevertheless, they reported a good reproducibility and validity for micronutrients from the diet [16]. In addition, we have previously found that a higher dietary NEAC was associated with a lower risk of myocardial infarction [40], stroke [41] and hip fracture [42] in the same study population, which further supports the validity of a FFQ to assess dietary NEAC. NEAC values were only available for 66 out of 85 food items. However, the NEAC content for the missing items (meat, dairy products, sweets and pastries) is known to be low. Further, NEAC values were calculated from a non-Swedish antioxidant food database. Although geographic location and growing conditions might affect absolute NEAC values, antioxidant databases likely show a similar ranking of the food items according to the NEAC values [43] and therefore, this should not have had an impact on our findings. Another limitation is that we could not include vitamin supplementation when assessing vitamin intake and NEAC, and indeed, the effect of dietary vitamin E intake varied among subgroups of supplements users and non-users. Nevertheless, we did not find any evidence when investigating the potential effect modification of dietary vitamin C, beta-carotene and NEAC by supplement use. Another limitation applies to the identification of OA cases. Although we were able to identify cases through the national In- and Out-patient register, data collection of hospital-based outpatient care started in 2001 [44]. We, therefore, lack information from the Outpatient register for four years. Turkiewicz et al. [3], who conducted a study on 10,000 Swedes, aged 56–84, found that 15% of their subjects had knee OA. However, only two-thirds of those had consulted a physician. Thus, in our study population there could be undiagnosed cases of OA. However, given the prospective design any potential misclassification of the outcome would be non-differential, which would bias estimates towards the null. Strengths of our study include the large study population, the prospective design and the long follow-up.
To conclude, our findings suggest a higher dietary vitamin E intake to be associated with an increased risk of overall and knee OA. No association was found between dietary vitamin C, beta-carotene, NEAC and the risk of OA. Further studies with tight control for confounding and well-assessed nutrient intake, favourably in combination with plasma measurements of dietary antioxidants, are needed to further clarify the association between dietary antioxidants and OA risk.
References
Johnson VL, Hunter DJ (2014) The epidemiology of osteoarthritis. Best Pract Res Clin Rheumatol 28(1):5–15
Neogi T, Zhang Y (2013) Epidemiology of osteoarthritis. Rheum Dis Clin N Am 39(1):1–19. https://doi.org/10.1016/j.rdc.2012.10.004
Turkiewicz A, Gerhardsson de Verdier M, Engström G, Nilsson PM, Mellström C, Lohmander LS, Englund M (2015) Prevalence of knee pain and knee OA in southern Sweden and the proportion that seeks medical care. Rheumatology (Oxford) 54(5):827–835. https://doi.org/10.1093/rheumatology/keu409
Plotnikoff R, Karunamuni N, Lytvyak E, Penfold C, Schopflocher D, Imayama I, Johnson ST, Raine K (2015) Osteoarthritis prevalence and modifiable factors: a population study. BMC Public Health. https://doi.org/10.1186/s12889-015-2529-0
Serafini M, Miglio C, Peluso I, Petrosino T (2011) Modulation of plasma non enzimatic antioxidant capacity (NEAC) by plant foods: the role of polyphenols. Curr Top Med Chem 11(14):1821–1846
Lepetsos P (1862) Papavassiliou AG (2016) ROS/oxidative stress signaling in osteoarthritis. Biochim Biophys Acta Mol Basis Dis 4:576–591. https://doi.org/10.1016/j.bbadis.2016.01.003
Yudoh K, Nguyen V, Nakamura H, Hongo-Masuko K, Kato T, Nishioka K (2005) Potential involvement of oxidative stress in cartilage senescence and development of osteoarthritis: oxidative stress induces chondrocyte telomere instability and downregulation of chondrocyte function. Arthritis Res Ther 7(2):R380–391. https://doi.org/10.1186/ar1499
Suantawee T, Tantavisut S, Adisakwattana S, Tanavalee A, Yuktanandana P, Anomasiri W, Deepaisarnsakul B, Honsawek S (2013) Oxidative stress, vitamin E, and antioxidant capacity in knee osteoarthritis. J Clin Diagn Res 7(9):1855–1859. https://doi.org/10.7860/JCDR/2013/5802.3333
Thomas S, Browne H, Mobasheri A, Rayman MP (2018) What is the evidence for a role for diet and nutrition in osteoarthritis? Rheumatology 57(4):61–74
Serafini M, Del Rio D (2004) Understanding the association between dietary antioxidants, redox status and disease: is the total antioxidant capacity the right tool? Redox Rep 9(3):145–152. https://doi.org/10.1179/135100004225004814
Li H, Zeng C, Wei J, Yang T, Gao S-g, Li Y-s, Lei G-h (2016) Associations between dietary antioxidants intake and radiographic knee osteoarthritis. Clin Rheumatol 35(6):1585–1592
Chaganti R, Tolstykh I, Javaid M, Neogi T, Torner J, Curtis J, Jacques P, Felson D, Lane NE, Nevitt M (2014) High plasma levels of vitamin C and E are associated with incident radiographic knee osteoarthritis. Osteoarthr Cartil 22(2):190–196
McAlindon TE, Jacques P, Zhang YQ, Hannan MT, Aliabadi P, Weissman B, Rush D, Levy D, Felson DT (1996) Do antioxidant micronutrients protect against the development and progression of knee osteoarthritis? Arthritis Rheum-Us 39(4):648–656. https://doi.org/10.1002/art.1780390417
Peregoy J, Wilder FV (2011) The effects of vitamin C supplementation on incident and progressive knee osteoarthritis: a longitudinal study. Public Health Nutr 14(4):709–715. https://doi.org/10.1017/S1368980010001783
Lagerros YT, Bellocco R, Adami HO, Nyren O (2009) Measures of physical activity and their correlates: the Swedish National March Cohort. Eur J Epidemiol 24(4):161–169. https://doi.org/10.1007/s10654-009-9327-x
Messerer M, Johansson S-E, Wolk A (2004) The validity of questionnaire-based micronutrient intake estimates is increased by including dietary supplement use in Swedish men. J Nutr 134(7):1800–1805
Michels KB, Willett WC (2009) Self-administered semiquantitative food frequency questionnaires: patterns, predictors, and interpretation of omitted items. Epidemiology 20(2):295–301. https://doi.org/10.1097/EDE.0b013e3181931515
National Food Administration (1998) Food composition tables. Uppsala, Sweden
Pellegrini N, Serafini M, Colombi B, Del Rio D, Salvatore S, Bianchi M, Brighenti F (2003) Total antioxidant capacity of plant foods, beverages and oils consumed in Italy assessed by three different in vitro assays. J Nutr 133(9):2812–2819
Pellegrini N, Serafini M, Salvatore S, Del Rio D, Bianchi M, Brighenti F (2006) Total antioxidant capacity of spices, dried fruits, nuts, pulses, cereals and sweets consumed in Italy assessed by three different in vitro assays. Mol Nutr Food Res 50(11):1030–1038. https://doi.org/10.1002/mnfr.200600067
Morales FJ, Somoza V, Fogliano V (2012) Physiological relevance of dietary melanoidins. Amino Acids 42(4):1097–1109. https://doi.org/10.1007/S00726-010-0774-1
Rautiainen S, Serafini M, Morgenstern R, Prior RL, Wolk A (2008) The validity and reproducibility of food-frequency questionnaire-based total antioxidant capacity estimates in Swedish women. Am J Clin Nutr 87(5):1247–1253
Pellegrini N, Salvatore S, Valtuena S, Bedogni G, Porrini M, Pala V, Del Rio D, Sieri S, Miglio C, Krogh V, Zavaroni I, Brighenti F (2007) Development and validation of a food frequency questionnaire for the assessment of dietary total antioxidant capacity. J Nutr 137(6):1499
Puchau B, Zulet MA, de Echavarri AG, Hermsdorff HHM, Martinez JA (2010) Dietary total antioxidant capacity is negatively associated with some metabolic syndrome features in healthy young adults. Nutrition 26(5):534–541. https://doi.org/10.1016/J.Nut.2009.06.017
Lagerros YT, Mucci LA, Bellocco R, Nyrén O, Bälter O, Bälter KA (2006) Validity and reliability of self-reported total energy expenditure using a novel instrument. Eur J Epidemiol 21(3):227–236. https://doi.org/10.1007/s10654-006-0013-y
Lagerros YT, Bellocco R, Adami H-O, Nyrén O (2009) Measures of physical activity and their correlates: the Swedish National March Cohort. Eur J Epidemiol 24(4):161–169. https://doi.org/10.1007/s10654-009-9327-x
Ainsworth BE, Haskell WL, Leon AS, Jacobs DR, Montoye HJ, Sallis JF, Paffenbarger RS (1993) Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc 25(1):71–80. https://doi.org/10.1249/00005768-199301000-00011
Willett WC, Howe GR, Kushi LH (1228S) Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr 65(4 Suppl):1220S–1228S
Kom EL, Graubard BI, Midthune D (1997) Time-to-event analysis of longitudinal follow-up of a survey: choice of the time-scale. Am J Epidemiol 145(1):72–80
Marrie RA, Dawson NV, Garland A (2009) Quantile regression and restricted cubic splines are useful for exploring relationships between continuous variables. J Clin Epidemiol 62(5):511–517. https://doi.org/10.1016/j.jclinepi.2008.05.015
Knol MJ, VanderWeele TJ (2012) Recommendations for presenting analyses of effect modification and interaction. Int J Epidemiol 41(2):514–520. https://doi.org/10.1093/ije/dyr218
Catapano AL, Graham I, De Backer G, Wiklund O, Chapman MJ, Drexel H, Hoes AW, Jennings CS, Landmesser U, Pedersen TR (2016) 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J 37(39):2999–3058
Rautiainen S, Levitan EB, Mittleman MA, Wolk A (2013) Total antioxidant capacity of diet and risk of heart failure: a population-based prospective cohort of women. Am J Med 126(6):494–500. https://doi.org/10.1016/j.amjmed.2013.01.006
Royston P (2005) Multiple imputation of missing values: update. Stata J 5(2):188–201
Rubin DB (1976) Inference and missing data. Biometrika 63(3):581–590. https://doi.org/10.1093/biomet/63.3.581
Carocho M, Ferreira IC (2013) A review on antioxidants, prooxidants and related controversy: natural and synthetic compounds, screening and analysis methodologies and future perspectives. Food Chem Toxicol 51:15–25. https://doi.org/10.1016/j.fct.2012.09.021
Galli F, Azzi A, Birringer M, Cook-Mills JM, Eggersdorfer M, Frank J, Cruciani G, Lorkowski S, Ozer NK (2017) Vitamin E: emerging aspects and new directions. Free Radic Biol Med 102:16–36. https://doi.org/10.1016/j.freeradbiomed.2016.09.017
Ghoochani N, Karandish M, Mowla K, Haghighizadeh MH, Jalali MT (2016) The effect of pomegranate juice on clinical signs, matrix metalloproteinases and antioxidant status in patients with knee osteoarthritis. J Sci Food Agric 96(13):4377–4381. https://doi.org/10.1002/jsfa.7647
Grover AK, Samson SE (2016) Benefits of antioxidant supplements for knee osteoarthritis: rationale and reality. Nutr J 15:1. https://doi.org/10.1186/s12937-015-0115-z
Hantikainen E, Grotta A, Serafini M, Trolle Lagerros Y, Nyren O, Ye W, Colarusso L, Bellocco R (2018) Dietary non-enzymatic antioxidant capacity and the risk of myocardial infarction: the Swedish National March Cohort. Int J Epidemiol 47(6):1947–1955
Colarusso L, Serafini M, Lagerros YT, Nyren O, La Vecchia C, Rossi M, Ye W, Tavani A, Adami HO, Grotta A, Bellocco R (2017) Dietary antioxidant capacity and risk for stroke in a prospective cohort study of Swedish men and women. Nutrition 33:234–239. https://doi.org/10.1016/j.nut.2016.07.009
Hantikainen E, Grotta A, Ye WM, Adami HO, Surkan PJ, Serafini M, Michaelsson K, Bellocco R, Lagerros YT (2016) Prospective study of dietary non enzymatic antioxidant capacity on the risk of hip fracture in the elderly. Bone 90:31–36. https://doi.org/10.1016/j.bone.2016.05.006
Carlsen MH, Halvorsen BL, Holte K, Bohn SK, Dragland S, Sampson L, Willey C, Senoo H, Umezono Y, Sanada C, Barikmo I, Berhe N, Willett WC, Phillips KM, Jacobs DR, Blomhoff R (2010) The total antioxidant content of more than 3100 foods, beverages, spices, herbs and supplements used worldwide. Nutr J. https://doi.org/10.1186/1475-2891-9-3
Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C, Heurgren M, Olausson PO (2011) External review and validation of the Swedish national inpatient register. BMC Public Health 11:450. https://doi.org/10.1186/1471-2458-11-450
Acknowledgements
Our thanks go to the Swedish Cancer Society for organizing the National March as well as to Statistics Sweden for scanning the questionnaires. This study was made possible by the Swedish Cancer Society (Grant CAN 2012/591), Telefonaktiebolaget LM Ericsson, ICA AB, and the Ulla och Gustaf af Ugglas Foundation.
Author information
Authors and Affiliations
Contributions
YTL designed research; all authors conducted research; EH, LV, MP, and AG analysed data; all authors interpreted data; the first draft of the manuscript was written by LV and EH; all authors revised the manuscript; all authors read and approved the final manuscript; EH has primary responsibility for final content.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Swedish Data Inspection Board and the regional Ethics committee.
Informed consent
All participants gave informed consent to participate in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Veen, L., Hantikainen, E., Bellocco, R. et al. Dietary antioxidants, non-enzymatic antioxidant capacity and the risk of osteoarthritis in the Swedish National March Cohort. Eur J Nutr 60, 169–178 (2021). https://doi.org/10.1007/s00394-020-02239-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-020-02239-8