Abstract
Background and aims
The Nordic diet (ND), is supposed to be associated with a reduced cardiovascular risk; however, clinical trials have led to inconsistent results regarding the effect of this diet on cardio-metabolic markers. Using systematic review and meta-analysis of randomized controlled trials (RCTs), this study aimed to investigate the effect of the ND on circulating levels of total, low-density lipoprotein (LDL), and high-density lipoprotein (HDL) cholesterol, and triglyceride (TG), as well as blood pressure in human adults.
Methods
PubMed, Scopus, ISI Web of Science, and Google Scholar were searched up to February 2018 for relevant articles. Random effects model was used to estimate the overall effects.
Results
Five RCTs consisting of 513 participants were included in the present review. The meta-analysis of five eligible studies showed that ND significantly reduces the total [weighted mean difference (WMD) = − 0.38 mmol/l, 95% confidence interval (CI) − 0.76, − 0.01, P = 0.044] and LDL cholesterol (WMD = − 0.30 mmol/l, 95% CI − 0.54, − 0.06, P = 0.013) levels compared with the control groups; however, none was seen for HDL cholesterol and TG levels. The meta-analysis of four eligible RCTs revealed that the ND significantly reduces the systolic (WMD = − 3.97 mmHg, 95% CI − 6.40, − 1.54, P = 0.001) and diastolic blood pressure (WMD = − 2.08 mmHg, 95% CI − 3.43, − 0.72, P = 0.003).
Conclusion
The Nordic dietary pattern improves blood pressure and also some of blood lipid markers and it should be considered as a healthy dietary pattern.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Nordic diet (ND) also known as the Baltic Sea diet, is developed in the Nordic or Northern European regions [1] and emphasizes on the consumption of different healthy foods such as whole grains, fruits (such as berries, apples, and pears), vegetables, legumes (such as oats, barley, and almonds), rapeseed oil, fatty fish (such as salmon, herring and mackerel), shellfish, seaweed, low-fat choices of meat (such as poultry and game), low-fat dairy, and salt restriction and also discourages the intake of sugar-sweetened products [2, 3].
The ND as well as the dietary approaches to stop hypertension (DASH) diet which is high in fruits, vegetables, whole grains, fish, poultry, nuts and low in sodium, and the Mediterranean diet which is known with high amounts of fruits, vegetables, legumes, nuts, fish, olive oil and low amount of red meat, and sweets have been considered as healthy dietary patterns. Several meta-analyses of clinical studies have shown that the adherence to the DASH and the Mediterranean dietary patterns is associated with improvements in lipid profile and blood pressure, and cardiovascular diseases (CVDs) risk [4,5,6,7]. Hypertension and dyslipidemia both contribute to a significant proportion of mortality; because they are well-known risk factors for CVDs as the worldwide leading causes of death [8,9,10]. Furthermore, hypertension and dyslipidemia are associated with other diseases including kidney diseases, and type 2 diabetes mellitus [8, 9].
The ND is also supposed to be effective in improving cardiovascular risk factors including blood pressure and blood lipid profile [11]. A number of observational studies have proposed an inverse association between adherence to the Nordic dietary pattern and risk of stroke, type 2 diabetes, and all-cause mortality [12,13,14]; however, the other investigations could not reveal the same results [15, 16]. Several randomized controlled clinical trials have been also conducted regarding the effect of the ND on blood pressure and lipid profile; this is while they have led to inconsistent findings. Although, a number of trials could not reveal the significant effect of the ND on some blood lipid concentrations and blood pressure [2, 17], the others represented the favorable effect of this dietary pattern on these outcomes [3, 18]. Randomized clinical trials are considered as the best methodological approaches to evaluate the causal association between diet and metabolic conditions. We are not aware of any study trying to summarize the effect of ND on cardiovascular risk factors. Therefore, the present systematic review and meta-analysis of randomized controlled trials (RCTs) was designed to assess the overall effect of the ND on cardio-metabolic markers including blood pressure and lipid profile among the adult population.
Materials and methods
The study protocol was registered in the PROSPERO database in January 2017 (http://www.crd.york.ac.uk/PROSPERO; CRD42017054096) [19]. The current report is also designed in accordance with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guideline [20].
Search strategy
Potentially eligible studies were identified through searching PubMed (http://www.pubmed.com; National Library of Medicine), Scopus (http://www.scopus.com/), ISI Web of Science (http://www.thomsonreuters.com), and Google Scholar (http://www.scholar.google.com) from inception up to February 2018. The search was performed without any restrictions, and the title and abstracts were searched with the use of the following search query: (Nordic AND diet*) OR (nordiet) OR (“baltic sea” AND diet*).
The initial screening of titles and abstracts of all potentially eligible articles, as well as further assessment of the full texts was done independently by two investigators (NRJ, MM) and any discrepancy was resolved by consulting the third author (ASA). In addition, the reference list of included papers and related review articles was manually scanned to identify any other potentially relevant trials.
Eligibility criteria
The following inclusion criteria were considered for selecting the relevant investigations: (1) RCTs which reported the effect of the ND or Nordic nutrition recommendations (which is similar to the Nordic diet [21]) on adult humans; (2) reporting circulating blood lipids [total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and triglyceride (TG)], apolipoproteins (apolipoprotein A1, and apolipoprotein B), and blood pressure (systolic and/or diastolic blood pressure) as the primary or secondary outcome variable.
Trials were excluded if (1) they were performed in children or adolescents aged younger than 18 years; (2) reported duplicate data of bigger studies (we included those with the longest follow-up and more sample size); (3) they were used the concomitant intervention in the ND arm/period (i.e., difference between the intervention and the control groups/periods was more than ND; such as pharmacological treatments or exercise); (4) evaluated the effect of replacing individual food component(s) rather than the whole dietary pattern.
Data extraction
Two authors (NRJ, MM) extracted data from the selected trials. This process was verified by another investigator (ASA). The following data were extracted: first author’s last name, publication year, country in which the study was performed, study design (parallel/crossover), sample size, age (mean or median), sex (female/male/both genders), intervention duration (day), participants’ health status, the food/nutrient composition of the dietary patterns advised to the intervention and control groups, the method used to check the dietary adherence, and the outcome variables. To obtain the data that were not presented in the original articles, we sent two e-mails 1 week apart to the corresponding authors.
Risk of bias assessment
The individual publications included in the present systematic review were checked using the Cochrane collaboration’s risk of bias assessment tool considering seven domains: (1) random sequence generation (selection bias), (2) allocation concealment (selection bias), (3) blinding of participants and personnel (performance bias), (4) blinding of outcome assessment (detection bias), (5) incomplete outcome data (attrition bias), (6) selective reporting (reporting bias), and (7) evaluation of the dietary compliance as another possible source of bias. Because blinding is not possible in dietary interventions, we graded the RCTs regarding the other six domains (random sequence generation, allocation concealment, blinding of outcome assessment, incomplete outcome data, selective reporting, and evaluation of dietary compliance). Each domain was judged as low risk of bias, high risk of bias, or unclear risk of bias [22]. Eventually, the overall quality of studies was classified as good (low risk for more than two domains), fair (low risk for two domains), and weak (low risk for less than two domains).
Statistical analysis
The mean change values from baseline to after follow-up for each intervention and control group/period and their standard deviations (SDs) were extracted to calculate the mean difference and its standard error (SE) between the Nordic and control diets, which was used as the effect size for meta-analysis. If the change values were not reported, we calculated SD for the change values by selecting 0.5 as the correlation coefficient (r = 0.5) and to make sure that the meta-analysis was not sensitive to the selected correlation coefficient, all analyses were repeated using correlation coefficients of 0.2 and 0.8.
The weighted mean difference (WMD) and its corresponding 95% confidence intervals (CIs) were calculated using the random effects model which takes the between-study heterogeneity into account [23]. The between-study heterogeneity was assessed using the Cochrane Q test and I-squared statistic (I2 is an estimate ranging from 0 to 100%, with its lower values indicate lower levels of heterogeneity) [24]. To examine the potential sources of between-study heterogeneity, several subgroup analyses were performed according to follow-up time (≤ 3 months/> 3 months), the health status of the participants (with/without metabolic syndrome), and type of control diet (typical diets/average Danish diet). Sensitivity analysis was used to assess the robustness of the meta-analyses results by sequentially removing individual included studies [25]. The presence of the publication bias was checked for each outcome through statistical asymmetry tests (Egger’s regression asymmetry test and Begg’s adjusted rank correlation test), and also by visually inspecting Begg’s funnel plot [26]. All statistical analyses were performed using STATA, version 11.2 (Stata Corp, College Station, TX) and two-sided P values less than 0.05 were considered as statistically significant.
Results
Study selection
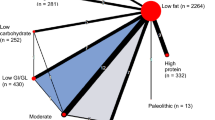
The electronic search resulted in 2719 potentially relevant studies. The screening of the titles/abstracts led to 44 papers in which their full texts were checked for their eligibility. Of these, 39 articles were excluded because (1) 10 studies were conducted in participants aged younger than 18 years [27,28,29,30,31,32,33,34,35,36], (2) 18 studies evaluated the effect of the ND on other outcomes and had no data on selected outcome variable [37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54], (3) 5 papers [50, 55,56,57,58] reported data from studies which were already included in the current review [2, 18, 59], (4) 4 studies examined the effect of individual food components rather than the whole Nordic dietary pattern [60,61,62,63]. One study compared the effect of the Nordic diet with the Paleolithic diet which was different from the control diets in other included studies [64], and (5) 1 study had no control group [65]. In total, five eligible RCTs were reviewed in the present systematic review and meta-analysis [2, 3, 17, 18, 59]. Five trials (n = 513) reported the effect of the ND on lipid profile and four trials (n = 492) reported the effect on blood pressure. The detailed steps of the study selection process are shown in Fig. 1.
Description of the intervention and the control diets
The intervention diets were as follows: Nordic diet [including whole grains, fruits (such as berries, apples, and pears), vegetables, legumes (such as oats, barley, and almonds), rapeseed oil, fatty fish (such as salmon, herring and mackerel), shellfish, seaweed, low-fat choices of meat (such as poultry and game), low-fat dairy and low-salt products and also no intake of sugar-sweetened products] [2, 3, 17, 18] or Nordic nutrition recommendation [including a low-fat (28% of energy) and high-fiber diet] which is similar to the Nordic diet [59].
The control diets were as follows: typical diets [the usual diets that subjects already consumed] or average Danish diet [including refined grains (e.g., rice and pasta), dairy and cheese, meat, convenience foods, sugary products and a lower content of low-fiber vegetables and imported fruit (e.g., citrus, bananas, and melons)] (Table 1). In overall, the main differences between the intervention and control diets were in the intake of whole grains, fatty fish, bilberries and salt.
Study characteristics
Four studies had a parallel design [2, 3, 17, 18] and one study used a crossover design [59]. The included investigations were performed between 1994 and 2014 in European countries, and enrolled 513 participants. The average intervention duration varied between 2 weeks and 6 months. The study population in all trials consisted of both gender, with the age ranging from 39 to 60 years. Moreover, studies had participants with different health status. One study included mildly hypercholesterolemic individuals [3], three studies were done in patients with MetS [2, 17, 18], and one study included healthy participants [59]. The characteristics of the included studies are abstracted in Table 1.
Risk of bias assessment
With regard to the specific domains of the risk of bias assessment tool developed by the Cochrane Collaboration, the overall quality of all included studies was rated as “good” (low risk of bias) [2, 3, 17, 18], except one that was “fair” in quality [59]. None of these dietary intervention trials could blind their participants or personnel. All of the studies stated that the participants were randomized; however a number of them did not mention the randomization method [2, 59]. There was no report of allocation concealment and blinding of outcome assessment in the majority of the trials. No indication of bias due to selective reporting or attrition was observed in all of the included studies. The majority of included studies were low risk regarding the method used for the assessment of the dietary compliance because they described a method to ensure this point and the food items were provided for the participants (Table 1). The included studies used several approaches to check the dietary compliance such as organizing regular meetings with dietitian for general advice on healthy eating and how to comply with the diet [18], using a short questionnaire regarding dietary compliance of participants and their satisfaction with the diet [18], providing daily study checklists including menus for up to 4 days [3], asking participants to comment and describe any deviation from the menu [3], assessing the dietary intake by 3- or 4-day dietary records several times during the study [2, 17, 18], and in two studies participants kept consumption records regarding the intake of main foods like cereal products, fish, vegetables and berries throughout the study period to ensure compliance in addition to the food records [2, 17]. There was only one study which did not report the method for assessing the adherence [59]. The methods used to assess the adherence in each eligible study is provided in Table 1. The results of the methodological quality assessment are summarized in Table 2.
Meta-analysis
Total cholesterol (TC)
The pooled mean difference derived from five trials with 513 subjects [2, 3, 17, 18, 59] was − 0.38 mmol/l (95% CI − 0.76, − 0.01, P = 0.044; Fig. 2a), with high between-study heterogeneity (Q statistic = 48.43, Cochrane Q test, P < 0.001, I2 = 91.7%). The subgroup analysis showed that adherence to the ND led to a significant reduction in TC concentrations compared with the average Danish diet (WMD = − 0.30 mmol/l, 95% CI − 0.48, − 0.13, P < 0.001; I2 = 24.8%, Cochrane Q test, P = 0.249), but when compared with typical diets, the effect was not significant. Moreover, significant change of TC following the ND was observed in studies with more than 3 months of follow-up (WMD = − 0.18 mmol/l, 95% CI − 0.31, − 0.05, P = 0.005; I2 = 0%, Cochrane Q test, P = 0.359), while there was no considerable difference in studies with less than 3 months of duration. The overall effect of ND on serum TC as well as the results of the subgroup analyses are provided in Table 3.
Low-density lipoprotein cholesterol (LDL-C)
Five clinical trials evaluated the effect of adherence to the Nordic dietary pattern on LDL-C levels [2, 3, 17, 18, 59]. The analysis showed that the ND intake was associated with a significant reducing effect on LDL-C levels (WMD = − 0.30 mmol/l, 95% CI − 0.54, − 0.06, P = 0.013; Fig. 2b). The heterogeneity between studies was also considerable (Cochran’s Q test, Q statistic = 32.73, P < 0.001, I2 = 87.8%). A remarkable reduction in LDL-C concentrations was observed following the ND in studies which conducted among patients with MetS (WMD = − 0.13 mmol/l, 95% CI − 0.23, − 0.02, P = 0.016; I2 = 0%, Cochrane Q test, P = 0.738), in studies with more than 3 months of follow-up (WMD = − 0.14 mmol/l, 95% CI − 0.25, − 0.03, P = 0.011; I2 = 0%, Cochrane Q test, P = 0.930), and also in studies in which the Nordic dietary pattern was compared to the average Danish diet (WMD = − 0.22 mmol/l, 95% CI − 0.37, − 0.07, P = 0.003; I2 = 55.6%, Cochrane Q test, P = 0.133) (Table 2).
High-density lipoprotein cholesterol (HDL-C)
Meta-analysis of data from five studies [2, 3, 17, 18, 59] evaluating the effect of adherence to the ND on HDL-C levels could not show a significant effect (WMD = − 0.06 mmol/l, 95% CI − 0.15, 0.02, P = 0.150; Fig. 2c). There was a significant between-study heterogeneity (Cochran’s Q test, Q statistic = 29.46, P < 0.001, I2 = 86.4%). The subgroup analysis revealed a significant reduction in HDL-C levels in studies with less than 3 months of intervention period (WMD = − 0.13 mmol/l, 95% CI − 0.22, − 0.03, P = 0.006; I2 = 62.5%, Cochrane Q test, P = 0.07), and also in studies conducted among subjects without MetS (WMD = − 0.17 mmol/l, 95% CI − 0.23, − 0.11, P < 0.001; I2 = 0%, Cochrane Q test, P = 0.684). The conciderable changes of HDL-C values were not observed in other subgroups (Table 3).
Triglyceride (TG)
The analysis of five studies [2, 3, 17, 18, 59] represented that the changes in TG levels following the ND were not statistically different from the control diets (WMD = − 0.007 mmol/l, 95% CI − 0.13, 0.11, P = 0.917; Fig. 2d). Moreover, a significant heterogeneity across the studies was observed (Q statistic = 9.92, Cochrane Q test, P = 0.042, I2 = 59.7%); however, it was explained by study duration, and the health status of the study participants (with/without MetS). No beneficial effect of the Nordic pattern on serum TG levels was observed in any of subgroups (Table 3).
Other lipid profile parameters
The results of our meta-analysis indicated that the ND considerably decreased the LDL-C/HDL-C ratio (WMD = − 0.15, 95% CI − 0.29, − 0.01, P = 0.029; data were available from three studies [2, 3, 18]) and the apoB/apoA1 ratio (WMD = − 0.04, 95% CI − 0.06, − 0.01, P = 0.002; data were available from three studies [2, 3, 17]); however, this dietary pattern did not significantly affect apoA1 (WMD = − 0.09 g/l, 95% CI − 0.33, 0.15, P = 0.456; data were available from two studies [2, 3]) and apoB (WMD = − 0.10 g/l, 95% CI − 0.25, 0.05, P = 0.212; data were available from three studies [2, 3, 17]). Although heterogeneity was evident between studies evaluating the effect on apoA1 (I2 = 97%, Cochrane Q test, P < 0.001) and apoB (I2 = 94.8%, Cochrane Q test, P < 0.001) levels, the subgroup analyses were not performed due to fewer number of studies.
Systolic and diastolic blood pressure (SBP and DBP)
The pooled estimate of four trials [2, 3, 17, 18] revealed a statistically significant reduction in SBP by 3.97 mmHg (95% CI − 6.40, − 1.54, P = 0.001; Fig. 3a) and DBP by 2.08 mmHg (95% CI − 3.43, − 0.72, P = 0.003; Fig. 3b) favoring the Nordic dietary pattern over the control diets. There was no significant between-study heterogeneity for SBP (I2 = 26.1%, Cochrane Q test, P = 0.255) and DBP (I2 = 0%, Cochrane Q tets, P = 0.486). The subgroup analysis revealed that the lowering effect of the Nordic dietary pattern on both systolic and diastolic blood pressure was significant in long-term interventions (> 3 months). The overall effects as well as subgroup analyses are summarized in Table 4.
Sensitivity analysis and publication bias
The results of the sensitivity analysis showed that removing the studies done by Uusitupa et al. [2], Poulsen et al. [18], and Marckmann et al. [59] changed the overall effect of the Nordic dietary pattern on TC levels to a non-significant value. It was also observed that removal of the study done by Marckmann et al. [59] also altered the pooled estimate of LDL-C levels to statistically non-significant result. The summary effect of the ND was sensitive to the study by Uusitupa et al. [2] for HDL values and the study by Poulsen et al. [18] for DBP values. None of the other pooled estimates were sensitive to individual studies.
Although slight asymmetries were seen in the funnel plots depicting the effect sizes (MD) against their corresponding standard errors, statistical asymmetry tests provided no evidence of publication bias for the meta-analysis of TC (Begg’s test, P = 0.806; Egger’s test, P = 0.680), LDL-C (Begg’s test, P = 1.00; Egger’s test, P = 0.692), HDL-C (Begg’s test, P = 0.462; Egger’s test, P = 0.486), TG (Begg’s test, P = 0.221; Egger’s test, P = 0.250), SBP (Begg’s test, P = 1.00; Egger’s test, P = 0.817), and DBP (Begg’s test, P = 0.734; Egger’s test, P = 0.719).
Discussion
In the present systematic review and meta-analysis, we assessed the effectiveness of the Nordic dietary pattern in improving cardio-metabolic markers including blood pressure and lipids by reviewing available published randomized controlled intervention trials. The synthesis of the data from five RCTs with 513 participants showed that adherence to the Nordic dietary pattern results in a significant reduction in systolic and diastolic blood pressure. Our results also showed that the ND significantly affects total and LDL cholesterol levels compared with the control diets. The Nordic dietary pattern failed to generate significant changes in HDL-C and TG values. Moreover, the LDL-C/HDL-C ratio and the apoB/apoA1 ratio which proposed to be better predictors of increased cardiovascular risk [66, 67], significantly decreased following the ND.
In addition, the beneficial effects of this dietary pattern appear to be greater among patients with MetS who had abnormal blood pressure and blood lipid levels, in longer intervention periods, and also when compared with the average Danish diet as a control diet. This result may be due to the food groups characteristics of the average Danish diet which consists of refined grains (e.g., rice and pasta), dairy and cheese, meat, convenience foods, sugary products and a lower content of low-fiber vegetables and imported fruit (e.g., citrus, bananas, and melons) [18]. Several fundamental differences are derived from the comparison of the ND components with this dietary pattern: (1) more calories from plant-based foods and fewer from meat; (2) more sea foods (e.g., fatty fish, shellfish, and seaweed); (3) more local foods collected in the wild; (4) avoidance of sugar-sweetened products [68]. Indeed, the ND provides healthy and effective recommendations for improving the health, compared with the average Danish diet which is highly similar to the Western diet.
Our results regarding the effect of the ND on blood pressure are consistent with a meta-analysis by Ndanuko et al. [9] which evaluated the effects of various healthy diets such as DASH diet, Nordic diet, and Mediterranean diet and found a significant benefit in terms of systolic and diastolic blood pressure reduction in all these dietary patterns. However, the mentioned meta-analysis could include three studies which evaluated the effects of the Nordic pattern on blood pressure. On the other hand, another meta-analysis of three Finnish cross-sectional studies [69] that examined the associations between the Nordic pattern and cardio-metabolic risk factors showed no difference in the TC and TG levels between the quintiles of the Nordic diet score. Moreover, the risk of lowered HDL-C levels was higher in women with the highest quintile compared to the lowest quintile of the ND adherence score. However, no association was observed between the Nordic diet score and hypertension [69].
Several possible mechanisms for the advantageous effect of the ND on lipid profile and blood pressure have been proposed. Some studies have shown that adherence to the Nordic dietary pattern led to lower energy intake compared to those with the control diets [3, 18]. A previously published meta-analysis demonstrated that every 1 kg of weight loss might decrease the systolic and diastolic blood pressure by 1 mmHg [70]. Therefore, the reduction in blood pressure might be the result of reduced energy intake, and consequently weight reduction in the ND recipients. On the other hand, a higher intake of fruits, vegetables, dietary fiber, and nuts as well as a lower intake of sodium could be associated with significant improvements in blood pressure following the ND [71, 72]. The results of two systematic review and meta-analysis also showed that the increased protein intake, as observed in the ND, is associated with improvement in blood pressure [73, 74].
According to the results of pervious meta-analyses, adherence to the DASH diet was favorably associated with SBP (− 6.74 mmHg, 95% CI − 8.25, − 5.2) and DBP (− 3.54 mmHg, 95% CI − 4.29, − 2.79) [5], and also the Mediterranean diet lowered SBP by 1.44 mmHg and DBP by 0.7 mmHg [75]. Although no study has directly compared the effect of the ND on blood pressure with the DASH and the Mediterranean diet, when the results of present meta-analysis are compared with other healthy dietary patterns such as the DASH and Mediterranean diets, the effect of the ND on blood pressure seems to be greater than the Mediterranean diet; however, it was not as effective as the DASH diet in reducing blood pressure. It should be mentioned that the reduced blood pressure following adherence to these dietary patterns could be of great importance at the population level because even a modest reduction of blood pressure in a long-term period might reduce the mortality from CVDs [71].
We also found that the ND beneficially affects some blood lipid markers such as total and LDL cholesterol, LDL-C/HDL-C ratio and the apoB/apoA1 ratio. The lowering effect of the ND on total and LDL cholesterol levels might be associated with its high content of dietary fiber and rapeseed oil [76, 77]. It has been reported that dietary fiber and rapeseed oil have a significant impact on LDL-C and TC values, but no beneficial effects have been observed on TG and HDL levels which are similar to our finding regarding the effects of the ND on lipid profile. Indeed, the high concentrations of alpha-linolenic acid in the rapeseed oil seem to be responsible for its favorable effect on some lipid profile parameters as well as blood pressure [78, 79]. The non-significant effect of the ND on serum HDL levels might be explained by the restricted fat intake in this diet [2]. On the other hand, it has been suggested that the TG concentrations will not increase if the diet is low in sucrose and high in fiber [80] as observed in the Nordic dietary pattern.
The present systematic review and meta-analysis was conducted based on comprehensive and systematic search to identify all relevant published studies and no evidence for publication bias was observed. Moreover, the meta-analysis was restricted to RCTs that met predetermined methodological criteria to minimize the bias. However, it should be considered that all reviewed trials were conducted in the European countries, and there are no data regarding the efficacy of the Nordic dietary pattern in other populations.
The present systematic review and meta-analysis, provides the evidence for beneficial effects of this diet in reducing blood pressure and some lipid profile parameters. Moreover, the ND can be more effective among patients with MetS probably because of more variability among them. Further studies with adequate duration and sample sizes are recommended to investigate the efficacy of the Nordic dietary pattern in the improvement of cardiovascular risk factors.
References
Uusitupa M, Hermansen K, Savolainen MJ, Schwab U, Kolehmainen M, Brader L, Mortensen LS, Cloetens L, Johansson-Persson A, Onning G, Landin-Olsson M, Herzig KH, Hukkanen J, Rosqvist F, Iggman D, Paananen J, Pulkki KJ, Siloaho M, Dragsted L, Barri T, Overvad K, Bach Knudsen KE, Hedemann MS, Arner P, Dahlman I, Borge GI, Baardseth P, Ulven SM, Gunnarsdottir I, Jonsdottir S, Thorsdottir I, Oresic M, Poutanen KS, Riserus U, Akesson B (2013) Effects of an isocaloric healthy Nordic diet on insulin sensitivity, lipid profile and inflammation markers in metabolic syndrome—a randomized study (SYSDIET). J Intern Med 274(1):52–66. https://doi.org/10.1111/joim.12044
Uusitupa M, Hermansen K, Savolainen MJ, Schwab U, Kolehmainen M, Brader L, Mortensen LS, Cloetens L, Johansson-Persson A, Ouml;nning G, Landin-Olsson M, Herzig KH, Hukkanen J, Rosqvist F, Iggman D, Paananen J, Pulkki KJ, Siloaho M, Dragsted L, Barri T, Overvad K, Knudsen KEB, Hedemann MS, Arner P, Dahlman I, Borge GIA, Baardseth P, Ulven SM, Gunnarsdottir I, Jonsdottir S, Thorsdottir I, Oresic M, Poutanen KS, Riserus U, Akesson B (2013) Effects of an isocaloric healthy Nordic diet on insulin sensitivity, lipid profile and inflammation markers in metabolic syndrome—a randomized study (SYSDIET). J Intern Med 274(1):52–66. https://doi.org/10.1111/joim.12044
Adamsson V, Reumark A, Fredriksson IB, Hammarstrom E, Vessby B, Johansson G, Riserus U (2011) Effects of a healthy Nordic diet on cardiovascular risk factors in hypercholesterolaemic subjects: a randomized controlled trial (NORDIET). J Intern Med 269(2):150–159. https://doi.org/10.1111/j.1365-2796.2010.02290.x
Siervo M, Lara J, Chowdhury S, Ashor A, Oggioni C, Mathers JC (2015) Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: a systematic review and meta-analysis. Br J Nutr 113(1):1–15. https://doi.org/10.1017/s0007114514003341
Saneei P, Salehi-Abargouei A, Esmaillzadeh A, Azadbakht L (2014) Influence of Dietary Approaches to Stop Hypertension (DASH) diet on blood pressure: a systematic review and meta-analysis on randomized controlled trials. Nutr Metab Cardiovasc Dis 24(12):1253–1261. https://doi.org/10.1016/j.numecd.2014.06.008
Kastorini C-M, Milionis HJ, Esposito K, Giugliano D, Goudevenos JA, Panagiotakos DB (2011) The effect of Mediterranean diet on metabolic syndrome and its components: a meta-analysis of 50 studies and 534,906 individuals. J Am Coll Cardiol 57(11):1299–1313
Sofi F, Abbate R, Gensini GF, Casini A (2010) Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr 92(5):1189–1196
Jeong JS, Kwon HS (2017) Prevalence and clinical characteristics of dyslipidemia in Koreans. Endocrinol Metab (Seoul, Korea) 32(1):30–35. https://doi.org/10.3803/EnM.2017.32.1.30
Ndanuko RN, Tapsell LC, Charlton KE, Neale EP, Batterham MJ (2016) Dietary patterns and blood pressure in adults: a systematic review and meta-analysis of randomized controlled trials. Adv Nutr 7(1):76–89. https://doi.org/10.3945/an.115.009753
Jolfaie NR, Rouhani MH, Surkan PJ, Siassi F, Azadbakht L (2016) Rice bran oil decreases total and ldl cholesterol in humans: a systematic review and meta-analysis of randomized controlled clinical trials. Hormone Metab Res Hormon- und Stoffwechselforschung Hormones et metabolisme 48 (7):417–426. https://doi.org/10.1055/s-0042-105748
Adamsson V, Reumark A, Cederholm T, Vessby B, Riserus U, Johansson G (2012) What is a healthy Nordic diet? Foods and nutrients in the NORDIET study. Food Nutr Res 56:18189. https://doi.org/10.3402/fnr.v56i0.18189
Hansen CP, Overvad K, Kyro C, Olsen A, Tjonneland A, Johnsen SP, Jakobsen MU, Dahm CC (2017) Adherence to a healthy Nordic diet and risk of stroke: a Danish cohort study. Stroke. https://doi.org/10.1161/STROKEAHA.116.015019
Lacoppidan SA, Kyro C, Loft S, Helnaes A, Christensen J, Hansen CP, Dahm CC, Overvad K, Tjonneland A, Olsen A (2015) Adherence to a healthy Nordic food index is associated with a lower risk of type-2 diabetes—the Danish diet, cancer and health cohort study. Nutrients 7(10):8633–8644. https://doi.org/10.3390/nu7105418
Roswall N, Sandin S, Löf M, Skeie G, Olsen A, Adami HO, Weiderpass E (2015) Adherence to the healthy Nordic food index and total and cause-specific mortality among Swedish women. Eur J Epidemiol 30(6):509–517. https://doi.org/10.1007/s10654-015-0021-x
Roswall N, Sandin S, Scragg R, Löf M, Skeie G, Olsen A, Adami HO, Weiderpass E (2015) No association between adherence to the healthy Nordic food index and cardiovascular disease amongst Swedish women: a cohort study. J Intern Med 278(5):531–541. https://doi.org/10.1111/joim.12378
Roswall N, Li YJ, Kyro C, Sandin S, Lof M, Adami HO, Weiderpass E (2015) No association between adherence to a healthy Nordic food index and colorectal cancer: results from a Swedish cohort study. Cancer Epidemiol Biomark Prev 24(4):755–757. https://doi.org/10.1158/1055-9965.epi-14-1314
Lankinen M, Kolehmainen M, Jaaskelainen T, Paananen J, Joukamo L, Kangas AJ, Soininen P, Poutanen K, Mykkanen H, Gylling H, Oresic M, Jauhiainen M, Ala-Korpela M, Uusitupa M, Schwab U (2014) Effects of whole grain, fish and bilberries on serum metabolic profile and lipid transfer protein activities: a randomized trial (sysdimet). PLoS One 9(2):e90352. https://doi.org/10.1371/journal.pone.0090352
Poulsen SK, Due A, Jordy AB, Kiens B, Stark KD, Stender S, Holst C, Astrup A, Larsen TM (2014) Health effect of the new nordic diet in adults with increased waist circumference: a 6-mo randomized controlled trial. Am J Clin Nutr 99(1):35–45. https://doi.org/10.3945/ajcn.113.069393
Ramezani-Jolfaie N, Salehi-Abargouei A, Mohammadi M (2017) Effects of Nordic diet on lipid profile and blood pressure in adults: a systematic review and meta-analysis of clinical trials. PROSPERO [Internet]. [cited 2017 Jan 4]: CRD42017054096. http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017054096. Accessed 9 Aug 2018
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100
Becker W, Lyhne N, Pedersen AN, Aro A, Fogelholm M, Phorsdottir I, Alexander J, Anderssen SA, Meltzer HM, Pedersen JI (2004) Nordic nutrition recommendations 2004—integrating nutrition and physical activity. Scand J Nutr 48(4):178–187. https://doi.org/10.1080/1102680410003794
Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration, London. http://www.cochrane-handbook.org.
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558. https://doi.org/10.1002/sim.1186
Egger M, Davey-Smith G, Altman D (2008) Systematic reviews in health care: meta-analysis in context. Wiley, Hoboken
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Damsgaard CT, Ritz C, Dalskov SM, Landberg R, Stark KD, Biltoft-Jensen A, Tetens I, Astrup A, Michaelsen KF, Lauritzen L (2016) Associations between school meal-induced dietary changes and metabolic syndrome markers in 8–11-year-old Danish children. Eur J Nutr 55(5):1973–1984. https://doi.org/10.1007/s00394-015-1013-z
Thorsen AV, Lassen AD, Andersen EW, Christensen LM, Biltoft-Jensen A, Andersen R, Damsgaard CT, Michaelsen KF, Tetens I (2015) Plate waste and intake of school lunch based on the new Nordic diet and on packed lunches: a randomised controlled trial in 8- to 11-year-old Danish children. J Nutr Sci. https://doi.org/10.1017/jns.2015.3
Sorensen LB, Dyssegaard CB, Damsgaard CT, Petersen RA, Dalskov SM, Hjorth MF, Andersen R, Tetens I, Ritz C, Astrup A, Lauritzen L, Michaelsen KF, Egelund N (2015) The effects of Nordic school meals on concentration and school performance in 8- to 11-year-old children in the OPUS School Meal Study: a cluster-randomised, controlled, cross-over trial. Br J Nutr 113(8):1280–1291. https://doi.org/10.1017/S0007114515000033
Sorensen LB, Damsgaard CT, Dalskov SM, Petersen RA, Egelund N, Dyssegaard CB, Stark KD, Andersen R, Tetens I, Astrup A, Michaelsen KF, Lauritzen L (2015) Diet-induced changes in iron and n-3 fatty acid status and associations with cognitive performance in 8–11-year-old Danish children: secondary analyses of the Optimal Well-Being, Development and Health for Danish Children through a Healthy New Nordic Diet School Meal Study. Br J Nutr 114(10):1623–1637. https://doi.org/10.1017/S0007114515003323
Petersen RA, Damsgaard CT, Dalskov SM, Sorensen LB, Hjorth MF, Andersen R, Tetens I, Krarup H, Ritz C, Astrup A, Michaelsen KF, Molgaard C (2015) Effects of school meals with weekly fish servings on vitamin D status in Danish children: secondary outcomes from the OPUS (Optimal well-being, development and health for Danish children through a healthy New Nordic Diet) School Meal Study. J Nutr Sci. https://doi.org/10.1017/jns.2015.15
Biltoft-Jensen A, Damsgaard CT, Andersen R, Ygil KH, Andersen EW, Ege M, Christensen T, Sorensen LB, Stark KD, Tetens I, Thorsen AV (2015) Accuracy of self-reported intake of signature foods in a school meal intervention study: comparison between control and intervention period. Br J Nutr 114(4):635–644. https://doi.org/10.1017/S0007114515002020
Andersen R, Biltoft-Jensen A, Andersen EW, Ege M, Christensen T, Ygil KH, Thorsen AV, Damsgaard CT, Astrup A, Michaelsen KF, Tetens I (2015) Effects of school meals based on the New Nordic Diet on intake of signature foods: a randomised controlled trial. the OPUS School Meal Study. Br J Nutr 114(5):772–779. https://doi.org/10.1017/S0007114515002299
Damsgaard CT, Dalskov SM, Laursen RP, Ritz C, Hjorth MF, Lauritzen L, Sorensen LB, Petersen RA, Andersen MR, Stender S, Andersen R, Tetens I, Molgaard C, Astrup A, Michaelsen KF (2014) Provision of healthy school meals does not affect the metabolic syndrome score in 8–11-year-old children, but reduces cardiometabolic risk markers despite increasing waist circumference. Br J Nutr 112(11):1826–1836. https://doi.org/10.1017/s0007114514003043
Andersen R, Biltoft-Jensen A, Christensen T, Andersen EW, Ege M, Thorsen AV, Dalskov SM, Damsgaard CT, Astrup A, Michaelsen KF, Tetens I (2014) Dietary effects of introducing school meals based on the New Nordic Diet—a randomised controlled trial in Danish children. The OPUS School Meal Study. Br J Nutr 111(11):1967–1976. https://doi.org/10.1017/S0007114514000634
Damsgaard CT, Dalskov SM, Petersen RA, Sorensen LB, Molgaard C, Biltoft-Jensen A, Andersen R, Thorsen AV, Tetens I, Sjodin A, Hjorth MF, Vassard D, Jensen JD, Egelund N, Dyssegaard CB, Skovgaard I, Astrup A, Michaelsen KF (2012) Design of the OPUS School Meal Study: a randomised controlled trial assessing the impact of serving school meals based on the New Nordic Diet. Scand J Public Health 40(8):693–703. https://doi.org/10.1177/1403494812463173
Salomo L, Poulsen SK, Rix M, Kamper AL, Larsen TM, Astrup A (2016) The New Nordic Diet: phosphorus content and absorption. Eur J Nutr 55(3):991–996. https://doi.org/10.1007/s00394-015-0913-2
Leder L, Kolehmainen M, Narverud I, Dahlman I, Myhrstad MCW, De Mello VD, Paananen J, Carlberg C, Schwab U, Herzig KH, Cloetens L, Storm MU, Hukkanen J, Savolainen MJ, Rosqvist F, Hermansen K, Dragsted LO, Ingibjörg G, Thorsdottir I, Risérus U, Åkesson B, Thoresen M, Arner P, Poutanen KS, Uusitupa M, Holven KB, Ulven SM (2016) Effects of a healthy Nordic diet on gene expression changes in peripheral blood mononuclear cells in response to an oral glucose tolerance test in subjects with metabolic syndrome: a SYSDIET sub-study. Genes Nutr. https://doi.org/10.1186/s12263-016-0521-4
Lankinen M, Schwab U, Kolehmainen M, Paananen J, Nygren H, Seppänen-Laakso T, Poutanen K, Hyötyläinen T, Risérus U, Savolainen MJ, Hukkanen J, Brader L, Marklund M, Rosqvist F, Hermansen K, Cloetens L, Önning G, Thorsdottir I, Gunnarsdottir I, Åkesson B, Dragsted LO, Uusitupa M, Orešič M (2016) A healthy Nordic diet alters the plasma lipidomic profile in adults with features of metabolic syndrome in a multicenter randomized dietary intervention. J Nutr 146(4):662–672. https://doi.org/10.3945/jn.115.220459
Khakimov B, Poulsen SK, Savorani F, Acar E, Gürdeniz G, Larsen TM, Astrup A, Dragsted LO, Engelsen SB (2016) New nordic diet versus average Danish diet: a randomized controlled trial revealed healthy long-term effects of the new nordic diet by GC-MS blood plasma metabolomics. J Proteome Res 15(6):1939–1954. https://doi.org/10.1021/acs.jproteome.6b00109
Cuparencu CS, Andersen MBS, Gürdeniz G, Schou SS, Mortensen MW, Raben A, Astrup A, Dragsted LO (2016) Identification of urinary biomarkers after consumption of sea buckthorn and strawberry, by untargeted LC–MS metabolomics: a meal study in adult men. Metabolomics 12(2):1–20. https://doi.org/10.1007/s11306-015-0934-0
Hanhineva K, Lankinen MA, Pedret A, Schwab U, Kolehmainen M, Paananen J, de Mello V, Sola R, Lehtonen M, Poutanen K, Uusitupa M, Mykkanen H (2015) Nontargeted metabolite profiling discriminates diet-specific biomarkers for consumption of whole grains, fatty fish, and bilberries in a randomized controlled trial. J Nutr 145(1):7–17. https://doi.org/10.3945/jn.114.196840
Roager HM, Licht TR, Poulsen SK, Larsen TM, Bahl MI (2014) Microbial enterotypes, inferred by the Prevotella-to-Bacteroides ratio, remained stable during a 6-month randomized controlled diet intervention with the New Nordic Diet. Appl Environ Microbiol 80(3):1142–1149. https://doi.org/10.1128/aem.03549-13
Brader L, Rejnmark L, Carlberg C, Schwab U, Kolehmainen M, Rosqvist F, Cloetens L, Landin-Olsson M, Gunnarsdottir I, Poutanen KS, Herzig KH, Risérus U, Savolainen MJ, Thorsdottir I, Uusitupa M, Hermansen K (2014) Effects of a healthy Nordic diet on plasma 25-hydroxyvitamin D concentration in subjects with metabolic syndrome: a randomized, placebo-controlled trial (SYSDIET). Eur J Nutr 53(4):1123–1134. https://doi.org/10.1007/s00394-014-0674-3
Andersen MBS, Rinnan A, Manach C, Poulsen SK, Pujos-Guillot E, Larsen TM, Astrup A, Dragsted LO (2014) Untargeted metabolomics as a screening tool for estimating compliance to a dietary pattern. J Proteome Res 13(3):1405–1418. https://doi.org/10.1021/pr400964s
Adamsson V, Cederholm T, Vessby B, Riserus U (2014) Influence of a healthy Nordic diet on serum fatty acid composition and associations with blood lipoproteins—results from the NORDIET study. Food Nutr Res. https://doi.org/10.3402/fnr.v58.24114
Jobs E, Adamsson V, Larsson A, Jobs M, Nerpin E, Ingelsson E, Arnlov J, Riserus U (2014) Influence of a prudent diet on circulating cathepsin S in humans. Nutr J 13:84. https://doi.org/10.1186/1475-2891-13-84
Magnusdottir OK, Landberg R, Gunnarsdottir I, Cloetens L, Akesson B, Onning G, Jonsdottir SE, Rosqvist F, Schwab U, Herzig KH, Savolainen MJ, Brader L, Hermansen K, Kolehmainen M, Poutanen K, Uusitupa M, Thorsdottir I, Riserus U (2013) Plasma alkylresorcinols reflect important whole-grain components of a healthy Nordic diet. J Nutr 143(9):1383–1390. https://doi.org/10.3945/jn.113.175588
Huseinovic E, Bertz F, Agelii ML, Johansson EH, Winkvist A, Brekke HK (2016) Effectiveness of a weight loss intervention in postpartum women: results from a randomized controlled trial in primary health care. Am J Clin Nutr 104(2):362–370. https://doi.org/10.3945/ajcn.116.135673
Kolehmainen M, Ulven SM, Paananen J, De Mello V, Schwab U, Carlberg C, Myhrstad M, Pihlajamäki J, Dungner E, Sjöolin E, Gunnarsdottir I, Cloetens L, Landin-Olsson M, Akesson B, Rosqvist F, Hukkanen J, Herzig KH, Dragsted LO, Savolainen MJ, Brader L, Hermansen K, Risérus U, Thorsdottir I, Poutanen KS, Uusitupa M, Arner P, Dahlman I (2015) Healthy Nordic diet downregulates the expression of genes involved in inflammation in subcutaneous adipose tissue in individuals with features of the metabolic syndrome. Am J Clin Nutr 101(1):228–239. https://doi.org/10.3945/ajcn.114.092783
Boraxbekk CJ, Stomby A, Ryberg M, Lindahl B, Larsson C, Nyberg L, Olsson T (2015) Diet-induced weight loss alters functional brain responses during an episodic memory task. Obes Facts 8:261–272. https://doi.org/10.1159/000437157
Poulsen S, Frost S, Rasmussen L, Astrup A, Larsen T (2011) Weight loss after 12 weeks with new Nordic diet vs. average Danish diet provided ad libitum—a randomized controlled trial using the shop model. Ann Nutr Metab 58:289–289
De Mello VDF, Schwab U, Kolehmainen M, Koenig W, Siloaho M, Poutanen K, Mykkänen H, Uusitupa M (2011) A diet high in fatty fish, bilberries and wholegrain products improves markers of endothelial function and inflammation in individuals with impaired glucose metabolism in a randomised controlled trial: the Sysdimet study. Diabetologia 54(11):2755–2767. https://doi.org/10.1007/s00125-011-2285-3
Chorell E, Ryberg M, Larsson C, Sandberg S, Mellberg C, Lindahl B, Antti H, Olsson T (2016) Plasma metabolomic response to postmenopausal weight loss induced by different diets. Metabolomics 12(5):85. https://doi.org/10.1007/s11306-016-1013-x
Marklund M, Magnusdottir OK, Rosqvist F, Cloetens L, Landberg R, Kolehmainen M, Brader L, Hermansen K, Poutanen KS, Herzig KH, Hukkanen J, Savolainen MJ, Dragsted LO, Schwab U, Paananen J, Uusitupa M, Åkesson B, Thorsdottir I, Risérus U (2014) A dietary biomarker approach captures compliance and cardiometabolic effects of a healthy nordic diet in individuals with metabolic syndrome. J Nutr 144(10):1642–1649. https://doi.org/10.3945/jn.114.193771
Marckmann P, Sandstrom B, Jespersen J (1995) [Food intake of Danes and cardiac risk factors]. Ugeskr Laeger 157(12):1667–1671
Brader L, Uusitupa M, Dragsted LO, Hermansen K (2014) Effects of an isocaloric healthy Nordic diet on ambulatory blood pressure in metabolic syndrome: a randomized SYSDIET sub-study. Eur J Clin Nutr 68(1):57–63. https://doi.org/10.1038/ejcn.2013.192
Fritzen AM, Lundsgaard AM, Jordy AB, Poulsen SK, Stender S, Pilegaard H, Astrup A, Larsen TM, Wojtaszewski JFP, Richter EA, Kiens B (2015) New nordic diet-induced weight loss is accompanied by changes in metabolism and AMPK signaling in adipose tissue. J Clin Endocrinol Metab 100(9):3509–3519. https://doi.org/10.1210/jc.2015-2079
Marckmann P, Sandström B, Jespersen J (1994) Low-fat, high-fiber diet favorably affects several independent risk markers of ischemic heart disease: observations on blood lipids, coagulation, and fibrinolysis from a trial of middle-aged Danes. Am J Clin Nutr 59(4):935–939
Ulven SM, Leder L, Elind E, Ottestad I, Christensen JJ, Telle-Hansen VH, Skjetne AJ, Raael E, Sheikh NA, Holck M, Torvik K, Lamglait A, Thyholt K, Byfuglien MG, Granlund L, Andersen LF, Holven KB (2016) Exchanging a few commercial, regularly consumed food items with improved fat quality reduces total cholesterol and LDL-cholesterol: a double-blind, randomised controlled trial. Br J Nutr 116:1–11. https://doi.org/10.1017/S0007114516003445
Adamsson V, Reumark A, Marklund M, Larsson A, Riserus U (2015) Role of a prudent breakfast in improving cardiometabolic risk factors in subjects with hypercholesterolemia: a randomized controlled trial. Clin Nutr 34(1):20–26. https://doi.org/10.1016/j.clnu.2014.04.009
Magnusdottir OK, Landberg R, Gunnarsdottir I, Cloetens L, Akesson B, Rosqvist F, Schwab U, Herzig KH, Hukkanen J, Savolainen MJ, Brader L, Hermansen K, Kolehmainen M, Poutanen K, Uusitupa M, Riserus U, Thorsdottir I (2014) Whole grain rye intake, reflected by a biomarker, is associated with favorable blood lipid outcomes in subjects with the metabolic syndrome—a randomized study. PLoS One 9(10):e110827. https://doi.org/10.1371/journal.pone.0110827
Magnusdottir OK, Landberg R, Gunnarsdottir I, Cloetens L, Akesson B, Landin-Olsson M, Rosqvist F, Iggman D, Schwab U, Herzig KH, Savolainen MJ, Brader L, Hermansen K, Kolehmainen M, Poutanen K, Uusitupa M, Thorsdottir I, Risérus U (2014) Plasma alkylresorcinols C17:0/C21:0 ratio, a biomarker of relative whole-grain rye intake, is associated to insulin sensitivity: a randomized study. Eur J Clin Nutr 68(4):453–458. https://doi.org/10.1038/ejcn.2014.12
Mellberg C, Sandberg S, Ryberg M, Eriksson M, Brage S, Larsson C, Olsson T, Lindahl B (2014) Long-term effects of a palaeolithic-type diet in obese postmenopausal women: a 2-year randomized trial. Eur J Clin Nutr 68(3):350–357. https://doi.org/10.1038/ejcn.2013.290
Darwiche G, Höglund P, Roth B, Larsson E, Sjöberg T, Wohlfart B, Steen S, Ohlsson B (2016) An Okinawan-based Nordic diet improves anthropometry, metabolic control, and health-related quality of life in Scandinavian patients with type 2 diabetes: a pilot trial. Food Nutr Res 60:32594. https://doi.org/10.3402/fnr.v60.32594
Goswami B, Rajappa M, Mallika V, Kumar S, Shukla DK (2008) Apo-B/apo-AI ratio: a better discriminator of coronary artery disease risk than other conventional lipid ratios in Indian patients with acute myocardial infarction. Acta Cardiol 63(6):749–755
Uche E, Adediran A, Damulak O, Adeyemo T, Akinbami A, Akanmu A (2013) Lipid profile of regular blood donors. J Blood Med 4:39–42. https://doi.org/10.2147/JBM.S42211
Mithril C, Dragsted LO, Meyer C, Tetens I, Biltoft-Jensen A, Astrup A (2013) Dietary composition and nutrient content of the New Nordic Diet. Public Health Nutr 16(5):777–785. https://doi.org/10.1017/S1368980012004521
Kanerva N, Kaartinen NE, Rissanen H, Knekt P, Eriksson JG, Saaksjarvi K, Sundvall J, Mannisto S (2014) Associations of the Baltic Sea diet with cardiometabolic risk factors—a meta-analysis of three Finnish studies. Br J Nutr 112(4):616–626. https://doi.org/10.1017/s0007114514001159
Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM (2003) Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension 42(5):878–884. https://doi.org/10.1161/01.HYP.0000094221.86888.AE
Adler AJ, Taylor F, Martin N, Gottlieb S, Taylor RS, Ebrahim S (2014) Reduced dietary salt for the prevention of cardiovascular disease. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD009217.pub3
Hu FB, Willett WC (2002) Optimal diets for prevention of coronary heart disease. JAMA 288(20):2569–2578
Altorf-van der Kuil W, Engberink MF, Brink EJ, van Baak MA, Bakker SJ, Navis G, van ‘t Veer P, Geleijnse JM (2010) Dietary protein and blood pressure: a systematic review. PLoS One 5(8):e12102. https://doi.org/10.1371/journal.pone.0012102
Rebholz CM, Friedman EE, Powers LJ, Arroyave WD, He J, Kelly TN (2012) Dietary protein intake and blood pressure: a meta-analysis of randomized controlled trials. Am J Epidemiol 176(Suppl 7):S27–S43. https://doi.org/10.1093/aje/kws245
Nissensohn M, Roman-Vinas B, Sanchez-Villegas A, Piscopo S, Serra-Majem L (2016) The effect of the mediterranean diet on hypertension: a systematic review and meta-analysis. J Nutri Educ Behav 48(1):42–53 e41. https://doi.org/10.1016/j.jneb.2015.08.023
Brown L, Rosner B, Willett WW, Sacks FM (1999) Cholesterol-lowering effects of dietary fiber: a meta-analysis. Am J Clin Nutr 69(1):30–42
Vega-Lopez S, Ausman LM, Jalbert SM, Erkkila AT, Lichtenstein AH (2006) Palm and partially hydrogenated soybean oils adversely alter lipoprotein profiles compared with soybean and canola oils in moderately hyperlipidemic subjects. Am J Clin Nutr 84(1):54–62
Baxheinrich A, Stratmann B, Lee-Barkey YH, Tschoepe D, Wahrburg U (2012) Effects of a rapeseed oil-enriched hypoenergetic diet with a high content of alpha-linolenic acid on body weight and cardiovascular risk profile in patients with the metabolic syndrome. Br J Nutr 108(4):682–691. https://doi.org/10.1017/s0007114512002875
Pedersen A, Baumstark MW, Marckmann P, Gylling H, Sandstrom B (2000) An olive oil-rich diet results in higher concentrations of LDL cholesterol and a higher number of LDL subfraction particles than rapeseed oil and sunflower oil diets. J Lipid Res 41(12):1901–1911
Obarzanek E, Sacks FM, Vollmer WM, Bray GA, Miller ER 3rd, Lin PH, Karanja NM, Most-Windhauser MM, Moore TJ, Swain JF, Bales CW, Proschan MA, Group DR (2001) Effects on blood lipids of a blood pressure-lowering diet: the Dietary Approaches to Stop Hypertension (DASH) Trial. Am J Clin Nutr 74(1):80–89
Funding
The study was funded by Nutrition and Food Security research center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
Author information
Authors and Affiliations
Contributions
ASA, NRJ and MM developed the study concept and designed the research; NRJ and MM wrote the protocol and conducted the electronic searches and study selection; NRJ and MM conducted data extraction and tabulated data; ASA and NRJ conducted the data analysis and interpretation of results; NRJ and ASA wrote the first draft of the manuscript; and all authors read and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest to report for this study.
Rights and permissions
About this article
Cite this article
Ramezani-Jolfaie, N., Mohammadi, M. & Salehi-Abargouei, A. The effect of healthy Nordic diet on cardio-metabolic markers: a systematic review and meta-analysis of randomized controlled clinical trials. Eur J Nutr 58, 2159–2174 (2019). https://doi.org/10.1007/s00394-018-1804-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-018-1804-0