Abstract
Purpose
To analyze the presence of total IgA and anti-gliadin antibodies (AGA) in BM from CD mothers who follow a gluten-free diet (GFD) and from mothers on a normal gluten-containing diet (ND).
Methods
218 samples of mature milk were obtained at different months of lactation (1–6) from 83 mothers (2 or more samples per mother) from Italy (Naples), The Netherlands (Leiden) and Spain (Madrid, Valencia and Reus): 42 CD mothers on GFD for more than 2 years and 41 non-CD mothers on a ND. Whey samples were analyzed for AGA-IgA by an indirect homemade ELISA and for total IgA (g/L) by a commercial ELISA kit.
Results
AGA-IgA was detected in BM, both in mothers on a GFD and mothers on a ND. AGA-IgA levels in both groups of mothers, CD and non-CD, show the same trend towards decreasing slightly along the months of lactation (p = 0.91). A different trend is observed for total IgA levels, decreasing markedly in CD mothers from the first month of lactation onwards but remaining stable in non-CD mothers (p = 0.048). A statistically significant association was found between the means of total IgA and AGA-IgA (p < 0.001).
Conclusion
AGA-IgA is present in BM from mothers on a ND as well as in BM from mothers who had been on a GFD for years. This reflects the existence of a long-lasting immunological memory independent of the mother’s diet. If the presence of these antibodies has any role in promoting the acquisition of gluten tolerance in the infant, our study shows that children of CD mothers would be on equal conditions as children of non-CD mothers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast milk (BM) contains not only nutrients necessary for the infants’ development, but also numerous bioactive factors such as enzymes, hormones, growth factors, cytokine, antimicrobial factors such as secretory IgA and oligosaccharides and specific food antibodies. It has been shown that BM antibodies against dietary proteins may modify the immune responses in the gut of young infants [1]. The relationship between maternal diet and antibody levels against food antigens in BM is contradictory [2,3,4,5]. BM has a complex composition and fat as well as protein content can interfere with the detection of specific antibodies, thus accounting for some discrepancies in reported studies. Additionally, according to different authors, antibodies concentration is not only influenced by recent mothers’ diet but can also reflect the mothers’ intestinal antigenic experience [4, 6].
Related to celiac disease (CD), retrospective observational studies suggested that breastfeeding may confer some protection against CD development and prolonged breastfeeding has been associated with a decreased incidence of CD in children [7,8,9,10]. However, a recent published meta-analysis, including prospective observational studies [11, 12] found no evidence of a protective effect of breastfeeding against the development of CD during childhood [13]. Still, these studies have all been at group level.
The relationship between the gluten and antibodies against gluten in BM and the development of CD in children has been hardly investigated. The only available studies in the field, have indeed found gliadin fractions of gluten and anti-gliadin antibodies (AGA) in BM of women on a gluten-containing diet [2, 14, 15]. However, the results about gliadin in BM are discrepant and difficult to interpret [16]. In addition, there are no published studies about AGA in BM of celiac mothers following a gluten-free diet (GFD).
Therefore the aim of our study is to determine the presence of AGA in BM samples in CD and non-CD mothers in the PreventCD trial (http://www.preventcd.com) and to assess the possible impact of GFD on AGA content in BM. In addition, we aimed to prospectively evaluate the relationship among AGA levels in BM and CD development in the offspring of the participating mothers. Additionally, as there is not a standardized method to analyze AGA in BM, we developed a specific in house method for this purpose.
Methods
Subjects
Infants with a high risk to develop CD were enrolled in the PreventCD study; a prospective, randomized, double-blind, placebo-controlled, dietary intervention performed from 2007 to 2010 in eight European countries to study the effect of the time of dietary gluten introduction on the risk to develop CD [11, 17]. Data collection, anthropometric measurements and blood collection in infants were as previously reported [18]. PreventCD participants had at least one first-degree family member with CD confirmed by small-bowel biopsy, and were HLA-DQ2 or HLA-DQ8 positive, or otherwise carrying the allele DQB1*02 [17]. Premature infants or infants with syndromes associated with an increased risk of CD, such as trisomy 21 or Turner’s syndrome, were excluded. In the PreventCD study, milk samples were donated by mothers with and without CD. Mothers were asked to express milk manually or by pump at the end of lactation, once a month during the first 6 months after birth. The milk samples were frozen at −20 °C in the home freezer and brought to the project site within 7 days to be stored at −80 °C until analysis. All women had delivered at term between week 37 and 42 of gestation. As the PreventCD cohort is still being followed up, for the purpose of this study, monitoring and data collection were closed on the 30th October 2014 when all children of the cohort had reached 4 years of age. The PreventCD study was approved by the medical ethics committee at each participating center and complied with Good Clinical Practice guidelines (ICH-GCP) regulations. The study was conducted according to the Declaration of Helsinki and registered at Current Controlled Trials (ICTRP CTRP NTR890). Participants signed a written informed consent which was an essential requirement for enrollment into the study.
Materials
The analyses reported here are based on the subsample of CD mothers on a GFD as well as non-CD mothers on a gluten-containing diet from the PreventCD cohort from Spain (Valencia, Madrid, Reus), Italy and The Netherlands [11].
Only those mothers who had provided 2 or more BM samples at different months of lactation were included.
Breast milk samples preparation
Samples stored at −20 °C, were defrosted at 4 °C, and subsequently homogenized, aliquoted and stored at −80 °C. To avoid interference in the immunoassays with fat content and cellular elements, these were removed by centrifugation, milk samples being centrifuged at 10,000×g at 5 °C, for 12 min. The aqueous phase was carefully separated and used to perform the antibody studies.
Determination of total IgA
Quantification of total IgA: Total IgA (g/L) was measured in human milk whey using an ELISA kit from Bethyl Laboratories® following the manufacturer’s instructions. Whey samples were analyzed at a 1:12,000 dilution. The inter- and intra-assay coefficients of variation (CV) were <10%.
Determination of IgA class anti-gliadin antibodies
The presence of IgA class anti-gliadin antibodies (AGA-IgA) was tested by an indirect homemade enzyme linked immunosorbent assay (ELISA). Taking as a starting point previously published assays for AGA-IgA [2, 19] we performed a series of assays to optimize the different variables such as sample dilutions, blocking agents, different conjugates dilution, etc. (more details in Supplemental Material). We used an anti-alpha- chain (AGA-IgA) antibody. Random selected samples were used for the development and optimization of the method. Test results were highly reproducible between experiments and between duplicate samples: inter-assay CV was <12% and intra-assay <10%.
Flat-bottomed 96-well microplates (ELISA plate high binding, Greiner®) were coated with 100 µL/well of gliadin extracted from wheat flour Scoutt-66 [20] at a concentration of 0.1 mg/mL in carbonate–bicarbonate buffer (pH 9.6) and incubated at room temperature (RT) overnight. After washing 4 times with PBS, non-specific binding sites were blocked with 200 µL/well of 1% (v/v) bovine serum albumin (BSA) in PBS-Tween (0.05% (v/v) Tween-20; pH 7.4) for 1 h at RT followed by washing with PBS–BSA. Samples were diluted at 1:5 (v/v) in BSA 0.5% (v/v) in PBS-Tween and 100 µL/well of each sample was incubated 1 h at RT. After washing, rabbit anti-human IgA conjugated to alkaline phosphatase (Sigma®) at 1:50 in BSA 0.5% (v/v) in PBS-Tween was incubated (100 µL/well) for 30 min at RT. The assay was developed with 100 µL/well of a solution containing p-nitrophenyl phosphate (1 mg/mL; Sigma®) in substrate buffer (1 vol. carbonate–bicarbonate buffer and 1 vol. of distilled water, plus 2 M MgCl2). The reaction was stopped after 25 min with 100 µL/well of NaOH 0.3 M and the absorbance was determined at 405 nm using a microplate reader (Multiskan FC, Thermo Scientific®).
Each sample was analyzed in duplicate. A reference BM sample (Standard) was analyzed in every experiment and its value was used to normalize the results. The first and last row of wells was incubated with PBS–BSA as blanks.
The antibody concentration was calculated in Arbitrary Units (AU), referred to a Standard sample, selected during the standardization procedure (medium values), after subtracting the blanks (Supplemental material).
Statistical analysis
Data were summarized by median (1st–3rd quartile) in the case of continuous variables and by relative frequencies in the case of categorical variables. Linear mixed models were used to assess the association of AGA-IgA and total IgA with the variables month, diet and location. An interaction between month and diet was added to the models to allow for different evolutions in time for each diet group. Individuals were added to the model as a random factor to account for the repeated measures design. Association between Total IgA and AGA-IgA values was assessed using Pearson’s correlation. All statistical analyses and graphs were performed using R (version 3.1.2). P values <0.05 were considered statistically significant.
Results
BM Total IgA
In total 218 samples of mature milk—obtained not earlier than 2 weeks after delivery—from 41 mothers on a ND and from 42 CD mothers on a GFD; all CD mothers on a GFD had been following the diet for more than 2 years (Table 1), were analyzed. Moreover, samples collected during exclusive breastfeeding represent 87% of the CD mothers and 90% of non-celiac mothers’ samples. No women reported selective IgA deficiency. BM total IgA values varied between 0.3 and 1.4 g/L (trimmed range), median was 0.668 g/L, and 1st and 3rd quartile were 0.482 and 0.86 g/L, respectively. In general the content on BM IgA was similar in mothers on a ND or on a GFD. For mothers on ND median BM IgA was 0.679 g/L and 1st and 3rd quartile were 0.53 and 0.93 g/L and for mothers on GFD 0.657 g/L and 1st and 3rd quartile were 0.45 and 0.93 g/L. Only the Italian mothers on a ND had statistically higher BM IgA compared to those following a GFD (p = 0.027).
There is a statistically significant interaction between the GFD variable with the variable month (p = 0.048), this means that total IgA levels in both diet groups do not evolve equally over time. A different course of total IgA BM levels in CD mothers on a GFD and non-CD mothers on a ND is observed. There is a marked decrease in IgA BM content in CD mothers along the months of lactation, but in non-CD mothers on ND, the levels remain stable from the first month of lactation onwards (Fig. 1). This difference was not affected by the country of origin (p = 0.73) (Supplemental Fig. 1). There was no significant difference in BM total IgA levels between primiparous and multiparous mothers (p = 0.26).
BM AGA-IgA
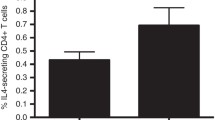
The content of AGA-IgA was similar in BM from mothers on GFD and mothers on ND (Table 1). No statistical significant differences were found between the different countries. In both groups of mothers BM AGA-IgA levels evolve similarly over time with a slightly decrease along the months of lactation (p = 0.91) (Fig. 2). This evolvement in BM AGA-IgA levels was similar in all the countries (p = 0.55) (Supplemental Fig. 2) and among primiparous and multiparous mothers (p = 0.21).
The variability of BM AGA-IgA values from different samples from the same mother (0.08) was significantly lower than the one between different mothers (0.33) (p < 0.001) (Fig. 3).
Variability of BM AGA-IgA concentration in samples from mothers on GFD (n = 112) and ND (n = 106). Each box represents data from one mother. Dashed lines represent first quartile, median and third quartile (all study samples). The graph shows that AGA-IgA values observed for each mother, represented as the spread within each box plot, are clearly less scattered than AGA-IgA values from different mother, represented as the spread between each box plot
Comparison of total IgA and AGA-IgA levels
Although in the majority of mothers, both total IgA and AGA-IgA, follow a similar longitudinal pattern, this is not the case in 36% of them. This phenomenon was independent of the mothers’ diet (data not shown).
Both in mothers on ND and on a GFD a significant association between the BM total IgA and AGA-IgA was found (p < 0.001) (Fig. 4).
Relationship between BM Total IgA and AGA levels and CD development
A total of 9 children from 83 mothers developed CD before 6 years of age, 3 children from Italy (2 from CD mothers and 1 from and non-CD mother) and 6 children from Spain (5 CD mothers and 1 non-CD). The BM total IgA and AGA levels were similar between the mothers whose children developed CD and those whose children did not develop the disease (Figs. 5, 6).
Discussion
In the present study, we have found that AGA are present in BM samples at different months of lactation both from CD mothers on a GFD and from non-CD mothers following a gluten-containing diet. Our findings show that diet is not a key factor influencing the presence of AGA in BM. Even if there is no exposure to the antigen (gliadin) during pregnancy, lactation and even in previous months and years, antibodies secretion still occurs in BM.
Previous studies have reported high levels of AGA-IgA in colostrum and BM in non-CD mothers which followed a gluten-containing diet [2, 5, 19, 21]. Ozcan et al. found that daily bread consumption in two groups with different socioeconomic status did not affect AGA levels in BM [5], but all the mothers consumed gluten at a greater or lesser extent. Our findings on decreasing AGA-IgA along the months of lactation are in agreement with those reported by Ozcan et al. within the first 45 days of lactation [5]. Moreover, our results in CD mothers on GFD are consistent with the findings of Mascart-Lemone in African mothers who did not consume bread or any other source of gluten [3]. Mothers with temporary exclusion of egg or cow’s milk proteins from their diet still secrete antibodies against these proteins in their BM and similar levels of these antibodies have been shown in colostrum from mothers on a restrictive diet and from mothers without dietary exclusions [2]. However, in these publications, the period of dietary restriction before BM sampling was about 3 months, which is shorter than the duration of GFD in our CD mothers. Other recent studies found casein and beta-lactoglobulin IgA in BM of mothers avoiding cow’s milk, but in this case lower levels of specific antibodies were found in mothers with restrictive diets as compared to those who consumed milk [22].
Our findings are in accordance with reports by Hanson [23] showing that memory lymphocytes migrate from the intestine to the mammary gland and that previous antigenic experiences of the mother are reflected in the broad spectrum of her milk antibodies [24]. Therefore, presence of AGA in BM samples from mothers on a GFD for years reflects the existence of a long-lasting immunological memory, independent of the mothers’ diet.
Although the celiac mothers in our study were following a GFD, we cannot exclude the possibility of dietary transgressions; however, we should take into account the high level of motivation of women with CD to adhere to the GFD during pregnancy and lactation. On the other hand, foods labeled as gluten-free products cannot exceed 20 ppm of gluten, but they may contain up to 19 ppm of gluten and these products may be consumed daily and in different amounts; therefore we could speculate that mothers on a strict GFD still ingest small amounts of gluten which are able to elicit an immunologic response and AGA production and secretion in BM and would, thus, explain similar AGA levels in CD and non-CD mothers. More research is needed to assess the minimal amount of gliadin needed to produce an antigenic stimulus both at serum as at BM level.
Moreover, mothers on a ND in our study have at least one family member diagnosed with CD; this may influence their diet, leading to less daily gluten consumption as compared to the general population [25, 26].
BM is rich in IgA, which is synthesized by resident B cells in the mammary glands that have migrated from the mother’s intestine. Attachment of dimeric IgA to a secretory component [22] allows secretory IgA to survive through the gastrointestinal tract, and provide passive immunoprotection against antigens of microorganisms and foods. According to the literature, in the early colostrum, secretory IgA appears in high concentration, but in mature milk levels are reduced to 0.5–1.5 g/L [23]. In our study, IgA levels (median: 0.67 g/L) in BM are similar to previous published data.
We found that the content on BM IgA was similar in CD and non-CD mothers. However, there is a marked tendency to a gradually decrease in CD mothers along the months, while it remains stable in non-CD mothers from the first month of lactation onwards; additional studies are needed to determine the reason and the potential relevance of this decrease. In previous studies, significantly lower levels of total and cow’s milk-specific IgA were found in colostrum and BM from mothers whose baby developed cow’s milk allergy [27]. A recent publication reported Spanish mothers with CD had lower S-IgA levels the first month of lactation compared to healthy mothers; the authors suggested a decrease in IgA concentrations in BM could reduce the infant’s mucosal protection and favor gluten intolerance [28]. However, our results are not directly comparable because our data are longitudinal, since we are measuring the evolution over time and Olivares et al. compares the data only at month 1 of lactation.
On the other hand, the association between total IgA and AGA levels in the two groups of mothers suggests that AGA production in BM depends on the same mechanism that regulates total IgA production by the mammary glands.
We found no relationship between the total IgA or AGA BM levels and the development of CD in the offspring, but as only 9 children developed CD during the study, the sample size is too small for a definitive statement.
In conclusion, AGA-IgA was present in BM of CD mothers following a GFD as well as in non-CD mothers on a ND. If the presence of these antibodies has any role in promoting the acquisition of gluten tolerance in the infant, our study shows that in this respect, children of CD mothers would be on equal conditions as children of non-CD mothers.
Abbreviations
- AGA:
-
Anti-gliadin antibodies
- CD:
-
Celiac disease
- BM:
-
Breast milk
- GFD:
-
Gluten-free diet
- ND:
-
Normal gluten containing diet
- AU:
-
Arbitrary units
- IgA:
-
Immunoglobulin A
References
MacGillivray DM, Kollmann TR (2014) The role of environmental factors in modulating immune responses in early life. Front Immunol 5:434
Fälth-Magnusson K (1989) Breast milk antibodies to foods in relation to maternal diet, maternal atopy and the development of atopic disease in the baby. Int Arch Allergy Appl Immunol 90(3):297–300
Mascart-Lemone F, Donnen P, Paluku B, Brasseur D, Van den Broeck J, Vaerman JP, Hennart P, Duchateau J (1991) Serum and breast milk antibodies to food antigens in African mothers and relation to their diet. Adv Exp Med Biol 310:201–206
Cruz JR, García B, Urrutia JJ, Carlsson B, Hanson LA (1981) Food antibodies in milk from Guatemalan women. J Pediatr 99(4):600–602
Ozcan T, Ozeke T, Meral A (2000) Gliadin-specific IgA antibodies in breast milk. J Int Med Res 28(5):234–240
Hanson LA (1998) Breastfeeding provides passive and likely long-lasting active immunity. Ann Allergy Asthma Immunol 81(6):523–533
Auricchio S, Follo D, de Ritis G, Giunta A, Marzorati D, Prampolini L, Ansaldi N, Levi P, Dall’Olio D, Bossi A et al (1983) Does breast feeding protect against the development of clinical symptoms of celiac disease in children? J Pediatr Gastroenterol Nutr 2(3):428–433
Greco L, Auricchio S, Mayer M, Grimaldi M (1988) Case control study on nutritional risk factors in celiac disease. J Pediatr Gastroenterol Nutr 7(3):395–399
Stevens FM, Egan-Mitchell B, Cryan E, McCarthy CF, McNicholl B (1986) Decreasing incidence of coeliac disease. Arch Dis Child 62(5):465–468
Agostoni C, Decsi T, Fewtrell M, Goulet O, Kolacek S, Koletzko B, Michaelsen KF, Moreno L, Puntis J, Rigo J, Shamir R, Szajewska H, Turck D, van Goudoever J, ESPGHAN Committee on Nutrition (2008) Complementary feeding: a commentary by the ESPGHAN Committee on Nutrition. J Pediatr Gastroenterol Nutr 46(1):99–110
Vriezinga SL, Auricchio R, Bravi E, Castillejo G, Chmielewska A, Crespo Escobar P, Kolaček S, Koletzko S, Korponay-Szabo IR, Mummert E et al (2014) Randomized feeding Intervention in infants at high risk for celiac disease. N Engl J Med 371(14):1304–1315. doi:10.1056/NEJMoa1404172
Lionetti E, Castellaneta S, Francavilla R, Pulvirenti A, Tonutti E, Amarri S, Barbato M, Barbera C, Barera G, Bellantoni A et al (2014) Introduction of gluten, HLA status, and the risk of celiac disease in children. N Engl J Med 371(14):1295–1303. doi:10.1056/NEJMoa1400697
Szajewska H, Shamir R, Chmielewska A, Pieścik-Lech M, Auricchio R, Ivarsson A, Kolacek S, Koletzko S, Korponay-Szabo I, Mearin ML, PREVENTCD Study Group et al (2015) Systematic review with meta-analysis: early infant feeding and coeliac disease-update 2015. Aliment Pharmacol Ther 41(11):1038–1054
Troncone R, Scarcella A, Donatiello A, Cannataro P, Tarabuso A, Auricchio S (1987) Passage of gliadin into human breast milk. Acta Paediatr Scand 76(3):453–456
Chirdo FG, Rumbo M, Añón MC, Fossati CA (1998) Presence of high levels of non-degraded gliadin in breast milk from healthy mothers. Scand J Gastroenterol 33(11):1186–1192
Mena MC, Lombardía M, Roca M, Ribes-Koninckx C, Albar JP (2013) Analysis of gluten in human milk samples in coeliac and non-coeliac mothers. Proceedings of the 26th Meeting of the Working Group on Prolamin analysis and toxicity. Verlag Wissenschaftliche Scripten, Leuven, pp 39–44. ISBN 978-3-938896-66-2
Hogen Esch CE, Rosén A, Auricchio R, Romanos J, Chmielewska A, Putter H, Ivarsson A, Szajewska H, Koning F, Wijmenga C et al (2010) The PreventCD Study design: towards new strategies for the prevention of coeliac disease. Eur J Gastroenterol Hepatol 22(12):1424–1430
Vriezinga SL, Farih N, van der Meulen-de Jong AE, Putter H, Rings EH, Schaart MW, Schweizer JJ, Wessels MM, Mearin ML (2016) A comparison of patients’ and doctors’ reports on health related quality of life in celiac disease. J Pediatr Gastroenterol Nutr 64(5):737–741 (Epub ahead of print)
Rumbo M, Chirdo FG, Añón MC, Fossati CA (1998) Detection and characterization of antibodies specific to food antigens (gliadin, ovalbumin and beta-lactoglobulin) in human serum, saliva, colostrum and milk. Clin Exp Immunol 112(3):453–458
Ribes Koninckx CR, Giliams JP, Polanco I, Peña AS (1984) IgA antigliadin antibodies in celiac and inflammatory bowel disease. J Pediatr Gastroenterol Nutr 3(5):676–682
Juto P, Holm S (1992) Gliadin-specific and cow’s milk protein-specific IgA in human milk. J Pediatr Gastroenterol Nutr 15(2):159–162
Järvinen KM, Westfall JE, Seppo MS, James AK, Tsuang AJ, Feustel PJ, Sampson HA, Berin C (2014) Role of maternal elimination diets and human milk IgA in the development of cow’s milk allergy in the infants. Clin Exp Allergy 44(1):69–78
Hanson LA, Korotkova M (2002) The role of breastfeeding in prevention of neonatal infection. Semin Neonatol 7(4):275–278
Hanson LA, Dahlman-Höglund A, Karlsson M, Lundin S, Dahlgren U, Telemo E (1999) Normal microbial flora of the gut and the immune system. Probiotics, other nutritional factors and intestinal microflora, 42nd edn. Lippincott-Raven, Philadelphia, pp 217–228
van Overbeek FM, Uil-Dieterman IG, Mol IW, Köhler-Brands L, Heymans HS, Mulder CJ (1997) The daily gluten intake in relatives of patients with coeliac disease compared with that of the general Dutch population. Eur J Gastroenterol Hepatol 9(11):1097–1099
Lerma JC, Escobar PC, Simo EM, Aliaga ED, Miguel BP, Ribes-Koninckx C (2014) Low gluten consumption by young children from families with a history of coeliac disease. J Pediatr Gastroenterol Nutr 58(5):e50
Järvinen KM, Laine ST, Järvenpää AL, Suomalainen HK (2000) Does low IgA in human milk predispose the infant to development of cow’s milk allergy? Pediatr Res 48(4):456–457
Olivares M, Albrecht S, De Palma G, Ferrer MD, Castillejo G, Schols HA, Sanz Y (2015) Human milk composition differs in healthy mothers and mothers with celiac disease. Eur J Nutr 54(1):119–128
Acknowledgements
We thank all the families who participated in this study. We are very grateful to Dr. Amado Salvador Peña for his critical revision of the manuscript. We are also grateful to Miguel Bolonio (Medical Research Institute La Fe) for his useful discussions. Supported by Grants from the European Commission (FP6-2005-FOOD-4B-36383–PREVENTCD), and a Grant of the Spanish Ministry of Health: FIS PS09/01056 Factores ambientales de riesgo asociados a la Enfermedad Celiaca y otras Enfermedades Autoinmunes en población con susceptibilidad genética, Eurospital, Fondazione Celiachia, Fria Bröd, Instituto de Salud Carlos III, Spanish Society for Pediatric Gastroenterology, Hepatology, and Nutrition, Stichting Coeliakie Onderzoek Nederland, Thermo Fisher Scientific, the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition The funding organizations have no role in the conception, design, or conduct of the study, in the analysis or interpretation of the data, or in the writing of the manuscript or the decision to submit it for publication. Author who received GRANTs: MLM, SLV, IP, CRK.
Author information
Authors and Affiliations
Consortia
Contributions
Ms. Roca had full access to all the data in the study and has taken responsibility for the integrity of the data and the accuracy of the data analysis. MR, MLM and CRK contributed to the study concept and design; MR conducted the research work, SLV, PCE, RA, GC, IP, RT, MCM, MLM and CRK provided samples and clinical data for the study; DH was responsible of the statistical analysis of the data; all authors contributed to writing the paper and provided critical revision and important intellectual content. MR, MLM and CRK had primary responsibility for final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None, any author has not potential conflicts of interest to declare.
Funding
No Funder/Sponsor has contributed to any aspect of the study.
Ethical statement
The study was approved by the Ethical Committee of La Fe University Hospital. The study was approved by the medical ethics committee at each participating center. All mothers were informed of the purpose of the study and voluntary provided the milk samples.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Roca, M., Vriezinga, S.L., Crespo-Escobar, P. et al. Anti-gliadin antibodies in breast milk from celiac mothers on a gluten-free diet. Eur J Nutr 57, 1947–1955 (2018). https://doi.org/10.1007/s00394-017-1476-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-017-1476-1