Abstract
Purpose
Interleukin (IL)-1β can activate glial cells to trigger neuroinflammation and neurodegeneration. Lower omega (n)-3 polyunsaturated fatty acids (PUFAs) and lower n-3/n-6 PUFA ratios occur in the brain of patients with Alzheimer’s disease (AD). We have previously reported that an n-3 PUFA, eicosapentaenoic acid (EPA), can improve memory and attenuate neurodegeneration-like changes in animal models of AD. However, whether and how EPA modulates glial cell activity and functions remains unclear. The aim of this study was to test the hypothesis that EPA may attenuate neuroinflammation by inhibiting microglial activation and microglia-produced proinflammatory cytokines, and by enhancing the expression of astrocytes-produced neurotrophins and their receptors.
Methods
Male Long-Evans rats were fed either palm oil supplemented diet or EPA supplemented diet for 42 days. On day 36 of diet feeding, rats received an intracerebroventricular injection of IL-1β or saline for 7 days. The glial activation, the expression of amyloid precursor protein (APP), calcium-dependent phospholipase (cPL) A2, brain-derived neurotrophic factor (BDNF) and its receptor, and PUFA profile in the hippocampus were analyzed.
Results
IL-1β elevated biomarkers of microglial CD11b and astrocyte GFAP expression, increased the expression of APP, tumor-necrosis factor (TNF)-α, but reduced BDNF and its receptor (TrKB). IL-1β also lowered n-3 EPA and docosapentaenoic acid concentrations but increased n-6 PUFAs and cPLA2 activity in the hippocampus. EPA supplement normalized the n-3 and n-6 PUFA profiles and cPLA2 levels, inhibited glial activation, reduced APP and TNF-α expression, as well as up-regulated BDNF and TrKB.
Conclusion
Supplementation with EPA appear to have potential effects on improving glial over-activation, n3/n6 imbalance and BDNF down-regulation, which contribute to anti-inflammatory and may provide beneficial effects on inflammation-associated disease such as AD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although the causes for the onset and progress of neurodegenerative diseases, such as Alzheimer’s disease (AD) remain poorly understood, increasing evidence suggests that neuroinflammation plays a crucial role in neurodegeneration [1]. Inflammation occurs in pathologically vulnerable brain regions of the neurodegenerative disease, with increased activated glial cells and proinflammatory cytokine levels, usually not observed in the normal brain [2, 3]. Two types of brain glial cells, microglia and astrocytes, are responsible for the inflammatory response and neuroprotection [4]. Over-activation of microglia-produced excessive proinflammatory cytokines and free radicals can induce neuronal dysfunction and even death [5]. In contrast, astrocytes are involved in neurogenesis and produce neurotrophins and anti-inflammatory mediators [6]. Proinflammatory factors from activated microglia may decrease the secretion of neurotrophins from astrocytes, such as brain-derived neurotrophic factor (BDNF) [7]. BDNF is a critical neurotrophin for neuronal differentiation and survival, exerting its biological effects by binding to either tyrosine kinase (Trk) B receptor or p75NTR receptor. Reduced levels of BDNF in the brain [8] and serum correlate with clinical severity of AD [9], whereas intrahippocampal administration of BDNF in rats protects against neuronal loss by inhibiting the activation of microglia and astrocytes [10]. Furthermore, intranasal BDNF-induced neuroprotection is associated with down-regulation of proinflammatory (TNF-α) and up-regulation of anti-inflammatory (IL-10) cytokines [11]. Because current treatments for neurodegenerative diseases are often ineffective and have numerous side-effects [12], anti-inflammatory/BDNF-augmenting treatments may represent new candidates for the future therapy.
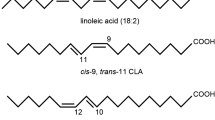
We have previously reported that an omega (n)-3 polyunsaturated essential fatty acid (PUFAs) can reduce inflammation and up-regulate neurotrophins [13,14,15]. n-3 PUFAs synthesized from dietary precursors are important components of membrane phospholipids in both neurons and immune cells. Therefore, they are critical for the modulation of both brain and immune functions [16]. n-3 PUFAs include α-linolenicacid, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). They are potent activators of peroxisome proliferator-activated receptors, which can inhibit inflammation. Phospholipids including linoleic acids (LA) can be utilized by phospholipase (PL)A2 to produce arachidonic acid (AA), which is converted into eicosanoid. Eicosanoids are the precursor of proinflammatory mediators, such as prostaglandin (PG) E2 and thromboxane A2 by COX2 [17,18,19]. Therefore, increased intake of n-6 FAs may raise the risk of inflammatory and neurodegenerative diseases, while protective effects of n-3 fatty acids supplementation have been demonstrated in experimental animal models of AD [20, 21]. Although EPA is far less abundant in the brain than DHA, it is highly neuroactive [22], and may be more effective than DHA in the treatment of psychiatric disorders [23]. However, whether and how EPA modulates glial cell activity and functions remains unknown. Previously, we have reported that EPA markedly attenuated IL-1β-induced decrease in the nerve growth factor and acetylcholine release, as well as improved spatial and working memory [14, 24]. Thus, we hypothesize that (1) EPA can attenuate neuroinflammation by inhibiting microglial activation, which reduces the production of proinflammatory cytokines; (2) EPA may enhance the expression of astrocyte-produced neurotrophins and their receptors; and (3) EPA effects may be related to increased n-3, but reduced n-6, PUFA in the brain. The pathway from IL-1 administration to cell death and possible targets of EPA on microglia and astrocytes are presented in Fig. 1.
Because IL-1β, a potent proinflammatory cytokine, is increased in AD human or mouse brain [25], it can evoke many AD-like changes, such as triggering microglial activation, enhancing the expression of amyloid precursor protein (APP) and impairing cognitive function. The present study used a rat model of AD induced by central administration of IL-1β [13, 15]. The hippocampal samples were collected from rats fed normal or EPA diet with or without IL-1β administration and the expression of microglial marker CD11b, astrocyte marker glial fibrillary acidic protein (GFAP), BDNF,BDNF receptors Trk B and P75, TNF-α as well as APP were measured in the hippocampus. The calcium-dependent (c) PLA2 and PUFA profile were also studied.
Methods
Animals and surgery
Forty male Long-Evans rats (4–8 weeks, 200–220 g) were purchased from Charles River, Montreal, Canada and randomly divided into 4 groups (n = 10). Animals were housed 2 per cage at 22 ± 1 °C, with a 12-h light-dark cycle, and free access to food and water at all times. Animals were handled daily (5 min, thrice per day). After acclimation for 5 days, animals were anesthetized with ketamine (100 mg/kg) and xylazine (20 mg/kg) and placed in a stereotaxic apparatus. Guide cannulae for saline or IL-1β intracerebroventricular (i.c.v.) administration were located over the right lateral ventricle (AP = 1 mm, L = 1.6 mm, 1 mm depth). Following surgery, the rats were allowed to recover for 14 days. The animal protocol was approved by the animal care committee of the University of Prince Edward Island, Canada, and complied with the University of Prince Edward Island guidelines for the care and use of laboratory animals. The experiments were conducted in a blinded fashion.
Diet
After recovery, animals were divided into four groups (n = 10) as follows: PS (palm oil supplemented diet + saline injection); ES (EPA supplemented diet + saline injection); PI (palm oil supplemented diet + IL-1β injection); EI (EPA supplemented diet + IL-1β injection). Rats were fed a diet consisting of regular chow powder (PMI® Richmond, Indiana, US) mixed with 0.8% ethyl (E)-EPA (99% pure) (Amarin Neuroscience Ltd, UK), or 0.8% palm oil (Sigma, Canada) as described previously [13, 14]. Palm oil was chosen as the control diet since it ensured comparable caloric values, contains low amounts of n-6 fatty acids and negligible amounts of n-3 fatty acids [15]. The diet was fed to rats (25–30 g per rat/day) before the light turning off and last for 12 h. Feeding period was 42 days. For preparation of the diet, the master bottle of E-EPA (oil) was taken from −20 °C freezer and aliquoted to Falcon tubes that were flushed with nitrogen gas to prevent oxidation. The EPA diets were prepared every 3 days and flushed with nitrogen, sealed and stored in 4 °C to prevent oxidation. To monitor EPA oxidization during feeding time, peroxide value (PV) was tested by the Peroxysafe kit (M.P. Biomedicals LLC, Solon, Ohio, USA) before and 12 h after the diet exposing to the food container. Briefly, calibration curve was set up by transferring 200 μL of each calibrator and control reagents into the corresponding labeled test tube. Following gentle swirl of the tubes, 1 aliquot of peroxide reagents A, B, C and control was dispensed into every calibrator and control test tube, respectively. After vortexing and stabilizing at the rocker for 10 min, calibration was carried out according to the instruction on the SafTest™ Analyzer. Duplicated diet samples were labeled and above mentioned reagents A–C were added, respectively. After reading the results from the analyzer, the PV value was adjusted by dilution factor and expressed as milliequivalents of peroxide per kilogram of sample. The PV was 0.2 meq/kg in the fresh diet and increased to 3.76 meq/kg after exposing to the feeding containers for 12 h.
I.c.v. saline or IL-1β injection
The i.c.v. injection of IL-1β or saline started on day 36 of diet feeding and continued for 7 days [11, 12]. To minimize handling/procedural stress, rats with implanted cannulae were gently handled and restricted in a soft cotton towel (3 min) daily for 14 days before the injection. On the injection day, 10 ng IL-1β or saline (a total 5 μl) were taken into a 4.2-mm internal needle connected to PE50 polyethylene tube [6, 13, 15]. The rats were gently restricted in the towel under waking state and the cap of the guide cannula was gently unscrewed. The needle was then inserted into the guide cannula, and IL-1β or saline was slowly infused into the brain over a period of 1 min. The injection needle was allowed to remain inside the guide cannula for another 1 min, and then slowly removed [6, 13, 15]. Injections were repeated daily, for 7 days. One day after the last injection, animals were deeply anesthetized by isoflurane inhalation, and decapitated. The brain was removed and dissected on ice, and hippocampi collected for further analyses.
Lipid extraction and gas chromatography (GC)
Lipid extraction and gas chromatography (GC) analyses were utilized to analyze FAs as described previously [26]. Briefly, hippocampal tissue was homogenized with chloroform: methanol solution (2:1). The lower phase containing lipids was dried under a nitrogen stream. The dried samples incubated in a water bath with ethanolic KOH, and then NaCl and hexane were added to make the phase separation; HCl has been added in the low layer to adjust pH, followed by hexane. After the separation, the top layer was dried under a nitrogen stream. Methanolic HCl was added to dry fatty acids, and then NaCl and hexane were added, to make the phase separation again, the top layer containing FAME (fatty acidmethyl ester) was collected for GC analysis. FAME was analyzed by GC using a Hewlett Packard (Palo Alto, CA) 6890 equipped with a flame ionization detector. The FAME was separated on a 60 m Agilent 122-2361 DB-23 capillary column using helium at a flow rate of 1.8 ml/min. The inlet and detector temperatures were constant at 225 °C. Peaks were identified by comparing retention times with external FAME standard mixtures (Nu-Chek-Prep, GLC-NESTLE-37) and DPA PUFA standard (Nu-Chek-Prep, U-101-M).
Western blot
Hippocampal samples were homogenized in lysis buffer (150 mM NaCl, 1% NP-40, 0.5% sodium deoxycholate, 0.1% SDS, 5 mM ethylenediamine tetraacetic acid, 50 mM Tris–Hcl, pH 8.0) supplemented with protease inhibitor cocktail (Pierce Biotechnology, Rockford, IL, USA), then centrifuged at 12,000 rpm for 15 min at 4 °C, the supernatant was collected and protein concentration was estimated by BCA Protein Assay Kit (Pierce Biotechnology). 30–50 μg protein was loaded onto a 10% gradient polyacrylamide gel, electrophoretically transferred to PVDF membrane, after incubation for 2 h at room temperature with 5% non-fat milk, membranes were then incubated with primary antibodies: anti-CD11b (1:1000), anti-GFAP (1:1000), anti-TNF-α (1:1000) anti-BDNF (1:1000), anti-TrkB (1:1000), anti-p75NTR (1:1000), anti-APP(1:1000), and anti-β-actin (1:2000) overnight at 4 °C. After washing, the membranes were incubated with goat radish peroxidase-conjugated secondary antibody (1:5000), followed by detection using enhanced chemiluminescence (Pierce Biotechnology). Band intensities were quantified using Image-Pro Express 4.0 software (Media Cybernetics Inc. Rockville, MD, USA). BDNF, TrkB and p75NTR antibody was purchased from Abcam (England). CD11b, GFAP, TNF-α, APP and β-actin antibody was purchased from Proteintech (Chicago, IL, USA).
Real-time PCR
The total RNA was extracted from hippocampal samples using Trizol reagent according to the manufacturer’s protocol (Gibco BRL, Rockville, MD). The first stranded cDNA was synthesized from 1 μg of total RNA using the Ominiscript RT kit according to the manufacturer’s instructions (Qiagen Inc., Valencia, CA). The PCR sequence was run by Corbett Life Science (Sydney, Australia) Rotor-Gene 6000 system with SYBR Green fluorescence (Qiagen). PCR reactions were carried out in a reaction mixture consisting of 7.5 μl SYBR Green Mix, 0.5 μl each primer (10 μM), 1 μl cDNA, and 6 μl RNase-free water. Amplification was performed using an initial 15-min step at 95 °C to activate the HotStarTaq DNA polymerase, followed by 45 cycles with 94 °C for 15 s (denaturing), 59 °C for 30 s (annealing) and 72 °C for 30 s (extension). All reactions were performed in triplicate for each sample. Gene expression levels were quantified by normalizing Ct values of target genes to Ct values of the reference gene (beta actin) with the ΔΔCt method (24). The primers (Invitrogen, Carlsbad, CA, USA) used to measure the target gene expression are listed in Table 1.
cPLA2 measurement
Hippocumpal samples were homogenized in ice-cold Tris buffer (PH 7.8). The protein concentration was determined in the homogenates with a Coomassie Plus Protein Assay Kit (Pierce), and the cPLA2 activity was measured with a commercial assay kit (Cayman Chemicals) according to the manufacturer’s protocols. Briefly, 1.5 mm arachidonoyl thio-PC in the kit was used as a synthetic substrate to detect PLA2 activity. Cytosolic fractions were obtained by centrifuging at 18,000g for 15 min at 4 °C. cPLA2 activity was determined in the cytosolic fractions with the presence of the iPLA2-specific inhibitor bromoenol lactone (10 M) and the sPLA2-specific inhibitor thioetheramide-PC (50 M), which were incubated with the samples for 20 min at 25 °C before the assay. According to our protocol [27], the assay was repeated and verified in the presence of 50 mol/L cPLA2-specific inhibitor arachidonyl trifluoromethyl ketone to confirm the reliability of this assay for cPLA2.
Statistical analysis
Data are presented as mean ± SEM and analyzed by two-way analyses of variance (ANOVA) for factors DIET and IL-1β treatments with post hoc Bonferroni-corrected t tests for significant ANOVA data. Significance was set at P < 0.05.
Results
Omega-3 FA profiles in the hippocampus
GC data show that the EPA content was significantly increased in both EPA group and EPA with IL-1β group (PS versus ES, P < 0.01; PI versus EI, P < 0.01) (Table 2). The docosapentaenoic acid (DPA) content was also significantly increased in ES and EI group (PS versus ES, P < 0.01, EI versus PI, P < 0.01) (Table 2), but not in α-LA (Table 2) and DHA content (Table 2).
Omega-6 FA profiles in the hippocampus
GC analyses show that LA (Table 2) and AA (Table 2) concentrations were significantly increased in animals which received IL-1β (PS versus PI, P < 0.05 for LA and P < 0.01 for AA). However, these effects were attenuated by EPA feeding (EI versus PI, both P < 0.05).
Changes in glial cell activation and TNF-α expression
As shown in Fig. 2, CD11b and GFAP mRNA expression was increased in PI group compared to PS group (P < 0.01 for both CD11 and GFAP). EPA partially but significantly attenuated the up-regulation of CD11b and GFAP in the IL-1β group (EI versus PI: P < 0.05 for CD11, and P < 0.05 for GFAP). Paralleling the gene expression data, western blot analyses showed a significantly increased CD11b and GFAP protein expressions in PI compared to PS group (both P < 0.01), while EPA supplementation significantly ameliorated this effect (both P < 0.01, EI versus PI, Fig. 3). At the protein expression level, the IL-1β administration strongly up-regulated TNF-α (PS versus PI, P < 0.01), whereas EPA significantly down-regulated TNF-α expression in the IL-1 group (EI versus PI, P < 0.01) or in EPA with saline group (ES versus PS, P < 0.05) (Fig. 3). Furthermore, IL-1β significantly increased the expression of TNF-α mRNA (PS versus PI, P < 0.01), which was attenuated by the EPA diet (EI versus PI, P < 0.05) (Fig. 2c).
Effects of IL-1β administrations in-vitro on mRNA expressions of microglial marker CD11b, astrocyte marker glial fibrillary acidic protein (GFAP), and inflammatory factor TNF-α in the rat hippocampus. CD11b (a), GFAP (b) and TNF-α (c) were significantly increased by IL-1β, while E-EPA attenuated this effect. Data from PCR were normalized by taking the value of control group as 1. **P < 0.01, PS versus PI; # P < 0.05, EI versus PI; ΔΔ P < 0.01, ES versus PS
Effects of IL-1β administrations on protein expressions of microglial marker CD11b, astrocyte marker GFAP, and TNF-α in the rat hippocampus, assessed by western blot (a) and quantified by densitometry (b). Data from western blot were normalized by taking the value of control group as 1. **P < 0.01, PS versus PI; ## P < 0.01, EI versus PI; Δ P < 0.05, ES versus PS
Hippocampal expressions of BDNF, Trk B and p75NTR receptor
At the qPCR level, IL-1β significantly down-regulated BDNF mRNA expression (PS versus PI, P < 0.01, Fig. 4a), and the down-regulation of BDNF expression induced by IL-1β was significantly attenuated by EPA supplementation (EI versus PI, P < 0.01). Similar to BDNF, IL-1β administration down-regulated Trk B mRNA expression (PS versus PI, P < 0.01, Fig. 4b), and EPA supplementation markedly attenuated these effects (EI versus PI, P < 0.01). In contrast, IL-1β up-regulated p75NTR expression (PS versus PI, P < 0.01, Fig. 4c), which was reversed by EPA treatment (PI versus EI, P < 0.01). Western blot analysis (Fig. 5) confirmed the PCR findings, showing that the protein expression of BDNF and TrkB was decreased, and p75NTR increased, in the PS versus PI group (P < 0.01 for BDNF, TrkB and p75), but was reversed in EI versus PI groups (P < 0.01 for BDNF and TrkB, P < 0.05 for p75). The present results also demonstrated that EPA by itself up-regulated the BDNF and TrkB protein expression (PS versus ES, P < 0.05, respectively, Fig. 5), but down-regulated the p75NTR protein expression (PS versus ES, P < 0.01, Fig. 5).
Effects of IL-1β administrations on mRNA expressions of BDNF and its receptor in the rat hippocampus. BDNF (a) and TrkB (b) were significantly decreased by IL-1β compared to the palm oil-fed group, whereas E-EPA attenuated this effect. c p75 was increased by IL-1β compared to the palm oil-fed group, and E-EPA attenuated this effect. Data from PCR were normalized by taking the value of control group as 1. **P < 0.01, PS versus PI; ## P < 0.01, EI versus PI
Effects of IL-1β administration on protein expressions of BDNF and its receptor in the rat hippocampus, assessed by western blot (a) and quantified by densitometry (b). Data from western blot were normalized by taking the value of control group as 1. **P < 0.01, PS versus PI; # P < 0.05, ## P < 0.01, EI versus PI; Δ P < 0.05, ΔΔ P < 0.01, PS versus ES
APP expressions and cPLA2 activity
Both PCR and western blot data demonstrated that APP expression was significantly increased by IL-1 administration (PS versus PI, P < 0.01), which was markedly reversed by EPA treatment (EI versus PI, P < 0.01 for both PCR and western blot) (Fig. 6a, c, d). The hippocampal activity of cPLA2 was also increased by IL-1 (PS versus PI, P < 0.01), but returned to the normal level in the EPA group with IL-1injection (PI versus EI, P < 0.01) (Fig. 6b).
Hippocampal APP expressions and cPLA2 activity in the rats with saline or IL-1 administration after palm or EPA feeding. Data from PCR or western blot were normalized by taking the value of control group as 1. The data of cPLA2 was normalized by taking the value of control group as 100. **P < 0.01, PS versus PI; ## P < 0.01, EI versus PI
Discussion
This study demonstrated that central IL-1β administration activated both microglial and astrocyte markers CD11b and GFAP, enhanced the expression of TNF-α, p75NTR and APP, but decreased BDNF and TrkB receptor expression. These changes were associated with robustly elevated activity of cPLA2 and major n-6 PUFA AA. The 6-week EPA diet significantly increased brain EPA and DPA, but not DHA, and prevented IL-1β-induced increases in cPLA2, AA and LA, attenuated IL-1β-induced glial activation and up-regulations of APP and TNF-α. Furthermore, EPA supplementation up-regulated the expression of BDNF and its TrKB receptor, and down-regulated the P75 receptor expression.
IL-1β, a pluripotent proinflammatory cytokine, can stimulate microglia to generate proinflammatory cytokines, reactive oxygen species (ROS) and nitric oxide, which can directly or indirectly damage neurons and cause neurodegeneration [28, 29]. In the present study, IL-1β induced up-regulation of CD11b and GFAP, as well as TNF-α expression, were all attenuated by the EPA diet, supporting our first hypothesis that EPA supplementation may indeed ameliorate neuroinflammation by modulating glial activity.
Previously, we have reported that microglial activation could affect astrocyte functions, thereby changing the system of neurotrophins [24, 30]. Astrocytes-produced neurotrophins, such as BDNF, can suppress neuroinflammation and protect neurons. Decreased BDNF levels were reported in the brain or blood of patients with neurodegenerative diseases (8). The biological effects of BDNF are mediated through the high-affinity (Trk B) and the low-affinity (p75NTR) receptors. Binding to high-affinity TrkB receptors activates several intracellular pathways, including the mitogen-activated protein kinase (MAPK) pathway, and the phosphoinositide 3-kinase (PI3 K)/Akt/Bcl2 pathway [31], which promotes neuronal survival, differentiation and regulates synaptic transmission [32]. However, Trk B reduction can trigger p75NTR receptor expression, thereby inducing neuron apoptosis [33]. The present study on one hand showed that EPA up-regulated BDNF and TrkB expression in control group, and prevents the down-regulation of BDNF and TrkB receptor in the IL-1β group. On the other hand, EPA down-regulated the p75NTR receptor expression in control animals, and reversed the up-regulation of p75NTR receptor in IL-1β group. Thus, these results support our second hypothesis that EPA may exert neuroprotective functions by modulating BDNF and neurotrophin receptors. Although the exact mechanisms by which EPA regulates neurotrophin function remain unknown, n-3 fatty acids can modify the activity of several membrane-bound enzymes, including protein kinase C [34], which is linked to BDNF transcription [35].
The mechanism by which sub-acute IL-1β increased n-6 PUFA also remains unclear. However, it is known that cellular stress induced by administration of IL-1β can activate pathways involved in fatty acid synthesis and turnover [36]. Since AA is a precursor of inflammatory mediators under the action of cPLA2 [37], increased the enzyme activity further supports that IL-1β can trigger an inflammation-associated FA profile in hippocampal neuronal membranes. More interestingly, increased contents of AA and PLA2 were reported in human amyloid precursor protein (hAPP) transgenic mice and AD patients [38], while β-amyloid can activate PLA2 and increase AA contents [38]. In the present study, up-regulation of APP was found in the hippocampus of rats received IL-1β which is consistent with our previous report [16]. Collectively, these findings may suggest an important link between neuroinflammation and APP; likely mediated by APP-induced activation of PLA2 and AA.
Following the EPA diet with or without IL-1β injections, the EPA and DPA rose, while cPLA2, AA and LA decreased, associated with reduced glial activation as well as APP and TNF-α expression, and up-regulated BDNF and TrKB receptor expression. Thus, these results seem to support the last hypothesis that EPA exerts anti-inflammatory and neuroprotective effects by increasing n-3, but reducing n-6, in the brain.
The last important finding from this study was that an n-3 PUFA, DPA, was increased, while DHA was unaffected after EPA feeding, which is consistent with data from another group [39]. Accumulated evidence shows that EPA and DHA may be synthesized separately or through different ways. Igarashi et al. reported that the liver is a major site of DHA synthesis from a-LNA and can maintain a normal concentration of DHA in the brain by this synthesis even if there is no DHA in the diet [40]. This finding is supported by Bourre et al who reported that a dietary absence DHA did not decrease the concentration of brain DHA in animals [41]. Similarly, using mice engineered to carry a fat-1 gene, which can convert n-6 PUFAs into n-3 PUFAs, Siegert et al. reported that a significant increase in EPA but not DHA levels was found in the brain of fat-1 mice compared to wt littermates [42]. Therefore, the finding from the present study that DHA levels were not affected by EPA administration is unsurprised. Taken together, these data suggest that the effects of EPA on glial cells and the neurotrophic system were not via DHA synthesis per se, but rather due to EPA own function, either directly or via its metabolite (DPA). Since the function of DPA in the brain is poorly understood, this possibility warrants further investigation.
In summary, the present results suggest that IL-1β, by triggering glial activation and increasing n-6 PUFA, induces neuroinflammation and APP expression, but suppresses neurotrophin BDNF function, in rat hippocampus. EPA treatment restored the n-3 and n-6 PUFA concentrations in the hippocampus, and normalized glial cell activity and BDNF signaling, thereby inducing anti-inflammation in IL-1β-injected animals. Thus, EPA may provide beneficial effects on neurodegenerative diseases such as AD.
Abbreviations
- AA:
-
Arachidonic acid
- AD:
-
Alzheimer’s disease
- APP:
-
Amyloid precursor protein
- BDNF:
-
Brain-derived neurotrophic factor
- cPLA2:
-
Calcium-dependent phospholipase A2
- DHA:
-
Docosahexaenoic acid
- DPA:
-
Docosapentaenoic acid
- EPA:
-
Eicosapentaenoic acid
- GC:
-
Gas chromatography
- GFAP:
-
Glial fibrillary acidic protein
- IL-1β:
-
Interleukin-1β
- LA:
-
Linoleic acids
- MAPK:
-
Mitogen-activated protein kinase
- p75NTR:
-
p75 neurotrophin receptor
- PUFAs:
-
Polyunsaturated fatty acids
- ROS:
-
Reactive oxygen species
- TNF-α:
-
Tumor-necrosis factor-α
- TrkB:
-
Tyrosine receptor kinase B
References
Esiri MM (2007) The interplay between inflammation and neurodegeneration in CNS disease. J Neuroimmunol 184(1–2):4–16. doi:10.1016/j.jneuroim.2006.11.013
Mrak RE, Griffin WST (2005) Glia and their cytokines in progression of neurodegeneration. Neurobiol Aging 26(3):349–354. doi:10.1016/jneurobiolaging.2004.05.010
Finch CE, Morgan TE (2007) Systemic inflammation, infection, ApoE alleles, and Alzheimer disease: a positionpaper. Curr Alzheimer Res 4(2):185–189
Heneka MT, Carson MJ, El Khoury J, Landreth GE, Brosseron F, Feinstein DL, Jacobs AH, Wyss-Coray T, Vitorica J, Ransohoff RM, Herrup K, Frautschy SA, Finsen B, Brown GC, Verkhratsky A, Yamanaka K, Koistinaho J, Latz E, Halle A, Petzold GC, Town T, Morgan D, Shinohara ML, Perry VH, Holmes C, Bazan NG, Brooks DJ, Hunot S, Joseph B, Deigendesch N, Garaschuk O, Boddeke E, Dinarello CA, Breitner JC, Cole GM, Golenbock DT, Kummer MP (2015) Neuroinflammation in Alzheimer’s disease. Lancet Neurol 14(4):388–405. doi:10.1016/S1474-4422(15)70016-5
Kitazawa M, Cheng D, Tsukamoto MR, Koike MA, Wes PD, Vasilevko V, Cribbs DH, LaFerla FM (2011) Blocking IL-1 signaling rescues cognition, attenuates tau pathology, and restores neuronal β-catenin pathway function in an Alzheimer’s disease model. J Immunol 187(12):6539–6549. doi:10.4049/jimmunol.1100620
Song C, Zhang Y, Dong Y (2013) Acute and subacute IL-1β administrations differentially modulate neuroimmune and neurotrophic systems: possible implications for neuroprotection and neurodegeneration. J Neuroinflammation 10:59. doi:10.1186/1742-2094-10-59
Min SK, Park JS, Luo L, Kwon YS, Lee HC, Shim HJ, Kim ID, Lee JK, Shin HS (2015) Assessment of C-phycocyanin effect on astrocytes-mediated neuroprotection against oxidative brain injury using 2D and 3D astrocyte tissue model. Sci Rep 5:14418. doi:10.1038/srep14418
Lee J, Fukumoto H, Orne J, Klucken J, Raju S, Vanderburg CR, Irizarry MC, Hyman BT, Ingelsson M (2005) Decreased levels of BDNF protein in Alzheimer temporal cortex are independent of BDNF polymorphisms. Exp Neurol 194(1):91–96. doi:10.1016/j.expneurol.2005.01.026
Laske C, Stransky E, Leyhe T, Eschweiler GW, Wittorf A, Richartz E, Bartels M, Buchkremer G, Schott K (2006) Stage dependent BDNF serum concentrations in Alzheimer’s disease. J Neural Transm 113(9):1217–1224. doi:10.1007/s00702-005-0397-y
Bovolenta R, Zucchini S, Paradiso B, Rodi D, Merigo F, Navarro Mora G, Osculati F, Berto E, Marconi P, Marzola A, Fabene PF, Simonato M (2010) Hippocampal FGF-2 and BDNF overexpression attenuates epileptogenesis-associated neuroinflammation and reduces spontaneous recurrent seizures. J Neuroinflammation 7:81. doi:10.1186/1742-2094-7-81
Jiang Y, Wei N, Lu T, Zhu J, Xu G, Liu X (2011) Intranasal brain-derived neurotrophic factor protects brain from ischemic insult via modulating local inflammation in rats. Neuroscience 172:398–405. doi:10.1016/jneuroscience.2010.10.054
Al-Amin MM, Reza HM (2014) Neuroinflammation: contemporary anti-inflammatory treatment approaches. Neurosciences (Riyadh) 19(2):87–92
Song C, Li X, Leonard BE, Horrobin DF (2003) Effects of dietary n-3 or n-6 fatty acids on interleukin-1beta-induced anxiety, stress, and inflammatory responses in rats. J Lipid Res 44(10):1984–1991. doi:10.1194/jlr.M300217-JLR200
Song C, Horrobin D (2004) Omega-3 fatty acid ethyl-eicosapentaenoate, but not soybean oil, attenuates memory impairment induced by central IL-1beta administration. J Lipid Res 45(6):1112–1121. doi:10.1194/jlr.M300526-JLR200
Song C, Manku MS, Horrobin DF (2008) Long-chain polyunsaturated fatty acids modulate interleukin-1beta-induced changes in behavior, monoaminergic neurotransmitters, and brain inflammation in rats. J Nutr 138(5):954–963
Horrobin DF, Bennett CN (1999) Depression and bipolar disorder: relationships to impaired fatty acid and phospholipid metabolism and to diabetes, cardiovascular disease, immunological abnormalities, cancer, ageing and osteoporosis. Possible candidate genes. Prostaglandins Leukot Essent Fatty Acids 60(4):217–234. doi:10.1054/plef.1999.0037
Russo GL (2009) Dietary n-6 and n-3 polyunsaturated fatty acids: from biochemistry to clinical implications in cardiovascular prevention. Biochem Pharmacol 77(6):937–946. doi:10.1016/j.bcp.2008.10.020
Lone AM, Taskén K (2013) Proinflammatory and immunoregulatory roles of eicosanoids in T cells. Front Immunol 4:130. doi:10.3389/fimmu.2013.00130
Bernardo A, Minghetti L (2006) PPAR-gamma agonists as regulators of microglial activation and brain inflammation. Curr Pharm 12(1):93–109
Fernández-Fernández L, Comes G, Bolea I, Valente T, Ruiz J, Murtra P, Ramirez B, Anglés N, Reguant J, Morelló JR, Boada M, Hidalgo J, Escorihuela RM, Unzeta M (2012) LMN diet, rich in polyphenols and polyunsaturated fatty acids, improves mouse cognitive decline associated with aging and Alzheimer’s disease. Behav Brain Res 228:261–271. doi:10.1016/j.bbr.2011.11.014
Hashimoto M, Hossain S (2011) Neuroprotective and ameliorative actions of polyunsaturated fatty acids against neuronal diseases: beneficial effect of docosahexaenoic acid on cognitive decline in Alzheimer’s disease. Pharmacol Sci 116(2):150–162
Horrobin DF (2002) A new category of psychotropic drugs: neuroactive lipids as exemplified by ethyl eicosapentaenoate (E-E). Prog Drug Res 59:171–199
Peet M, Stokes C (2005) Omega-3 fatty acids in the treatment of psychiatric disorders. Drugs 65(8):1051–1059
Taepavarapruk P, Song C (2010) Reductions of acetylcholine release and nerve growth factor expression are correlated with memory impairment induced by interleukin-1beta administrations: effects of omega-3 fatty acid EPA treatment. J Neurochem 112(4):1054–1064. doi:10.1111/j.1471-4159.2009.06524.x
Zhou WW, Lu S, Su YJ, Xue D, Yu XL, Wang SW, Zhang H, Xu PX, Xie XX, Liu RT (2014) Decreasing oxidative stress and neuroinflammation with a multifunctional peptide rescues memory deficits in mice with Alzheimer disease. Free Radic Biol Med 74:50–63. doi:10.1016/j.freeradbiomed.2014.06.013
Meng Q, Luchtman DW, El Bahh B, Zidichouski JA, Yang J, Song C (2010) Ethyl-eicosapentaenoate modulates changes in neurochemistry and brain lipids induced by parkinsonian neurotoxin 1-methyl-4-phenylpyridinium in mouse brain slices. Eur J Pharmacol 649(1–3):127–134. doi:10.1016/j.ejphar.2010.09.046
Song C, Li X, Kang Z, Kadotomi Y (2007) Omega-3 fatty acid ethyl-eicosapentaenoate attenuates IL-1beta-induced changes in dopamine and metabolites in the shell of the nucleus accumbens: involved with PLA2 activity and corticosterone secretion. Neuropsychopharmacology 32(3):736–744. doi:10.1038/sj.npp.1301117
Qian L, Hong JS, Flood PM (2006) Role of microglia in inflammation-mediated degeneration of dopaminergic neurons: neuroprotective effect of interleukin 10. J Neural Transm Suppl 70:367–371
Colombo E, Cordiglieri C, Melli G, Newcombe J, Krumbholz M, Parada LF, Medico E, Hohlfeld R, Meinl E, Farina C (2012) Stimulation of the neurotrophin receptor TrkB on astrocytes drives nitric oxide production and neurodegeneration. J Exp Med 209(3):521–535. doi:10.1084/jem.20110698
Capsoni S, Brandi R, Arisi I, D’Onofrio M, Cattaneo A (2011) A dual mechanism linking NGF/proNGF imbalance and early inflammation to Alzheimer’s disease neurodegeneration in the AD11 anti-NGF mouse model. CNS Neurol Disord Drug Targets 10(5):635–647
Huang EJ, Reichardt LF (2003) Trk receptors: roles in neuronal signal transduction. Annu Rev Biochem 72:609–642. doi:10.1146/annurev.biochem.72.121801.161629
Bibel M, Barde YA (2000) Neurotrophins: key regulators of cell fate and cell shape in the vertebrate nervous system. Genes Dev 14(23):2919–2937
Mamidipudi V, Wooten MW (2002) Dual Role for p75NTR signaling in survival and cell death: can intracellular mediators provide and explanation? J Neurosci 68(4):373–384. doi:10.1002/jnr.10244
Madani S, Hichami A, Legrand A, Belleville J, Khan NA (2001) Implication of acyl chain of diacylglycerols in activation of different isoforms of protein kinase C. FASEB J 15(14):2595–2601. doi:10.1096/fj.01-0753int
Lee JG, Cho HY, Park SW, Seo MK, Kim YH (2010) Effects of olanzapine on brain-derived neurotrophic factor gene promoter activity in SH-SY5Y neuroblastoma cells. Prog Neuropsychopharmacol Biol Psychiatry 34(6):1001–1006. doi:10.1016/j.pnpbp.2010.05.013
Parazzoli S, Harmon JS, Vallerie SN, Zhang T, Zhou H, Robertson RP (2012) Cyclooxygenase-2, not microsomal prostaglandin E synthase-1, is the mechanism for interleukin-1β-induced prostaglandin E2 production and inhibition of insulin secretion in pancreatic islets. J Biol Chem 287(38):32246–32253. doi:10.1074/jbc.M112.364612
Tanikawa M, Lee HY, Watanabe K, Majewska M, Skarzynski DJ, Park SB, Lee DS, Park CK, Acosta TJ, Okuda K (2008) Regulation of prostaglandin biosynthesis by interleukin-1 in cultured bovine endometrial cells. J Endocrinol 199(3):425–434. doi:10.1677/JOE-08-0237
Sanchez-Mejia RO,Mucke L (2010) Phospholipase A2 and arachidonic acid in Alzheimer’s disease. Biochim Biophys Acta. Biochim Biophys Acta 1801(8):784–790. doi:10.1016/j.bbalip.2010.05.013
Willis S, Samala R, Rosenberger TA, Borges K (2009) Eicosapentaenoic and docosahexaenoic acids are not anticonvulsant or neuroprotective in acute mouse seizure models. Epilepsia 50(1):138–142. doi:10.1111/j.1528-1167.2008.01722.x
Igarashi M, DeMar JC Jr, Ma K, Chang L, Bell JM, Rapoport SI (2007) Docosahexaenoic acid synthesis from alpha-linolenic acid by rat brain is unaffected by dietary n-3 PUFA deprivation. J Lipid Res 48(5):1150–1158. doi:10.1194/jlr.M600549-JLR200
Bourre JM, Dumont OS, Piciotti MJ, Pascal GA, Gurand GA (1992) Dietary alpha-linolenic acid deficiency in adult rats for 7 months does not alter brain docosahexaenoic acid content, in contrast to liver, heart and testes. Biochim Biophys Acta 1124(2):119–122
Siegert E, Paul F, Rothe M, Weylandt KH (2017) The effect of omega-3 fatty acids on central nervous system remyelination in fat-1 mice. BMC Neurosci 18(1):19. doi:10.1186/s12868-016-0312-5
Acknowledgements
This work was supported by grants from the National Natural Science Funds of China to CS (81171118) and to YLD (81360179), the Education Department of Guangdong Provincial grant to CS (Q14183, Q14175), as well as by Famous Oversea Professor program of Ministry of Education of China to CS.
Author contribution
CS designed the experiments, analyzed the data, wrote and edited the manuscript. DYL performed the experiment, analyzed the data and drafted the manuscript. XM analyzed FA profile by GC and discussed the data, AK discussed the data and edited the manuscript. All authors have reviewed and approved the final version of the manuscript. Technical assistances provided by Dr. Azoy Kundu, Ms. Qinjia Meng and Ms. Yuyu Li are appreciated.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declared no conflicts of interest. The study was partially funded by Amarine Neuroscience Ltd. (UK), a manufacturer of CNS drugs based in fatty acids. The funder had no involvement in guiding this study, interpreting its results, discussing its findings and writing the manuscript, and making the decision about the submission and publication.
Additional information
Affiliations one and two (two universities) are equal as the first affiliations.
Rights and permissions
About this article
Cite this article
Dong, Y., Xu, M., Kalueff, A.V. et al. Dietary eicosapentaenoic acid normalizes hippocampal omega-3 and 6 polyunsaturated fatty acid profile, attenuates glial activation and regulates BDNF function in a rodent model of neuroinflammation induced by central interleukin-1β administration. Eur J Nutr 57, 1781–1791 (2018). https://doi.org/10.1007/s00394-017-1462-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-017-1462-7