Abstract
Background
Toll-like receptors (TLRs) are a family of pattern-recognition receptors which play a role in eliciting innate/adaptive immune responses and developing chronic inflammation. So, the aim of this study was to analyze the effect of TLR7 gene single nucleotide polymorphisms (SNPs) rs3853839 and rs179019 on systemic lupus erythematosus (SLE) susceptibility and to assess their relations with various clinical and laboratory data of the patients.
Methods
This is a case–control study including 50 SLE female patients and 50 healthy controls. TLR7 rs3853839 and rs179019 genotyping was performed using real-time polymerase chain reaction (PCR) TaqMan-based allelic discrimination assay.
Results
Regarding rs3853839, there was a statistically significant difference in the distribution of the genotypes between SLE patients and the control group in our study (P = 0.009). A significant association was detected between TLR7 genotypes (rs385389) and lupus nephritis (p = 0.021). Regarding rs179019, there was no statistically significant difference in the distribution of the genotypes between SLE patients and the control group in our study (P = 0.271)
Conclusion
This study revealed the plausible role of TLR7 rs3853839 SNP in SLE in Egyptian women.
Zusammenfassung
Hintergrund
„Toll-like receptors” (TLR) sind eine Familie von Mustererkennungsrezeptoren, die an der Auslösung von angeborenen oder adaptiven Immunreaktionen und an der Entwicklung einer chronischen Entzündung beteiligt sind. Ziel dieser Studie war es daher, die Wirkung der Einzelnukleotidpolymorphismen (SNP) rs3853839 und rs179019 in TLR7 auf die Anfälligkeit für einen systemischen Lupus erythematodes (SLE) zu untersuchen. Zudem sollte ihr Zusammenhang mit verschiedenen klinischen und laboranalytischen Patientendaten ermittelt werden.
Methoden
In die vorliegende Fall-Kontroll-Studie wurden 50 Patientinnen mit SLE und 50 gesunde Kontrollen eingeschlossen. Die Genotypisierung für TLR7 rs3853839 und rs179019 wurde mithilfe eines Real-time-Polymerase-Kettenreaktions-TaqMan-basierten Assays zur Alleldifferenzierung durchgeführt.
Ergebnisse
Für rs3853839 bestand in unserer Studie ein statistisch signifikanter Unterschied bezüglich der Genotypverteilung zwischen SLE-Patientinnen und der Kontrollgruppe (p = 0,009). Eine signifikante Assoziation wurde zwischen TLR7-Genotypen (rs385389) und Lupusnephritis gefunden (p = 0,021). Für rs179019 bestand in unserer Studie kein statistisch signifikanter Unterschied bezüglich der Genotypverteilung zwischen SLE-Patientinnen und der Kontrollgruppe (p = 0,271).
Schlussfolgerung
Diese Studie zeigt die plausible Bedeutung des TLR7-rs3853839-SNP für den SLE bei ägyptischen Frauen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) is a polygenic disease that is affected by ethnicity, gender, and environmental factors. Toll-like receptor 7 (TLR7) has been thoroughly studied using lupus-prone mouse models [1].
The human TLR family consists of ten receptors classified as members of the IL-1 receptor (IL-1 R) superfamily on the basis of a common cytoplasmic (Toll/IL-1 R) domain. The extracellular parts of TLRs are diverse, incorporating varying numbers of leucine-rich repeats. Following encounter with a ligand, TLRs elicit a cascade of events leading to the induction of a number of proinflammatory genes [2]. These TLR responses are crucial for the functioning of both the innate immunity and the adaptive immunity [3].
TLRs could respond to both exogenous, microbe-derived pathogen-associated molecular patterns (PAMPs) and also endogenous or self ligands. The capability of TLRs to recognize host-derived danger signals which are produced on cell necrosis and damage was also identified [4]. In addition, studies have found that the immune complexes containing self-DNA and/or self-RNA can act as endogenous triggers for the activation of TLRs inducing the expression of type I interferon (type I IFN), a cardinal cytokine in the pathogenesis of SLE [5].
Up-regulated TLR7 mRNA expression has been detected in peripheral blood mononuclear cells (PBMCs) from SLE patients and levels correlate with the expression of type I IFNs, including IFN-alpha (IFNα) [6]. Normally, type I IFNs serve an important function in the defense against viral infections but in SLE elevated levels of serum type I IFN is frequently reported and is of importance to many aspects of the pathology and etiology of SLE representing a possible link between TLR and SLE [7].
Toll-like receptor 7 (TLR7) gene is situated at Xp22.2 and encodes TLR7 protein [3]. The association between TLR7 single nucleotide polymorphisms (SNPs) and SLE could be explained by overproduction of proinflammatory cytokines in addition to type I IFN [8].
It has now been demonstrated that miRNAs can act to adjust TLR signaling by targeting expression itself or by modulating downstream regulators, adaptor molecules, and cytokines [9]. Variants in the 3′ untranslated region (UTR) of TLR7 rs3853839 (G/C) may affect miRNAs binding and consequently TLR7 expression and/or responsiveness. The G‑allele carriers have increased TLR7 transcripts and are more anticipated than C‑allele carriers to have anti-RNA associated autoantibodies [10]. The non-risk C allele has a binding site for microRNA-3148 (miR-3148) resulting in a faster breakdown of the transcript and thus lower levels of TLR7 gene product [11].
Within this context, this case–control study was carried out to detect whether TLR7 rs3853839 and rs179019 SNPs confer risk to SLE in a cohort of Egyptian female patients and also to explore the association of the polymorphisms with various parameters of the disease.
Material and methods
Study subjects
Fifty females with SLE, diagnosed according to the 2012 Systemic Lupus International Collaborating Clinics (SLICC) classification criteria, [12] were studied. Their mean age was 28.8 ± 8.7 years. All patients were recruited from Rheumatology and Rehabilitation Department, Kasr Al Ainy Hospital Cairo University, and tenants of declaration of Helsinki were respected. Disease activity was assessed with the Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) [13]. It includes 24 weighted clinical and laboratory variables of nine organ systems. The range of scores of the descriptors is from 1–8, and the total possible score for all 24 descriptors is 105. Activity categories were defined on the basis of SLEDAI scores: no activity (SLEDAI < 2), mild activity (SLEDAI = 2–8), moderate activity (SLEDAI > 10), severe activity (SLEDAI > 20) [13].
Healthy controls
Fifty healthy subjects served as controls and were matched as closely as possible for age (with mean of 29.3 ± 8.6 years old), sex (100% females), and ethnic group.
Peripheral blood samples were obtained from all subjects after they were provided with a written informed consent.
Because TLR7 is located on an X chromosome, male and female individuals needed to be analyzed for the association separately. However, because of the female predominance of SLE, the sample size of male SLE patients was too small to be analyzed statistically. Therefore, male patients and controls were excluded from this study.
Genotyping
Total genomic DNA of patients and healthy controls was extracted from about 2 ml anticoagulated whole blood on EDTA using Qiagen extraction kit (catalog number 51104, USA).
The genotyping of TLR-7 SNPs at rs3853839 and rs179010 was performed by real-time polymerase chain reaction (PCR) TaqMan-based allelic discrimination assay, on the Applied Biosystems 7300 real-time PCR system (ABI, USA).The primers and probes for these assays, which were purchased from Applied Biosystems (PN:4351379, USA), were provided as a commercially complete kit. The kit contains both forward and reverse primers in addition to probes for both wild and minor type alleles.
Briefly, PCR was performed in the presence of 5 μl genomic DNA, 12.5 µl TaqMan master mix, and 1.25 µl of 20x assay mix. Polymerase chain reaction analysis was performed in 96-well plates on a thermal cycler (ABI 7300; Applied Biosystems). Reaction conditions were 60 °C for 30 s and 95 °C for 10 min, followed by 45 cycles at 92 °C for 15 s and 60 °C for 1 min. Genotype calls for individual samples were made by plotting the normalized intensity of the reporter dyes in each sample well on an allelic discrimination plot.
For quality control, genotyping was repeated for random samples in each group to confirm our results.
Statistical methods
Data were statistically described in terms of mean ± standard deviation (± SD), median and range, or frequencies (number of cases) and percentages when appropriate. Odds ratio (OR) and 95% confidence interval (95% CI) were used to describe the quantitative difference in genotypes between cases and controls. Comparison of numerical variables between the study groups was done using Mann–Whitney U test for independent samples. For comparing categorical data, Chi square (χ2) test was performed. Exact test was used instead when the expected frequency is less than 5; p values less than 0.05 was considered statistically significant. All statistical calculations were done using computer programs SPSS (Statistical Package for the Social Science; SPSS Inc., Chicago, IL, USA) version 15 for Microsoft Windows.
Results
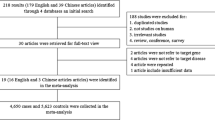
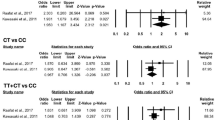
Genotype frequencies of TLR7 SNPs rs3853839 and rs179019 in the case–control cohort of patients with SLE were shown in Tables 1 and 2, respectively. Regarding TLR7 SNP rs3853839, these frequencies carry a statistically significant difference as regards the susceptibility to SLE (P = 0.009).
The SLE patients were classified according to the different TLR7 rs3853839 genotypes into 2 distinct groups: the wild (C/C) genotype group which included 20 patients, the polymorphic (C/G, G/G) genotype group which included 30 patients. These 2 groups were compared as regards clinical data including age, the frequency of malar rash, alopecia, arthritis, vasculitis, photosensitivity, fever, lupus headache, mucosal ulcer, pleurisy, seizure, psychosis, positive family history of similar condition, and SLEDAI score. Also the two groups were compared regarding the age at onset of SLE symptoms. There was no statistical significance between both groups as the p-value was > 0.05. However, patients with polymorphic (CG and GG) genotype showed higher frequency of nephritis than the wild (CC) genotype (p = 0.021) (Table 3).
As regards to the laboratory data of SLE group of patients in relation to TLR7 rs3853839 genotypes, we could not find any statistically significant difference between the group with the wild genotype (CC) and the group carrying the polymorphic genotypes (CG and GG) regarding anti-double stranded deoxyribonucleic acid (anti-dsDNA) (p = 0.589), erythrocyte sedimentation rate (ESR) (p = 0.032), complement consumption (p = 0.572), haemoglobin (HB) level (p = 0.766), total leucocytic count (TLC) (p = 0.699), platelets count (p = 0.394), and serum creatinine (p = 0.598).
Comparison between SLE patients according to their TLR7 rs179019 genotypes regarding the clinical and laboratory data revealed no statistical significant difference (data not shown).
Discussion
Although the sex effect has been attributed to sex hormones, the fact that XXY male subjects have a 14-fold higher risk of developing SLE than 46 XY men indicates that X‑linked genes may be risk factors for human SLE [14]. Several common polymorphisms in the TLR7 gene, located at Xp22.2, have been described. In this study, we focused on (rs3853839) in the 3′ untranslated region and rs179019 in intron 2 of the TLR7 gene for genetic analysis, as these polymorphisms have been studied in different ethnic groups, but not previously in the Egyptian population.
Analysis of the distribution of TLR7 rs3853839 genotypes among the SLE patients and controls showed higher frequency of polymorphic genotypes (CG and GG) in SLE patients (60%) compared to the healthy controls (34%) and this difference was statistically significant. Thus, in our study the presence of the polymorphic genotype increases the susceptibility to SLE compared to the CC wild-type carriers.
In concordance to our study, a large multicentered and multiethnic study comprising Chinese, Korean, and Japanese participants identified such SNP in the 3′ UTR region of TLR7 rs3853839(G/C) as a risk factor for SLE [10].
This is in agreement with the 2011 Kawasaki et al. study in Japan. They also showed that SLE female patients carrying rs3853839 polymorphism were at a higher risk of developing SLE [15].
Similarly, Deng et al. reported TLR7 SNP rs3853839 association with SLE in African Americans, European Americans, and Amerindian/Hispanics. [11].
Furthermore, Laska et al. and Enoveld et al. demonstrated contribution of TLR7 gene SNP to SLE in the Danish population [16, 7].
Furthermore, analysis of the distribution of TLR7 rs179019 genotypes among the SLE patients and controls showed higher frequency of polymorphic genotypes (CA&AA) in SLE patients (34%) compared to the healthy controls (24%); however, this difference was not statistically significant.
Previous studies supported the association between the risk allele of the 3′ untranslated region (UTR) and elevated expression of TLR7, evidence for the association of the intronic SNP with levels of TLR7 mRNA was not reported; therefore, the molecular mechanism of the intronic SNP remains to be clarified by further studies [15].
Background factors (genetic and otherwise) differentiating populations can modify the expression of a gene and lead to different levels of association. It is necessary to reproduce allelic association studies in many ethnically diverse populations to evaluate the real importance of this gene in SLE.
We also evaluated the contribution of these polymorphisms to different clinical symptoms and laboratory data of SLE. No statistically significant difference could be elicited between the groups with the wild genotype and the groups carrying the polymorphic genotypes except for nephritis with increased frequency in the group carrying the polymorphic genotypes in TLR7 rs3853839.
This finding was in agreement with Kawasaki et al. and Enoveld et al. who reported association of TLR7 SNP rs3853839 with lupus nephritis [15, 7].
The reduced sample size might be a limitation to our study. More studies are needed to investigate the different TLR7 gene polymorphisms and their biological function in SLE patients. Analyzing the correlation between TLR7 SNP, TLR7 mRNA expression in PBMCS and type I IFN in patients’ sera is highly recommended.
Targeting genetic risk factors for diseases might provide a backdoor for designing future therapies. This is valuable especially for complex diseases with expensive, noneffective treatments bearing several side effects that may even lead to death in many cases [16].
The accumulation of evidence pointing towards TLRs in autoimmunity has attracted the attention for possible therapeutic interventions directed towards the modulation of Toll-like receptors and their signaling pathways [17].
Conclusion
Our study suggests a possible role of TLR7 gene rs3853839 polymorphism in increasing the susceptibility of females carrying this polymorphism to SLE. In addition, a statistical significant influence of the rs3853839 polymorphism on development of nephritis was observed. This association indicates that the TLR7 rs 3853839 polymorphism can be used as a prognostic marker as well as a likely pathogenetic role for TLR7 and suggests TLR7 as a candidate for targeted therapy in SLE.
References
Celhar T, Fairhurst A‑M (2014) Toll-like receptors in systemic lupus erythematosus: potential for personalized treatment. Front Pharmacol 5:265
Akira S, Uematsu S, Takeuchi O (2006) Pathogen recognition and innate immunity. Cell 124:783–801
Banchereau J, Pascual V (2006) Type I interferon in systemic lupus erythematosus and other autoimmune diseases. Immunity 25:383–392
Montero Vega MT, de Andres Martin A (2008) Toll-like receptors: a family of innate sensors of danger that alert and drive immunity. Allergol Immunopathol (Madr) 36(6):347–357
Hurst J, von Landenberg P (2008) Toll-like receptors and autoimmunity. Autoimmun Rev 7(3):204–208
Lyn-Cook BD, Xie C, Oates J, Treadwell E, Word B, Hammons G, Wiley K (2014) Increased expression of Toll-like receptors (TLRs) 7 and 9 and other cytokines in systemic lupus erythematosus (SLE) patients: ethnic differences and potential new targets for therapeutic drugs. Mol Immunol 61:38–43
Enevold C, Nielsen CH, Jacobsen RS, Hermansen MLF, Molbo D, Avlund K, Bendtzen K, Jacobsen S (2014) Single nucleotide polymorphisms in genes encoding toll-like receptors 7, 8 and 9 in Danish patients with systemic lupus erythematosus. Mol Biol Rep 41:5755–5763
Savitsky D, Tamura T, Yanai H, Taniguchi T (2010) Regulation of immunity and oncogenesis by the IRF transcription factor family. Cancer Immunol Immunother 59(4):489–510
O’Neill LA, Sheedy FJ, Mccoy CE (2011) MicroRNAs: the fine-tuners of Toll-like receptor signaling. Nat Rev Immunol 11:163–175
Shen N, Fu Q, Deng Y, Qian X, Zhao J, Kaufman KM, Wu YL, Yu CY, Tang Y, Chen JY, Yang W, Wong M, Kawasaki A, Tsuchiya N, Sumida T, Kawaguchi Y, Howe HS, Mok MY, Bang SY, Liu FL, Chang DM, Takasaki Y, Hashimoto H, Harley JB, Guthridge JM, Grossman JM, Cantor RM, Song YW, Bae SC, Chen S, Hahn BH, Lau YL, Tsao BP (2010) Sex-specific association of X‑linked Toll-like receptor 7 (TLR7) with male systemic lupus erythematosus. Proc Natl Acad Sci U S A 107:15838–15843
Deng Y, Zhao J, Sakurai D, Kaufman KM, Edberg JC, Kimberly RP, Kamen DL, Gilkeson GS, Jacob CO, Scofield RH, Langefeld CD, Kelly JA, Ramsey-Goldman R, Petri MA, Reveille JD, Vilá LM, Alarcón GS, Vyse TJ, Pons-Estel BA, Argentine Collaborative Group, Freedman BI, Gaffney PM, Sivils KM, James JA, Gregersen PK, Anaya JM, Niewold TB, Merrill JT, Criswell LA, Stevens AM, Boackle SA, Cantor RM, Chen W, Grossman JM, Hahn BH, Harley JB, Alarcόn-Riquelme ME, BIOLUPUS and GENLES networks, Brown EE, Tsao BP (2011) MicroRNA-3148 modulates allelic expression of Toll-like receptor 7 variant associated with systemic lupus erythematosus. PLOS Genet 9(2):e1003336
Petri M, Orbai AM, Alarcon GS, Gordon C, Merrill JT, Fortin PR, Bruce IN, Isenberg D, Wallace DJ, Nived O, Sturfelt G, Ramsey-Goldman R, Bae SC, Hanly JG, Sánchez-Guerrero J, Clarke A, Aranow C, Manzi S, Urowitz M, Gladman D, Kalunian K, Costner M, Werth VP, Zoma A, Bernatsky S, Ruiz-Irastorza G, Khamashta MA, Jacobsen S, Buyon JP, Maddison P, Dooley MA, van Vollenhoven RF, Ginzler E, Stoll T, Peschken C, Jorizzo JL, Callen JP, Lim SS, Fessler BJ, Inanc M, Kamen DL, Rahman A, Steinsson K, Franks AG Jr, Sigler L, Hameed S, Fang H, Pham N, Brey R, Weisman MH, McGwin G Jr, Magder LS (2012) Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum 64:2677–2686
Bombardier C, Gladman DD, Urowitz MB, Caron D, Chang CH (1992) Derivation of the SLEDAI. A disease activity index for lupus patients. The Committee on Prognosis Studies in SLE. Arthritis Rheum 35:630–640
Scofield RH, Bruner GR, Namjou B, Kimberly RP, Ramsey-Goldman R, Petri M, Reveille JD, Alarcón GS, Vilá LM, Reid J, Harris B, Li S, Kelly JA, Harley JB (2008) Klinefelter’s syndrome (47, XXY) in male systemic lupus erythematosus patients: support for the notion of a gene-dose effect from the X chromosome. Arthritis Rheum 58(8):2511–2517
Kawasaki A, Furukawa H, Kondo Y, Ito S, Hayashi T, Kusaoi M, Matsumoto I, Tohma S, Takasaki Y, Hashimoto H, Sumida T, Tsuchiya N (2011) TLR7 single-nucleotide polymorphisms in the 3′ untranslated region and intron 2 independently contribute to systemic lupus erythematosus in Japanese women: a case-control association study. Arthritis Res Ther 13:R41
Laska MJ, Troldborg A, Hansen B, Stengaard-Pedersen K, Junker P, Nexø BA, Voss A (2014) Polymorphisms within Toll-like receptors are associated with systemic lupus erythematosus in a cohort of Danish females. Rheumatology 53(1):48–55
Horton CG, Pan Z‑J, Farris AD (2010) Targeting Toll-like receptors for treatment of SLE. Mediators Inflamm:9. doi:10.1155/2010/498980
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no competing interest. The authors alone are responsible for the content and writing of the paper.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Redaktion
U. Müller-Ladner, Bad Nauheim
U. Lange, Bad Nauheim
The authors have no financial or proprietary interest in any product mentioned in this paper.
Rights and permissions
About this article
Cite this article
Raafat, I.I., El Guindy, N., Shahin, R.M.H. et al. Toll-like receptor 7 gene single nucleotide polymorphisms and the risk for systemic lupus erythematosus: a case-control study. Z Rheumatol 77, 416–420 (2018). https://doi.org/10.1007/s00393-017-0283-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00393-017-0283-7
Keywords
- Lupus nephritis
- Real time polymerase chain reaction TaqMan-based allelic discrimination assay
- Single nucleotide polymorphisms (SNPs)
- Systemic lupus erythematosus (SLE)
- Toll-like receptor 7 (TLR7)