Abstract
Objective
Growth hormone (GH) and insulin-like growth factor-1 (IGF-1) play a major role in bone homeostasis. In this study, we aimed to assess bone mineral density (BMD) in active acromegaly.
Materials and methods
A total of 29 patients with active acromegaly (age 46.10 ± 13.27 years; body mass index [BMI]: 29.51 ± 4.91 kg/m2) and 42 healthy individuals matched for age and BMI (age: 40.35 ± 11.74 years; BMI: 28.18 ± 7.35 kg/m2) were included in the study. BMD was measured by DXA.
Results
The mean levels of GH and IGF-1 were found to be 12.61 ± 11.34 ng/ml and 676.47 ± 316.19 ng/ml in acromegaly, respectively, while the mean levels of GH and IGF-1 were found to be 0.59 ± 0.81 ng/ml (p = 0.0001) and 178.17 ± 57.11 ng/ml (p = 0.0001) in the control group, respectively. Only total hip t‑score was determined to be significantly lower in acromegaly compared to the control group (p = 0.037). No significant differences were found between the other parameters in DXA and only a positive correlation was found between IGF-1 levels and L1–L4 BMD (r = 0.259, p = 0.029).
Conclusions
Although GH and IGF-1 levels were increased in acromegalic patients, no significant difference was found in terms of vertebral BMD. Only hip t‑scores were found to be lower in acromegalic patients, but this low hip t‑score did not reach the osteopenic level. The positive correlation between IGF-1 and lumbar vertebral BMD suggested a more prominent effect of IGF-1 on BMD compared to GH.
Zusammenfassung
Ziel
Wachtumshormon („growth hormone“, GH) und der insulinähnliche Wachstumsfaktor 1 („insulin-like growth factor 1“, IGF-1) spielen eine wichtige Rolle bei der Knochenhomöostase. Ziel dieser Studie war es, die Knochenmineraldichte („bone mineral density“, BMD) bei aktiver Akromegalie zu beurteilen.
Material und Methoden
Neunundzwanzig Patienten mit aktiver Akromegalie (Alter: 46,10 ± 13,27 Jahre; Body-Mass-Index [BMI]: 29,51 ± 4,91 kg/m2) und 42 gesunde Personen mit entsprechendem Alter und BMI (Alter: 40,35 ± 11,74 Jahre; BMI: 28,18 ± 7,35 kg/m2) wurden in die Studie eingeschlossen. Die BMD wurde mittels DXA gemessen.
Ergebnisse
Die mittleren GH- und IGF-1-Serumspiegel bei Akromegalie betrugen 12,61 ± 11,34 ng/ml bzw. 676,47 ± 316,19 ng/ml, während die mittleren GH- und IGF-1-Serumspiegel in der Kontrollgruppe bei 0,59 ± 0,81 ng/ml (p = 0,0001) bzw. 178,17 ± 57,11 ng/ml (p = 0,0001) lagen. Der T‑Score der Gesamthüfte war signifikant niedriger bei Akromegalie im Vergleich zur Kontrollgruppe (p = 0,037). Es wurden keine signifikanten Unterschiede zwischen den anderen DXA-Parametern gefunden, und zwischen den IGF-1-Serumspiegeln und der BMD in L1–L4 wurde lediglich eine positive Korrelation festgestellt (r = 0,259, p = 0,029).
Schlussfolgerungen
Obwohl bei Patienten mit Akromegalie erhöhte GH- und IGF-1-Serumspiegel festgestellt wurden, gab es keine Hinweise auf signifikante Unterschiede bezüglich der BMD der Wirbelsäule. Der T‑Score der Hüfte war bei Patienten mit Akromegalie niedriger. Diese niedrigen T‑Score-Werte der Hüfte erreichten jedoch kein osteopenisches Ausmaß. Die positive Korrelation zwischen IGF-1 und der BMD im Lendenwirbelsäulenbereich zeigte, dass IGF-1 im Vergleich zu GH eine größere Auswirkung auf die BMD hat.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction and objective
Acromegaly is generally characterized by a growth hormone (GH)-secreting pituitary adenoma [1]. Most of the patients have been exposed to GH in supraphysiological doses for years (7–10 years) before the diagnosis is established [2]. Growth hormone and insulin-like growth factor-1 (IGF-1) play a major role in bone homeostasis by increasing bone mass and linear bone growth [3]. The anabolic effects of GH on bones are well-known [4]. Although GH stimulates both osteoblastic and osteoclastic activities, it particularly increases bone formation [4–6]. Besides, IGF-1 which mediates peripheral effects of GH, increases bone formation by stimulating osteoblasts [7]. Both bone formation and resorption are increased in acromegalic patients with excessive secretion of GH [7, 8]. Interestingly, unlike acromegaly, hypopituitary patients with GH deficiency are known to have bone loss [9]. However it has not been possible to clearly explain yet the effects of GH excess on bone mineralization.
Traditionally, acromegaly has been known as a cause of secondary osteoporosis [10]. In the earlier studies, one attempted to explain the pathogenesis by hypercalciuria and negative calcium balance [11, 12]. However, conflicting data related to the anabolic effects of GH on bone metabolism render the issue more complicated. In patients with active acromegaly, increased cortical bone mass, as well as increased, decreased or unaffected trabecular bone mass depending also on gonadal functions were reported in a limited number of studies in medical literature [13–15]. An increased trabecular bone mass was reported by Scillitani et al. [16] in eugonadal patients with active acromegaly. In acromegaly, in addition to conflicting findings in bone mineral density, it is not clear whether or not the risk of fracture is increased in bones exposed to excessive amounts of GH/IGF-1.
In this study we aimed to assess bone mineral density (BMD) in active acromegalic patients with known high GH and/or IGF-1 levels.
Materials and methods
Twenty-nine patients with newly diagnosed active acromegaly applying to endocrinology outpatient clinic of Erzurum Regional Training and Research Hospital (mean age 46.10 ± 13.27 years and mean body mass index [BMI]: 29.51 ± 4.91 kg/m2) and 42 healthy individuals of age and BMI matching (mean age 40.35 ± 11.74 years; mean BMI: 28.18 ± 7.35 kg/m2) were included into the study (Table 1). All patients presented with symptomatic acromegaly. Baseline serum levels of glucose, calcium, phosphorus, GH, IGF-1, follicle-stimulating hormone (FSH), luteinizing hormone (LH), estradiol, progesterone, total testosterone, cortisol, adrenocorticotrophic hormone (ACTH), thyroid stimulating hormone (TSH), dehydroepiandrosteron sulphate (DHEA‑S), and prolactin were measured. All the patients underwent oral glucose tolerance test and GH suppression test after 12 h of fasting, performed by the intake of 75 g of glucose between 8 and 9 o’clock (0 min) in the morning and during the oral glucose tolerance testing, serum glucose and GH levels were measured at 0, 30, 60, 90, 120 min. The diagnosis of acromegaly was established according to clinical findings as well as IGF-1 levels higher than the reference range adjusted for age and sex as well as unsuppressed GH during GH suppression test [17]. The GH values were not suppressed to less than 1 ng/ml in any patient in the acromegaly group during the GH suppression test [17]. Serum prolactin levels were within normal range. At the time of oral glucose tolerance test (OGTT), 3 patients had diabetes mellitus; however, impaired glucose tolerance was detected in 5 patients in the acromegaly group. In addition, all patients in the acromegaly group had normal gonadal and adrenal functions or received hormone replacement therapy for the treatment of hypopituitarism during the previous 6 months. Other risk factors for secondary osteoporosis were ruled out. No patient was taking any medication that might influence the BMD. Those patients on medication due to known osteoporosis, patients on medications that might affect bone metabolism, those with coexisting endocrinological disorder such as polycystic ovary syndrome, hyperthyroidism, hyperparathyroidism, patients with a history of chronic alcohol consumption, as well as patients with chronic liver diseases and chronic renal diseases were excluded from the study. A written informed consent form was obtained from each subject.
Anthropometric measurements
Body weights (kg) and heights (cm) were measured without shoes. BMI was expressed as weight (kilograms) per height (meters) squared.
Dual energy x‑ray absorptiometry (DXA)
In our study, the femur and lumbar vertebral (L1–L4) BMD values were measured by DXA (Stratos-Dexa digital fast beam whole body densitometer). The patients were placed on the imaging table in the supine position in accordance with technique of DXA. The bone mineral density measurements of proximal femur were obtained from various areas including femur neck, intertrochanteric area, trochanter, and Ward’s triangle. Total femoral BMD was calculated by using mean BMD of the femoral regions. Posteroanterior images of the lumbar spine vertebral bodies (L1–L4) were calculated. A t-score (the difference of standard deviation [SD], is calculated according to the peak bone mass of young adults from the same race and sex) and z‑score (the difference of standard deviation [SD], is calculated in the healthy controls from the same race, age, and sex). A t-score between −1 and −2.5 SD is defined as osteopenia. A t-score of ≤−2.5 SD is defined as osteoporosis. Bone mineral density was calculated by dividing the bone mineral content (BMC) to the estimated areas of scanned images (BMD = BMC/area [g/cm 2]).
Biochemical analysis
Serum levels of glucose, calcium, phosphorus, 25-OH vitamin D, GH, IGF-1 were measured at baseline conditions following 12 hours of fasting. Serum glucose levels and GH secretion were evaluated in the blood samples obtained at 30 min intervals at 30, 60, 90 and 120 min. In addition, hormone profiles were determined by the measurements of FSH, LH, cortisol, progesterone, estradiol, cortisol, TSH, prolactin, and DHEA-S in baseline conditions at the 0 min of the OGTT. All the blood samples were subsequently centrifuged, the serum was separated and the serum samples were stored at −20 ºC until analysis. Glucose levels were determined by using enzymatic colorimetric method (Beckman Coulter AU2700 plus). Serum total testosterone, progesterone, estradiol, cortisol, prolactin, and DHEA-S levels were determined by enzyme chemiluminescence (Siemens IMMULITE 2000 xpi, Advia Centaur® XP Immunoassay System). FSH, LH, TSH, and 25-OH vitamin D levels were determined by chemiluminescence assay (Siemens IMMULITE 2000 xpi, Advia Centaur® XP Immunoassay System [Siemens Medical Solutions Diagnostics Tarrylown NY 10591-5097 USA]). Serum human GH levels were measured with enzyme chemiluminescence assay by using Siemens IMMULITE 2000 xpi (Diagnostic Products Corporation, Los AngelesUSA). Serum IGF-1 levels were measured with enzyme immunoassay Siemens IMMULITE 2000 xpi (Siemens Healthcare Diagnostics Inc., Los Angeles, USA). Serum phosphorus levels were measured through photometric UV test by Beckman Coulter AU 2700 plus (Beckman Coulter, Inc., Fullerton, © Copyright 2007 Beckman Coulter, Inc. Printed in U.S.A.). Serum calcium levels, however, were measured through photometric color test by Beckman Coulter AU 2700 plus (Beckman Coulter, Inc., Fullerton, © Copyright 2007 Beckman Coulter, Inc. Printed in U.S.A.).
Statistical analysis
SPSS statistics 17 was used for statistical analysis. All of the results were expressed as mean ± standard deviation (SD). Differences the between groups were tested by independent student’s t test. The relationship between variables was evaluated by Pierson’s correlation test. A p value less than 0.05 was considered statistically significant.
Results
The mean serum levels of GH and IGF-1 were 12.61 ± 11.34 ng/ml and the serum 676.47 ± 316.19 ng/ml, respectively, in the acromegaly group. On the other hand, the mean serum level of GH and IGF-1 in the control group were 0.59 ± 0.81 ng/ml and 178.17 ± 57.11 ng/ml, respectively. Both serum GH levels (p = 0.0001) and IGF-1 levels (p = 0.0001) were found significantly elevated in acromegaly group. The hormonal profiles of the study groups are shown in Table 2. The gonadal status in acromegaly group was not different from control subjects.
The mean total hip BMD was determined as 1.01 ± 0.16 g/cm2, t‑score as −0.33 ± 1.16, z score as 0.08 ± 1.05; the mean total L1–L4 BMD was found to be 0.98 ± 0.14 g/cm2, t‑score −0.87 ± 1.18, and z‑score −0.28 ± 1.30 in the acromegaly group. The mean total hip BMD was determined as 1.00 ± 0.08 g/cm2, t‑score as 0.17 ± 0.84, z score as 0.39 ± 0.83; the mean total L1–L4 BMD was 0.94 ± 0.12 g/cm2, t‑score −1.00 ± 1.11, and z‑score −0.55 ± 1.03 in the control group. Only total hip t‑score was determined to be significantly lower in the acromegaly group compared to the control group (p = 0.037). No statistically significant differences were found between the other parameters. All DXA results are shown in Table 3.
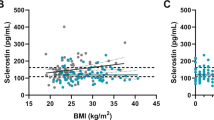
Using Pearson’s correlation analysis, a positive correlation was only found between the serum IGF-1 levels and L1–L4 BMD (r = 0.259, p = 0.029) in our study population (Fig. 1). No significant correlation was found between the serum GH levels and DXA parameters.
Discussion
GH and its peripheral modulator IGF-1 play major roles on bone mineralization. Our study revealed that BMD was not affected in patients with active acromegaly apart from femoral mineral density. Although our data indicated that only total hip t‑score was statistically significantly lower in acromegaly compared to the control group, this decrease was not yet at the level of osteoporosis or osteopenia. Certain previous studies in the medical literature reported increased bone turnover [18] and decreased BMD in acromegaly [19]; however, in a study conducted by Mazziotti G et al. [20], BMD was found normal in acromegalic males. The presence of hypogonadism in acromegalic patients may be due to the difference between the studies. In our study, hypogonadism was not present in patients with acromegaly except three patients, and these patients took hormone replacement therapy for at least 6 months.
It is also well known that BMD is not a good indicator of fracture risk [21]. In spite of a normal BMD in postmenopausal active acromegaly, the development of asymptomatic vertebral fractures has been reported earlier [22]. The negative influence on trabecular bone in acromegaly was particularly pointed out by Madeira M et al. [23]; however, no hip fracture was detected in our study in spite of statistically significantly decreased femoral t‑score. In a study investigating osteoporosis and the prevalence of vertebral fracture in acromegalic patients, Padova G et al. [11] revealed the presence of osteoporosis and osteopenia at a rate of 58–74 %, by using DXA and quantitative ultrasound [11]. The results of that study showed a decreased BMD in femoral region. Ostepenia was reported for the first time in that study, in a similar way to our study. Padova G et al. [11] suggested that this situation had developed independently from the disease activity or hypogonadism.
In a restricted number of studies investigating fracture risk in acromegalic patients, vertebral fractures were detected even in acromegalic patients with a normal t‑score [11]. The vertebral fracture risk in acromegaly was reported as 59 % by Vassenaar et al. [24]. In this study, the subgroup analysis also revealed that the result developed independent from BMD. Therefore, more advanced methods are required in the investigation of bone metabolism in acromegaly. The bone turnover rate is known to increase in chronic GH/IGF-1 excess [11]. Furthermore, bone resorption markers are also known to increase relatively to bone formation markers, and actually these markers may be used in clinical practice in order to reflect the degree of bone loss [11, 25]. In our study, bone turnover markers could not be studied due to technical reasons.
According to our findings, we detected only a slight decrease in femoral t‑score even no level of osteopenia. Chronic and long-standing GH/IGF-1 excess in acromegaly may lead to unfavorable changes in the femoral microarchitecture. Our findings may be speculated as the requirement of further studies where the cortical bone density of other bones including femur is evaluated by using histomorphometry, QTC, or MRI, even if DXA may give a clue for fracture risk, it cannot be used in the assessment of bone quality.
Hübsch et al. [26] reported that BMD was found elevated in femoral neck and Ward’s triangle due to the anabolic effects of GH; however, osteoporosis was not detected in the radiological examinations. Nevertheless, in acromegaly, mineralization may also vary among the bones. When Jockenhövel et al. [27] evaluated cortical and trabecular bones separately in acromegalic patients by using peripheral CT and specific scanner (Stratec XCT 900), they found a prominent increase in cortical BMD but no difference was found in spinal BMD [27]. However different they might be from other studies, cortical bone measurements were obtained from ultradistal radius in that study [27]. This situation may be explained by the effects of GH/IGF-1 on osteoclasts. GH stimulates both recruitment and activity of osteoclasts. On the other hand, Ueland et al. [28] asserted an increase in osteoclast like cells. Moreover, GH and IGF-1 stimulate both osteoblasts and osteoclasts [28].
The unique positive correlation was found between lumbal BMD and IGF-1 levels in our study suggesting the more prominent role of IGF-1 in bone mineral density in comparison to GH. The effects of GH excess on the axial skeleton differ from its effects on appendicular skeleton. While the vertebral density has been reported as reduced or unchanged, certain studies have reported an increased mineralization at forearm bone [8, 11, 12, 29]. IGF-1 regulates the differentiation of osteoclasts [30] and osteoblasts [31] at the cellular level. Low BMD was reported in mice with knock-out IGF-1 gene [32]. The detection of impaired chondrocyte maturation and short femur length in mice with deleted IGF-1 gene accentuates the presence of the role of IGF-1 in chondrocyte differentiation [32]. The role of IGF-1 in cortical bone may be more important than its role in trabecular bone [33]. The osteoporotic fracture risk was reported as 3.1-fold higher in postmenopausal women with low IGF-1 levels [34, 35]. However, one year of treatment with low dose of IGF-1 did not increase BMD in healthy postmenoposal women [34, 36]. In addition, it is not clear that longer treatments or higher doses might be beneficial. Further studies are required to be carried out for the effects of chronic IGF-1 excess on cortical and trabecular bone in acromegaly. A better understanding of the issue may render possible the development of new agents concerning the GH/IGF-1 axis in the treatment of osteoporosis.
Likewise, Perrini et al. [37] showed that the decrease of GH levels with the age resulted in the reduced bone mass. The impaired GH axis may be important in postmenopausal and senile osteoporosis [11]. In acromegaly, the decrease of GH and/or IGF-1 levels following the treatment may influence bone mineralization in a similar way. However, our study was a cross-sectional study, and post-treatment bone mineral density measurements were not performed. Further studies are required on this issue. In addition, somatostatin analogues administered in the treatment of acromegaly may also affect bone mineralization.
In conclusion, hip t‑scores were found to be lower in acromegalic patients in comparison to the control patients. Although GH and IGF-1 levels were found elevated in acromegalic patients, no difference was found between the acromegalic patients and control patients in spinal BMD. However, the positive correlation that was determined between serum IGF-1 levels and lumbal BMD suggested the more prominent effect of IGF-1 on bone mineral density in comparison to GH.
References
Melmed S (2009) Acromegaly pathogenesis and treatment. J Clin Invest 119(11):3189–3202
Rajasoorya C, Holdaway IM, Wrightson P et al (1994) Determinants of clinical outcome and survival in acromegaly. Clin Endocrinol (Oxf) 41:95–102
Ahmed SF, Farquharson C (2010) The effect of GH and IGF1 on linear growth and skeletal development and their modulation by SOCS proteins. J Endocrinol 206(3):249–259
Kasukawa Y, Miyakoshi N, Mohan S (2004) The anabolic effects of GH/IGF system on bone. Curr Pharm Des 10(21):2577–2592
Chihara K, Sugimoto T (1997) The action of GH/IGF-I/IGFBP in osteoblasts and osteoclasts. Horm Res 48(Suppl 5):45–49
Ueland T, Fougner SL, Godang K, Schreiner T, Bollerslev J (2006) Serum GH and IGF-I are significant determinants of bone turnover but not bone mineral density in active acromegaly: a prospective study of more than 70 consecutive patients. Eur J Endocrinol 155(5):709–715
DiGirolamo DJ, Mukherjee A, Fulzele K, Gan Y, Cao X, Frank SJ, Clemens TL (2007) Mode of growth hormone action in osteoblasts. J Biol Chem 282(43):31666–31674
Biermasz NR, Hamdy NA, Pereira AM, Romijn JA, Roelfsema F (2005) Long-term maintenance of the anabolic effects of GH on the skeleton in successfully treated patients with acromegaly. Eur J Endocrinol 152(1):53–60
White HD, Ahmad AM, Durham BH, Joshi AA, Fraser WD, Vora JP (2011) Effect of oral phosphate and alendronate on bone mineral density when given as adjunctive therapy to growth hormone replacement in adult growth hormone deficiency. J Clin Endocrinol Metab 96(3):726–736
Killinger Z, Kužma M, Sterančáková L, Payer J (2012) Osteoarticular changes in acromegaly. Int J Endocrinol 2012:Article ID 839282. doi:10.1155/2012/839282
Padova G, Borzì G, Incorvaia L, Siciliano G, Migliorino V, Vetri M, Tita P (2011) Prevalence of osteoporosis and vertebral fractures in acromegalic patients. Clin Cases Miner Bone Metab 8(3):37–43
Colao A, Ferone D, Marzullo P, Lombardi G (2004) Systemic complications of acromegaly: epidemiology, pathogenesis and management. Endocr Rev 25:102–152
Morselli LL, Manetti L, Cosci C et al (2006) Bone and joint alterations in acromegaly. J Orthop Traumatol 7:169–175
Ho PJ, Fig LM, Barkan AL, Shapiro B (1992) Bone mineral density of the axial skeleton in acromegaly. J Nucl Med 33(9):1608–1612
Kotzmann H, Bernecker P, Hübsch P, Pietschmann P, Woloszczuk W, Svoboda T, Geyer G, Luger A (1993) Bone mineral density and parameters of bone metabolism in patients with acromegaly. J Bone Miner Res 8(4):459–465
Scillitani A, Battista C, Chiodini I, Carnevale V, Fusilli S, Ciccarelli E, Terzolo M, Oppizzi G, Arosio M, Gasperi M, Arnaldi G, Colao A, Baldelli R, Ghiggi MR, Gaia D, Di Somma C, Trischitta V, Liuzzi A (2003) Bone mineral density in acromegaly: the effect of gender, disease activity and gonadal status. Clin Endocrinol (Oxf) 58(6):725–731
Katznelson L, Atkinson JL, Cook DM, Ezzat SZ, Hamrahian AH, Miller KK, AACE Acromegaly Task Force (2011) American Association of Clinical Endocrinologists medical guidelines for clinical practice for the diagnosis and treatment of acromegaly–2011 update: executive summary. Endocr Pract 17(4):636–646
Bolanowski M, Daroszewski J, Medraś M, Zadrozna-Sliwka B (2006) Bone mineral density and turnover in patients with acromegaly in relation to sex, disease activity, and gonadal function. J Bone Miner Metab 24(1):72–78
Giuseppina P, Graziella B, Laura I et al (2011) Prevalence of osteoporosis and vertebral fractures in acromegalic patients. Clin Cases Miner Bone Metab 8(3):37–43
Mazziotti G, Bianchi A, Bonadonna S, Cimino V, Patelli I, Fusco A, Pontecorvi A, De Marinis L, Giustina A (2008) Prevalence of vertebral fractures in men with acromegaly. J Clin Endocrinol Metab 93(12):4649–4655
Unnanuntana A, Gladnick BP, Donnelly E, Lane JM (2010) The assessment of fracture risk. J Bone Joint Surg Am 92(3):743–753
Bonadonna S, Mazziotti G, Nuzzo M, Bianchi A, Fusco A, De Marinis L, Giustina A (2005) Increased prevalence of radiological spinal deformities in active acromegaly: a cross-sectional study in postmenopausal women. J Bone Miner Res 20(10):1837–1844
Madeira M, Neto LV, de Paula Paranhos Neto F, Barbosa Lima IC, Carvalho de Mendonça LM, Gadelha MR, Fleiuss de Farias ML (2013) Acromegaly has a negative influence on trabecular bone, but not on cortical bone, as assessed by high-resolution peripheral quantitative computed tomography. J Clin Endocrinol Metab 98(4):1734–1741
Wassenaar MJ, Biermasz NR, Hamdy NA, Zillikens MC, van Meurs JB, Rivadeneira F, Hofman A, Uitterlinden AG, Stokkel MP, Roelfsema F, Kloppenburg M, Kroon HM, Romijn JA, Pereira AM (2011) High prevalence of vertebral fractures despite normal bone mineral density in patients with long-term controlled acromegaly. Eur J Endocrinol 164(4):475–483
Ezzat S, Melmed S, Endres D, Eyre DR, Singer FR (1993) Biochemical assessment of bone formation and resorption in acromegaly. J Clin Endocrinol Metab 76(6):1452–1457
Hübsch P, Kotzmann H, Svoboda T, Kainberger FM, Bankier A, Seidl G (1993) Bone density of the lumbar spine and femur in acromegaly. Radiologe 33(8):457–461
Jockenhövel F, Rohrbach S, Deggerich S, Reinwein D, Reiners C (1996) Differential presentation of cortical and trabecular peripheral bone mineral density in acromegaly. Eur J Med Res 1(8):377–382
Ueland T (2005) GH/IGF-I and bone resorption in vivo and in vitro. Eur J Endocrinol 152(3):327–332
Jean Ho P, Lorraine M, Barkan A, Shapiro B (1992) Bone mineral density of the axial skeleton in acromegaly. J Nucl Med 33:1608–1612
Wang Y, Nishida S, Elalieh HZ, Long RK, Halloran BP, Bikle DD (2006) Role of IGF-I signaling in regulating osteoclastogenesis. J Bone Miner Res 21(9):1350–1358
Neve A, Corrado A, Cantatore FP (2011) Osteoblast physiology in normal and pathological conditions. Cell Tissue Res 343(2):289–302
Yakar S, Courtland HW, Clemmons D (2010) IGF-1 and bone: new discoveries from mouse models. J Bone Miner Res 25(12):2543–2552
Bikle D, Majumdar S, Laib A, Powell-Braxton L, Rosen C, Beamer W, Nauman E, Leary C, Halloran B (2001) The skeletal structure of insulin-like growth factor I‑deficient mice. J Bone Miner Res 16(12):2320–2329
Bach LA (2004) The insulin-like growth factor system: towards clinical applications. Clin Biochem Rev 25(3):155–164
Garnero P, Sornay-Rendu E, Delmas PD (2000) Low serum IGF-1 and occurrence of osteoporotic fractures in postmenopausal women. Lancet 355(9207):898–899
Friedlander AL, Butterfield GE, Moynihan S, Grillo J, Pollack M, Holloway L, Friedman L, Yesavage J, Matthias D, Lee S, Marcus R, Hoffman AR (2001) One year of insulin-like growth factor I treatment does not affect bone density, body composition, or psychological measures in postmenopausal women. J Clin Endocrinol Metab 86(4):1496–1503
Perrini S, Laviola L, Carreira MC, Cignarelli A, Natalicchio A, Giorgino F (2010) The GH/IGF1 axis and signaling pathways in the muscle and bone: mechanisms underlying age-related skeletal muscle wasting and osteoporosis. J Endocrinol 205(3):201–210
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S. Tuzcu, Ş.A. Durmaz, A. Carlıoglu, Z. Demircan, A. Tuzcu, C. Beyaz and A. Tay confirm that they have no conflict of interest.
Authors confirm that all procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Redaktion
U. Müller-Ladner, Bad Nauheim
U. Lange, Bad Nauheim
Rights and permissions
About this article
Cite this article
Tuzcu, S., Durmaz, Ş.A., Carlıoğlu, A. et al. The effects of high serum growth hormone and IGF-1 levels on bone mineral density in acromegaly. Z Rheumatol 76, 716–722 (2017). https://doi.org/10.1007/s00393-016-0171-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00393-016-0171-6