Abstract
Background
Patients with atherothrombotic risk are at high hazard of ischemic events. Preventive medicine plays a major role in modifying their outcomes. Whether the choice of a BP-SES or DP-EES can contribute to the occurrence of events remains unclear. We sought to investigate the outcomes of patients with higher atherothrombotic risk (H-ATR) versus lower atherothrombotic risk (L-ATR) undergoing percutaneous coronary intervention (PCI) with either bioresorbable-polymer sirolimus-eluting stent (BP-SES) or durable-polymer everolimus-eluting stent (DP-EES).
Methods
Patients (n = 2361) from BIOFLOW-II, -IV, and -V randomized trials were categorized into H-ATR vs. L-ATR. L-ATR patients had ≤ 1 and H-ATR ≥ 2 of the following criteria: presentation in ACS, diabetes mellitus, previous myocardial infarction, previous PCI/CABG, or previous stroke. Endpoints were target lesion failure (TLF: cardiac death, target-vessel myocardial infarction [TV-MI], target lesion revascularization [TLR]) and stent thrombosis (ST) at three years.
Results
H-ATR patients (n = 1023) were more morbid than L-ATR patients (n = 1338). TLF rate was significantly higher in H-ATR patients as compared with L-ATR (11.6% vs. 7.0%; HR 1.67, 95% CI 1.27–2.20, p < 0.0001). With BP-SES TLF rates were numerically lower as compared with DP-EES in H-ATR (10.5% vs. 13.5%; HR 0.78, 95% CI 0.54–1.14, p = 0.20) and significantly lower in L-ATR (5.6% vs. 9.8%; HR 0.57, 95% CI 0.38–0.85, p = 0.006).
Conclusion
In the era of newer-generation DES, patients with H-ATR still are at hazard for ischemic events. Patients with BP-SES had lower TLF rates as compared with DP-EES, most consistent in L-ATR whereas in H-ATR patients most probably secondary preventive strategies are of higher value.
Clinical trial registration
Clinicaltrial.gov. NCT01356888, NCT01939249, NCT02389946. https://clinicaltrials.gov/show/NCT01356888, https://clinicaltrials.gov/show/NCT01939249, https://clinicaltrials.gov/show/NCT02389946.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease is the leading cause of mortality worldwide [1]. Primary and secondary prevention is the major strategy in these patients with atherothrombotic risk (ATR) to reduce the hazard of clinical events. A change in dietary behavior in patients with metabolic disorders along with physical exercise is a cornerstone in preventive medicine [2]. Modern antidiabetic [3] and cholesterol lowering agents [4, 5] have significantly reduced mortality and a therapy with potent antiplatelet inhibitors demonstrated to reduce mortality after an acute coronary syndrome as well [6, 7]. However, whether the choice of a specific stent platform during percutaneous coronary intervention (PCI) in patients with ATR can modify the clinical outcome is not well studied.
Recently, the BIOFLOW-V trial [8] demonstrated a lower rate of target lesion failure (TLF) and stent thrombosis (ST) with an ultra-thin strut bioresorbable-polymer sirolimus-eluting stent (BP-SES) as compared with a thin-strut durable-polymer everolimus-eluting stent (DP-EES).
In the present study from a pooled dataset of the randomized BIOFLOW-II [9], BIOLFOW-IV [10], and BIOFLOW-V [8] trials we sought to investigate the long-term clinical outcomes of patients with higher atherothrombotic risk (H-ATR) and with lower atherothrombotic risk (L-ATR) undergoing PCI with newer generation drug eluting stents (DES) and whether the outcomes can be modified by the choice of a BP-SES or DP-EES.
Methods
Study population and design
In this post-hoc analysis from the multicenter, randomized BIOFLOW-II, BIOFLOW-IV, and BIOFLOW-V trials data were pooled at the patient-level. The trials compared PCI with DP-EES (Xience, Abbott, Santa Clara, CA) versus BP-SES (Orsiro, Biotronik AG, Bülach, Switzerland) in de novo native coronary artery lesions. The study designs were previously described and are available on ClinicalTrials.gov (NCT01356888, NCT01939249, NCT02389946). The inclusion and exclusion criteria were previously reported [8,9,10,11,12].
The trials complied with the provisions of the Declaration of Helsinki and were approved by the institutional review board or ethics committee at each enrolling site. Eligible patients signed written informed consent. An independent clinical events committee adjudicated all clinical endpoints. All angiographic data were analyzed by an independent core laboratory (MedStar Cardiovascular Research Network, Angiographic Core Laboratory, Washington DC, USA). The trials were funded by Biotronik. The authors (R.H., R.T., G.R.) had access to the data and are responsible for the analyses and drafting of the manuscript.
For this study, we divided the population into patients with lower atherothrombotic risk (L-ATR) versus high atherothrombotic risk (H-ATR). L-ATR was defined as the presence of ≤ 1 and H-ATR as the presence of ≥ 2 of the following five characteristics: presentation in ACS, diabetes mellitus, previous myocardial infarction, previous PCI or CABG, or previous stroke. This definition [13, 14] is based on the criteria used in the CHARISMA trial [15] and the clinical variables available in the pooled data set.
Study endpoints
The main clinical endpoints were target lesion failure (TLF) at three years (a composite of cardiac death, target-vessel myocardial infarction [TV-MI], or ischemia-driven target lesion revascularization [TLR]) and definite or probable stent thrombosis (ST; according to the Academic Research Consortium criteria [ARC]) [16].
Periprocedural MI was defined according to the modified ARC criteria as a troponin, or creatine kinase myocardial band (CK-MB) measured within 48 h of the interventional procedure elevated > 3 times above the upper normal limit of normal. Spontaneous MI was defined as any troponin or CK-MB elevation above the upper limit of normal with associated ischemic symptoms, new electrocardiographic abnormalities suggestive of ischemia, or new development of imaging evidence of infarction. Ischemia-driven revascularization was defined as any repeat revascularization of the target lesion or vessel due to either ischemic symptoms or abnormal coronary physiologic study and ≥ 50% coronary stenosis by quantitative angiography; or any revascularization of a ≥ 70% diameter stenosis. Cardiac death was any death due to any proximate cardiac cause, unwitnessed death, or death of unknown cause.
Statistical methods
Patient-level data were pooled in one dataset. Continuous variables were summarized as mean ± SD or as medians with lower and upper quartile and compared using two-sided t-test or the nonparametric Wilcoxon rank-sum test. Categorical variables were summarized as frequencies and percentages and were compared using the chi-square or Fischer’s exact test. The clinical endpoints were compared using the time-to-event Kaplan–Meier estimates and Cox regression. For calculation of predictors of TLF and TV-MI a Cox regression analysis was performed using the following co-variables: age, BMI, gender, hypertension, hyperlipidemia, smoker, renal disease, reference vessel diameter ≤ 2.75 mm. Additionally the stent (DP-ESS vs BP-SES) and atherothrombotic risk were forced into the analysis. The treatment effect associated with BP-SES or DP-EES with H-ATR or L-ATR was calculated from the Cox regression analysis with a p value for interaction. All analyses were performed using SAS, version 9.4 (SAS Institute, Cary, NC, USA). A p value of less than 0.05 was established as the level of statistical significance.
Results
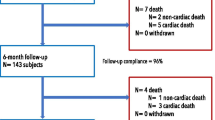
Out of 2361 patients, 1023 patients were categorized as H-ATR (43%) and 1338 patients as L-ATR (57%). Follow-up at three years was complete in 92.5% of H-ATR patients and 94.4% of L-ATR patients (p = 0.063). Both cohorts were similar in age and gender but H-ATR patients were more morbid. H-ATR patients particularly had more prior myocardial infarctions (Table 1). Lesion and procedural characteristics are listed in Table 2. Remarkably, the rate of complex lesions was not different between the H-ATR and L-ATR patients. L-ATR patients had larger reference diameters in their treated lesions.
Figure 1 and Table 3 present the clinical outcomes at three years. The TLF rate was significantly higher in H-ATR patients as compared with L-ATR (11.6% vs. 7.0%, p Log Rank < 0.0002; HR 1.67, 95% CI 1.27–2.20, p < 0.0001). Moreover, all components of the endpoint i.e. the rates of TV-MI, clinically driven TLR, and cardiac death were significantly higher among H-ATR as compared with L-ATR patients. Definite or probable ST occurred in ten patients (1.0%) with H-ATR and in three patients (0.2%) with L-ATR (p Log Rank = 0.014) (suppl. Figure 1).
Clinical outcomes after three years in patients with higher atherothrombotic risk and lower atherothrombotic risk. Kaplan–Meier estimates for target lesion failure (A) and their components target-vessel myocardial infarction (B), clinical indicated target lesion revascularization (C), and cardiac death (D)
Patients with ≥ 2 risk factors were at significantly higher risk for ischemic events as compared with patients with 1 risk factor or with no risk factor (Fig. 2, suppl. Table 1). Definite or probable ST occurred in ten patients (1.0%) with ≥ 2 risk factors, in one patient (0.1%) with one risk factor, and in one patient (0.2%) with no risk factors (p Log Rank = 0.020) (suppl. Figure 2).
Among H-ATR patients, TLR rates were numerically lower for BP-SES compared with DP-EES (10.5% vs. 13.5%, p Log Rank = 0.196; HR 0.78, 95% CI 0.54–1.14, p = 0.20) and significantly lower in L-ATR patients with a BP-SES (5.6% vs. 9.8%, p Log Rank = 0.005; HR 0.57, 95% CI 0.38–0.85, p = 0.006) though with no interaction (pinteraction = 0.243). The rates of TV-MI were numerically lower with BP-SES as compared with DP-EES in H-ATR patients (6.0% vs. 7.3%, p Log Rank = 0.314; HR 0.78, 95% CI 0.48–1.28, p = 0.321) and significantly lower in L-ATR patients with a BP-SES (3.3% vs. 6.1%, p Log Rank = 0.017; HR 0.54, 95% CI 0.32–0.91, p = 0.02) still with no interaction (pinteraction = 0.308). The rates of clinically driven TLR, cardiac death, and ST did not significantly differ between the groups (Fig. 3, suppl. Table 2).
Clinical outcomes after three years in patients with higher atherothrombotic risk and lower atherothrombotic risk undergoing PCI with bioresorbable-polymer sirolimus-eluting stents or durable-polymer everolimus-eluting stents. Kaplan–Meier estimates for target lesion failure (A), target-vessel myocardial infarction (B), and clinical indicated target lesion revascularization (C)
The clinical outcomes of the different stent platforms in relationship with the increasing number of risk factors is demonstrated in Fig. 4 and suppl. Table 3. In patients with ≥ 2 risk factors the rates of TLF were numerically lower when a BP-SES was implanted. In patients with 1 risk factor TLF rates were significantly lower, and in L-ATR the TLF rates were numerically lower with BP-SES as compared with DP-EES.
Clinical outcomes after three years in patients with ≥ 2 risk factors, 1 risk factor, and without risk factors undergoing PCI with bioresorbable-polymer sirolimus-eluting stents or durable-polymer everolimus-eluting stents. Kaplan–Meier estimates for target lesion failure (A), target-vessel myocardial infarction (B), and clinical indicated target lesion revascularization (C)
After accounting for potential confounders, the use of BP-SES was independently associated with a reduced TLF rate (aHR 0.70, 95% CI 0.53–0.94, p = 0.017) and TV-MI rate (aHR 0.69, 95% CI 0.47–0.99, p = 0.045) (Suppl. Table 4).
Discussion
The main findings of this patient-level pooled analysis from the randomized BIOFLOW trials were the following: (1) patients with H-ATR still had higher rates of TLF in the era of newer-generation DES; (2) more risk factors resulted in higher TLF, TV-MI and TLR rates; (3) the favorable clinical outcome after implantation of BP-SES over DP-EES was observed among patients with H-ATR and L-ATR, but more consistent in the group with L-ATR.
Coronary stents were continuously improved. Early generation DES platforms were out of stainless steel which required thicker struts to reach sufficient radial strength. The Taxus stent strut thickness was 132 µm and the Cypher strut thickness was 140 µm. Next refinements were a more biocompatible or bioresorbable polymer with -limus drugs (e.g. everolimus or zotarolimus) and the reduction of strut thickness to 80–90 µm by using alloys such as cobalt nickel, platinum chromium or cobalt chromium. The reduction of strut thickness by using special alloys lead to greater stent flexibility and an improved deliverability. This allowed the treatment of more complex lesion subsets and consequently the treatment of older and more morbid patients. Thus, the proportion of patients with H-ATR will increase, and as seen in our analysis as well as in previous studies, patients with H-ATR are also at higher ischemic risk [13, 14], which makes this analysis of interest. Although newer-generation DES could dramatically improve clinical outcomes as compared with early-generation DES or bare-metal stents [17], their outstanding clinical performance plateaued and stent-related events still occur at a rate of approximately 2% per year [18]. Given this limitation, the role of preventive medicine increased in the last years and remarkable progress could be achieved. SGLT-2 inhibitors reduce ischemic events not only patients with diabetes [3]. In patients with dyslipidemia the LDL-cholesterol levels and consequently mortality can be reduced with PCSK-9 inhibitors if not sufficiently managed with statins [19]. A therapy with the potent antiplatelet inhibitors Prasugrel and Ticagrelor demonstrated to reduce mortality after an acute coronary syndrome as well [6, 7]. Whether newer-generation DES can also contribute to a reduction of ischemic events in this vulnerable patient subset with H-ATR is not well studied. Our analysis demonstrates that despite the refinements in newer-generation DES, they could not reduce the allover ischemic event rate in patients with H-ATR to similar event rates of patients with L-ATR. Remarkably, the angiographic lesion complexity was not increased in the H-ATR cohort, which indicates the dominance of metabolic and/or humoral factors as triggers of the ischemic events in these patients.
The Xience DP-EES has a thin strut design with 81 µm, durable polymer and is eluting everolimus. The Orsiro BP-SES is a further development with an ultra-thin strut design with 60 µm for the ≤ 3.0 mm diameter stents, with bioresorbable polymer and is sirolimus eluting. Ultra-thin strut sirolimus eluting stents have shown to reduce the risk of TLF in two large meta-analysis [20, 21]. Nevertheless, mortality was not significantly modified by the use of an ultra-thin strut DES. We could demonstrate that the improved clinical outcome of BP-SES vs DP-EES was present in patients with H-ATR and L-ATR, with a much larger relative risk reduction by BP-SES in L-ATR patients. Nevertheless, the test for interaction did not reach statistical significance. The lower rate of TLF was driven by lower rates of TV-MI. ST occurred most in patients with H-ATR and less frequent with BP-SES. The lower strut thickness might cause less vessel injury and less side branch coverage with a reduction of turbulences and regions of lower shear resulting in a decreased thrombogenicity [21]. It is possible that the superior clinical performance of the Orsiro BP-SES in patients with L-ATR, results from the fact that TV-MIs are more sensitive to the stent, which was implanted. On the other hand, in morbid patients the numerous risk factors may trigger events apart from the device, which by nature cannot be modified by the stent. In those patients the specific therapies may play a more important role as described above.
Limitations
The following limitations need to be addressed for the interpretation of the results. First, this is a post-hoc analysis of three randomized trials. This analysis was not prespecified. Thus, the results should be considered as hypothesis generating rather than conclusive. Second, the database did not include variables of the therapy with antiplatelet inhibitors, cholesterol lowering medication or anti-diabetics, which would have been of interest in patients with ATR. Third, the division of the patients assigned to the treatment with BP-SES or DP-EES into H-ATR and L-ATR reduced the statistical power of the analysis.
Conclusion
In the current analysis from the randomized BIOFLOW trials patients with H-ATR still had higher rates of TLF in the era of newer-generation DES. Patients treated with BP-SES had lower TLF rates as compared with DP-EES. The improved clinical outcome of BP-SES vs DP-EES was related to a lower rate of TV-MIs and was strongest in patients with L-ATR. Most probably in patients with H-ATR secondary preventive strategies are of higher value than the choice of stent.
Abbreviations
- BP-SES:
-
Bioresorbable-polymer sirolimus-eluting stent
- DES:
-
Drug-eluting stent
- DP-EES:
-
Durable-polymer everolimus-eluting stent
- PCI:
-
Percutaneous coronary intervention
- ST:
-
Stent thrombosis
- TLF:
-
Target lesion failure
- TLR:
-
Target lesion revascularization
- TV-MI:
-
Target-vessel myocardial infarction
References
Roth GA, Mensah GA, Johnson CO et al (2020) Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol 76:2982–3021
Visseren FLJ, Mach F, Smulders YM et al (2021) ESC guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J 42:3227–3337
Cosentino F, Grant PJ, Aboyans V et al (2020) ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J 41:255–323
Robinson JG, Farnier M, Krempf M et al (2015) Efficacy and safety of alirocumab in reducing lipids and cardiovascular events. N Engl J Med 372:1489–1499
Sabatine MS, Giugliano RP, Keech AC et al (2017) Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med 376:1713–1722
Wiviott SD, Braunwald E, McCabe CH et al (2007) Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 357:2001–2015
Wallentin L, Becker RC, Budaj A et al (2009) Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 361:1045–1057
Kandzari DE, Mauri L, Koolen JJ et al (2017) Ultrathin, bioresorbable polymer sirolimus-eluting stents versus thin, durable polymer everolimus-eluting stents in patients undergoing coronary revascularisation (BIOFLOW V): a randomised trial. Lancet 390:1843–1852
Windecker S, Haude M, Neumann FJ et al (2015) Comparison of a novel biodegradable polymer sirolimus-eluting stent with a durable polymer everolimus-eluting stent: results of the randomized BIOFLOW-II trial. Circ Cardiovasc Interv 8:e001441
Saito S, Toelg R, Witzenbichler B et al (2019) BIOFLOW-IV, a randomised, intercontinental, multicentre study to assess the safety and effectiveness of the Orsiro sirolimus-eluting stent in the treatment of subjects with de novo coronary artery lesions: primary outcome target vessel failure at 12 months. EuroIntervention 15:e1006–e1013
Hemetsberger R, Abdelghani M, Toelg R et al (2021) Impact of coronary calcification on clinical outcomes after implantation of newer-generation drug-eluting stents. J Am Heart Assoc 10:e019815
Hemetsberger R, Abdelghani M, Toelg R et al (2022) Complex vs. non-complex percutaneous coronary intervention with newer-generation drug-eluting stents: an analysis from the randomized BIOFLOW trials. Clin Res Cardiol. https://doi.org/10.1007/s00392-022-01994-4
Giustino G, Baber U, Salianski O et al (2016) Safety and efficacy of new-generation drug-eluting stents in women at high risk for atherothrombosis: from the women in innovation and drug-eluting stents collaborative patient-level pooled analysis. Circ Cardiovasc Interv 9:e002995
Sorrentino S, Giustino G, Baber U et al (2018) Dual antiplatelet therapy cessation and adverse events after drug-eluting stent implantation in patients at high risk for atherothrombosis (from the PARIS Registry). Am J Cardiol 122:1638–1646
Bhatt DL, Fox KA, Hacke W et al (2006) Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Engl J Med 354:1706–1717
Cutlip DE, Windecker S, Mehran R et al (2007) Clinical end points in coronary stent trials: a case for standardized definitions. Circulation 115:2344–2351
Bangalore S, Toklu B, Amoroso N et al (2013) Bare metal stents, durable polymer drug eluting stents, and biodegradable polymer drug eluting stents for coronary artery disease: mixed treatment comparison meta-analysis. BMJ 347:f6625
Madhavan MV, Kirtane AJ, Redfors B et al (2020) Stent-related adverse events >1 year after percutaneous coronary intervention. J Am Coll Cardiol 75:590–604
Schwartz GG, Steg PG, Szarek M et al (2018) Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med 379:2097–2107
Madhavan MV, Howard JP, Naqvi A et al (2021) Long-term follow-up after ultrathin vs. conventional 2nd-generation drug-eluting stents: a systematic review and meta-analysis of randomized controlled trials. Eur Heart J 42:2643–2654
Bangalore S, Toklu B, Patel N, Feit F, Stone GW (2018) Newer-generation ultrathin strut drug-eluting stents versus older second-generation thicker strut drug-eluting stents for coronary artery disease. Circulation 138:2216–2226
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study was sponsored by Biotronik. Dr. Toelg has received speakers’ honoraria from Biotronik. Dr. Garcia-Garcia has received institutional research/grant support from Biotronik. Dr. Hemetsberger, Dr. Mankerious, Dr. Abdelghani, Dr. Farhan, Dr. Elbasha, Dr. Allali have nothing to declare. Dr. Windecker reports research and educational grants to the institution from Abbott, Amgen, Astra Zeneca, BMS, Bayer, Biotronik, Boston Scientific, Cardinal Health, CardioValve, CSL Behring, Daiichi Sankyo, Edwards Lifesciences, Guerbet, InfraRedx, Johnson & Johnson, Medicure, Medtronic, Novartis, Polares, OrPha Suisse, Pfizer, Regeneron, Sanofi-Aventis, Sinomed, Terumo, V-Wave. SW serves as unpaid member of the steering/executive group of trials funded by Abbott, Abiomed, Amgen, Astra Zeneca, BMS, Boston Scientific, Biotronik, Cardiovalve, Edwards Lifesciences, MedAlliance, Medtronic, Novartis, Polares, Sinomed, V-Wave and Xeltis, but has not received personal payments by pharmaceutical companies or device manufacturers, He is also member of the steering/excecutive committee group of several investigated-initiated trials that receive funding by industry without impact on his personal remuneration. Stephan Windecker is an unpaid member of the Pfizer Research Award selection committee in Switzerland. Dr Lefèvre has received consultant fees from Biotronik and Abbott and Honoraria from Abbott, Terumo, Boston and Edwards. Dr. Saito has nothing to declare. Dr. Kandzari has received institutional research/grant support from Biotronik, Boston Scientific, Medinol, Medtronic, and Orbus Neich, and personal consulting honoraria from Boston Scientific, Cardiovascular Systems, Inc., and Medtronic. Dr Waksman reports consultant fees from Abbott Vascular, Amgen, Biosensors, Biotronik, Boston Scientific, Corindus, Lifetech Medical, Medtronic, and Philips Volcano; advisory board for Abbott Vascular, Amgen, Boston Scientific, Medtronic, and Philips Volcano; grant support from Abbott Vascular, Biosensors, Biotronik, Boston Scientific, and Edwards Lifesciences; and speakers bureau from AstraZeneca. Dr. Richardt has received institutional research grants from St. Jude Medical, Biotronik, and Medtonic.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hemetsberger, R., Mankerious, N., Toelg, R. et al. Patients with higher-atherothrombotic risk vs. lower-atherothrombotic risk undergoing coronary intervention with newer-generation drug-eluting stents: an analysis from the randomized BIOFLOW trials. Clin Res Cardiol 112, 1278–1287 (2023). https://doi.org/10.1007/s00392-023-02205-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-023-02205-4