Abstract
Background
Coronary vasomotor dysfunction represents an important mechanism responsible for myocardial ischaemia in patients with non-obstructive coronary artery disease (CAD). The use of invasive provocative tests allows identifying patients with epicardial or microvascular spasm. Of note, clinical characteristics associated with the occurrence of epicardial or microvascular spasm have still not completely clarified.
Methods and results
We prospectively enrolled consecutive patients undergoing coronary angiography for suspected myocardial ischaemia/necrosis with evidence of non-obstructive CAD and undergoing intracoronary provocative test for suspected vasomotor dysfunction. Patients with a positive provocative test were enrolled. Clinical, echocardiographic and angiographic characteristics of patients were evaluated according to the pattern of vasomotor dysfunction (epicardial vs. microvascular spasm). We included 120 patients [68 patients with stable angina and 52 patients with myocardial infarction and non-obstructive coronary arteries (MINOCA)]. In particular, 77 (64.2%) patients had a provocative test positive for epicardial spasm and 43 (35.8%) patients for microvascular spasm. Patients with epicardial spasm were more frequently males, smokers, had higher rates of diffuse coronary atherosclerosis at angiography and more frequently presented with MINOCA. On the other hand, patients with microvascular spasm presented more frequently diastolic dysfunction. At multivariate logistic regression analysis male sex, smoking, and diffuse coronary atherosclerosis were independent predictors for the occurrence of epicardial spasm.
Conclusions
Our study showed that specific clinical features are associated with different responses to intracoronary provocative test. Epicardial spasm is more frequent in males and in MINOCA patients, whereas microvascular spasm is more frequent in patients with stable angina and is associated with diastolic dysfunction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ischaemic heart disease represents the leading cause of morbidity and mortality worldwide [1]. The presence of obstructive coronary artery disease (CAD) represents a common pathophysiologic mechanism responsible for myocardial ischaemia. However, a sizeable portion of patients undergoing coronary angiography for suspected myocardial ischaemia presents normal or non-obstructive CAD (stenosis < 50%) [2, 3] and functional mechanisms may be involved in the pathogenesis of myocardial ischaemia in these patients [3,4,5,6,7,8]. In particular, an enhanced vasoreactivity may induce coronary spasm at both epicardial and microvascular level [9]. Of interest, the ACOVA study [10] showed that nearly 50% of patients with stable angina undergoing coronary angiography presented non-obstructive CAD and in these patients a provocative invasive test of vasoreactivity using acetylcholine (ACh) was positive in two-thirds of patients, demonstrating the occurrence of epicardial spasm in 45% patients and microvascular spasm in 55% of patients. Moreover, we recently demonstrated that in patients presenting with myocardial infarction and non-obstructive coronary arteries (MINOCA) and suspected vasomotion abnormalities, an invasive provocative test using ACh or ergonovine was safe and identified a subset of patients with a higher risk of death and recurrence of acute coronary syndrome (ACS) [11].
Several studies evaluated clinical characteristics associated with the occurrence of epicardial or microvascular spasm at intracoronary provocative test [12,13,14], yet results deriving from these studies were conflicting. Moreover, these studies mainly enrolled patients presenting with stable angina and whether these findings may be extended also to patients presenting with ACS is unknown.
In our study, we aimed at assessing the clinical characteristics of consecutive patients presenting with stable angina or ACS, non-obstructive CAD and a positive response to invasive provocative testing according to current definitions [15, 16].
Methods
The authors declare that all supporting data are available within the article.
Study population
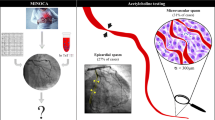
We prospectively enrolled consecutive patients admitted to the Department of Cardiovascular and Thoracic Sciences of Fondazione Policlinico Universitario A. Gemelli IRCCS in Rome, Italy, undergoing coronary angiography for suspected myocardial ischaemia with evidence of non-obstructive CAD (angiographically normal coronary arteries or diffuse atherosclerosis with stenosis < 50%) and undergoing an intracoronary provocative test from September 2015 to June 2018. We enrolled both patients admitted with a diagnosis of stable angina and patients with MINOCA (Fig. 1). Patients with stable angina were defined as patients admitted with a stable pattern of typical chest pain at rest, on exertion, or a combination of both, without signs of myocardial infarction (MI). Patients with MINOCA were diagnosed based on their reporting of one or more episodes of chest pain at rest, typical enough to suggest a cardiac ischaemic origin, in the previous 24 h, associated with ST-segment and/or T wave abnormalities on the ECG and detection of raise and fall of serum troponin T levels with at least one value exceeding the 99th percentile of a normal reference population with an upper limit of 0.014 µg/L [17]. Among patients presenting with MINOCA, we excluded those with obvious causes of MI other than suspected coronary vasomotor abnormalities and in whom provocative testing was not performed. In particular, we excluded 26 patients with a diagnosis of Takotsubo syndrome confirmed by left ventricle angiography, 24 patients with a suspected diagnosis of myocarditis (diagnosis based on the presence of signs and symptoms of infection and/or inflammatory activation associated with wall motion abnormalities at left ventricular angiography and echocardiogram suggesting a non-epicardial pattern and confirmed by subsequent cardiac magnetic resonance imaging), 82 patients with type 2 myocardial infarction with mechanisms other than suspected vasospasm (e.g. pulmonary embolism, evidence of coronary thrombosis on an unstable plaque confirmed by optical coherence tomography, cardiotoxic drug administration, hypertensive crisis or severe aortic stenosis). Finally, 90 patients with a negative response to provocative testing were excluded. The remaining 120 patients with a positive response to intracoronary provocative test were included in the final analysis (Fig. 1).
Study flow-chart of enrolled patients. Asterisk Among patients presenting with MINOCA, we excluded those with causes of MI other than suspected coronary vasomotor abnormalities and in whom provocative testing was not performed. FFR using iv adenosine was performed in 2 patients with stenosis 50% and with a positive response to intracoronary provocative test. In both cases coronary stenosis resulted non-hemodynamically significant
The study protocol complied with the Declaration of Helsinki and the study was approved by the institutional review committee. All patients gave written informed consent before angiography.
Invasive provocative test protocol
Coronary angiography was performed through radial or femoral artery approach and the intracoronary ACh provocative test was performed immediately after coronary angiography. The choice to perform an intracoronary provocative test during coronary angiography was left to operator’s discretion. ACh was administered in a stepwise manner into the left coronary artery (LCA) (20–200 µg) or into the right coronary artery (RCA) (20–50 µg) over a period of 3 min with a 2–3 min interval between injections. When ergonovine was used, it was administrated as a bolus in a stepwise manner into the LCA (8–64 mg) and RCA (8–40 mg) with an interval of 2–3 min between each injection. Coronary angiography was performed 1 min after each injection of these agents and when chest pain and/or ischaemic ECG shifts were observed. The decision of testing with provocative test LCA or RCA as first was left to the discretion of the physicians; both LCA and RCA were tested if the first test was negative. In patients taking vasoactive drugs (calcium-channel blockers and nitrates), the provocation tests were performed after a washout period for these drugs of at least 24 h. A fasting period (including caffeine consumption) > 12 h was requested in all stable patients. Finally, in patients with coronary stenoses of 50%, assessment of fractional-flow reserve (FFR), preceded by intracoronary nitroglycerin administration, was performed after the provocative vasoreactivity test.
Angiographic responses during the provocative test were assessed in multiple orthogonal views in order to detect the most severe narrowing and/or analysed by using computerized quantitative coronary angiography (QCA-CMS, Version 6.0, Medis-Software, Leiden, The Netherlands). The test was considered positive for epicardial coronary spasm in the presence of focal or diffuse epicardial coronary diameter reduction ≥ 90% in comparison with the relaxed state following intracoronary nitroglycerin administration given to relieve the spasm, associated with the reproduction of the patient’s symptoms and ischaemic ECG shifts [15]. Microvascular spasm was diagnosed when typical ischaemic ST-segment changes and angina developed in the absence of epicardial coronary constriction ≥ 90% diameter reduction. Patients who experienced no angina, spasm, or ST-segment shifts were considered to have a negative test response (normal coronary vasoreactivity). Furthermore, patients who experienced ischaemic ECG shifts without angina were considered to have a negative test response [16]. Occurrence of bradyarrhythmias (defined as bradycardia with heart rate < 50 bpm or second- or third-degree AV block lasting more than 3 s), atrial fibrillation, and ventricular tachycardia (defined as three or more consecutive premature ventricular complexes) during the provocative test were also recorded.
Echocardiographic assessment
All patients underwent a comprehensive echocardiographic evaluation during hospital admission using a standard ultrasound machine (Artida, Toshiba Medical System, Japan) and all images were digitally saved in raw data format to magneto optical discs for offline analysis performed by an experienced echocardiographer (SM). Left ventricle (LV) and left atrial dimensions were obtained by M-mode and two-dimensional (2D) images whereas LV end-diastolic and end-systolic volumes and LVEF were calculated using the modified Simpson’s biplane method. LV diastolic function was evaluated using trans-mitral diastolic flow tracing assessed with pulsed-wave Doppler from an apical four-chamber view with E-wave and A-wave velocity measurement as previously described [18]. Moreover, also pulsed-wave tissue Doppler imaging (TDI) e’ velocity (average of lateral and septal basal regions) and average E/e’ ratio were assessed. The presence of diastolic dysfunction was assessed as previously described [18, 19]. In particular, we evaluated four variables for identifying diastolic dysfunction with their abnormal cut-off values: (1) annular e’ velocity: septal e’ < 7 cm/s, lateral e’ < 10 cm/s; (2) average E/e’ ratio > 14; (3) left atrial volume index > 34 mL/m2; (4) peak tricuspid regurgitation velocity > 2.8 m/s. LV diastolic dysfunction was present if more than half of the available parameters meet these cut-off values [18].
Statistical analysis
Data distribution was assessed according to the Kolmogorov–Smirnov test. Continuous variables were compared using an unpaired Student’s t test or Mann–Whitney U test, as appropriate, and data were expressed as mean ± standard deviation or as median (range). Categorical data were evaluated using the χ2 test or Fisher exact test as appropriate. A multivariable logistic regression analysis for the occurrence of epicardial spam vs. microvascular spasm was performed including all variables with a p value of < 0.05 at the univariate analysis. All tests were two-sided, and a p value of < 0.05 represented statistically significant differences. All analyses were performed using SPSS version 21 (SPSS Inc., Chicago, IL, USA).
Results
We included in the final analysis 120 patients with non-obstructive coronary arteries and a positive intracoronary provocative test [mean age 62.71 ± 11.01 years; 58 (48.3%) men]. In the overall population 68 (56.7%) patients presented with stable angina and 52 (43.3%) patients with MINOCA. The provocative test was performed using ACh in 99 (82.5%) patients and ergonovine in 21 (17.5%) patients. In particular, 77 (64.2%) patients had a provocative test positive for epicardial spasm and 43 (35.8%) patients for microvascular spasm.
Clinical correlates of epicardial vs microvascular spasm
Patients with epicardial spasm compared with patients with microvascular spasm were more frequently males [50 (64.9%) vs 8 (18.6%) p < 0.001], smokers [24 (31.2%) vs 3 (6.9%) p = 0.003]. and presenting with MINOCA [39 (50.7%) vs 13 (30.2%) p = 0.03]. Accordingly, peak of Troponin I was higher in epicardial spasm compared with microvascular spasm [0.007 (0.003–22.80) ng/mL vs 0.006 (0.003–8.00) ng/mL, p = 0.026]. There were no differences in the occurrence of epicardial or microvascular spasm between patients undergoing ACh or ergonovine test. Clinical characteristics of the overall study population and according to the type of response at provocative test are reported in Table 1.
Angiographic and echocardiographic correlates of epicardial vs microvascular spasm
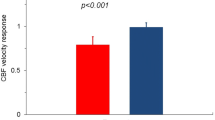
Of interest, at coronary angiography, patients with epicardial spasm had a higher occurrence of diffuse coronary atherosclerosis compared with microvascular spasm [61 (79.2%) vs 20 (46.5%), p < 0.001] (Table 1). Moreover, at echocardiogram performed during hospital admission, patients with microvascular spasm had higher rates of diastolic dysfunction [9 (20.9%) vs 6 (7.8%), p = 0.036] with higher values of E/e’ ratio [9 (5–18) vs 6 (5–16), p = 0.041] compared with patients with epicardial spasm (Fig. 2), while left ventricular ejection fraction did not differ between the two groups (Table 1).
Predictors of epicardial vs microvascular spasm
At univariate logistic regression analysis, male sex (β = 8.10, 95% CI 3.30–19.92, p < 0.001), smoking (β = 6.04, 95% CI 1.70–21.47, p = 0.005), ACS as clinical presentation (β = 2.92, 95% CI 1.32–6.44, p = 0.008), and diffuse coronary atherosclerosis (β = 4.38, 95% CI 1.94–9.90, p < 0.001) were predictors of occurrence of epicardial vs microvascular spasm (Table 2). At multivariable logistic regression analysis male sex only (β = 5.93, 95% CI 2.26–15.60, p < 0.001), smoking (β = 4.18, 95% CI 1.04–16.86, p = 0.044), and diffuse coronary atherosclerosis (β = 3.58, 95% CI 1.37–9.34, p = 0.009) were independent predictors for the occurrence of epicardial spasm (Table 2).
Safety evaluation of invasive provocative test
Arrhythmic complications during provocative test occurred in 10 (8.3%) patients. In particular, transient AV block occurred in 5 (4.2%) patients, sinus block in 1 (0.8%) patient and paroxysmal atrial fibrillation in 4 (3.5%) patients (Table 3). There were no differences in the occurrence of AV or sinus block between patients with epicardial vs microvascular spasm. However, paroxysmal atrial fibrillation occurred more frequently in patients with microvascular spasm compared with epicardial spasm [4 (9.3%) vs 0 (0.0%), p = 0.014] (Table 3). Finally, there were no differences in the complication rates according to the type of drug used for the provocative test.
Discussion
Our study analysed clinical, angiographic and echocardiographic characteristics of patients with a positive response at invasive provocative test, comparing patients with epicardial spasm vs patients with microvascular spasm. Of importance, we demonstrated that patients with epicardial spasm compared with microvascular spasm more frequently: (1) were male and smokers; (2) presented with MINOCA; (3) had higher prevalence of diffuse coronary atherosclerosis. In contrast, patients with microvascular spasm more frequently had evidence of diastolic dysfunction (Fig. 3). Importantly, provocative testing was safe; transient and well-tolerated arrhythmic complication only were occasionally observed during provocative testing with paroxysmal atrial fibrillation being more frequently observed in patients with microvascular spasm than in those with epicardial spasm.
Differences in clinical, angiographic and echocardiographic characteristics among patients with non-obstructive CAD and positive provocative test according to the occurrence of epicardial or microvascular spasm. CAD coronary artery disease, MINOCA myocardial infarction and non-obstructive coronary arteries
A previous study by Aziz et al. [12] enrolling only patients with stable angina and non-obstructive CAD demonstrated a sex-difference in the response to intracoronary ACh test, showing a higher prevalence of vasomotor dysfunction assessed by intracoronary ACh administration in women compared with men, with a higher incidence of both microvascular spasm (OR 4.2) and epicardial spasm. In contrast, a study by Ong et al. [13] enrolling 921 patients with non-obstructive CAD and undergoing ACh intracoronary test, showed that male sex was a predictor of epicardial spasm. Of note, this study also enrolled almost exclusively stable patients, with a prevalence of MINOCA of 4% only. In contrast with previous studies, we enrolled both patients with stable angina and patients presenting with MINOCA (43% of the overall study population), providing further insight into this clinical setting.
In our study we demonstrated a clear sex-related difference in the vasomotor response to provocative test, with a higher prevalence of microvascular spasm among women and of epicardial spasm among men. The sex-difference observed in our study is in keeping with the greater burden of coronary microvascular dysfunction (CMD) observed in women [3, 20,21,22,23]. Several mechanisms have been suggested to explain CMD in women including smaller body size and myocardial mass [24]. Moreover, the coronary arteries in women have a smaller diameter, thinner walls and more winding course [25, 26]. Finally, also hormonal factors may play an important role [22].
In addition, we found that while three-fourths of patients presenting with MINOCA had an intracoronary provocative test positive for epicardial spasm, this was observed in half of patients only among those presenting with stable angina. Accordingly, peak of Troponin I was higher in patients with epicardial spasm compared with patients with microvascular spasm.
It is worth noting that in a recent study by our group [11] including patients presenting with MINOCA, we showed that among patients with a positive response to provocative test clinical outcome was significantly worse in patients with epicardial spasm compared to those with microvascular spasm at 1-year follow-up. Of note, a study by Lee et al. [14] including only patients with stable angina demonstrated no difference in prognostic according to pattern of vasomotor response at provocative test.
Previous studies demonstrated that diffuse non-obstructive coronary atherosclerosis was associated with a positive response to provocative testing and to occurrence of focal vasospasm [27, 28]. However, the relation between diffuse non-obstructive CAD and pattern of coronary vasomotor response has never been investigated. Our study shows that most of the patients with epicardial spasm have diffuse non-obstructive CAD, while patients with microvascular spasm may present with diffuse non-obstructive CAD or normal coronary arteries with similar percentages, thus suggesting a critical role for local atherosclerosis as substrate for epicardial hyperreactivity. On the other hand, microvascular spasm probably occurs in the context of a CMD, irrespective of an underlying epicardial coronary atherosclerosis [29].
In our study, patients with microvascular spasm had a higher prevalence of diastolic dysfunction compared to that in patients with epicardial spasm. Previous reports indicated that patients with microvascular spasm may have a transient diastolic dysfunction during ACh provocative test [30, 31]. Our study extends these findings and is in keeping with recent growing evidences suggesting that coronary microvascular ischaemia may play an important role in the pathophysiology of diastolic dysfunction in patients with heart failure with preserved ejection fraction (HFpEF) [32,33,34]. Of note, diastolic dysfunction is also recognized risk factor for the occurrence of AF [35] and this may explain the higher rate of paroxysmal AF as arrhythmic complication in patients with microvascular spasm during the provocative test.
Our study has some limitations. First, it is a single-centre study. Second, the study population is not large. Third, the optimal test to be used (either ergonovine or ACh) cannot be deduced by our results. In our institution, as each operator is familiar with a particular vasoactive drug, the choice of the vasoactive drug was left to physician’s discretion to facilitate enrolment process. However, the use of two different drugs, with two different mechanisms of action, to induce coronary spasm may be another limitation of our study. Moreover, we did not measure invasively coronary blood flow and coronary flow reserve using an intracoronary Doppler or pressure/thermodilution wire and therefore, their potential relationship with the response to vasoconstrictor stimuli remains undetermined. We did not further evaluate patients with “negative” response with adenosine, exploring endothelium-independent mechanisms of CMD. Finally, the choice to perform a provocative test, in particular in patients presenting with stable angina, was left to operator’s discretion. This could have resulted in a selection bias and explains why the prevalence of MINOCA patients in our study population is higher compared with previous studies [13]. However, the aim of our study was to compare the predictors of epicardial vs. microvascular spasm and not to evaluate the frequency of epicardial or microvascular coronary spasm in response to provocative test among patients presenting with myocardial ischaemia and non-obstructive CAD.
In conclusion, coronary vasomotor abnormalities represent an important cause of myocardial ischaemia both in patients presenting with stable angina and in patients presenting with MINOCA. Our study demonstrates that epicardial spasm is more frequent in men, in smokers and in patients who present with MINOCA and with diffuse non-obstructive coronary atherosclerosis. On the other hand, microvascular spasm is more frequent in women and is associated with the presence of diastolic dysfunction. Further studies are needed in order to clarify whether different patterns of vasomotor dysfunction are associated with different outcomes.
Change history
03 November 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00392-022-02110-2
References
Timmis A, Townsend N, Gale C, Grobbee R, Maniadakis N, Flather M, Wilkins E, Wright L, Vos R, Bax J, Blum M, Pinto F, Vardas P (2018) Atlas writing group—European society of cardiology: cardiovascular disease statistics 2017. Eur Heart J 39:508–579
Bugiardini R, Merz CN (2005) Angina with “normal” coronary arteries: a changing philosophy. JAMA 293:477–484
Crea F, Camici PG, Merz CN (2014) Coronary microvascular dysfunction: an update. Eur Heart J 35:1101–1111
Lanza GA, Crea F (2010) Primary coronary microvascular dysfunction: clinical presentation, pathophysiology, and management. Circulation 121:2317–2325
Lanza GA, Careri G, Crea F (2011) Mechanisms of coronary artery spasm. Circulation 124:1774–1782
Kaski JC, Crea F, Gersh BJ, Camici PG (2018) Reappraisal of ischemic heart disease. Circulation 138:1463–1480
De Vita A, Manfredonia L, Lamendola P, Villano A, Ravenna SE, Bisignani A, Niccoli G, Lanza GA, Crea F (2019) Coronary microvascular dysfunction in patients with acute coronary syndrome and no obstructive coronary artery disease. Clin Res Cardiol. https://doi.org/10.1007/s00392-019-01472-4(Epub ahead of print)
Yu M, Zhang Q, Huang X (2018) Acute coronary syndrome due to right coronary spasm and documented lambda-like J waves. Clin Res Cardiol 107:729–732
Ong P, Athanasiadis A, Sechtem U (2013) Patterns of coronary vasomotor responses to intracoronary acetylcholine provocation. Heart 99:1288–1295
Ong P, Athanasiadis A, Borgulya G, Mahrholdt H, Kaski JC, Sechtem U (2012) High prevalence of a pathological response to acetylcholine testing in patients with stable angina pectoris and unobstructed coronary arteries. The ACOVA Study (Abnormal COronary VAsomotion in patients with stable angina and unobstructed coronary arteries). J Am Coll Cardiol. 59:655–662
Montone RA, Niccoli G, Fracassi F, Russo M, Gurgoglione F, Cammà G, Lanza GA, Crea F (2018) Patients with acute myocardial infarction and non-obstructive coronary arteries: safety and prognostic relevance of invasive coronary provocative tests. Eur Heart J 39:91–98
Aziz A, Hansen HS, Sechtem U, Prescott E, Ong P (2017) Sex-related differences in vasomotor function in patients with angina and unobstructed coronary arteries. J Am Coll Cardiol 70:2349–2358
Ong P, Athanasiadis A, Borgulya G, Vokshi I, Bastiaenen R, Kubik S, Hill S, Schäufele T, Mahrholdt H, Kaski JC, Sechtem U (2014) Clinical usefulness, angiographic characteristics, and safety evaluation of intracoronary acetylcholine provocation testing among 921 consecutive white patients with unobstructed coronary arteries. Circulation 29(129):1723–1730
Lee EM, Choi MH, Seo HS, Kim HK, Kim NH, Choi CU, Kim JW, Lim HE, Kim EJ, Rha SW, Park CG, Oh DJ (2017) Impact of vasomotion type on prognosis of coronary artery spasm induced by acetylcholine provocation test of left coronary artery. Atherosclerosis. 257:195–200
Beltrame JF, Crea F, Kaski JC, Ogawa H, Ong P, Sechtem U, Shimokawa H, Bairey Merz CN, Coronary Vasomotion Disorders International Study Group (COVADIS) (2017) International standardization of diagnostic criteria for vasospastic angina. Eur Heart J. 38:2565–2568
Ong P, Camici PG, Beltrame JF, Crea F, Shimokawa H, Sechtem U, Kaski JC, Bairey Merz CN, Coronary Vasomotion Disorders International Study Group (COVADIS) (2018) International standardization of diagnostic criteria for microvascular angina. Int J Cardiol. 250:16–20
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD, ESC Scientific Document Group (2018) Fourth universal definition of myocardial infarction (2018). Eur Heart J. 1:1. https://doi.org/10.1093/eurheartj/ehy462(Epub ahead of print)
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P, Marino P, Oh JK, Popescu B, Waggoner AD (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the american society of echocardiography and the European Association Of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 17:1321–1360
Khoury S, Steinvil A, Gal-Oz A, Margolis G, Hochstatd A, Topilsky Y, Keren G, Shacham Y (2018) Association between central venous pressure as assessed by echocardiography, left ventricular function and acute cardio-renal syndrome in patients with ST segment elevation myocardial infarction. Clin Res Cardiol 107:937–944
Shaw LJ, Merz CN, Pepine CJ, Reis SE, Bittner V, Kelsey SF, Olson M, Johnson BD, Mankad S, Sharaf BL, Rogers WJ, Wessel TR, Arant CB, Pohost GM, Lerman A, Quyyumi AA, Sopko G, WISE Investigators (2006) Insights from the NHLBI-sponsored Women’s ischemia syndrome evaluation (WISE) Study: Part I: gender differences in traditional and novel risk factors, symptom evaluation, and gender-optimized diagnostic strategies. J Am Coll Cardiol. 47:S4–S20
Humphries KH, Izadnegahdar M, Sedlak T, Saw J, Johnston N, Schenck-Gustafsson K, Shah RU, Regitz-Zagrosek V, Grewal J, Vaccarino V, Wei J, Merz CN (2017) Sex differences in cardiovascular disease—impact on care and outcomes. Front Neuroendocrinol 46:46–70
Ong P, Athanasiadis A, Sechtem U (2013) Gender aspects in patients with angina and unobstructed coronary arteries. Clin Res Cardiol Suppl 8:25–31
Waits GS, O’Neal WT, Sandesara PB, Li Y, Shah AJ, Soliman EZ (2018) Association between low diastolic blood pressure and subclinical myocardial injury. Clin Res Cardiol 107:312–318
Paul TK, Sivanesan K, Schulman-Marcus J (2017) Sex differences in nonobstructive coronary artery disease: recent insights and substantial knowledge gaps. Trends Cardiovasc Med 27:173–179
Kitzman DW, Scholz DG, Hagen PT, Ilstrup DM, Edwards WD (1988) Age-related changes in normal human hearts during the first 10 decades of life. Part II (Maturity): a quantitative anatomic study of 765 specimens from subjects 20 to 99 years old. Mayo Clin Proc 63:137–146
Paulsen S, Vetner M, Hagerup LM (1975) Relationship between heart weight and the cross sectional area of the coronary ostia. Acta Pathol Microbiol Scand A Pathol 83:429–432
Koizumi T, Yokoyama M, Namikawa S, Kuriyama N, Nameki M, Nakayama T, Kaneda H, Sudhir K, Yock PG, Komiyama N, Fitzgerald PJ (2006) Location of focal vasospasm provoked by ergonovine maleate within coronary arteries in patients with vasospastic angina pectoris. Am J Cardiol 97:1322–1325
Yamagishi M, Miyatake K, Tamai J, Nakatani S, Koyama J, Nissen SE (1994) Intravascular ultrasound detection of atherosclerosis at the site of focal vasospasm in angiographically normal or minimally narrowed coronary segments. J Am Coll Cardiol 23:352–357
Camici PG, Crea F (2007) Coronary microvascular dysfunction. N Engl J Med 356:830–840
Arrebola-Moreno AL, Arrebola JP, Moral-Ruiz A, Ramirez-Hernandez JA, Melgares-Moreno R, Kaski JC (2014) Coronary microvascular spasm triggers transient ischemic left ventricular diastolic abnormalities in patients with chest pain and angiographically normal coronary arteries. Atherosclerosis. 236:207–214
Ong P, Athanasiadis A, Mahrholdt H, Shah BN, Sechtem U, Senior R (2013) Transient myocardial ischemia during acetylcholine-induced coronary microvascular dysfunction documented by myocardial contrast echocardiography. Circ Cardiovasc Imaging 6:153–155
Taqueti VR, Solomon SD, Shah AM, Desai AS, Groarke JD, Osborne MT, Hainer J, Bibbo CF, Dorbala S, Blankstein R, Di Carli MF (2018) Coronary microvascular dysfunction and future risk of heart failure with preserved ejection fraction. Eur Heart J 39:840–849
Crea F, Bairey Merz CN, Beltrame JF, Kaski JC, Ogawa H, Ong P, Sechtem U, Shimokawa H, Camici PG, Coronary Vasomotion Disorders International Study Group (COVADIS) (2017) The parallel tales of microvascular angina and heart failure with preserved ejection fraction: a paradigm shift. Eur Heart J. 38:473–477
Bohnen S, Prüβner L, Vettorazzi E, Radunski UK, Tahir E, Schneider J, Cavus E, Avanesov M, Stehning C, Adam G, Blankenberg S, Lund GK, Muellerleile K (2019) Stress T1-mapping cardiovascular magnetic resonance imaging and inducible myocardial ischemia. Clin Res Cardiol. https://doi.org/10.1007/s00392-019-01421-1(Epub ahead of print)
Tiwari S, Schirmer H, Jacobsen BK, Hopstock LA, Nyrnes A, Heggelund G, Njølstad I, Mathiesen EB, Løchen ML (2015) Association between diastolic dysfunction and future atrial fibrillation in the Tromsø Study from 1994 to 2010. Heart 101:1302–1308
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have anything to disclose regarding this manuscript.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of our institutional committee (Fondazione Policlinico Universitario Agostino Gemelli IRCCS-Università Cattolica del Sacro Cuore; Code 26710/13) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
The original online version of this article was revised: the author's name Filippo Gurgoglione was incorrectly given as Filippo Gurguglione.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Montone, R.A., Niccoli, G., Russo, M. et al. Clinical, angiographic and echocardiographic correlates of epicardial and microvascular spasm in patients with myocardial ischaemia and non-obstructive coronary arteries. Clin Res Cardiol 109, 435–443 (2020). https://doi.org/10.1007/s00392-019-01523-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-019-01523-w