Abstract
Background
Prognostic value of right ventricular (RV) systolic function is well established in valvular disease, heart failure but has not been evaluated in patients undergoing cardiac surgery.
Objectives
The aim of the present study was to evaluate the prognostic value of preoperative RV dysfunction extensively evaluated on the basis of a large set of echocardiographic parameters [S′, RV fractional area change (RVFAC), right myocardial performance index (RMPI), isovolumic acceleration (IVA), RV dP/dt and basal longitudinal strain (BLS)] in a large population of unselected patient awaiting cardiac surgery.
Methods
We prospectively studied 400 consecutive patients referred for cardiac surgery, in a single surgical center. Echocardiography was performed 24 h before surgery and phone interview assessed the survival status (overall and cardiovascular death) 3-years after surgery.
Results
Among 400 patients, 271 were male, mean age was 70.3 ± 10.2. At 3-years the overall and cardiovascular mortality was, respectively, 10.5 and 6.8%. The univariate Cox analysis identified all RV function parameters excepted BLS as predictive factors of overall mortality, with the strongest value for RVFAC < 35% (HR 4.8), S′ < 10 cm/s (HR 3.8) and IVA < 1.8 m/s2 (HR 3.2) (all P < 0.001). All parameters were associated to cardiovascular mortality. In multivariate analysis, RVFAC, S′, dP/dt and IVA were significantly associated to 3-years overall mortality whatever the EuroSCORE. Abnormal RVFAC, S′, IVA and BLS were associated to cardiovascular mortality.
Conclusions
The presence of RV dysfunction before cardiac surgery assessed by echo significantly predicts postoperative mortality, and this is true whatever the EuroSCORE level. This result demonstrates the need of adding the assessment of echographic RV function before cardiac surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Right ventricular (RV) systolic function is a prognosticator in various pathological conditions including patients undergoing cardiac surgery. These results relied on data arising from single-centre studies, focusing on a specific pathological condition (ischemic cardiomyopathy or valvular heart disease) and mostly based on retrospective or small prospective studies. Moreover, in these studies, the assessment of RV function relied on heterogeneous approaches: clinical definition [1], invasive assessment by thermodilution [2], scintigraphic RV ejection fraction [3] and echographic data. Among echographic studies none were standardized, and RV dysfunction assessment was based on the use of a single parameter: Maslow et al [4]. showed that RV fractional area change (RVFAC) <35% was associated with an increased risk of long-term mortality. Right myocardial performance index (RMPI) >0.49 has been related to a reduced short-term survival rate [5]. In patients with previous myocardial infarction undergoing surgical ventricular reconstruction, preoperative RV dysfunction based on tricuspid annular plane systolic excursion (TAPSE) was an independent predictor of long-term mortality [6].
This heterogeneity of parameters demonstrates that the definition of RV dysfunction is not unequivocal. The 2010 ASE recommendations do not solve this discrepancy. Indeed, it is stipulated that RV systolic function can be evaluated using at least one parameter among several validated parameters such as S′, RVFAC, TAPSE or RMPI. However, it is also mentioned that combining more than one parameter may more reliably distinguish normal from abnormal function.
In the present study, we sought to evaluate if a quantitative prospective multiparametric echocardiographic analysis of the RV function allowed prediction of post-operative long-term prognosis in patients undergoing cardiac surgery.
Methods
Study population
This prospective study enrolled consecutive patients awaiting cardiac surgery from September 1, 2010 to December 31, 2010. The study group consisted of 413 patients recruited at the Department of Cardiology and Cardiac Surgery (Clinique Saint-Augustin, Bordeaux, France).
Nine patients (2.1%) were excluded from all subsequent analysis because of poor ultrasound window. Four were lost of follow-up. Accordingly, data from 400 patients were analyzed.
Echocardiography was performed ≤24 h before surgery in all patients, and relevant clinical data were collected at the same time. The clinical variables obtained before surgery included demographics and medications. Preoperative EuroSCORE was calculated as recommended [7].
Echocardiographic studies
Comprehensive echocardiography was performed by a senior cardiologist on a VividE9 ultrasound system (GE Vingmed Ultrasound SA, Horten, Norway) equipped with multifrequency transducers (1.5–4 MHz). Physician performing echocardiographic study was not aware of the outcome of patient surgery.
Systolic pulmonary artery pressure (sPAP) was determined from peak tricuspid regurgitation (TR) velocity using the simplified Bernoulli equation and combined with an estimated right atrial pressure (based on the inferior vena cava collapse index). Pulmonary vascular resistance (PVR) was estimated using the ratio of peak TR velocity to the RV outflow tract time-velocity integral (the formula published by Abbas et al. [8]. was applied).
Left ventricular filling pressures were estimated according to the 2009 ASE recommendations. Briefly, classification was based on Mitral E/A, E/e′ (using average e′), sPAP, left atrial volume, and when necessary the difference between pulmonary and mitral A wave duration.
Echocardiographic measurements of right ventricular function
Special care has been taken to evaluate right ventricular function according to recent guidelines [9].
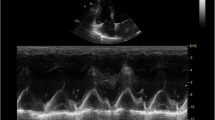
A modified apical 4-chamber view focused on the RV was used to calculate RVFAC (%) defined as [(end-diastolic RV area − end-systolic RV area)/end-diastolic RV area) × 100 [10, 11].
All measurements using pulsed-wave TDI were performed in a 4-chamber view focused on RV using a tissue Doppler mode with a pulsed-wave Doppler sample volume placed in the basal segment of the RV free wall. A special care has been taken to ensure optimal image orientation to avoid underestimation of velocities. The following data was obtained: (1) peak S′ was the peak longitudinal velocity of the basal RV free wall [12, 13]. (2) RMPI obtained by the TDI method was defined as the ratio of the sum of isovolumic relaxation time (IVRT) and isovolumic contraction time divided by ejection time [14]. (3) IVA (m/s2) was defined as the slope of isovolumic myocardial velocity [15].
RV dP/dt (mmHg/s) was calculated by measuring the time required for the tricuspid regurgitation (TR) continuous-wave Doppler signal to increase in velocity from 0.5 to 2 m/s [16].
An apical 4-chamber view used for two-dimensional strain analysis was obtained as previously extensively described [17], to measure the RV free wall basal longitudinal strain (BLS).
Endpoints
The primary end-point was predefined as follow:
-
overall survival was defined as a follow-up period continued from the date of inclusion (24 h prior surgery) until death all causes or December 31, 2013 (data cut-off) if patients were still living,
-
specific survival was defined as a follow-up period continued from the date of inclusion (24 h prior surgery) until cardiovascular death (death related to heart failure with or without cardiogenic shock, death secondary to myocardial infarction, sudden cardiac death, death secondary to stroke) or December 31, 2013 (data cut-off) if patients were still living. Sudden cardiac death was defined as witnessed sudden and unexpected collapse that occurs within one hour of symptom onset or nocturnal death with no previous deterioration.
Figure 1 displays the flowchart of the study design.
Ethics
Our study complies with the Declaration of Helsinski. Local ethic committee (CPP-SOO3, University of Bordeaux, France) approved the protocol study and all included patients gave their consent.
Statistical analyses
Continuous and qualitative variables were expressed as mean, standard deviation (SD) and discrete variables as absolute numbers and percentages. Descriptive data were analyzed for normality using visual histograms and the Shapiro–Wilks test. The groups were first tested using a Chi-squared test to compare categorical variables. The clinical and echocardiographic data were compared using 2-sample Student t test or Wilcoxon’s rank-sum (Mann–Whitney) non-parametric tests as appropriate according to the variance R test. The feasibility and reproducibility have been already published elsewhere [17].
Overall survival as defined above, was estimated using the Kaplan–Meier method and survival curves were compared using log-rank tests. For univariate and multivariate analysis, the Cox regression model was applied. The significant level α = 0.2 in the univariate analysis was used to select variables for the multivariate model (using backward stepwise elimination).
Specific survival as defined above, was estimated using Fine-Gray proportional hazards regression analyses to integrate the competing risk of other causes of death for univariate and multivariate analyses [18]. Given the relatively low number of events for specific survival, sequential multivariate analyses tested the variables with EuroSCORE (according to its weight) in separate models by blocks.
Estimated Hazard ratios (HR) and their 95% confident intervals (CI) were calculated.
All p values were two-sided, and values <0.05 were considered statistically significant. All statistical analyses were performed using Stata® software version 11.0 (StataCorp LP, College Station, TX).
Results
Descriptive analysis
Four hundred patients (mean age: 70.3 ± 10.2 years) were enrolled of which 63% were awaiting valve surgery (severe valvular disease as follow: aortic stenosis 44.2%, aortic regurgitation 3.3%, mitral stenosis 3.3% and mitral regurgitation 10%), 49% coronary artery bypass grafting and 3% other cardiac surgery (myxoma resection, atrial septal defect closure, pericardiectomy, aortic dissection repair, coarctation repair). Fifty-one patients (12.7%) had concomitant valvular surgery (replacement or repair) with coronary artery bypass. Table 1 shows patients’ characteristic in each group.
Deceased patients were on average older than alive for both overall and cardiovascular death. Gender, blood pressure, as well as others cardiovascular risk factors did not differ significantly between the groups. Medications were also not significantly different.
During the study period, the primary end-point was reached in 42 patients of 400 for all causes mortality (10.5%) and in 27 patients of 400 for cardiovascular mortality (6.8%). The predictive preoperative 30 days mortality based on the mean logistic EuroSCORE was 6.2 ± 6.0% in the cohort and was higher in the endpoints groups.
RV function in the study population
Table 2 displayed echographic parameters of the study population. In our population, according to the applied definition of RV dysfunction, RV dysfunction prevalence was variable as follow: 9% (n = 36) for RVFAC < 35%, 14% (n = 56) for S′ < 10 cm/s, 33.7% (n = 135) for RMPI > 0.55, 37.7% (n = 151) for dP/dt < 400 mmHg/s, 21.2% (n = 85) for IVA < 1.8 cm/s2 and 30.5% (n = 122) for GLS (>−17%).
Consequently, when considering two parameters to define RV dysfunction, discrepancies were frequent. For example, S′ and RVFAC were discrepant (S′ > 10 cm/s and RVFAC < 35%, or S′ < 10 cm/s and RVFAC > 35%) in 53 patients (13.3% of the total population) while these parameters matched in 347 patients (89.3%) Such discrepancies were also found according to S′ and RMPI (18.3%), S′ and IVA (29.5%), RVFAC and RMPI (14%) and RVFAC and IVA (30.8%).
Also worthy of note were the mean values of sPAP and PVR significantly higher in patients with events (overall death or cardiovascular death) as compared to live patients (Table 2).
Association between preoperative echo RV parameters and survival
Univariate analysis (Table 3), shows that preoperative values of S′, RVFAC, RMPI, dP/dt and IVA were all predictors of 3-years overall and cardiovascular mortality. The strongest prognosticator was a RVFAC < 35% for both overall and cardiovascular mortality, respectively, HR 4.8 (95% CI 2.4–9.4) and HR 14.7 (95% CI 6.26–31.96).
Interestingly, RV dysfunction was also predictive of overall mortality at 3-years in two subgroups of the cohort:
-
in the CABG subgroup of 172 patients: S′ < 10 cm/s and RVFAC < 35% were predictive of overall mortality (HR 3.8, 95% CI 1.4–10.3 and HR 5.1, 95% CI 2.4–11.7, respectively, P value = 0.001);
-
in the valve subgroup of 183 patients: S′ < 10 cm/s, RVFAC < 35% and IVA < 1.8 m/s2 were predictive of overall mortality (HR 3.3, 95% CI 1.6–8.1, HR 4.9, 95% CI 2.3–10.5 and HR 1.9, 95% CI 1.1–4.2, respectively, P value = 0.001 for S′ and RVFAC and P value 0.002 for IVA).
RV afterload using sPAP and PVR were both predictive of overall mortality in univariate analysis. HR for sPAP was 1.03 (95% CI 1.01–1.05) with a P value = 0.004 and HR for PVR was 1.5 (95% CI 1.13–2.09) with a P value = 0.006.
In multivariate regression analysis (Tables 4, 5), S′, RVFAC, dP/dt and IVA after adjustment to the EuroSCORE, remained prognosticator for overall and cardiovascular mortality. The strongest predictor was RVFAC < 35% for both overall and cardiovascular mortality, respectively, HR 3.0 (95% CI 1.5–6.1) and HR 10.5 (95% CI 4.3–19.9) (Tables 4, 5; Fig. 2).
Systolic PAP and PVR did not influence significantly the overall survival in a multivariate model adjusted to S′ and RVFAC [HR for sPAP was 1.00 (95% CI 0.98–1.02) with a P value = 0.96 and HR for PVR was 1.03 (95% CI 0.91–1.17) with a P value = 0.65].
Discussion
This study shows (1) the high prevalence of RV dysfunction in patients planned for cardiac surgery (i.e. ranging from 9 to 34%) and (2) the importance of pre-operative RV dysfunction as a prognosticator for overall and cardiovascular mortality.
Assessment of RV function
This study used echocardiography, although cardiac magnetic resonance imaging (CMR) is considered as gold standard for RVEF measurement. However, CMR is not easily available everywhere for cardiac purpose, especially as a daily to use prognostic tool. Moreover, CMR has an imperfect reproducibility: in an interstudy reproducibility work [19], CMR showed a variation of 8.3% (4.3–10.4%) for RVEF measurement and 14.1% (8.1–18.1%) for end-systolic volume. In the literature, the interobserver coefficient of variation of RVEF measurement has been found to be up to 10.7% [20] and can increase to 16% in particular situations [21]. More specifically RVEF measurement using CMR is limited by lack of standardization and unknown issues (i.e. valvular plane measurement, evaluation of apical trabeculations, issues about acquisition protocol, differences between manufacturers’ software packages). Finally, RVEF whatever the technique of measurement applied is a reflection of contractility, preload and afterload. While global hemodynamic is possible to assess by the use of echocardiography, it is still challenging to assess pre and afterload using CMR. Our study underlines that echocardiography is a first line method for the assessment of RV function and identification of patient at risk. Hence, echocardiography is considered as a qualitative tool for the evaluation of the RV function until 2005 [22], exploded these last years by proposing numerous quantitative parameters individually validated. Indeed, indices of longitudinal and radial RV function, isovolumic periods, indices of preload and afterload (pulmonary vascular resistance and pressure) are easily available.
RVFAC depends on both radial and longitudinal RV function and thus, can be considered as an indirect approach of the RVEF [23] with the same limitations (preload and afterload dependency).
S′ and TAPSE are very similar, measuring the same physiological phenomenon—the longitudinal displacement—and both depend on load conditions. RMPI is considered as a global RV function parameter with also a load dependency.
Of all these parameters of RV function, IVA is the less load dependant, which best reflect intrinsic contractility with a good correlation with the slope of elastance curve [15, 17]. Interestingly, guidelines do not recommend IVA as a first line parameter [8] or even ignore it [24] while our results strongly underline the diagnostic and the prognostic value of IVA. All these parameters have a good reproducibility and feasibility to allow a routine use [17], particularly for IVA (coefficient of variation for inter and intraobserver reproducibility 1.9 and 2.1%, respectively).
According to the recommendations, RV dysfunction diagnosis should be based on a single parameter among RVFAC, S′, TAPSE while RMPI should not be applied alone. However, our data strongly support a multiparametric approach for at least three reasons. First, the definition of RV dysfunction remains an issue in clinical practice. In our population, RV dysfunction prevalence was variable according to the parameter used, ranging from 9 to 38%. This is in accordance with recent findings, among 250 patients evaluated before cardiac surgery: 8% had RV dysfunction using RVFAC, 14% using TAPSE, and 40% using 2D strain [25]. These apparent discrepancies could be explained mainly by the fact that these indices are more complementary than similar: S′ is a regional parameter exploring the longitudinal function while RVFAC is more global and IVA explores isovolumic period; Second, the extreme susceptibility of the RV to load conditions which forces to consider the RV function in its loading conditions, its particular anatomy and its physiology, makes the monoparametric study not reasonable. Indeed, these parameters are modified differently by loading conditions [17]. The addition of several parameters should not be redundant, allowing not only the study of many complementary physiological aspects of RV function (longitudinal, radial, global function, isovolumic period, deformation), but also the afterload (pulmonary resistance, LV filling pressure). Third, logically, combining any of the RV parameters tested in the present work should increase the prediction of both endpoints (overall or cardiovascular survival) but only further large-scale study testing a dedicated multiparametric approach with a long-term longitudinal follow-up will demonstrate how many of this hypothesis is accurate.
Prognostic value
Previous studies focusing on long-term prognosis of patient planned for cardiac surgery have suggested the prognostic importance of RV function. These studies are limited by the small number of patients and most of the time by a monoparametric approach. One of the first study showed, in patients with mitral or mitro-aortic valve disease, that preoperative RV dysfunction assessed qualitatively (382 patients) was a strong predictor of 5-years postoperative mortality (38 vs 4% if no RV dysfunction) [1]. Later in a very small study including 14 patients, preoperative RV dysfunction identified using RVEF < 20% [3] has been shown to be associated with an increased 9-years mortality after mitral surgery. In a retrospective study [4] involving 41 patients with ischemic cardiomyopathy and LVEF < 25% undergoing coronary artery bypass surgery, the presence of RV dysfunction defined as RVFAC < 35% was associated with an increase of 2-years mortality (100 vs 9% if no RV dysfunction). RMPI has also been shown as having an incremental value in predicting postoperative mortality in valvular heart surgery [5]: in a prospective study involving 50 patients, a RMPI threshold >0.5 increases significantly the risk of postoperative mortality and circulatory failure (OR 25.2). Recently, Garatti et al. [6] demonstrated that preoperative RV dysfunction assessed by TAPSE < 16 mm in 324 patients was also associated with an increased risk of 5-years mortality (39 vs 17% if no RV dysfunction) and 8-years mortality (52 vs 23%).
In few studies, preoperative evaluation of RV function was performed using a multiparametric approach. In 250 patients referred for cardiac surgery, among RVFAC, TAPSE and global longitudinal strain (GLS), only RV GLS was associated with patient outcome (1-month mortality) by multivariate analysis adjusted to EuroSCORE [25]. In 539 patients with previous left heart procedure (time from procedure to enrolment 50 ± 30 months) followed for 53 ± 15 months, RVFAC was associated with mortality in multivariate analysis (with age, LA size, diabetes, previous CABG) [26].
Multiparametric approach has also been applied in non cardiac surgery studies: In 136 patients with heart failure, S′ predicted mortality in multivariate analysis (among RVFAC, TAPSE and S′) [27]; As well, in 575 patients with pulmonary hypertension, RV GLS predicted mortality in multivariate analysis (S′, Tei, TAPSE and RVFAC were also tested) [28].
In the present study, S′, RVFAC, IVA and dP/dt predicted overall and cardiovascular mortality in multivariate analysis. Interestingly, these parameters explore various physiological aspects of the RV function: IVA, which is non-load dependent, reflects the intrinsic myocardial contractility while S′ and RVFAC measure, respectively, the longitudinal and the radial function and are both load dependent. Of note, IVA has been surprisingly occulted in the most recent guidelines dealing with cardiac cavities measurement [24].
Our results also show that in absence of RV dysfunction, overall survival was excellent at 3 years follow-up. Interestingly, all these results were adjusted to the EuroSCORE quartiles and apply whatever the preoperative EuroSCORE value.
Conclusions
Nowadays, RV function is not included in risk stratification model such as EuroSCORE, widely applied in Europe. The present study demonstrates the importance of preoperative evaluation of RV function, since this evaluation has an independent prognostic value on top of EuroSCORE, and this is true whatever the initial preoperative risk level. Early recognition of RV dysfunction would help to guide the decision to improve the risk stratification before cardiac surgery, and change the pattern of follow-up in high-risk patients or when the indication is ambiguous.
Limitations
To avoid redundancy, we used S′, but not TAPSE. Indeed, TAPSE and S′ measure the same phenomenon—the longitudinal displacement of the tricuspid annulus—and are both load dependant. Moreover, there is no need to record a new image for S′, since the same record allows to measure Tei, IVA, and S′. Finally, TAPSE reproducibility is questionable. In a study by Miller [29], the interobserver variability for TAPSE, was 9.0 ± 7.6%.
In the present study, we did not perform 3D RV ejection fraction (RVEF) because our aim was to follow newest guidelines and to validate parameters of everyday life, easy to record with all the echo machines available on the market and no time consuming; However, RVFAC and RVEF have been correlated in various work, and both parameters have the same limitations (load dependency).
Abbreviations
- CI:
-
Confidence interval
- CMR:
-
Cardiac magnetic resonance imaging
- GLS:
-
Global longitudinal strain
- HR:
-
Estimated hazard ratios
- IVA:
-
Isovolumic acceleration
- IVRT:
-
Isovolumic relaxation time
- LVEF:
-
Left ventricular ejection fraction
- PVR:
-
Pulmonary vascular resistance
- RMPI:
-
Right myocardial performance index
- RV:
-
Right ventricle
- RVEF:
-
Right ventricular ejection fraction
- RVFAC:
-
Right ventricular fractional area change
- S′:
-
Doppler-derived tricuspid lateral annular systolic velocity
- SD:
-
Standard deviation
- sPAP:
-
Systolic pulmonary artery pressure
- TAPSE:
-
Tricuspid annular plane systolic excursion
- TDI:
-
Tissue Doppler imaging
- TR:
-
Tricuspid regurgitation
References
Pinzani A, de Gevigney G, Pinzani V, Ninet J, Milon H, Delahaye JP (1993) Pre- and postoperative right cardiac insufficiency in patients with mitral or mitral-aortic valve diseases. Arch Mal Coeur Vaiss 86(1):27–34
Boldt J, Zickmann B, Herold C, Dapper F, Hempelmann G (1992) Right ventricular function in patients with reduced left ventricular function undergoing myocardial revascularization. J Cardiothorac Vasc Anesth 6(1):24–28
Wencker D, Borer JS, Hochreiter C, Devereux RB, Roman MJ, Kligfield P, Supino P, Krieger K, Isom OW (2000) Preoperative predictors of late postoperative outcome among patients with nonischemic mitral regurgitation with ‘high risk’ descriptors and comparison with unoperated patients. Cardiology 93(1–2):37–42
Maslow AD, Regan MM, Panzica P, Heindel S, Mashikian J, Comunale ME (2002) Precardiopulmonary bypass right ventricular function is associated with poor outcome after coronary artery bypass grafting in patients with severe left ventricular systolic dysfunction. Anesth Analg 95(6):1507–1518
Haddad F, Denault AY, Couture P, Cartier R, Pellerin M, Levesque S, Lambert J, Tardif JC (2007) Right ventricular myocardial performance index predicts perioperative mortality or circulatory failure in high-risk valvular surgery. J Am Soc Echocardiogr 20(9):1065–1072
Garatti A, Castelvecchio S, Di Mauro M, Bandera F, Guazzi M, Menicanti L (2015) Impact of right ventricular dysfunction on the outcome of heart failure patients undergoing surgical ventricular reconstruction. Eur J Cardiothorac Surg 47(2):333–340
Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R (1999) European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg 16(1):9–13
Abbas AE, Fortuin FD, Schiller NB, Appleton CP, Moreno CA, Lester SJ (2003) A simple method for noninvasive estimation of pulmonary vascular resistance. J Am Coll Cardiol 41:1021–1027
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23(7):685–713
Kaul S, Tei C, Hopkins JM, Shah PM (1984) Assessment of right ventricular function using two-dimensional echocardiography. Am Heart J 107(3):526–531
Anavekar NS, Gerson D, Skali H, Kwong RY, Yucel EK, Solomon SD (2007) Two-dimensional assessment of right ventricular function: an echocardiographic-MRI correlative study. Echocardiography. 24(5):452–456
Vinereanu D, Khokhar A, Fraser AG (1999) Reproducibility of pulsed wave tissue Doppler echocardiography. J Am Soc Echocardiogr 12(6):492–499
Meluzín J, Spinarová L, Bakala J et al (2001) Pulsed Doppler tissue imaging of the velocity of tricuspid annular systolic motion; a new, rapid, and non-invasive method of evaluating right ventricular systolic function. Eur Heart J 22(4):340–348
Tei C, Dujardin KS, Hodge DO et al (1996) Doppler echocardiographic index for assessment of global right ventricular function. J Am Soc Echocardiogr 9(6):838–847
Vogel M, Schmidt MR, Kristiansen SB et al (2002) Validation of myocardial acceleration during isovolumic contraction as a novel noninvasive index of right ventricular contractility: comparison with ventricular pressure-volume relations in an animal model. Circulation 105(14):1693–1699
Anconina J, Danchin N, Selton-Suty C et al (1992) Measurement of right ventricular dP/dt. A simultaneous/comparative hemodynamic and Doppler echocardiographic study. Arch Mal Coeur Vaiss 85(9):1317–1321
Peyrou J, Parsaï C, Chauvel C, Simon M, Dehant P, Abergel E (2014) Echocardiographic assessment of right ventricular systolic function in a population of unselected patients before cardiac surgery: a multiparametric approach is necessary. Arch Cardiovasc Dis 107(10):529–539
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94:496–509
Grothues F, Moon JC, Bellenger NG, Smith GS, Klein HU, Pennell DJ (2004) Interstudy reproducibility of right ventricular volumes, function, and mass with cardiovascular magnetic resonance. Am Heart J 147:218–223
Hudsmith LE, Petersen SE, Francis JM, Robson MD, Neubauer S (2005) Normal human left and right ventricular and left atrial dimensions using steady state free precession magnetic resonance imaging. J Cardiovasc Magn Reson 7:775–782
Bonnemains L, Mandry D, Marie PY, Micard E, Chen B, Vuissoz PA (2012) Assessment of right ventricle volumes and function by cardiac MRI: quantification of the regional and global interobserver variability. Magn Reson Med 67:1740–1746
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ, Chamber Quantification Writing Group; American Society of Echocardiography’s Guidelines and Standards Committee; European Association of Echocardiography (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18(12):1440–1463
Caudron J, Fares J, Lefebvre V, Vivier PH, Petitjean C, Dacher JN (2012) Cardiac MRI assessment of right ventricular function in acquired heart disease: factors of variability. Acad Radiol 19(8):991–1002. doi:10.1016/j.acra.2012.03.022
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28(1):1-39.e14
Ternacle J, Berry M, Cognet T, Kloeckner M, Damy T, Monin JL, Couetil JP, Dubois-Rande JL, Gueret P, Lim P (2013) Prognostic value of right ventricular two-dimensional global strain in patients referred for cardiac surgery. J Am Soc Echocardiogr 26(7):721–726
Kammerlander AA, Marzluf BA, Graf A, Bachmann A, Kocher A, Bonderman D, Mascherbauer J (2014) Right ventricular dysfunction, but not tricuspid regurgitation, is associated with outcome late after left heart valve procedure. J Am Coll Cardiol 64(24):2633–2642
Damy T, Viallet C, Lairez O, Deswarte G, Paulino A, Maison P, Vermes E, Gueret P, Adnot S, Dubois-Randé JL, Hittinger L (2009) Comparison of four right ventricular systolic echocardiographic parameters to predict adverse outcomes in chronic heart failure. Eur J Heart Fail 11(9):818–824
Fine NM, Chen L, Bastiansen PM, Frantz RP, Pellikka PA, Oh JK, Kane GC (2013) Outcome prediction by quantitative right ventricular function assessment in 575 subjects evaluated for pulmonary hypertension. Circ Cardiovasc Imaging 6(5):711–721
Miller D, Farah MG, Liner A, Fox K, Schluchter M, Hoit BD (2004) The relation between quantitative right ventricular ejection fraction and indices of tricuspid annular motion and myocardial performance. J Am Soc Echocardiogr 17(5):443–447
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author Eric Abergel states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Peyrou, J., Chauvel, C., Pathak, A. et al. Preoperative right ventricular dysfunction is a strong predictor of 3 years survival after cardiac surgery. Clin Res Cardiol 106, 734–742 (2017). https://doi.org/10.1007/s00392-017-1117-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-017-1117-y