Abstract
Background
Anemia and hypoalbuminemia (HA) are acknowledged independent risk factors for morbidity and mortality in geriatric patients and are associated with nutritional status and frailty. Data exist regarding the association between albumin and frailty, anemia and frailty as well as frailty and nutritional status; however, there is a lack of information on the association between HA, anemia and nutritional status in older people.
Patients and methods
This study retrospectively analyzed 626 patients admitted to a German geriatrics department (average age 81.1 years, 68.2 % female and 31.8 % male) for anemia and HA. Data from the comprehensive geriatric assessment (CGA) and from the mini-nutritional assessment (MNA) were available in all patients.
Results
Patients with anemia suffered significantly more often from HA (p < 0.001) than patients without anemia, with an odds ratio (OR) of 1.99 (95 % confidence interval CI: 1.2-3.2) and of 5.41 (CI 95 %: 2.3-12.6) in patients at risk for malnutrition and in malnourished patients, respectively. A moderately significant association was seen between hemoglobin (Hb) and albumin values (Pearson’s correlation r = 0.330; p < 0.001) as well as between albumin values and the Barthel index (Spearman’s correlation r = 0.210; p < 0.001).
Conclusion
Anemia appears to be a risk factor for HA in inpatients with malnutrition and the observed association between albumin and Hb warrants further research. Geriatric inpatients with anemia should be evaluated in terms of the presence of malnutrition risk and HA.
Zusammenfassung
Hintergrund
Anämie und Hypoalbuminämie (HA) sind bei geriatrischen Patienten bekannte unabhängige Risikofaktoren für Morbidität und Mortalität, sie stehen im Zusammenhang mit Ernährungststatus und Frailty. Es gibt Untersuchungen zum Zusammenhang zwischen Albumin und Frailty, Anämie und Frailty, sowie Frailty und dem Ernährungsstatus. Bisher fehlen jedoch Daten zu einem Zusammenhang zwischen HA, Anämie und Ernährungsstatus bei geriatrischen Patienten.
Patienten und Methoden
Retrospektive Datenanalyse von 626 stationären geriatrischen Patienten (mittleres Alter 81,1 Jahre, 68,2 % Frauen, 31,8 % Männer) hinsichtlich Anämie, HA und einem Zusammenhang mit dem Ernährungsstatus (Mini Nutritional Assessment, MNA) und dem multidimensionalen geriatrischen Assessment (Comprehensive Geriatric Assessment, CGA).
Ergebnisse
Patienten mit Anämie wiesen signifikant häufiger eine HA auf (p < 0,001) als Patienten ohne Anämie, wobei anämische Patienten mit einem Risiko für Mangelernährung eine erhöhte Chance auf eine HA hatten (OR I,9; 95 %-KI: 1,2-3,2) und Patienten mit einer Mangelernährung eine OR von 5,4 (95 %-KI: 2,3-12,6) aufwiesen. Ein moderater signifikanter Zusammenhang konnte gezeigt werden zwischen Hämoglobin (Hb) und Albumin (Pearsons Korrelationskoeffizient r = 0,330; p < 0,001) sowie zwischen Albumin und Barthel Index.
Schlussfolgerungen
Anämie scheint bei mangelernährten stationär geriatrischen Patienten ein Risikofaktor für HA zu sein, wobei der beobachtete Zusammenhang zwischen Albumin und Hb weiterer wissenschaftlicher Untersuchungen bedarf. Im klinischen Alltag sollte bei stationär geriatrischen Patienten mit Anämie eine Überprüfung auf HA erwogen werden, besonders bei drohender oder bereits bestehender Mangelernährung.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anemia and hypoalbuminemia (HA) have been shown to be associated with frailty in older people [19, 24, 36, 37] and frailty has been shown to be closely associated with nutritional status in the elderly [5, 20]. Low albumin blood levels have been previously shown to be associated with anemia [27, 29, 34, 35,] but comparable analyses among German inpatients are, however, currently lacking.
Anemia is a common problem in older people
Anemia is a common problem in older people [3, 15]. Depending on the patient cohort, the prevalence may vary between 20 % among independent community-dwelling seniors and 40–60 % among inpatients [14, 15, 46]. Anemia in older people has been shown to be associated with increased morbidity and mortality as well as with a higher rate of hospitalization and longer hospital stay [9, 42]. Anemia also appears to be associated with impaired cognitive function in patients over 70 years of age [38]. A recent systematic review by Andro et al. identified several studies showing a significant association between anemia and cognitive decline, incidence of dementia and reduced executive functions [1]. Several risk factors for anemia have been identified in geriatric patients, such as chronic kidney disease [33, 45], iron deficiency and inflammation [30, 32].
The association between nutritional status and frailty is widely acknowledged
The role of albumin as a nutritional marker still remains controversial
Low serum albumin is also acknowledged to be a risk factor for mortality and morbidity [2, 13]. A recent study in older subjects with femoral neck fractures showed that albumin was a significant predictor of 12-month survival [23]. Similar findings could be shown by Kato et al. in cardiology patients undergoing heart surgery [22]. Furthermore, low serum albumin levels have been shown to be associated with anemia in smaller cohorts [27, 29, 34, 35]. The association of functional decline and serum albumin has been studied before. Isaia et al. could show an increased functional decline in Italian geriatric patients who had been admitted to hospital and presented with low serum albumin [18]. The association between nutritional status and frailty is widely acknowledged [5, 20]. Smit et al. showed a dependency of frailty on daily energy intake among older American adults and the authors additionally reported lower serum albumin levels in the frail than in the not frail subgroups of this patient cohort [37]; however, despite the fact that albumin was found to be associated with nutritional status in many studies [27, 35], the role of albumin as a nutritional marker still remains controversial [16, 25]. The present study aimed to fill the gap in knowledge on the relationship between anemia, HA and nutritional status in a typical geriatric inpatient population. Another aim of the study was to address the presence and degree of functional impairment as assessed by means of the comprehensive geriatric assessment (CGA), the cornerstone of geriatric methodology.
Patients and methods
The ethics commission of the Cologne University Faculty of Medicine approved the study (No 11-032) and it was performed in accordance with the 1964 Declaration of Helsinki and its later amendments. The study data was based on 1252 patients routinely evaluated by the clinical nutritionist between January and December 2011 at the Geriatric Department of the University Hospital at St. Marien Hospital in Cologne, Germany. Data were retrospectively collected on nutritional status, diagnosis on admission with the international classification of diseases version 10 (ICD 10), body mass index (BMI, kg/m2, laboratory data and the CGA score. Patients with edema were excluded to avoid dilution-associated anemia and HA in the analysis. Patients with inflammation were also excluded from the analysis based on a C-reactive protein (CRP) value > 6 mg/l and a ferritin value > 651 ng/ml [7, 39] but patients with reduced glomerular filtration rate (GFR) were not excluded because approximately 60 % of the study patients showed a GFR < 90 ml/min and recent findings revealed that a reduction of GFR does not necessarily predispose to HA [12]. Due to a lack of data, liver disease as a possible reason for reduced albumin synthesis could not be excluded. A total of 626 patients could be included in the final analysis. Nutritional risk at hospital admission was assessed using the modified mini-nutritional assessment (m-MNA), a validated tool specially developed for older people [16]. The m-MNA includes the assessment of BMI, weight loss, mobility, food intake, number of main dishes consumed, fluid intake and self-assessment of health status. Based on the m-MNA scores, patients were divided into three groups: without malnutrition (group A), at risk for malnutrition (group B) and malnourished patients (group C) [21]. The CGA scores from all patients were included in the analysis. In this setting the CGA consisted of the Barthel index [26], Tinetti test [40] and timed up and go (TUG) test [31] for the functional assessment, mini-mental state examination (MMSE) [11] and clock drawing test [41] for the cognitive status and the geriatric depression scale (GDS) [44] to screen for major depression. Laboratory parameters included in the analysis comprised hemoglobin (Hb, g/dl) using the sodium lauryl sulphate (SLS) method (Sysmex®Analyzer XE-2100/XE-5000, Sysmex, Norderstedt Germany), serum albumin (g/dl, photometric method, Beckman Coulter® Analyzer, Beckmann Coulter, Krefeld Germany ), CRP (mg/l) (immune turbidimetric method, Beckman Coulter® analyzer), folate (ng/ml, immunoassay, Cobas®, Roche, Mannheim, Germany), serum calcium (mmol/l, photometric arsenazo method, Beckman Coulter® analyzer), transferrin (mg/dl, immune turbidimetric method, Beckman Coulter® analyzer) with calculated transferrin saturation (%), ferritin (µg/l, immune turbidimetric method, Beckman Coulter® analyzer), vitamin B12 (ng/ml, electro-chemiluminescence ECLIA immunoassay, Cobas®) and creatinine/estimated GFR (ml/min), Jaffé method, Beckman Coulter® analyzer and modification of diet in renal disease formula MDRD). While the estimated GFR could be considered in the statistical analysis, the absolute levels of creatinine were not available. For this study HA was defined as serum albumin< 3.5 g/dl, anemia was defined as Hb < 12 g/dl (females) and Hb < 13 g/dl (males) [4]. Statistical analysis was performed by means of the IBM SPSS statistical package Version 20.0 (IBM, Armonk NY). The main parameters Hb and albumin were analyzed as original metric data. Frequencies were compared by the χ2-test, normally distributed variables by the t-test or ANOVA for more than two groups and two normally distributed variables by Pearson’s correlations. For association between anemia and albumin odds ratios (OR) with 95 % confidence intervals (CI) were calculated. Assessment tests and laboratory variables were analyzed as categorical data, distinguishing between pathological or normal values. The significance level was defined at 0.05.
Results
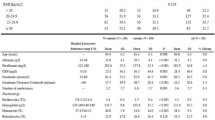
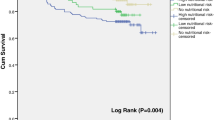
Descriptive characteristics of the 626 patients are shown in Table 1 including 427 women (68.2 %) and 199 men (31.8 %). The most frequent diagnoses according to ICD 10 that were found in more than 3 % of study patients are shown in Table 2. The high number with the diagnosis reduced mobility (32.3 %) is related to the relatively low number of TUG and Tinetti test results on admission, which were often not possible to be conducted due to a reduced functional status of the patient. The prevalence of anemia in all 626 patients was 67.9 % (425) with 66.0 % (282 out of 427) in women and 71.9 % (143/199) in men. The prevalence of HA was 39.8 % (249/626), 40.5 % (173/427) in women and 38.2 % (76/199) in men (Table 1). Patients with HA had lower Hb levels, more often anemia, a lower Barthel index, lower BMI, higher vitamin B12 levels as well as lower levels of serum calcium than patients without HA. These differences were highly significant (p < 0.001) (Table 1). Ferritin and folate levels were significantly higher in hypoalbuminemic patients than in patients with normal albumin values (p = 0.008 and p = 0.004, respectively). In patients with anemia, HA was present significantly more often as well as lower albumin levels, lower serum calcium levels and higher CRP levels than in patients without anemia (p < 0.001). Anemic patients had significantly lower GFR values than patients without anemia (p < 0.05). No significant differences in CGA scores were seen among the groups. One-way ANOVA revealed that depending on the nutritional status according to the m-MNA, albumin levels, the BMI and Barthel index differed significantly (p < 0.001): the lowest albumin levels, BMI and Barthel index were found in patients with malnutrition (group C) compared to better nourished patients of m-MNA groups A and B. No statistically significant differences were seen for Hb levels (Table 3). A weak to moderately significant correlation was observed between albumin and Hb values (Pearson's correlation r = 0.33; p < 0.001) as well as between albumin values and the Barthel index (r = 0.21, p < 0.001). No other associations were observed. Patients with anemia had an elevated chance (OR 2.6, 95 % CI 1.8-3.9) to be hypoalbuminemic. Anemic patients at risk for malnutrition (m-MNA group B) showed an OR of 1.99 (95 % CI 1.2-3.2) to be hypoalbuminemic, reaching an OR of 5.41 (95 % CI 2.3-12.6) in malnourished patients belonging to m-MNA group C. No correlation between anemia and HA was found in m-MNA group A patients (OR 2.6, 95 % CI 0.95-7.3).
Discussion
The main result of this study is that anemia was found to be associated with HA and malnutrition in this geriatric population. Anemic patients at risk for malnutrition have an increased risk of hypoalbuminemia and this risk increases even more in malnourished patients. To the best of our knowledge this increase has not been described before among geriatric inpatients. An association between Hb and albumin values in older patients has been described before among geriatric patients outside of Germany but data are scarce and most of the studied patient cohorts are smaller than the present geriatric inpatient cohort [27, 29, 34, 35]. The prevalence of HA found in this patient cohort is similar to that found in previous studies. In the study of Mizrahi et al. HA was found in 38.8 % of geriatric patients on admission [28]. The high prevalence of anemia in the present study sample is comparable to the prevalence recently described by Chan et al. of 67 % in 812 old nursing home adults [8]. The data are also consistent with another recent study on 100 geriatric inpatients, in which a prevalence of 60 % was observed [46]. In this study cohort HA was associated with all abnormal laboratory values with the exception of GFR and transferrin saturation. Recent findings by Friedman et al. revealed that a reduction of GFR does not necessarily predispose to HA [12]. Bonilla-Palomas et al. described an independent association between HA and low transferrin values in patients with acute heart failure [6].
Different patient characteristics between the studies might be responsible for the different results. As hypoalbuminemic patients have a significantly lower body weight and significantly lower folate, vitamin B12 and serum calcium levels, an association between albumin and nutritional status might be assumed. In most of the studies albumin is associated with nutritional status [27, 35]; however, the role of albumin as a nutritional marker still remains controversial [16, 25]. The association between anemia, HA and nutritional status in this study cohort might suggest protein deficiency anemia but a causality cannot be proven due to a lack of variables of visceral protein storage (e.g. coagulation factors and liver function) and somatic protein storage (skeletal muscle mass). The association of HA with elevated levels of folate and vitamin B12 might be due to the role of albumin as a transport protein: a lack of albumin might result in higher levels of free folate and vitamin B12 [17]. Another important finding of this study is the observed association of HA values with the Barthel index, lower body weight and anemia (Table 1) which are all factors that have been associated with frailty [10, 19]. Although the identification of frailty was not an aim of the present study, the findings are consistent with an earlier frailty study on a smaller patient cohort by Silva et al. [36]. In that study, an association between HA, nutrition status and functionality assessed by the Barthel index was found. Isaia et al. could also show a reduced functionality in relation to low serum albumin levels [18]. As ICD 10 does not include a code for frailty, in Germany medical controllers resort to disease codes describing symptoms of frailty, indicating the need for geriatric treatment, such as R15, R26.8, R29.6 and R32 [43]. In this patient cohort, the diagnosis code reduced mobility (R26.8, ICD 10) was found in one third of the patients as the main diagnosis (Table 2). This finding implies functional problems that are assumed to be caused by reasons other than the main diagnosis, such as hip fractures (S72.-) or stroke (I63.-) (Table 2). An association with frailty might be assumed but this assumption remains vague due to the lack of confirmatory data.
The strengths of this study include the size of the study population among geriatric inpatients in Germany. Moreover, the CGA including assessment of nutritional status was performed in a standardized manner by the application of validated tests [11, 26, 31, 40, 41, 44].
There are some shortcomings to this investigation. The retrospective nature and the broad, less precise selection of patients presenting to the nutritionist curtail an interpretation of the data.
Conclusion
This study shows that anemia and HA are highly prevalent in a typical German geriatric inpatient population. Anemia appears to be a risk factor for HA in malnourished geriatric inpatients, while HA is associated with reduced functionality based on the Barthel index. The study results support the assumption of an association between anemia and serum albumin which, to the knowledge of the authors, has not been shown before in a German geriatric inpatient cohort. These findings encourage further research in the complex field of frailty in association with nutritional status, anemia and HA and the effects on CGA in geriatric patients. A screening for HA should be considered in anemic geriatric inpatients, particularly if a nutritional risk screening (e.g. MNA) indicates malnutrition.
References
Andro M, Le Squere P, Estivin S, Gentric A (2013) Anaemia and cognitive performances in the older people: a systematic review. Eur J Neurol 20(9):1234–1240
Barchel D, Almoznino-Sarafian D, Shteinshnaider M, Tzur I, Cohen N, Gorelik O (2013) Clinical characteristics and prognostic significance of serum albumin changes in an internal medicine ward. Eur J Intern Med 24(8):772–778
Beghé C, Wilson A, Ershler WB (2004) Prevalence and outcomes of anaemia in geriatrics: a systematic review of the literature. Am J Med 116(Suppl 7A):3S–10S
Blanc B, Finch CA, Hallberg L (1968) Nutritional anaemias. Report of a WHO Scientific Group. World Health Organ Tech Rep Ser 405:1–40
Bollwein J, Volkert D, Diekmann R, Kaiser MJ, Uter W, Vidal K, Sieber CC, Bauer JM (2013) Nutritional status according to the mini nutritional assessment (MNA®) and frailty in community dwelling older persons: a close relationship. J Nutr Health Aging 17(4):351–356
Bonilla-Palomas JL, Gámez-López AL, Moreno-Conde M, López-Ibáñez MC, Anguita-Sánchez M, Gallego de la Sacristana A, García-Catalán F, Villar-Ráez A (2014) Hypoalbuminemia in acute heart failure patients: causes and its impact on hospital and long-term mortality. J Card Fail 20(5):350–358
Cankurtaran M, Yavuz BB, Halil M, Ulger Z, Haznedaroglu IC, Ariogul S (2012) Increased ferritin levels could reflect ongoing aging-associated inflammation and may obscure underlying iron deficiency in the geriatric population. Eur Geriatr Med 3:277–280
Chan TC, Yap DY, Shea YF, Luk JK, Chan FH, Chu LW (2013) Prevalence of anaemia in Chinese nursing home older adults: implication of age and renal impairment. Geriatr Gerontol Int 13(3):591–596
Chi Z, Mi SH, Zhang XX, Guan Y, Zhao QM, Wu XS (2012) Impact of anaemia on long-term outcome in older people patients with acute coronary syndrome undergoing percutaneous coronary interventions. Zhonghua Xin Xue Guan Bing Za Zhi 40:920–923
de la Rica-Escuín M, González-Vaca J, Varela-Pérez R, Arjonilla-García MD, Silva-Iglesias M, Oliver-Carbonell JL, Abizanda P (2014) Frailty and mortality or incident disability in institutionalized older adults: the FINAL study. Maturitas 78 (4):329–334
Folstein MF, Folstein SE, McHugh PR (1975) "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Friedman AN, Fadem SZ (2010) Reassessment of albumin as a nutritional marker in kidney disease. J Am Soc Nephrol 21(2):223–230
Fuhrmann MP (2002) The albumin-nutrition connection: separating myth from fact. Nutrition 18:199–200
Gaskell H, Derry S, Andrew Moore R, McQuay HJ (2008) Prevalence of anaemia in older persons: systematic review. BMC Geriatr 8:1
Guralnik JM, Eisenstaedt RS, Ferrucci L, Klein HG, Woodman RC (2004) Prevalence of anaemia in persons 65 years and older in the United States: evidence for a high rate of unexplained anaemia. Blood 104(8):2263–2268
Hengstermann S, Nieczaj R, Steinhagen-Thiessen E, Schulz RJ (2008) Which are the most efficient items of mini nutritional assessment in multimorbid patients? J Nutr Health Aging 12:117–122
Hou HN, Qi ZD, Ouyang YW, Liao FL, Zhang Y, Liu Y (2008) Studies on interaction between Vitamin B12 and human serum albumin. J Pharm Biomed Anal 47(1):134–139
Isaia G, Maero B, Gatti A, Neirotti M, Aimonino Ricauda N, Bo M, Ruatta C, Gariglio F, Miceli C, Corsinovi L, Fissore L, Marchetto C, Zanocchi M (2009) Risk factors of functional decline during hospitalization in the oldest old. Aging Clin Exp Res 21(6):453–457
Juárez-Cedillo T, Basurto-Acevedo L, Vega-García S, Manuel-Apolinar L, Cruz-Tesoro E, Rodríguez-Pérez JM, García-Hernández N, Pérez-Hernández N, Fragoso JM (2014) Prevalence of anemia and its impact on the state of frailty in elderly people living in the community: SADEM study. Ann Hematol 93(12):2057–2062
Jürschik P, Botigué T, Nuin C, Lavedán A (2014) Association between mini nutritional assessment and the fried frailty index in older people living in the community. Med Clin (Barc) 143(5):191–195
Kaiser MJ, Bauer JM, Ramsch C, Uter W, Guigoz Y, Anthony P, Charlton KE, Maggio M, Tsai AC, Grathwohl D, Vellas B, Sieber CC, MNA International Group (2009) Validation of the Mini Nutritional Assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging 13(9):782–788
Kato TS, Cheema FH, Yang J, Kawano Y, Takayama H, Naka Y, Farr M, Lederer DJ, Baldwin MR, Jin Z, Homma S, Mancini DM, Schulze PC (2013) Preoperative serum albumin levels predict 1-year postoperative survival of patients undergoing heart transplantation. Circ Heart Fail 6(4):785–791
Kumar V, Alva A, Akkena S, Jones M, Murphy PN, Clough T (2014) Are albumin and total lymphocyte count significant and reliable predictors of mortality in fractured neck of femur patients? Eur J Orthop Surg Traumatol 24(7):1193–1196
Kutner NG, Zhang R, Huang Y, McClellan WM, Soltow QA, Lea J (2014) Risk factors for frailty in a large prevalent cohort of hemodialysis patients. Am J Med Sci 348(4):277–282
Kuzuya M, Izawa S, Enoki H, Okada K, Iguchi A (2007) Is serum albumin a good marker for malnutrition in the physically impaired older people? Clin Nutr 26:84–90
Mahoney F, Barthel D (1965) Functional evaluation: the Barthel Index. Md State Med J 14:61–65
Mitrache C, Passweg JR, Libura J, Petrikkos L, Seiler WO, Gratwohl A, Stähelin HB, Tichelli A (2001) Anaemia: an indicator for malnutrition in the older people. Ann Hematol 80(5):295–298
Mizrahi EH, Fleissig Y, Arad M, Blumstein T, Adunsky A (2007) Admission albumin levels and functional outcome of older people hip fracture patients: is it that important? Aging Clin Exp Res 19(4):284–289
Nakashima AT, de Moraes AC, Auler F, Peralta RM (2012) Anaemia prevalence and its determinants in Brazilian institutionalized older people. Nutrition 28(6):640–643
Pang WW, Schrier SL (2012) Anaemia in the older people. Curr Opin Hematol 19(3):133–140
Podsiadlo D, Richardson S (1991) The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39:142–148
Ramel A, Jonsson PV, Bjornsson S, Thorsdottir I (2008) Anaemia, nutritional status, and inflammation in hospitalized older people. Nutrition 24(11–12):1116–1122
Röhrig G, Nobbe C, Weiß V, Schulz RJ. (2013) Hepcidin in anaemic geriatric patients with non-dialysis chronic kidney disease (ND-CKD) Eur Geriatr Med 4:221–225
Sasatomi Y, Ito K, Abe Y, Miyakle K, Nakashima H, Saito T (2012) Association of HA with severe anaemia in patients with diabetic nephrosclerosis. Ren Fail 34(2):189–193
Silva CL, Lima-Costa MF, Firmo JO, Peixoto SV (2012) Hemoglobin level in older adults and the association with nutritional status and use of health services: the Bambui Project. Cad Saude Publica 28(11):2085–2094
Silva JC, de Moraes ZV, Silva C, de Barros Mazon S, Guariento ME, Neri AL, Fattori A (2014) Understanding red blood cell parameters in the context of the frailty phenotype: interpretations of the FIBRA (Frailty in Brazilian Seniors) study. Arch Gerontol Geriatr 59(3):636–641
Smit E, Winters-Stone KM, Loprinzi PD, Tang AM, Crespo CJ (2013) Low nutritional status and higher food insufficiency in frail older US adults. Br J Nutr 110(1):172–178
Terekeci HM, Kucukardali Y, Onem Y, Erikci AA, Kucukardali B, Sahan B, Sayan O, Celik S, Gulec M, Sanisoglu YS, Nalbant S, Top C, Oktenli C (2010) Relationship between anaemia and cognitive functions in older people. Eur J Intern Med 21(2):87–90
Thomas L, Ansorg R, Arndt T, Barlage T (2005) Labor und Diagnose: Indikation und Bewertung von Laborbefunden für die medizinische Diagnostik, 6. Aufl. TH-Books, Frankfurt am Main
Tinetti ME (1986) Performance-oriented assessment of mobility problems in older people patients. J Am Geriatr Soc 34(2):119–126
Watson YI, Arfken CL, Birge SJ (1993) Clock completion: an objective screening test for dementia. J Am Geriatr Soc 41(11):1235–1240
Willems JM, de Craen AJ, Nelissen RG, van Luijt PA, Westendorp RG, Blauw GJ (2012) Haemoglobin predicts length of hospital stay after hip fracture surgery in older patients. Maturitas 72:225–228
www.update-arztpraxis.de. Zugegriffen: 26. Sept. 2014
Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, Leirer VO (1982) Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 39:37–49
Zaritsky J, Young B, Wang HJ, Westerman M, Olbina G, Nemeth E, Ganz T, Rivera S, Nissenson AR, Salusky IB (2009) Hepcidin—a potential novel biomarker for iron status in chronic kidney disease. Clin J Am Soc Nephrol 4:1051–1056
Zilinski, J Zillman R, Becker I, Schulz RJ, Benzing T, Röhrig G (2014) Prevalence of anemia among elderly inpatients and its association with multidimensional loss of function. Ann Hematol 93:1645–1654
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
G. Röhrig, I. Becker, M.C. Polidori, R.-J. Schulz and M. Noreik state that there are no conflicts of interest in connection with the content of this paper.
The ethics commission of the Cologne University Faculty of Medicine approved the study (No 11-032) and it was performed in accordance with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all patients included in this study.
Rights and permissions
About this article
Cite this article
Röhrig, G., Becker, I., Polidori, M. et al. Association of anemia and hypoalbuminemia in German geriatric inpatients. Z Gerontol Geriat 48, 619–624 (2015). https://doi.org/10.1007/s00391-015-0872-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00391-015-0872-5