Abstract
Purpose
To evaluate the clinical efficacy and safety of different analgesic interventions in the treatment of pain after open hemorrhoidectomy by systematic review and network meta-analysis.
Methods
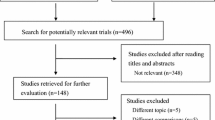
Randomized controlled trials that met the inclusion criteria in PubMed, Cochrane Library, Embase, Web of Science, Scopus, CNKI, WANFANG DATA, and VIP were searched from the date of database construction to June 28, 2022.
Results
Among the 13 randomized controlled trials (RCTs), 731 patients were included in the network meta-analysis. Most interventions are more effective than placebo in relieving postoperative pain. 24 h postoperative Visual Analogue Scale (VAS): glyceryl trinitrate (GTN) (mean difference (MD) − 4.20, 95% CI − 5.35, − 3.05), diltiazem (MD − 1.97, 95% CI − 2.44, − 1.51), botulinum toxin (BT) (MD − 1.50, 95% CI − 2.25, − 0.75), sucralfate (MD − 1.01, 95% CI − 1.53, − 0.49), and electroacupuncture (EA) (MD − 0.45, 95% CI − 0.87, − 0.04). 48 h postoperative VAS: diltiazem (MD − 2.45, 95% CI − 2.74, − 2.15), BT (MD − 2.18, 95% CI − 2.52, − 1.84), and sucralfate (MD − 1.41, 95% CI − 1.85, − 0.97). 7 d postoperative VAS: diltiazem (MD − 2.49, 95% CI − 3.20, − 1.78) and sucralfate (MD − 1.42, 95% CI − 2.00, − 0.85). The first postoperative defecation VAS: EA (MD − 0.70, 95% CI − 0.95, − 0.46). There are few data on intervention safety, and additional high-quality RCTs are expected to study this topic in the future.
Conclusion
Diltiazem ointment may be the most effective medication for pain relief following open hemorrhoidectomy, and it can dramatically reduce pain within one week of surgery. The second and third recommended medications are BT and sucralfate ointment. GTN has a significant advantage in alleviating pain 24 h after open hemorrhoidectomy, but whether it causes headache is debatable; thus, it should be used with caution. EA’s analgesic efficacy is still unknown. There was limited evidence on the safety of the intervention in this study, and it was simply presented statistically.






Similar content being viewed by others
References
van Tol RR, Kleijnen J, Watson AJM, Jongen J, Altomare DF, Qvist N et al (2020) European Society of ColoProctology: guideline for haemorrhoidal disease. Colorectal Dis 22(6):650–662
Peery AF, Crockett SD, Barritt AS, Dellon ES, Eluri S, Gangarosa LM et al (2015) Burden of gastrointestinal, liver, and pancreatic diseases in the United States. Gastroenterology 149(7):1731–1741.e1733
Sandler RS, Peery AF (2019) Rethinking what we know about hemorrhoids. Clin Gastroenterol Hepatol 17(1):8–15
Hosch SB, Knoefel WT, Pichlmeier U, Schulze V, Busch C, Gawad KA et al (1998) Surgical treatment of piles: prospective, randomized study of Parks vs Milligan-Morgan hemorrhoidectomy. Dis Colon Rectum 41(2):159–164
Lohsiriwat V, Jitmungngan R (2022) Strategies to reduce post-hemorrhoidectomy pain: a systematic review. Medicina (Kaunas) 58:3. https://doi.org/10.3390/medicina58030418
Bhatti MI, Sajid MS, Baig MK (2016) Milligan-Morgan (open) versus Ferguson haemorrhoidectomy (closed): a systematic review and meta-analysis of published randomized, controlled trials. World J Surg 40(6):1509–1519
Simillis C, Thoukididou SN, Slesser AA, Rasheed S, Tan E, Tekkis PP (2015) Systematic review and network meta-analysis comparing clinical outcomes and effectiveness of surgical treatments for haemorrhoids. Br J Surg 102(13):1603–1618
Joshi GP, Neugebauer EA (2010) Evidence-based management of pain after haemorrhoidectomy surgery. Br J Surg 97(8):1155–1168
Bindu S, Mazumder S, Bandyopadhyay U (2020) Non-steroidal anti-inflammatory drugs (NSAIDs) and organ damage: a current perspective. Biochem Pharmacol 180:114147
Seth P, Rudd RA, Noonan RK, Haegerich TM (2018) Quantifying the epidemic of prescription opioid overdose deaths. Am J Public Health 108(4):500–502
Rudiman R, Hanafi RV, Evan C, Halim F (2022) The efficacy of topical sucralfate in improving pain and wound healing after haemorrhoidectomy procedure: a systematic review, meta-analysis, and meta-regression of randomised clinical trials. Int Wound J. https://doi.org/10.1111/iwj.13901
Sammour T, Barazanchi AW, Hill AG (2017) Evidence-based management of pain after excisional haemorrhoidectomy surgery: a PROSPECT review update. World J Surg 41(2):603–614
Matak I, Bölcskei K, Bach-Rojecky L, Helyes Z (2019) Mechanisms of botulinum toxin type A action on pain. Toxins (Basel) 11(8). https://doi.org/10.3390/toxins11080459
Sirikurnpiboon S, Jivapaisarnpong P (2020) Botulinum toxin injection for analgesic effect after hemorrhoidectomy: a randomized control trial. J Anus Rectum Colon 4(4):186–192
Jonas M, Amin S, Wright JW, Neal KR, Scholefield JH (2001) Topical 0.2 percent glyceryl trinitrate ointment has a short-lived effect on resting anal pressure. Dis Colon Rectum 44(11):1640–1643
Carapeti EA, Kamm MA, Evans BK, Phillips RK (1999) Topical diltiazem and bethanechol decrease anal sphincter pressure without side effects. Gut 45(5):719–722
Masuelli L, Tumino G, Turriziani M, Modesti A, Bei R (2010) Topical use of sucralfate in epithelial wound healing: clinical evidences and molecular mechanisms of action. Recent Pat Inflamm Allergy Drug Discov 4(1):25–36
Gupta PJ, Heda PS, Kalaskar S, Tamaskar VP (2008) Topical sucralfate decreases pain after hemorrhoidectomy and improves healing: a randomized, blinded, controlled study. Dis Colon Rectum 51(2):231–234
Shuming Z, Fang C, Fuchun W (2017) Analysis of acupoint selection rules in modern literature on acupuncture and moxibustion treatment of hemorrhoids based on data mining. Chinese Archives of Traditional Chinese Medicine 35(12):2994–2996. https://doi.org/10.13193/j.issn.1673-7717.2017.12.003
Yu X, Ma Z (2011) Electroacupuncture for pain after hemorhoids surgery. Shanghai J Acupunct Moxibustion 30(05):304–306
Xia W, Park B, Otutaha BF, MacFater WS, MacCormick AD, Sammour T et al (2020) Topical analgesia following excisional haemorrhoidectomy: a systematic review and meta-analysis of randomised controlled trials. Int J Colorectal Dis 35(2):181–197
Xiaoyun H, Yue L, Hao J, Ningning M, Jiao W (2021) Effect of electroacupuncture at Zusanli on postoperative pain and inflammatory stress response of mixed hemorrhoids. Shanghai Journal of Acupuncture and Moxibustion 40(12):1418–1423. https://doi.org/10.13460/j.issn.1005-0957.2021.12.1418
Huang YJ, Chen CY, Chen RJ, Kang YN, Wei PL (2018) Topical diltiazem ointment in post-hemorrhoidectomy pain relief: a meta-analysis of randomized controlled trials. Asian J Surg 41(5):431–437
Ratnasingham K, Uzzaman M, Andreani SM, Light D, Patel B (2010) Meta-analysis of the use of glyceryl trinitrate ointment after haemorrhoidectomy as an analgesic and in promoting wound healing. Int J Surg 8(8):606–611
Siddiqui MR, Abraham-Igwe C, Shangumanandan A, Grassi V, Swift I, Abulafi AM (2011) A literature review on the role of chemical sphincterotomy after Milligan-Morgan hemorrhoidectomy. Int J Colorectal Dis 26(6):685–692
Chen H, Zhang W, Sun Y, Jiao R, Liu Z (2022) The role of acupuncture in relieving post-hemorrhoidectomy pain: a systematic review of randomized controlled trials. Front Surg 9:815618. https://doi.org/10.3389/fsurg.2022.815618
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C et al (2015) The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 162(11):777–784
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Davis BR, Lee-Kong SA, Migaly J, Feingold DL, Steele SR (2018) The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of hemorrhoids. Dis Colon Rectum 61(3):284–292
Ala S, Saeedi M, Eshghi F, Rafati M, Hejazi V, Hadianamrei R (2013) Efficacy of 10% sucralfate ointment in the reduction of acute postoperative pain after open hemorrhoidectomy: a prospective, double-blind, randomized, placebo-controlled trial. World J Surg 37(1):233–238
Vejdan AK, Khosravi M, Amirian Z, Daneshmand M, Babak B, Samira K et al (2020) Evaluation of the efficacy of topical sucralfate on healing haemorrhoidectomy incision wounds and reducing pain severity: a randomised clinical trial. Int Wound J 17(4):1047–1051
Albatanony AA (2016) Sucralfate ointment reduces pain and improves healing following haemorrhoidectomy: a prospective, randomized, controlled and double-blinded study. Egypt J Surg 35(2):102–105
Patti R, Luigi AP, Matteo A, Sergio S, Pietro R, Calogero F et al (2006) Botulinum toxin vs. topical glyceryl trinitrate ointment for pain control in patients undergoing hemorrhoidectomy: a randomized trial. Dis Colon Rectum 49(11):1741–1748
Patti R, Almasio PL, Muggeo VM, Buscemi S, Arcara M, Matranga S et al (2005) Improvement of wound healing after hemorrhoidectomy: a double-blind, randomized study of botulinum toxin injection. Dis Colon Rectum 48(12):2173–2179
Alvandipour M, Tavallaei M, Rezaei F, Khodabakhsh H (2021) Postoperative outcomes of intrasphincteric botox injection during hemorrhoidectomy: a double-blind clinical trial. J Res Med Sci 26:53. https://doi.org/10.4103/jrms.JRMS_612_18
Wu J, Chen B, Zhang X, Yin P, Xu S (2016) Therapeutic observation of surround electroacupuncture in relieving pain after operation for mixed hemorrhoids. Shanghai J Acupunct Moxibustion 35(06):680–683
Zhu Y, Jin Z, Huang L, Chang Z, Cao L, Zou Q (2021) clinical study on electroacupuncture in the treatment of postoperative pain of mixed hemorrhoids after internal binding and external excising. Modern J Integr Trad Chin West Med 30(27):2987–2990+2995
Wu J, Chen B, Yin X, Yin P, Lao L, Xu S (2018) Effect of acupuncture on post-hemorrhoidectomy pain: a randomized controlled trial. J Pain Res 11:1489–1496
Wang W, Han E, Zhang J, Wu H, Wu L (2018) Study on topical diltiazem in the control of post-hemorrhoidectomy pain. Jilin Med J 39(08):1454–1455
Yadav S, Khandelwal RG, Om P, Ravindra K, Choudhary KL (2018) A prospective randomized double-blind study of pain control by topical calcium channel blockers versus placebo after Milligan-Morgan hemorrhoidectomy. Int J Colorectal Dis 33(7):895–899
Amoli H, Notash A, Shahandashti F, Kenari A, Ashraf H (2011) A randomized, prospective, double-blind, placebo-controlled trial of the effect of topical diltiazem on posthaemorrhoidectomy pain. Colorectal Dis 13(3):328–332
Vahabi S, Beiranvand S, Karimi A, Moradkhani M (2019) Comparative study of 0.2% glyceryl trinitrate ointment for pain reduction after hemorrhoidectomy surgery. Surg J 5(04):e192–e196
Ho YH, Tan M (1997) Ambulatory anorectal manometric findings in patients before and after haemorrhoidectom. Int J Colorectal Dis 12(5):296–297
Vijayaraghavalu S, Prasad RG, Rajkumar S (2021) The role of lateral internal sphincterotomy in haemorrhoidectomy: a study in a tertiary care center. Cureus 13(6):e15630
Wang WG, Lu WZ, Yang CM, Yu KQ, He HB (2018) Effect of lateral internal sphincterotomy in patients undergoing excisional hemorrhoidectomy. Medicine (Baltimore) 97(32):e11820
Chauhan A, Tiwari S, Mishra VK, Bhatia PK (2009) Comparison of internal sphincterotomy with topical diltiazem for post-hemorrhoidectomy pain relief: a prospective randomized trial. J Postgrad Med 55(1):22–26
Carapeti EA, Kamm MA, Phillips RK (2000) Topical diltiazem and bethanechol decrease anal sphincter pressure and heal anal fissures without side effects. Dis Colon Rectum 43(10):1359–1362
Loder PB, Kamm MA, Nicholls RJ, Phillips RK (1994) ‘Reversible chemical sphincterotomy’ by local application of glyceryl trinitrate. Br J Surg 81(9):1386–1389
Zhang R, Lao L, Ren K, Berman BM (2014) Mechanisms of acupuncture-electroacupuncture on persistent pain. Anesthesiology 120(2):482–503
Author information
Authors and Affiliations
Contributions
Conception: Li Qiu and Guofeng Li; software: Yue Yang, Yuting Lei, and Ke Feng; writing original draft preparation: Yue Yang, Ke Feng, and Yuting Lei; review and editing: Yue Yang, Guofeng Li, and Chengjiang Liu.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, Y., Feng, K., Lei, Y. et al. Comparing the efficacy and safety of different analgesic strategies after open hemorrhoidectomy: a systematic review and network meta-analysis. Int J Colorectal Dis 38, 4 (2023). https://doi.org/10.1007/s00384-022-04294-5
Accepted:
Published:
DOI: https://doi.org/10.1007/s00384-022-04294-5