Abstract
Background
Restorative proctocolectomy with ileal-pouch anal anastomosis (IPAA) is a curative and cancer preventative procedure in patients with ulcerative colitis (UC) and familial adenomatous polyposis (FAP). It can be technically difficult laparoscopically, and hence the robotic platform has been suggested as a way to enable minimally invasive surgery in more patients. This systematic review examines robotic proctectomy or proctocolectomy with IPAA. A limited meta-analysis was performed on data comparing the robotic approach to laparoscopy.
Methods
We searched MEDLINE, EMBASE and the Cochrane database for case series of robotic IPAA procedures and studies comparing the robotic to laparoscopic or open procedures. Data examined includes operating time, conversion to open, length of stay, complications, blood loss, return of bowel function, reoperation rate and functional outcomes.
Results
Five non-randomised studies compared robotic to laparoscopic techniques; one compared robotic to open surgery and three case series are included. Operating time was significantly longer in robotic cases. Estimated blood loss was significantly less in three of four studies which reported this; hospital stay was significantly less in two. There were nonsignificant reductions in complications and readmission rates. Pooled analysis of four papers with adequate data showed a nonstatistically significant trend to less complications in robotic procedures. Three studies assessed functional and quality of life outcomes, with little difference between the platforms.
Conclusions
Available data suggests that the robotic platform is safe to use for IPAA procedures. There is minimal evidence for clinical advantages, but with little data to base decisions and significant potential for improvements in technique and cost-effectiveness, further use of the platform for this operation is warranted. It is vital that this occurs within an evaluation framework.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA) is the procedure of choice for many patients with ulcerative colitis (UC), offering an effective cure when medical treatments have been insufficient, while avoiding a permanent stoma. The technique is also an effective strategy to reduce risk of malignancy in patients with UC and patients with familial adenomatous polyposis (FAP).
The procedure has three stages, which can be performed over one, two or three separate operations: total colectomy, proctectomy and IPAA with loop ileostomy, and lastly the reversal of the ileostomy. Like many procedures that were initially performed via an open incision, the laparoscopic approach has been utilised increasingly since it was first described in the 1990s [1]. This shift has resulted in longer operative times but faster recovery [2,3,4]. There is some evidence for better bowel function [2], and reduced impact on fertility and sexual function [5, 6]. A Cochrane review in 2009 [7] comparing open to laparoscopic IPAA found no significant differences in mortality or complications. Other long-term benefits to laparoscopy include lower rates of adhesive bowel obstructions [8] and better cosmesis [7]. Despite these positive attributes, the technical complexities of this pelvic operation have limited the uptake of the laparoscopic platform.
Since its introduction in the early 2000s, the use of robotic-assisted laparoscopy has gradually expanded from its initial use in urology across a number of surgical specialties. The wristed instruments, tremor reduction and three-dimensional, high-definition views are particularly valuable in confined spaces such as the pelvis. As a result, some surgeons report being more likely to attempt and complete more complex procedures [9], suggesting the platform may increase the proportion of patients able to benefit from a minimally invasive approach. The typically younger cohort of patients undergoing proctectomy and IPAA may particularly benefit from advantages of minimally invasive surgery, such as faster recovery and hence return to work. They are also expected to have a longer remaining life span during which to benefit from a reduction in morbidity and healthcare costs caused by adhesive complications.
Despite this, only a small number of reports of robotic IPAA procedures exist within the literature. The purpose of this literature review is to assess whether robotic restorative proctocolectomy is safe, and whether there are any advantages over laparoscopic surgery by performing a systematic review and meta-analysis of the current literature.
Method
Search strategy
Medical Literature Analysis and Retrieval System Online (MEDLINE), Excerpta Medica (EMBASE) and Cochrane databases were searched for studies between 1996 and 2020. MeSH search headings and keywords used were ‘robotics’, ‘robotic surgical procedures’, ‘robotic surgery’, ‘laparoscopy, ‘proctocolectomy’, ‘restorative’, ‘ileal pouch anal anastomosis’ and ‘IPAA’.
Evaluation of studies
Included studies were comparative studies or cases series of more than five patients where robotic IPAA was performed. Hybrid techniques were included provided the proctectomy part of the operation was performed robotically. Comparative studies were those comparing robotic proctectomy ± colectomy with IPAA to either a laparoscopic or open technique. Studies were excluded from the analysis if two or more of the outcomes of interest were not reported.
The quality of the papers was graded according to the Newcastle-Ottawa Quality Assessment Scales [10] for either case control studies or cohort studies as appropriate, which assigned a star rating out of nine.
Primary outcomes of interest were mortality and complication rates (in particular, anastomotic leak and ileus), operating time, conversion to open surgery, length of stay and readmission rates. Secondary outcomes were estimated blood loss, return of bowel function, reoperation rate, and functional and quality of life outcomes.
Statistical analysis
Due to reporting heterogeneity for continuous variables, only categorical variables were pooled. Hence, we were able to pool all complications, anastomotic leaks, ileus rates and hospital readmissions. These data were collected as absolute values and a Cochran-Mantel-Haenszel test was performed to generate odds ratios for each study and eventual pooled value. I2 statistic was performed to assess study heterogeneity and a p-value < 0.05 was considered significant. All data analysis was performed in R Studio Team (2015). RStudio: Integrated Development for R Studio, Inc., Boston, MA, and using the metaphor package for meta-analysis [11].
Results
Included studies
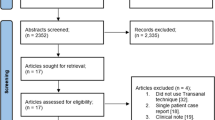
The initial search revealed 59 papers. After reviewing all titles and abstracts, 50 studies were identified for full-text review. Reasons for exclusion included the following: case reports or case series of five or less patients, video vignette papers with minimal outcome information, and a number of review articles, most looking broadly at all types of surgery related to inflammatory bowel disease. The search findings are summarised by the PRISMA flowchart in Fig. 1.
Ultimately, nine papers were included into this study. Six were comparative studies, and three were case series of robotic proctectomies with IPAA. The study characteristics are summarised in Table 1. Of the comparative studies, three papers and two conference abstracts compared robotic to laparoscopic procedures. Four of these were case matched reviews [13, 14, 16, 21] and one a cohort study [15] comparing robotic and laparoscopic cases, which was the largest study with more patients than the combined totals of the remaining papers comparing robotic to laparoscopic surgery. There was also one cohort study [17] comparing robotic to open procedures.
In total, 640 patients undergoing proctectomy ± colectomy and IPAA were included. 286 patients had robotic surgery, 174 patients laparoscopic and 170 had open surgery. A further 20 patients (10 robotic and 10 laparoscopic) included in two of these studies [13, 21] underwent proctectomy and end ileostomy. Ulcerative colitis or indeterminate colitis was the indication for surgery for most patients; however, in the robotic arm, the indication was Crohn’s disease for 6 patients, familial adenomatous polyposis or polyps for 13 patients and unspecified for 20 patients. In the laparoscopic arm, the indication was Crohn’s disease for 7 patients, familial adenomatous polyposis or polyps for 22 patients and unspecified for 18 patients. The indications in the largest comparative study [15] were significantly different, with 8% due to FAP in the robotic arm but 38% due to FAP in the laparoscopic arm (the remainder being ulcerative or indeterminate colitis in both arms).
Four of the papers contained suitable data for pooling the results for anastomotic leak and complication rates [13,14,15, 21], with one of these papers [15] being a conference abstract and the other three full peer-reviewed papers. Three peer-reviewed papers were suitable for pooling rates of ileus and hospital readmission [13, 15, 21].
Robotic surgical techniques
Overall, a two-stage procedure was performed in 71 robotic cases, meaning that the data reported pertains to the proctocolectomy and IPAA procedure. A three-stage procedure was performed in 148 robotic cases, indicating completion proctectomy and IPAA. Although all proctectomies were performed using the robotic platform, the platform used for the total colectomy stage of the operation varied; 10 patients had a robotic approach, 24 laparoscopic and six hand-assisted laparoscopy. Specimen extraction and pouch construction was via an open incision [17, 20, 21] in 101 patients while one group [19] extracted it via the anus in their six patients. A summary of the techniques can be seen in Table 2.
Main outcomes
There was no mortality in any of the studies. The main outcomes are summarised in Table 3.
Overall operating times ranged from means of 247 to 407 minutes for robotic cases and 234 to 316 minutes in laparoscopic cases. The mean operating time for open procedures was 130 min.
For two-stage procedures (proctocolectomy, IPAA and ileostomy), there were three noncomparative studies that reported operating times for robotic procedures. Their means were 247 and 407 minutes [18, 19] and a median of 380 min in the third study [20]. As for the three-stage procedures (proctectomy, IPAA and ileostomy), operating times for robotic procedures were reported as means of 284, 304 and 370 min [12, 13, 17]. To summarise, all the studies comparing robotic to laparoscopic surgery showed a longer operating time using the robotic technique, which was statistically significant in all studies.
Estimated blood loss in robotic cases ranged from means of 50 to 360 mL, and medians of 65 to 75 mL, while in laparoscopic cases, the range of means was 100 to 264 mL. Estimated blood loss was lower in the robotic cases than laparoscopic in two of the comparative studies (both statistically significant) but greater in the other two studies, though only statistically significant in one of these.
4% of robotic cases and 3% of laparoscopic cases were converted to open, with no statistically significant differences in any of the comparative papers. Mean times to first bowel motion after robotic surgery was 2.29 and 3.6 days in the two papers where this was reported [12, 13], compared with 2.6 and 2.79 days in the laparoscopic cases. Neither was a statistically significant difference. All papers reported length of hospital stay. The means in robotic cases ranged from 5.8 to 13.2 days. In the laparoscopic patients, means were from 6 to 11 days. Two papers [15, 16] reported statistically significant differences in time to hospital discharge in favour of robotic surgery. Mark-Christensen et al. [17] also reported a statistically significant shorter length of stay in robotic patients compared to those who had open surgery.
Postoperative complications are summarised in Tables 4 and 5. Mark-Christensen et al. [17] showed higher overall all complication rates in robotic patients (70% versus 50% of cases) compared to open. However, when broken down according to grade, the robotic patients experienced high numbers of lower grade complications, while those in the open cohort had more serious complications. The authors suspected biased reporting may have led to this, as patients undergoing a new technique may have been more closely monitored. Those studies comparing robotic to laparoscopic surgery showed little difference in complication rates or type. Four of the comparative studies contained comparable data suitable to pool overall complication rates. This showed an odds ratio of 0.65 in favour of robotic surgery, but was not significant with a 95% confidence interval of 0.38–1.12 (see Fig. 2)
.
Pooled analyses from the same four studies showed no statistically significant difference in anastomotic leak rates. Three of the comparative papers contained comparable data on ileus, and hospital readmission rates, with pooled analyses showing no statistically significant findings, though all showed a trend in favour of the robotic technique (see Figs. 2, 3, 4 and 5)
Functional and quality of life outcomes
The two conference abstracts briefly refer to these outcomes, with Marino et al. [14] stating that there were higher sexual function scores in robotic versus laparoscopic technique but quality of life scores did not differ. Domajnko et al. [18] also note in their conference abstract that all patients in their case series had ‘excellent’ functional outcomes aside from two patients subsequently diagnosed as Crohn’s disease.
Only three papers [12, 13, 19] explored functional or quality of life outcomes in any detail, and each used differing methods of comparison. In Miller et al.’s [12] study of 10 robotic and 10 laparoscopic IPAA procedures, 6 and 8 patients completed questionnaires, respectively. There were no significant differences between the groups. The bowel function questionnaire included an assessment of bowel movement frequency, nighttime movements, and need to adjust meal times to accommodate for bowel movements. For those who had IPAA, there was no significant difference in reported continence or ability to postpone bowel movements. Sexual function was also found to be similar between groups, and returned to preoperative levels in most patients regardless of the surgical platform used. Both groups reported high levels of satisfaction with the procedure, and quality of life scores were similar.
In their case series of 6 patients who underwent robotic restorative proctectomy, Morelli et al. [19] assessed bowel function, sexual and urinary function and quality of life. They assessed patients at 1, 6 and 12 months post-op, using International Index of Erectile Function (IIEF) [22], Female Sexual Function (FSFI) [23], Wexner [24] and Faecal Incontinence Quality of Life (mFIQL) [25] scores. These patients report continence for stool and flatus, no nighttime bowel movements and no need to adjust meal times to accommodate movements. Mean pouch frequency was 5.8 (± 1.3) times per day with no urgency. After an initial reduction of sexual and urinary function, scores returned to preoperative levels at 6 months and 1 year postoperatively. Quality of life at one year was equal to preoperative levels in the FAP patients, and the patient with UC had an improved score.
Rencuzogullari et al. [13] assessed quality of life using the Cleveland Global Quality of Life score (CGQOL) [26] and the 12 item Short Form survey (SF12) [27] (both mental and physical components), with no significant difference seen between the 21 patients in the robotic and laparoscopic groups in their study.
Surgeon learning curve
Among the comparative studies used to pool data, Miller et al. and Rencuzogullari et al. describe this as their ‘initial’ or ‘early’ experience. Rencuzogullari et al state that surgeons were experienced colorectal surgeons, but there is no description for either study as to experience with robotic surgery. Marino et al. and Lightner et al., however, do not provide any information on the learning curve status of the surgeons.
In the other papers, Mark-Christensen et al., Morelli et al. and Hamzaoglu et al. have described their series as their initial experiences. Mark-Christensen et al. also state that open surgeons were experienced, but some robotic procedures were performed by fellows under their supervision; their robotic experience was not described. Morelli et al. state that the surgeons were experienced in both laparoscopy and robotic surgery.
Discussion
In this systematic review of non-randomised studies addressing robotic restorative proctocolectomy, it has been shown that the procedure can be performed safely, with equivalent rates of overall complications, anastomotic leaks and returns to theatre. There were no reported deaths for this procedure in either laparoscopic or robotic arms. The potential added benefit (although not pooled) is the lower conversion rate and estimated blood loss in exchange for a longer operative time.
It is now clear that the benefits of minimally invasive colorectal surgery include reduced overall pain, ileus rates, surgical site infections and reductions in length of stay. However, limitations in laparoscopy such as inflexible instruments (particularly around acute angles) and 2D visualisation of tissue make dissection, particularly in a narrow pelvis, challenging [28]. This has driven the evolution of the robotic platform in colorectal surgery, adapted from its beginnings in urological procedures [28]. As the applications of the robotic platform are expanded, it is crucial to ensure that patient safety is not compromised, with widely accepted standard of care measurements such as mortality, complication rates and morbidity [29]. To our knowledge, this is the first review specifically assessing robotic restorative proctocolectomy, its safety profile and functional outcomes. This is a technique used for UC, a subsection of inflammatory bowel disease, as well as for FAP. It therefore has specific considerations that warrant this closer examination, being a technique often used for younger patients and benign disease.
The available data, as reviewed in this paper, does not show any evidence for a lack of safety in performing restorative proctectomy using the robotic platform, despite our inexperience. This reflects the evidence in other robotic procedures. Therefore, it is reasonable to continue to develop the technology in the rational belief that the significant potential for improvements to the platform may lead to clinical benefits in future. The key to justifying integration of the robotic platform into routine care will be to identify clinical benefits while addressing the two main detractors which are consistently identified: increased operating times and increased costs.
Robotic techniques are generally felt to be easier than standard laparoscopy, and this has been reflected in studies showing a faster learning curve [30, 31] and lower conversion rates [28]. This is thought to be related to a more stable view and greater dexterity, though it does come with additional skills to master, such as coordinating the docking procedure, minimising instrument clashes and adjusting to the total loss of haptic feedback [31]. As a result of this perception of an easier technique, it has been suggested that some surgeons tend to select the robotic platform for more complex cases [9] and may do so relatively early in their learning curve [32]. This may be a source of selection bias in non-randomised trials.
This paper shows longer operating times in the robotic cases, consistent with studies on other robotic procedures. This can have a significant impact on the cost of a procedure. However, progressive reductions in operating time are seen with growing experience [12, 17] as would be expected in any new technique. With inadequate information on the experience of the surgeons in these studies, it is difficult to determine the extent to which their learning curves may have affected the reported operating times.
The technology used in robotic surgery has far more potential for ongoing advances than laparoscopy so the possibility for the platform to gain superiority over laparoscopy in the future must be considered. If this possibility eventuates, and predictions of lower costs eventuate, the robotic platform will likely become a routine part of colorectal practice, particularly for more specialised procedures such as proctectomy and IPAA, which are more likely to be done in larger centres with robotic access. As such ongoing development and the collection of unbiased, high quality data is vital.
The limitations of this study are predominantly related to the small amount of data and the heterogeneity and quality of the papers, with 3 studies having been published as conference abstracts only, and therefore limited in detail and not peer reviewed. One of these abstracts was included in the pooled analysis for anastomotic leak and complication rates. In some of the papers, details of the surgical technique were missing or unclear. Where it was reported, there were significant differences between the surgical techniques used. Some included cases where a completion proctectomy with end ileostomy was performed. Although these were case-matched studies, nonetheless, comparison of proctectomies with IPAA to those without is clearly problematic, affecting, in particular, operative time and anastomotic leak rates. The procedure was performed in either two or three stages. Most of the papers used the same number of stages for most of their patients. However, two of the four comparative studies report a mixture of two and three stage procedures. This includes the largest comparative study [15], in which half of the robotic patients had UC and three-stage procedures and the other half had a two-stage procedures and a diagnosis of FAP. In the laparoscopic arm, however, almost all of the patients had FAP and two-stage procedures. This makes it likely that the surgeries in the laparoscopic arm were technically easier, with no previous pelvic inflammation or adhesions from the previous operation. On the other hand, their surgery involved a significant extra step (the colectomy). This difference in the indication and the procedure performed (both the inclusion or exclusion of the colectomy and the degree of difficulty) makes the comparison across all outcomes very difficult to interpret. Operating for FAP is a different operation than UC; the mixture of the two procedures in these studies limits the applicability of the results to both patients with UC and those with FAP.
Different techniques for the colectomy in two-stage operations further limit comparisons. This aspect of the procedure was performed by laparoscopy, hand-assisted laparoscopy or totally robotically—an approach that will reduce costs, as only one set of equipment is required, but increases operative time through multiple docking. Most of the studies did not specify whether the robotic platform used was Xi or the older Si, and this will also have important effects on operative and docking times, which are much shorter with the newer model [33]. With the more recent introduction of in-table motion technology, the docking procedures for multiquandrant surgery will be further minimised [33]. This highlights the need for ongoing assessment as techniques and technology evolve, and the need for clear documentation of the version of the technology that has been used, in order to enable comparisons between studies and allow surgeons to identify results that they can aim to emulate in their own practice according to local resources.
This heterogeneity in the technique, in addition to the small numbers and non-randomised nature of the studies means that there is significant potential for bias. Larger randomised trials are required to definitively prove or disprove the differences in outcomes seen here.
Conclusion
This study has examined the literature documenting the early implementation of the robotic platform for proctectomy ± colectomy and IPPA formation in benign disease and prophylactic resections. The procedure is safe with no significant adverse short-term outcomes. More data is required on short- and long-term clinical outcomes. Given that outcomes are equivalent to laparoscopic surgery, despite the technique being in its infancy, ongoing development is likely to improve on techniques and technology, while conventional laparoscopy has little room for ongoing development.
References
Ng KS, Gonsalves SJ, Sagar PM (2019) Ileal-anal pouches: a review of its history, indications, and complications. World J Gastroenterol 25(31):4320–4342. https://doi.org/10.3748/wjg.v25.i31.4320
Singh P, Bhangu A, Nicholls RJ, Tekkis P (2013) A systematic review and meta-analysis of laparoscopic vs open restorative proctocolectomy. Color Dis 15(7):e340–e351. https://doi.org/10.1111/codi.12231
Larson DW, Cima RR, Dozois EJ, Davies M, Piotrowicz K, Barnes SA, Wolff B, Pemberton J (2006) Safety, feasibility, and short-term outcomes of laparoscopic ileal-pouch-anal anastomosis: a single institutional case-matched experience. Ann Surg 243(5):667–670; discussion 670-662. https://doi.org/10.1097/01.sla.0000216762.83407.d2
White I, Jenkins JT, Coomber R, Clark SK, Phillips RK, Kennedy RH (2014) Outcomes of laparoscopic and open restorative proctocolectomy. Br J Surg 101(9):1160–1165. https://doi.org/10.1002/bjs.9535
Bartels SA, D'Hoore A, Cuesta MA, Bensdorp AJ, Lucas C, Bemelman WA (2012) Significantly increased pregnancy rates after laparoscopic restorative proctocolectomy: a cross-sectional study. Ann Surg 256(6):1045–1048. https://doi.org/10.1097/SLA.0b013e318250caa9
Beyer-Berjot L, Maggiori L, Birnbaum D, Lefevre JH, Berdah S, Panis Y (2013) A total laparoscopic approach reduces the infertility rate after ileal pouch-anal anastomosis: a 2-center study. Ann Surg 258(2):275–282. https://doi.org/10.1097/SLA.0b013e3182813741
Ahmed Ali U, Keus F, Heikens JT, Bemelman WA, Berdah SV, Gooszen HG, van Laarhoven CJ (2009) Open versus laparoscopic (assisted) ileo pouch anal anastomosis for ulcerative colitis and familial adenomatous polyposis. Cochrane Database Syst Rev 1:CD006267. https://doi.org/10.1002/14651858.CD006267.pub2
Ha GW, Lee MR, Kim JH (2016) Adhesive small bowel obstruction after laparoscopic and open colorectal surgery: a systematic review and meta-analysis. Am J Surg 212(3):527–536. https://doi.org/10.1016/j.amjsurg.2016.02.019
Narasimhan V, Das A, Waters P, McCormick J, Heriot A, Warrier S (2020) Complete mesocolic excision and central vascular ligation for right-sided cancers: is it time to jump on board? ANZ J Surg 90(1-2):11–12. https://doi.org/10.1111/ans.15444
Stang A (2010) Critical Evaluation Of The Newcastle Ottawa scale for the assessment of the quality of non randomized studies in meta analyses. Eur J Epidemiol 25:603–605. https://doi.org/10.1007/s10654-010-9491-z
Viechtbauer W (2010) Conducting meta-analyses in R with the metafor package. J Stat Softw 36(3):1–48
Miller AT, Berian JR, Rubin M, Hurst RD, Fichera A, Umanskiy K (2012) Robotic-assisted proctectomy for inflammatory bowel disease: a case-matched comparison of laparoscopic and robotic technique. J Gastrointest Surg 16(3):587–594. https://doi.org/10.1007/s11605-011-1692-6
Rencuzogullari A, Gorgun E, Costedio M, Aytac E, Kessler H, Abbas MA, Remzie FH (2016) Case-matched comparison of robotic versus laparoscopic proctectomy for inflammatory bowel disease. Surg Laparosc Endos Percutan Tech 26:e37–e40
Marino MV, Glagoleva A (2018) Robotic-assisted vs. laparoscopic proctectomy for inflammatory bowel disease: results of the case-match comparison in single institution. J Crohn's Colitis 12(Supplement 1):S322
Lightner AL, Grass F, McKenna NP, Tilman M, Alsughayer A, Kelley SR, Behm K, Merchea A, Larson DW (2019) Short-term postoperative outcomes following robotic versus laparoscopic ileal pouch-anal anastomosis are equivalent. Tech Coloproctol 23(3):259–266. https://doi.org/10.1007/s10151-019-01953-8
Elias AW, Landmann RG (2019) Chasing Zero Cuff: Robotic distal dissection superior to laparoscopy in ileal pouch anal anastomosis. Gastroenterology 156(6 S1):S-1496
Mark-Christensen A, Pachler FR, Norager CB, Jepsen P, Laurberg S, Tottrup A (2016) Short-term outcome of robot-assisted and open IPAA: an observational single-center study. Dis Colon Rectum 59(3):201–207. https://doi.org/10.1097/DCR.0000000000000540
Domajnko B, Ognibene S, Farid A, Rauh S (2012) Robotic ileal pouch-anal anastomoses: the first 27 cases. Dis Colon Rectum 55(5):e179–e180
Morelli L, Guadagni S, Mariniello MD, Furbetta N, Pisano R, D'Isidoro C, Caprili G, Marciano E, Di Candio G, Boggi U, Mosca F (2015) Hand-assisted hybrid laparoscopic-robotic total proctocolectomy with ileal pouch--anal anastomosis. Langenbeck's Arch Surg 400(6):741–748. https://doi.org/10.1007/s00423-015-1331-x
Hamzaoglu I, Baca B, Esen E, Aytac E, Ozben V, Aghayeva A, Bilgin I, Karahasanoglu T (2020) Short-term results after totally robotic restorative total proctocolectomy with ileal pouch anal anastomosis for ulcerative colitis. Surg Laparosc Endos Percutan Tech 30:40–44
Miller PE, Dao H, Paluvoi N, Bailey M, Margolin D, Shah N, Vargas HD (2016) Comparison of 30-day postoperative outcomes after laparoscopic vs robotic colectomy. J Am Coll Surg 223(2):369–373
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A (1997) The International Index of Erectile Function (IIEF): A multidimensional scale for assessment of erectile dysfunction. Urology 49(6):822–830
Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, Ferguson D, D'Agostino R (2000) The Female Sexual Function Index (FSFI): a multidimensional self report instrument for the assessment of female sexual function. J Sex Marital Ther 26:191–208. https://doi.org/10.1080/009262300278597
Vaizey C, Carapeti E, Cahill J, Kamm M (1999) Prospective comparison of faecal incontinence grading systems. Gut 44:77–80
Hashimoto H, Shiokawa H, Funahashi K, Saito N, Sawada T, Shirouzu K, Yamada K, Sugihara K, Watanabe T, Sugita A, Tsunoda A, Yamaguchi S, Teramoto T (2010) Development and validation of a modified fecal incontinence quality of life scale for Japanese patients after intersphincteric resection for very low rectal cancer. J Gastroenterol 45(9):928–935. https://doi.org/10.1007/s00535-010-0239-z
Fazio VW, O'Riordain MG, Lavery IC, Church JM, Lau P, Strong SA, Hull T (1999) Long-term functional outcome and quality of life after stapled restorative proctocolectomy. Ann Surg 230(4):575
Ware JE, Kosinski M, Keller S (1996) A 12-item short-form health survey. Med Care 34(3):220–233
Prete FP, Pezzolla A, Prete F, Testini M, Marzaioli R, Patriti A, Jimenez-Rodriguez RM, Gurrado A, Strippoli GFM (2018) Robotic versus laparoscopic minimally invasive surgery for rectal cancer: a systematic review and meta-analysis of randomized controlled trials. Ann Surg 267(6):1034–1046. https://doi.org/10.1097/SLA.0000000000002523
Jones HJS, de Cossart L (1999) Risk scoring in surgical patients. Br J Surg 86:149–157
Foo CC, Law WL (2016) The learning curve of robotic-assisted low rectal resection of a novice rectal surgeon. World J Surg 40(2):456–462. https://doi.org/10.1007/s00268-015-3251-x
de’Angelis N, Lizzi V, Azoulay D, Brunetti F (2016) Robotic versus laparoscopic right colectomy for colon cancer: analysis of the initial simultaneous learning curve of a surgical fellow. J Laparoendosc Adv Surg Tech A 26(11):882–892
Shaw DD, Wright M, Taylor L, Bertelson NL, Shashidharan M, Menon P, Menon V, Wood S, Ternent CA (2018) Robotic colorectal surgery learning curve and case complexity. J Laparoendosc Adv Surg Tech A 28(10):1163–1168. https://doi.org/10.1089/lap.2016.0411
Guadagni S, di Franco G, Palmeri M, Furbetta N, Gianardi D, Morelli L (2019) Total abdominal proctocolectomy: what is new with the da Vinci Xi? J Robot Surg 13(5):711–712. https://doi.org/10.1007/s11701-019-00970-x
Acknowledgements
The authors gratefully acknowledge the Epworth Knowledge Services’ contribution to collating the required papers for this work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design, material preparation, data collection and analysis. The first draft of the manuscript was written by J Flynn and JT Larach, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate and for publication
Not required.
Conflict of interest
J Flynn: no conflicts of interest or financial ties to disclose. JT Larach: educational grant funded by Intuitive Surgical. J Kong: no conflicts of interest or financial ties to disclose. S Warrier: honorarium for proctoring robotic cases. A Heriot: no conflicts of interest or financial ties to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Flynn, J., Larach, J.T., Kong, J.C.H. et al. Robotic versus laparoscopic ileal pouch-anal anastomosis (IPAA): a systematic review and meta-analysis. Int J Colorectal Dis 36, 1345–1356 (2021). https://doi.org/10.1007/s00384-021-03868-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-021-03868-z